Long-term follow-up of 96 patients younger than age 25 with 119 primary cemented total hip arthroplasties
Erim Özdemir, Martijn F L Kuijpers, B Willem Schreurs, and Wim H C Rijnen
Radboud University Medical Center, Radboud Institute for Health Sciences, Department of Orthopedics, Nijmegen, The Netherlands
Background and purpose — Long-term follow-up of young patients following cemented primary THA is scarce. Therefore, we analyzed the survival of all consecutive primary THAs in patients under 25 years performed at our institute.
Patients and methods — All primary THAs performed in patients younger than 25 years in our tertiary care institute between 1988 and 2015 were included (n = 119). Cemented fixation was used in all patients. In the case of acetabular bone deficiencies, reconstruction was performed using impaction bone grafting (IBG). We used Kaplan–Meier analysis to determine the survival of the primary THA with endpoints revision for any reason and aseptic loosening.
Results — The mean age at the primary THA was 20 years. The most prevalent diagnosis was avascular necrosis (31%). The mean follow-up of the primary THA was 11 years (range 0–32). 2 patients (2 hips) were lost to follow-up. 16 revisions were registered. The survival of any component for endpoint revision for any reason was estimated at 92% (95% confidence interval [CI] 84–96) and 81% (CI 67–90) at 10- and 15-year follow-up, respectively. The survival of any component for endpoint revision for aseptic loosening was 99% (CI 93–100) and 88% (CI 71–95) at 10 and 15 years, respectively. 3 hips were revised due to infection.
Conclusion — Favorable long-term outcomes of primary THA in very young patients can be obtained using cemented fixation and IBG.
Citation: Acta Orthopaedica 2023; 94: 102–106 DOI: https://doi.org/10.2340/17453674.2023.9410.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-08-24. Accepted: 2023-01-04. Published: 2023-02-28.
Correspondence: wim.rijnen@radboudumc.nl
EÖ: data collection, assessment of radiologic images, performing analysis, writing the manuscript with input of all authors. MK: supervising the process, performing analysis, aided in interpreting the results. BWS: supervising the process, performed included surgeries, assessment of radiologic images, aided in interpreting the results. WR: supervising the process, assessment of radiologic images, aided in interpreting the results.
The authors would like to thank P A N Van der Voort, MSc, for her aid in the acquisition of patient data.
Handling co-editors: Li Felländer-Tsai and Philippe Wagner
Acta thanks Harald Brismar and Gösta Ullmark for help with peer review of this study.
Due to the benefits for quality of life, a total hip arthroplasty (THA) is nowadays more often performed in younger and younger patients. However, studies reporting the long-term follow-up of patients who had their THA performed under 25 years of age are scarce, and often based on small study populations or on mixed fixation techniques and bearings (1-15). Considering the low age at time of surgery, these young patients can expect revision procedures.
As reports of uniform treatment protocols in these very young patients are scarce, the aim of our study was to determine the 10- and 15-year clinical and radiological outcome of cemented primary THA in patients younger than 25 years. The primary outcomes were survival for the endpoint revision of any component for any reason and revision of any component due to aseptic loosening. The secondary outcomes were survival for the endpoint revision of any component due to infection, revision of the acetabular component for any reason, revision of the femoral component for any reason, revision of the acetabular component due to aseptic loosening, and revision of the femoral component due to aseptic loosening. Further secondary outcomes were radiographic outcomes and PROMs.
Patients and methods
We have follow the STROBE guidelines during the writing of this report. We performed a historical prospective cohort study including all THA patients who were younger than 25 years at the time of index surgery. All patients were treated and included in our tertiary care center between April 1988 and January 2015. All indications for the THA were included. Exclusion criterion was THA for an oncologic indication, however there were none in this cohort. According to our standard follow-up protocol, patients are evaluated regularly during their follow-up. For this study, all patients were clinically evaluated between January 2017 and 2021; however, 2 patients (2 hips) were lost to follow-up.
