Prosthesis survival after revision knee arthroplasty for “pain without loosening” versus “aseptic loosening”: a Danish nationwide study
Kristine Bollerup ARNDT 1,2, Henrik M SCHRØDER 3,4, Anders TROELSEN 5, and Martin LINDBERG-LARSEN 1,2
1 Department of Orthopaedic Surgery and Traumatology, Odense University Hospital; 2 Department of Clinical Research, University of Southern Denmark, Odense; 3 Department of Regional Health Research, University of Southern Denmark, Odense; 4 Department of Orthopaedic Surgery, Naestved Hospital. Naestved; 5 Department of Orthopaedic Surgery, Copenhagen University Hospital, Hvidovre, Denmark
Background and purpose — Patients having a knee arthroplasty revision for the indication “pain without loosening” may have a higher risk of re-revisions than patients revised for other indications. The primary aim of this study was to compare the survival of knee arthroplasties revised for “pain without loosening” compared with “aseptic loosening.” The second was to investigate the prosthesis survival rates in 3 surgical subgroups (total knee arthroplasty (TKA)–TKA; partial revision (revision of tibial or femoral component); unicompartmental knee arthroplasty–TKA) and to compare the prosthesis survival rates for 1997–2009 and 2010–2018.
Patients and methods — 4,299 revisions were identified in the period 1997–2018 from the Danish Knee Arthroplasty Register. Of these, 1,111 (26%) were performed due to “pain without loosening” without any other indications, 674 (16%) due to “pain without loosening” combined with other indications, and 2,514 (59%) due to “aseptic loosening”. Survival analysis was performed by a Cox multivariate analysis and Kaplan–Meier curves were presented.
Results — The cumulated proportions of re-revision after 2, 5, and 20 years were 12% (95% CI 10–14), 18% (CI 16–20), and 23% (CI 20–25) for “pain without loosening” versus 11% (CI 9.3–12), 16% (CI 14–17), and 19% (CI 18–21) for “aseptic loosening.” There were no statistically significant differences between the 2 indications in repeated analyses for each of the surgical subgroups. The hazard ratio for re-revision comparing “pain without loosening” with “aseptic loosening” was 1.03 (CI 0.87–1.2). The 8-year risk of re-revision for “pain without loosening” was 22% (CI 19–26) versus 22% (CI 20–25) for “aseptic loosening” in the period from 1997–2009, and 18% (CI 15–22) versus 14% (CI 13–16) in the period from 2010–2018.
Interpretation — The risk of re-revision was similar for patients having a knee arthroplasty revision for the indication “pain without loosening” compared with “aseptic loosening.” However, we observed a slight improvement of prosthesis survival rates after revisions for both indications from 1997–2009 to 2010–2018. We cannot recommend for or against revision in cases with “pain without loosening” based on these data alone.
Citation: Acta Orthopaedica 2022; 93: 103–110. DOI http://dx.doi.org/10.1080/17453674.2021.1999069.
Copyright: © 2021 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2021-06-02. Accepted: 2021-10-08. Published: 2022-01-03.
Correspondence: kristine.bollerup.arndt@rsyd.dk
KBA, HMS, AT, and MLL designed the study protocol. The analyses were planned by KBA, HMS, AT, and MLL and conducted by KBA. KBA drafted the manuscript, which was critically revised first by MLL and later by HMS and AT.
The authors acknowledge Odense Patient data Explorative Network for their help and advice on this study. Furthermore, they thank Odense University Hospital and the University of Southern Denmark for their financial support.
Acta thanks Ove N Furnes and Andreas Kappel for help with peer review of this study.
The number of primary knee arthroplasties—and the number of revisions—is expected to increase over the next decades (1). Up to 20% of patients experience some degree of knee pain after a primary total knee arthroplasty (TKA) and an even higher proportion after revision knee arthroplasty (2–6). Petersen et al. reported persistent pain in 47% of patients after a revision TKA for any indication compared with 19% after a primary TKA (6).