Surgery
In all patients, a cemented THA was performed. Surgical Simplex cement (Stryker, Newbury, UK) was used in 97% of hips and Palacos cement (Heraeus, Wehrheim, Germany) in 3% of hips. Third-generation cementing techniques were used, though in some early cases second-generation techniques were applied. The posterolateral approach was used in all cases. Different types of cemented implants were used over time. For cup components, the Exeter Contemporary flanged cup (72 hips), Exeter Contemporary hooded cup (13 hips), Exeter Rimfit X3 cup (13 hips), De Puy Elite Plus LPW cup (11 hips), Muller cup (6 hips), and unspecified Exeter cup (4 hips) were used. For stem components, Exeter polished stems (111 hips), Charnley/Charnley Elite stem (4 hips), and Muller straight stem (4 hips) were used. 13 of the cups were highly crosslinked polyethene, all others were conventional polyethylene. Cobalt-chrome femoral heads were used in all cases: 11 femoral heads had a diameter of 22 mm, 102 heads had a diameter of 28 mm, and 6 heads had a diameter of 32 mm. Antibiotics were administered preoperatively and postoperatively for a maximum of 24 hours. IBG was used to reconstruct acetabular defects in case of bone-stock deficiencies during the primary procedure, using autologous and/or allograft bone. The IBG technique has been described extensively in the literature previously (16). IBG of the acetabulum was performed in 93 hips. The impacted bone chips (8–12 mm) were produced out of femoral head autograft (n = 62), femoral head allograft (n = 10), or a combination of allograft and autograft (n = 21). If needed, segmental bone defects were reconstructed using mesh in combination with IBG (n = 51). In 4 hips a medial wall mesh, and in 42 hips a superolateral rim mesh was used. In 5 hips mesh was used both on the medial wall and on the superolateral rim.
Radiology and PROMs
All radiographic images were evaluated by at least 2 researchers (EÖ, BWS, WR) and were classified based on consensus. For all patients, we studied AP views. Radiologic loosening of the acetabular component was defined as radiolucent lines of more than 2 mm in all 3 zones according to Charnley (17), more than 5° tilting, and/or migration of 5 mm or more in any direction. Radiologic loosening of the stem was defined as the appearance of a radiolucent line in all AP Gruen zones (18) that did not exist on the immediate postoperative radiographs, or as a crack in the cement or fracture of the stem (19). Periarticular ossifications were scored according to Brooker (20).
For patient-reported outcome measures (PROMs), we used the Oxford Hip Score (OHS) and Harris Hip Score (HHS). Patients were asked to complete questionnaires preoperatively, and at 3 months and 1 year postoperatively. After the first year, patients were asked to complete the questionnaires biannually. Questionnaire series were continued until final follow-up. We included all OHSs since introduction of the questionnaire in 2001. All missing questionnaires due to this later introduction were considered as not completed.
Statistics
The follow-up of primary THA was calculated as time from the primary procedure to the date of final follow-up, revision procedure, or death of the patient. Bilateral THAs were considered as independent observations. The Kaplan–Meier survival analyses were used to estimate survival, including 95% confidence intervals (CI). Radiological findings and PROMS were analyzed using descriptive statistics. The data of patients who were lost to follow-up or deceased were included in the study until their latest clinical follow-up. Missing entries/data were not taken into the calculations.
Ethics, data sharing, funding, and disclosures
This study was evaluated by the local ethics committee in Nijmegen, Netherlands (file number 2021-8225). In terms of data sharing, data is available at Radboudumc Research server. No funding was received for conducting this study. The authors disclose receipt of the following financial or material support for the research, authorship, and/or publication of this article: WHR and BWS are involved in Stryker educational courses, therefore a reimbursement is sent to the department. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.9410
Results
In total, 96 patients (119 THAs) were included. 63 patients (76 THAs) were female. 67 THAs were performed on the left hip. The mean age at time of surgery was 20 years (range 12–24 years). The mean follow-up was 11 years (range 0–32 years). The most common diagnosis for THA was avascular necrosis (37 hips). Other diagnoses were developmental hip dysplasia (28 hips), Perthes disease (14 hips), juvenile rheumatoid arthritis (12 hips), rheumatoid arthritis (4 hips), epiphysiolysis (4 hips), primary osteoarthritis (2 hips), and 18 not specified diagnoses. 6 patients (8 hips) died after a mean follow-up of 9 years (range 4–18 years) due to causes not related to their THA. 2 patients (2 hips) were lost to follow-up after 2 and 4 years, respectively.
Survival
16 revisions were registered. The reasons for revision THA were aseptic loosening (7 hips), recurrent dislocations (3 hips), septic loosening (3 hips), wear (1 hip), and 2 for other reasons. Of the cups revised for aseptic loosening, 3 of 7 were reconstructed using mesh and IBG during primary THA and 1 of 7 initially had only IBG during primary THA. The survival of the THA in our study population with endpoint revision for any reason was 81% (CI 67–90) at 15-year follow-up (Figure 1). The survival of any component with endpoint aseptic loosening was 88% (CI 71–95) at 15-year follow-up. For the acetabular component, survival with endpoint revision for any reason was 84% (CI 69–92) at 15-year follow-up (Figure 2). The survival of the acetabular component with endpoint aseptic loosening was 88% (CI 70–94) at 15-year follow-up. For the femoral component, the survival with endpoint revision for any reason was 94% (CI 87–97) at 15-year follow-up (Figure 3). The survival of the femoral component for aseptic loosening was 100% at 15-year follow-up (Table 1). 3 hips were revised due to an infection of the implant. In these 3 cases, both components were revised after 0.3, 6, and 7 years (mean: 4.4), so there was 1 early infection and 2 late infections. Another 3 hips, all with a head diameter of 28 mm, were revised for recurrent dislocations.
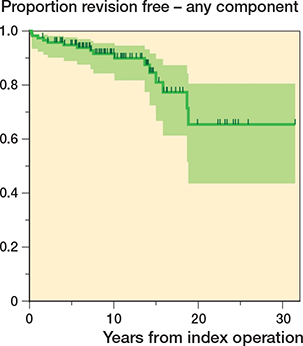
Figure 1. Kaplan–Meier curve—endpoint: revision of any component for any reason.
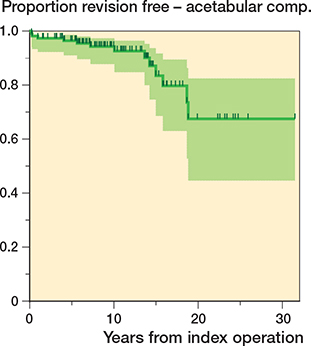
Figure 2. Kaplan–Meier curve—endpoint: acetabular component revision for any reason.
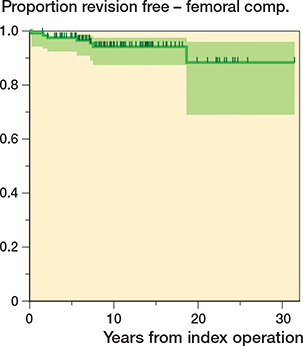
Figure 3. Kaplan–Meier curve—endpoint: femoral component revision for any reason.
Radiographic results
For all 119 hips radiographs were available for assessment. For revised THAs, the last radiograph before revision was used. The most recent radiographs were taken at a mean of 10 years (range 0–31; IQR 6–13) after primary THA.
For the acetabular component, radiolucent lines were found in 26 (22%) hips. According to the classification of DeLee and Charnley, radiolucency in zone 1 was found in 21 hips, in zone 2 in 3 hips, in zone 3 in 13 hips. Radiolucent lines in 2 zones were found in 8 hips and lines in all 3 zones, defining a radiolucent loosening, were found in 3 hips. Also, 4 acetabular components were found to have migrated; all had IBG during the primary THA. In total, therefore, 7 acetabular components were radiologically loose after a mean follow-up of 10 years (range 0.2–16; IQR 4–15); all were revised. There were no radiologically loose cups that were not revised. No periarticular ossification was found in 93 hips, Brooker grade 1 in 12 hips, grade 2 in 6 hips, grade 3 in 5 hips.