Revision TKA on the grounds of unexplained pain is generally not recommended (3,6,7). Revision TKA in the absence of knee pathology may not relieve pain, and it may result in worse outcome and higher rates of re-revision than for TKA revision for more established indications such as “aseptic loosening.” Re-revision TKA rates of 12–27% have been reported (8–11), but survival rates after revision TKA for various indications are unknown. Pain is available as an indication for TKA revision in most national orthopedic registries.
Although the number of TKA revisions is expected to increase, better outcomes are also expected due to improvements in revision surgery because of organizational changes in the healthcare system, including enhanced recovery programs, greater surgical experience with revision surgery, and technical developments such as improved bone substitution and fixation (12).
The primary aim of this study was to compare the prosthesis survival rates after TKA revision for the indication “pain without loosening” versus the indication “aseptic loosening.” Secondary aims were to investigate the prosthesis survival rates in four surgical subgroups (TKA–TKA, partial revision, unicompartmental knee arthroplasty (UKA)–TKA, secondary patellar button) and to compare the prosthesis survival rates for 1997–2009 and 2010–2018.
Patients and methods
This study is a nationwide retrospective cohort study of prospectively collected data from the Danish Knee Arthroplasty Register (DKR) and the Danish National Patient Register (DNPR). The RECORD guidelines for reporting of routinely collected, observational data were followed.
Data sources
Data on all knee arthroplasty revisions registered for the indications “pain without loosening” or “aseptic loosening” in the period January 1, 1997 to December 31, 2018 was collected from the Danish Knee Arthroplasty Register (DKR). DKR is a nationwide clinical database that has collected data on primary and revision knee arthroplasties in Denmark since 1997 (13). All hospital orthopedic departments (including private hospitals) report pre- and intraoperative data to the database. In 2018, the completeness of the register was 98% for primary arthroplasties and 95% for revision arthroplasties (14).
We obtained information on diagnosis and procedure codes from the Danish National Patient Registry (DNPR) for 1987 to 2018. The DNPR is an administrative registry established in 1977 that holds information on all hospital contacts in Denmark (15,16). Patients can be identified by their social security number—a personal unique 10-digit code that also enables linkage between registries. Information on patient characteristics including age, sex, and Charlson comorbidity index (CCI) were obtained from the DNPR (Table 1). The burden of comorbidities for each patient was estimated by the CCI, using the DNPR ICD-8 and ICD-10 diagnostic codes for the 10-year period up to the date of the first revision (Table 2, see Supplementary data). We classified patients into 3 groups according to their burden of comorbidities: CCI of 0 (low), CCI 1–2 (medium), or CCI ≥ 3 (high).
Participants
The study cohort comprised patients undergoing first-time TKA revision for the indications “pain without loosening” or “aseptic loosening” (control group). Patients who underwent bilateral revision were included in the study.
We defined surgical subgroups according to the type of prosthesis removed and the type of prosthesis inserted at the first revision. We included subgroup 1 (TKA–TKA), subgroup 2 (partial revision), subgroup 4 (unicompartmental knee arthroplasty (UKA)–TKA), and subgroup 5 (secondary patellar button). The included subgroups comprised numbers of revisions appropriate for further analysis and the types of revisions all included change of components, which is considered relevant for this study. We excluded subgroup 3 (liner exchange), subgroup 6 (UKA–UKA), subgroup 7 (hemicap), subgroup 8 (exchange of patellar button), subgroup 9 (all components removed), and subgroup 10 (spacer–TKA). The excluded subgroups comprised small numbers of revisions or did not include change of components, and were therefore not considered relevant to compare with the other subgroups. Furthermore, we excluded subgroup 5 (secondary patellar button) in combination with the indication “aseptic loosening” as these cases were considered to be misclassified in the register.
After exclusion of surgical subgroups and removal of duplicate records, 4,299 revisions were included in the study. Of these 1,111 (26%) were included on the indication “pain without loosening” without any other indications, 674 (16%) on the indication “pain without loosening” combined with other indications, and 2,514 (58%) on the indication “aseptic loosening” without any other indications.