For the femoral component, according to the classification of Gruen, radiolucent lines were found in 4 (3%) hips. None of the 103 unrevised THAs were considered radiologically loose. The mean subsidence of the stem within the cement mantle was 1.5 mm (range 0.0–9.6). 14 femoral components subsided more than 3.0 mm after a mean follow-up of 11 years (range 6–26). However, given the fact the definition of radiological loosening based on subsidence in tapered stems is not well defined, we concluded that none of the stems were radiologically loose. In addition, there was no relation between migration of the stem and clinical complaints.
Clinical results
The median OHS increased from 24 (range 8–41) preoperatively to 41 (range 11–48) at 10 years postoperatively and 40 (range 11–48) at 15 years postoperatively. The HHS increased from 51 (range 23–100) preoperatively to respectively 91 (range 63–100) and 81 (range 47–100) at 10 and 15 years postoperatively (Table 2).
Discussion
In this paper we show that consistent use during more than 30 years of cemented THA, if need be combined with acetabular bone impaction grafting, leads to a survival of 81% (CI 67–90) for endpoint loosening of any component for any reason and a survival of 88% (CI 71–95) for endpoint aseptic loosening of any component at 15 years after surgery in patients aged under 25 years. Radiographically, the 103 unrevised hips did not show additional acetabular or femoral loosening.
Most studies on patients with a THA under the age of 25 years have shorter reported follow-up periods. However, Torchia et al. (3) reported on 63 cemented THAs in 50 patients under 20 years old; a subgroup of this original population was studied (40 patients, 52 THAs) at an average follow-up of 13 years. The survival reported with endpoint revision for any reason was 73% at 10 years and 55% at 15 years. Most revisions were performed for aseptic cup loosening. An explanation for their disappointing outcome is the period in which these implants were cemented, which was between 1972 and 1980. In this period only first-generation cementation techniques were used. Tsukanaka et al. (8) studied 111 patients with 132 THAs performed between 1987 and 2010, based on a register study from Norway. In their population, 89% of the cups and 95% of the stems were uncemented. All patients were aged under 20 years at surgery, and the survival at 10 years for endpoint revision for any reason was 70%. Witt et al. (2) reported on 96 cemented THAs in 54 patients who had surgery under the age of 27 years for juvenile rheumatoid arthritis with an average follow-up of 11.5 years. The survival rate with endpoint any reason was 75% at 10 years. The implants were inserted between 1969 and 1984, most with first-generation techniques. Wroblewski et al. (1) reported a small series of 28 patients with 39 cemented THA performed between 1968 and 2001; all patients were under 20 years old. Data extraction is difficult from this paper. 16 revisions were performed after an average of 19 years (8–34 years) after surgery, so the estimated survival is about 60% after 20 years of follow-up.