For survival rate analysis TKA revisions were divided into 2 time groups, 1997–2009 and 2010–2018. 2009 was set as the cutoff point in order to have 2 almost equal sizes of groups for the analysis.
Outcomes
We extracted data from the DKR on all the re-revisions that were undertaken. Re-revisions registered in the DNPR on the procedure codes KNGU0-1 and KNGC0-9 were also obtained to ensure complete follow-up.
Statistics
The risks of re-revision at 2, 5, 10, 15, and 20 years are presented as cumulated proportions calculated as percentages with 95% confidence intervals (CI). The proportion were calculated both by indication (“pain without loosening” with and without other indications and “aseptic loosening”) and by surgical subgroups (for “pain without loosening” without other indications and “aseptic loosening”).
Survival analysis was performed using the Cox regression model to estimate the effect of the primary exposure variable “indication” on the outcome crude failure of revision knee arthroplasties, with adjustment for the covariates age groups, CCI, sex, and surgical subgroups. The estimates are presented as hazard ratios. To meet the model assumptions, data must be independent. The data of the unilaterally revised patients were assumed to be independent, but the data of bilaterally revised patients were assumed to be dependent. We adjusted for dependency by applying adjustment of the standard error for clustered data to our model. The model was tested for proportionality of hazards.
We used a Cox model to estimate the effect on the outcome “re-revision” for the secondary covariates age group, CCI, sex, and surgical subgroups when controlled for the primary exposure “indication” by the regression, calculated as hazard ratios. We present survival of knee arthroplasties as Kaplan– Meier curves. The level of statistical significance was set at 0.05 for all analyses.
The statistical software package Stata version 16.0 was used (StataCorp, College Station, TX, USA).
Ethics, funding, and potential conflicts of interest
The study was approved by the Danish Data Protection Agency (Journal no. 19/14416). Ethical approval was not needed as the study was non-interventional. The study was conducted in accordance with the Declaration of Helsinki. The study was funded by the Danish Rheumatism Association. The authors have no competing interests to declare.
Results
6,667 TKA revisions for the selected indications were identified in the DKR between 1997 and 2018 (Figure 1). The revisions were performed on 4,183 patients. 116 patients were bilaterally revised. The mean patient age for TKA revisions undertaken for “pain without loosening” (63 years; 29–92) was lower than that for TKA revisions undertaken for “aseptic loosening” (66 years; 22–96), p < 0.001, but the proportion of men and women was broadly similar (Table 1). 856 knees had undergone re-revision; 836 of these were identified from the DKR and 20 from the DNPR. The proportion of re-revisions after TKA revision was for “pain without loosening” without other indications (n = 252, 23%), “pain without loosening” with other indications (n = 128, 19%), and “aseptic loosening” (n = 476, 19%).

Figure 1. Flowchart of TKA revision cases identified and included in the study analysis.
The number of TKA revisions for “pain without loosening” increased from 2004 to 2012 and decreased thereafter, while revisions for “aseptic loosening” increased from 2001 to 2012 and decreased thereafter (Figure 2).
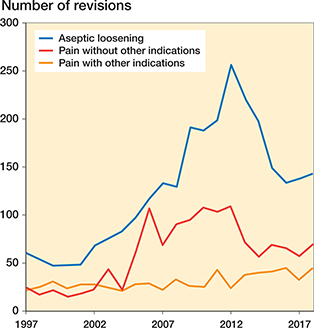
Figure 2. Incidence of TKA revision surgery for indications of “pain without loosening” with and without other indications and “aseptic loosening” without other indications. Data source = Danish Knee Arthroplasty Register, 1997–2018.
The cumulated proportions of re-revision after 2, 5, 10, 15, and 20 years are presented in Table 3. The proportion of re-revision after 20 years was slightly higher for “pain without loosening” without other indications (23%) than for “aseptic loosening” (19%), with overlapping confidence intervals at all follow-up times. This finding was unchanged when the analyses were repeated for each of the 4 surgical subgroups (Table 4 and Figure 3).