Many studies are based on a limited number of patients and THAs (1,7,11,12,14,15,21). Some studies report on more patients but with a very short follow-up. Clohisy et al. (13) reported on 88 patients with 102 THA, all aged under 25 years. These numbers are comparable with our study. However, the original series had 95 patients with 113 THAs. Thus, 11 THAs were lost within 2 years, which is about 10%. All sockets were uncemented, as were all but 5 stems. They reported 7 revisions at an average follow-up of 4.5 years, so the survival at 5 years for endpoint of any revision is about 94%. Given the relatively high number lost to follow-up, the survival may be considerably lower. Halvorsen et al. (9) described a study based on data from the NARA, the combined national registries of Norway, Sweden, Denmark, and Finland. They studied 881 THAs in 747 patients, all aged under 22 years. They reported survival with endpoint revision for any reason of 94% (CI 92–96) at 5 years, 86% (CI 83–89) at 10 years, and 73% (CI 68–78) at 15 years. Although more than 74% of their THAs were uncemented, they concluded that there was no statistically significant difference in outcome between cemented and uncemented THA. Most revisions were done for acetabular loosening. Another study based on large numbers is the registry study by Metcalfe et al. (6) using data from the NJR registry from the United Kingdom. They report on 769 THAs in 703 patients who were all aged under 20 years at the time of the surgery. There were 451 uncemented implants, 73 cemented, 147 other including (reverse) hybrids, and 88 resurfacing THAs. The survival with endpoint revision for any reason was 96% (CI 94–98) at 5 years. There was no statistically significant difference in outcome between uncemented and cemented fixation. However, metal-on-metal bearings and resurfacing THAs were at higher risk of revision. Sedrakyan et al. (4), using data from the AOANJRR (the Australian registry), reported on 297 THAs performed in patients aged under 21 years between 1999 and 2012. The cumulative revision rate at 5 years was 4.5% (CI 2–9).
Although there certainly is a strong trend to use uncemented total hip implants in young patients, none of the studies based on patients who had a THA performed under the age of 25 years proves the superiority of uncemented implants. Also, the register studies based on large data sets from many centers and many surgeons found no statistically significant difference in outcome between cemented and uncemented implants (6,9).
Strengths
One of the strengths of our study is the consistent use of surgical techniques using 1 type of fixation and 1 type of articulation. Only 2 patients were lost to follow-up, implying a near complete dataset for survival.
Limitations
As this is a non-comparative study, we cannot state whether there would be any difference between cement and uncemented implants. We hesitated to start early with highly cross-linked cemented cups as their long-term outcome was unclear until 10-year data was available. This, together with the use of several different component types, may have increased the revision rate.
In addition, in young patients with acetabular defects we advocate the use of acetabular IBG in combination with a cemented cup. A disadvantage is that there is certainly a learning curve for this technique. However, consequent use of the technique, especially in patients with developmental dysplasia of the hip, can prevent insufficient bone stock hampering future revision surgery as stated in the paper by Tsukanaka et al. (8).
In our study, bilateral THAs (n = 23) were considered independent observations. According to Bryant (22), inclusion of THA in both hips in 1 patient may produce bias by providing more observations with less variability. This may lead to an inaccurate estimation of the survival rate. To account for this chance of bias, we produced a sensitivity analysis of THA survival where the first THA was excluded for patients with bilateral THA. Here, we found a negligible difference in survival of only 0–2% for endpoint revision for any component for any reason and revision for any component for aseptic loosening, for 5–15 year follow-up. Therefore, we assume our results are minimally influenced by the possible bias created by including bilateral THA.
Conclusion
Our study shows favorable long-term results for cemented primary THA in combination with IBG in patients younger than 25 years old, up to 15 years postoperatively.
In perspective, it is important to consider the lifelong course of the THA in very young patients as these patients are expected to have a number of revisions over their lifetime. Further research should focus on the long-term outcomes of other techniques in young primary THA patients as well as the outcome of the inevitable subsequent revisions in these younger patients.
- Wroblewski B M, Purbach B, Siney P D, Fleming P A. Charnley low-friction arthroplasty in teenage patients: the ultimate challenge. J Bone Joint Surg Br 2010; 92(4): 486-8.
- Witt J D, Swann M, Ansell B M. Total hip replacement for juvenile chronic arthritis. J Bone Joint Surg Br 1991; 73(5): 770-3.
- Torchia M E, Klassen R A, Bianco A J. Total hip arthroplasty with cement in patients less than twenty years old: long-term results. J Bone Joint Surg Am 1996; 78(7): 995-1003.
- Sedrakyan A, Romero L, Graves S, Davidson D, de Steiger R, Lewis P, et al. Survivorship of hip and knee implants in pediatric and young adult populations: analysis of registry and published data. J Bone Joint Surg Am 2014; 96(
Suppl. 1 ): 73-8. - Ruddlesdin C, Ansell B M, Arden G P, Swann M. Total hip replacement in children with juvenile chronic arthritis. J Bone Joint Surg Br 1986; 68(2): 218-22.
- Metcalfe D, Peterson N, Wilkinson J M, Perry D C. Temporal trends and survivorship of total hip arthroplasty in very young patients: a study using the National Joint Registry data set. Bone Joint J 2018; 100-B(10): 1320-9.
- Kamath A F, Sheth N P, Hosalkar H H, Babatunde O M, Lee G C, Nelson C L. Modern total hip arthroplasty in patients younger than 21 years. J Arthroplasty 2012; 27(3): 402-8.
- Tsukanaka M, Halvorsen V, Nordsletten L, Engesaeter I O, Engesaeter L B, Fenstad A M, et al. Implant survival and radiographic outcome of total hip replacement in patients less than 20 years old. Acta Orthop 2016; 87(5): 479-84.
- Halvorsen V, Fenstad A M, Engesæter L B, Nordsletten L, Overgaard S, Pedersen A B, et al. Outcome of 881 total hip arthroplasties in 747 patients 21 years or younger: data from the Nordic Arthroplasty Register Association (NARA) 1995–2016. Acta Orthop 2019; 90(4): 331-7.
- Hannouche D, Devriese F, Delambre J, Zadegan F, Tourabaly I, Sedel L, et al. Ceramic-on-ceramic THA implants in patients younger than 20 years. Clin Orthop Relat Res 2016; 474(2): 520-7.
- Finkbone P R, Severson E P, Cabanela M E, Trousdale R T. Ceramic-on-ceramic total hip arthroplasty in patients younger than 20 years. J Arthroplasty 2012; 27(2): 213-19.
- D’Ambrosi R, Marciandi L, Frediani P V, Facchini R M. Uncemented total hip arthroplasty in patients younger than 20 years. J Orthop Sci 2016; 21(4): 500-6.
- Clohisy J C, Oryhon J M, Seyler T M, Wells C W, Liu S S, Callaghan J J, et al. Function and fixation of total hip arthroplasty in patients 25 years of age or younger. Clin Orthop Relat Res 2010; 468(12): 3207-13.
- Restrepo C, Lettich T, Roberts N, Parvizi J, Hozack W J. Uncemented total hip arthroplasty in patients less than twenty-years. Acta Orthop Belg 2008; 74(5): 615-22.
- Ledford C K, Vap A R, Bolognesi M P, Wellman S S. Total hip arthroplasty in very young bone marrow transplant patients. J Surg Orthop Adv 2015; 24(2): 99-104.
- Schreurs B W, Slooff T J J H, Gardeniers J W M, Buma P. Acetabular reconstruction with bone impaction grafting and a cemented cup: 20 years’ experience. Clin Orthop Relat Res 2001; (393): 202-15.
- DeLee J G, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res 1976; (121): 20-32.
- Gruen T A, McNeice G M, Amstutz H C. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res 1979; (141): 17-27.
- Harris W H, McCarthy J C J, O’Neill D A. Femoral component loosening using contemporary techniques of femoral cement fixation. J Bone Joint Surg Am 1982; 64(7): 1063-7.
- Brooker A F, Bowerman J W, Robinson R A, Riley L H J. Ectopic ossification following total hip replacement: incidence and a method of classification. J Bone Joint Surg Am 1973; 55(8): 1629-32.
- Learmonth I D, Heywood A W, Kaye J, Dall D. Radiological loosening after cemented hip replacement for juvenile chronic arthritis. J Bone Joint Surg Br 1989; 71(2): 209-12.
- Bryant D, Havey T C, Roberts R, Guyatt G. How many patients? how many limbs? Analysis of patients or limbs in the orthopaedic literature: a systematic review. J Bone Joint Surg Am 2006; 88(1): 41-5.