Figure 3. Kaplan–Meier survival curves with 95% confidence interval for the indications “pain without loosening” (without other indications) and “aseptic loosening” (without other indications).
The adjusted hazard ratio (HR) risk of re-revision for “pain without loosening” without other indications compared with “aseptic loosening” estimated by Cox regression was 1.03 (CI 0.87–1.2). Table 5 shows the effects of the covariates on the risk of revision adjusted for the effect of the primary exposure “indication.” The Charlson Comorbidity score did not influence the risk of re-revision. Subgroup 2 (partial revision) had increased risk of re-revision compared with subgroup 1 (TKA–TKA) with an HR of 1.52 (CI 1.26–1.83), p < 0.001. Male sex and age below 60 years increased risk of re-revision.
To estimate changes in risk of TKA re-revision over time, the cases were divided into 2 time-periods of 1997–2009 and 2010–2018 (Tables 6, 7, and Figure 4). For both indications, the 8-year risk of re-revision was higher in the first period (both 22%) than in the second period (14–18%).

Figure 4. Kaplan-Meier curves over 2 time-periods for the indications “pain without loosening” (without other indications) and “aseptic loosening” (without other indications). Aseptic loosening 1997–2009 reference (HR 1); Aseptic loosening 2010–2018: HR 0.87 (CI 0.72–1.04), p = 0.1; Pain 1997–2009: HR 1.06 (CI 0.87–1.30), p = 0.6; Pain 2010–2018: HR 1.19 (CI 0.88–1.62), p = 0.3.
A Cox regression was performed to explore any differences between the time-periods. HR for “pain without loosening” without other indications comparing the later time-period with the earlier time-period was 1.2 (CI 0.88–1.6). HR for “aseptic loosening” comparing the later time-period with the earlier time-period was 0.87 (CI 0.72–1.0). Thus, we did not find any statistically significant changes in the risk of revision for “pain without loosening” without other indications or “aseptic loosening.”
The time between the first revision and re-revision (Table 8) was slightly longer for “pain without loosening” without other indications (3.4 years [CI 2.9–3.8]) than for aseptic loosening” (2.9 years [CI 2.6–3.2]) (Table 1).
Discussion
In this study on prosthesis survival after total knee arthroplasty (TKA) revision, we found a slightly higher, but not statistically significant risk of re-revision after TKA revision for the indication “pain without loosening” without other indications compared with the indication “aseptic loosening”. Analyses for 3 surgical subgroups showed the same tendency. To our knowledge, this is the first study to report re-revision rates after TKA revisions performed because of unexplained pain. Our study findings oppose the general belief that revisions for pain should be avoided, as the risk of re-revision was not significantly elevated. However, many other aspects than re-revision rates should be considered. The threshold for performing a re-revision is possibly higher in patients who were initially revised due to pain than in those revised due to aseptic loosening, resulting in lower rates of re-revision for patients with persistent pain. Furthermore, we cannot draw any conclusions about whether patients experienced pain relief or improved quality of life after the revisions.
The indication “pain without loosening” can be combined with other indications when surgeons record the event in the DKR. According to the Australian Hierarchy of Indications, pain is inferior to all other indications for revision (17), thus the highest ranked indication is the dominant problem. This may explain why “pain without loosening” combined with other indications had a lower re-revision risk than “pain without loosening” without any other indications. The reason we include data for the indication “pain without loosening” without other indications is to provide estimates that are unbiased by other indications.
We investigated the risk of re-revision after TKA revision for the indications “pain without loosening” and “aseptic loosening” over the 2 time-periods 1997–2009 and 2010–2018. We observed an overall reduction in the proportion of re-revision on both indications in the later time-period compared with the earlier period, although the difference for “pain without loosening” was less pronounced than for “aseptic loosening.” The overall reduction in re-revision risk between time-periods was not statistically significant by the Kaplan–Meier estimates for either indication group. However, the 8-year cumulated proportion of re-revisions for TKA-to-TKA revisions (subgroup 1) changed from 20% in the earlier period to 12% in the later period for “aseptic loosening.” Encouragingly, this may be interpreted as an improvement over recent years in the performance of revision knee arthroplasties, especially for TKAs revised because of aseptic loosening.
There are limitations to this study. We are not able to present data on all index revisions performed nationwide as the completeness of revisions in the DKR is 89%, but a complete follow-up on re-revisions was ensured by using data from both DKR and DNPR (completeness > 99%) (15). We have no reason to believe that the lack of index revisions would bias our results in any way. The study may not have enough sample-size power to identify a statistically significant difference in the re-revision rates between the 2 indications, and no pre-study power calculation was performed as we included all available procedures.
The indication “pain without loosening” was itself associated with limitations. No validation of the indication has been done. It may be an exclusion indication chosen by the individual surgeon performing the surgery when there are no other obvious indications. No clear-cut definition of this indication exists, and it might cover a broad spectrum of patients who may or may not have a similar underlying problem.
Further investigations of the validity and use of this indication are warranted as well as clinical results after revisions performed on the basis of this indication.
In conclusion, we found similar risk of re-revision for patients having a knee arthroplasty revision for the indication of “pain without loosening” compared with that of “aseptic loosening.” We also did not find any differences at surgical subgroup level. However, we found a small improvement of prosthesis survival rates after revisions for both indications from 1997–2009 to 2010–2018, which we interpret as an improvement in the performance of revision knee arthroplasties. We cannot recommend for or against revision in cases with “pain without loosening” based on these data alone.
- Klug A, Gramlich Y, Rudert M, Drees P, Hoffmann R, Weißenberger M, et al. The projected volume of primary and revision total knee arthroplasty will place an immense burden on future health care systems over the next 30 years. Knee Surg Sports Traumatol Arthrosc 2020: 1-12.
- Baker P N, van der Meulen J H, Lewsey J, Gregg P J. The role of pain and function in determining patient satisfaction after total knee replacement: data from the National Joint Registry for England and Wales. J Bone Joint Surg Br 2007; 89(7): 893-900.
- Reichel F, Innmann M, Gotterbarm T, Schiltenwolf M, Merle C. [Predictors for persistent pain and dissatisfaction after total knee arthroplasty]. Schmerz (Berlin, Germany) 2019; 33(3): 185-90.
- Wylde V, Beswick A, Bruce J, Blom A, Howells N, Gooberman-Hill R. Chronic pain after total knee arthroplasty. EFORT Open Rev 2018; 3(8): 461-70.
- Lewis G N, Rice D A, McNair P J, Kluger M. Predictors of persistent pain after total knee arthroplasty: a systematic review and meta-analysis. Br J Anaesth 2015; 114(4): 551-61.
- Petersen K K, Simonsen O, Laursen M B, Nielsen T A, Rasmussen S, Arendt-Nielsen L. Chronic postoperative pain after primary and revision total knee arthroplasty. Clin J Pain 2015; 31(1): 1-6.
- Vince K G. The problem total knee replacement: systematic, comprehensive and efficient evaluation. Bone Joint J 2014; 96-b(11 Supple A): 105-11.
- Klasan A, Magill P, Frampton C, Zhu M, Young S W. Factors predicting repeat revision and outcome after aseptic revision total knee arthroplasty: results from the New Zealand Joint Registry. Knee Surg Sports Traumatol Arthrosc 2021; 29(2): 579-85.
- Chalmers B P, Pallante G D, Sierra R J, Lewallen D G, Pagnano M W, Trousdale R T. Contemporary revision total knee arthroplasty in patients younger than 50 years: 1 in 3 risk of re-revision by 10 years. J Arthroplasty 2019; 34(7s): S266-s70.
- Postler A, Lützner C, Beyer F, Tille E, Lützner J. Analysis of total knee arthroplasty revision causes. BMC Musculoskelet Disord 2018; 19(1): 55.
- Belt M, Hannink G, Smolders J, Spekenbrink-Spooren A, Schreurs B W, Smulders K. Reasons for revision are associated with rerevised total knee arthroplasties: an analysis of 8,978 index revisions in the Dutch Arthroplasty Register. Acta Orthop 2021: 1-5.
- Price A J, Alvand A, Troelsen A, Katz J N, Hooper G, Gray A, et al. Knee replacement. Lancet 2018; 392(10158): 1672-82.
- Pedersen A B, Mehnert F, Odgaard A, Schrøder H M. Existing data sources for clinical epidemiology: the Danish Knee Arthroplasty Register. Clin Epidemiol 2012; 4: 125-35.
- DKR. The Danish Knee Arthroplasty Register, Annual Report 2020.
- Schmidt M, Schmidt S A, Sandegaard J L, Ehrenstein V, Pedersen L, Sørensen H T. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 2015; 7: 449-90.
- Lynge E, Sandegaard J L, Rebolj M. The Danish National Patient Register. Scand J Public Health 2011; 39(7 Suppl.): 30-3.
- AONJRR. AOANJRR Annual Report. Adelaide: AOA; 2009.
- Quan H, Bing Li B, Couris C M, Fushimi K, Graham P, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 2011; 173(6): 676-82.
Supplementary data
| Charlson comorbidity | ICD, 8th edition | ICD, 10th edition | Charlson weight a |
| Myocardial infarction | 410 | DI121–22, DI252 | 0 |
| Congestive heart failure | 42709–10, 42719, 42899, 78249 | DI099–110, DI130, DI132, DI255, DI420, DI425–29, DI43, DI50, DP290 | 2 |
| Peripheral vascular disease | 440–45 | DI70–71. DI731, DI738–39, DI771, DI790, DI792, DK551, DK558–59, DZ958–59 | 0 |
| Cerebrovascular disease | 430–38 | DG45–46, DH340, DI60–69 | 0 |
| Dementia | 2900–1, 29309 | DF00–3, DF051, DG30, DG311 | 2 |
| Chronic pulmonary disease | 490–93, 515–18 | DI278–79, DJ40–47, DJ60–67, DJ684, DJ701, DJ703 | 1 |
| Rheumatologic disease | 712, 716, 734, 446, 13599 | DM05–6, DM315, DM32–34, DM351, DM353, DM360 | 1 |
| Peptic ulcer disease | 53091, 53098, 531–34 | DK25–28 | 0 |
| Mild liver disease | 571,57301, 57304 | DB18, DK700–3, DK709, DK713–15, DK717, DK73–74, DK760, DK762–64, DK768, DZ944 | 2 |
| Diabetes without chronic complications | 24900, 24906–7, 24909, 25000, 25006–7, 25009 | DE100–1, DE106, DE108–111, DE116, DE118–21, DE126, DE128–31, DE136, DE138–41, DE146, DE148, DE149 | 0 |
| Diabetes with chronic complications | 24901–5, 24908, 25001–5, 25008 | DE102–5, DE107, DE112–15, DE117, DE122–25, DE127, DE132–35, DE137, DE142–45, DE147 | 1 |
| Hemiplegia or paraplegia | 344 | DG041, DG114, DG801–2, DG81–82, DG830–34, DG839 | 2 |
| Renal disease | 403–4, 580–84, 59009, 59319, 7531, 792 | DI120, DI131, DN032–37, DN052–57, DN18–19, DN250, DZ490–92, DZ940, DZ992 | 1 |
| Any malignancy, including leukemia and lymphoma | 140–72, 174–94, 200–7, 27559 | DC00–26, DC30–34, DC37–41, DC43, DC45–58, DC60–76, DC81–85, DC88, DC90–97 | 2 |
| Moderate or severe liver disease | 7000, 7002, 7004, 7006, 57300, 4560 | DI850, DI859, DI864, DI982, DK704, DK711, DK721, DK729, DK765–67 | 4 |
| Metastatic solid tumor | 195–99 | DC77–80 | 6 |
| AIDS/HIV | 7983 | DB20–22, DB24 | 4 |
| a Charlson weight according to Quan 2011 (18). ICD = International Classification of Diseases |
|||