Influence of implant variations on survival of the Lubinus SP II stem: evaluation of 76,530 hips in the Swedish Arthroplasty Register, 2000–2018
Raed ITAYEM 1-3, Ola ROLFSON 1-3, Maziar MOHADDES 1-3, and Johan KÄRRHOLM 1-3
1 Department of Orthopaedics, Institute of Clinical Science, Sahlgrenska Academy, University of Gothenburg Gothenburg; 2 The Swedish Arthroplasty Register, Gothenburg; 3 Department of Orthopaedics, Sahlgrenska University Hospital, Region Västra Götaland, Gothenburg, Sweden
Background and purpose — Almost all prosthetic implant brands include several variations. Most studies on implant performance investigate an implant system without sub-analysis of implant attributes. We studied the influence of design variations during the last 2 decades on implant survival of the most frequently used cemented femoral stem, the Lubinus SPII, reported to the Swedish Arthroplasty Register (SHAR).
Patients and methods — Between 2000 and 2018, 100,032 cemented Lubinus SP II stems had been reported to SHAR. Patients with primary osteoarthritis operated on with stem length 150 mm together with a cemented cup from the same manufacturer (n = 76,530) were included in this analysis. Primary study outcome was non-infectious stem revision. Cox regression with adjustment for age, sex, surgical approach, and year of surgery was used. Hazard rates (HR) are presented with 95% confidence intervals (CI).
Results — Average follow-up was 7.6 years (SD 4.2). At 18 years the overall stem survival was 99.1 (CI 98.9–99.3). Increased revision rate was observed for stems with extra offset, when a long or an extra-long head length had been used. Smaller stem sizes, in particular the smallest stem size (01), substantially increased the rate of mechanical failure as reflected by an almost 10 times increased rate of revision compared with the standard size (2).
Interpretation — In this study with larger sample size and longer follow-up than previously presented from the same register, we observed more pronounced effects of previously documented design variations. Based on our results, surgeons using the Lubinus SPII stems are advised to consider an alternative solution if a Lubinus stem size 01, Lubinus extra offset, or an extra-long head seems to be the most suitable choice at the preoperative planning.
Citation: Acta Orthopaedica 2022; 93: 37–42. DOI http://dx.doi.org/10.1080/17453674.2021.1984669.
Copyright: © 2021 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2021-03-15. Accepted: 2021-08-31. Published: 2022-01-03.
Correspondence: raed.itayem@vgregion.se
All authors contributed to the study design, interpretation of data and results, and the content of the final manuscript. JK, OR, and MM contributed to the conception of the study and to the ethical review application. JK performed the statistical analyses. RI drafted the manuscript.
Acta thanks Ove Furnes and Wierd P Zijlstra for help with peer review of this study.
In Sweden, cemented fixation in total hip replacement (THR) is still dominant despite a decrease since 2006, mainly in favor of all-uncemented fixation (Kärrholm et al. 2019). The most used stem in Sweden is the cemented Lubinus SPII stem. This stem is frequently combined with the cemented Lubinus eccentric cup (Waldemar Link, Hamburg, Germany). In 2018, the SPII stem was used in 34% of all primary THRs (Kärrholm et al. 2018). The stem is made of cobalt-chromium alloy. It has a matte surface, anatomic shape, and is double curved with anterior and posterior ridges.
Some previous studies have focused on how variations in stem design may influence implant survival (Olofsson et al. 2006, Thien and Kärrholm 2010, Kadar et al. 2011a). These studies show that variations in stem size and the features of the modular implant when finally assembled during the operation can also influence the risk of failure. Thien and Kärrholm (2010) studied design-related risk factors for revision of 3 primary cemented stems (the Lubinus SP II, the Exeter, and the Spectron EF) implanted between 1999 and 2006. The follow-up included 43,036 Lubinus SP II stems that received 28 mm heads with an average follow-up of 3.3 years. Revisions were few and mainly caused by dislocation, aseptic loosening, or fracture. Nonetheless, higher risk for revision was observed for the smallest stem size, compared with all other sizes. Higher risk of revision was also found with increased offset and the use of a long neck. The use of ceramic heads was advantageous and associated with reduced risk of revision, reaching almost 50% when compared with cobalt-chromium heads.
Since then, distribution between sexes, choice of modular components, and cup material have undergone varying degrees of changes, which could motivate an updated analysis of the potential influence of implant characteristics. Furthermore, the increasing use of uncemented fixation in Sweden could imply that any changes in indications for use of an all-cemented THR has altered the influence of modularity and choice of stem size. We investigated whether the findings by Thien and Kärrholm (2010) as regards the Lubinus SPII stem are sustained or alter when a larger cohort with longer follow-up is studied.
Patients and methods
Study population
Data collection included all the 100,032 Lubinus SPII stems implanted in THRs in Sweden between 2000 and 2018 reported to the SHAR during that period.
Only hips operated on due to primary osteoarthritis and stems inserted together with a cemented Lubinus cup were included to obtain as homogeneous a study group as possible. Only a posterior surgical approach (68%) or the direct lateral approach (32%) were included. Stem length other than 150 mm and head sizes other than 28, 32, or 36 mm were excluded. Bilaterally operated hips were included.
76,530 implants matched our selection criteria (Figure 1). The largest 3 stem sizes were clustered into 1 group to obtain homogeneous comparable group sizes for statistical analysis.

Figure 1. Flowchart for stem selection.
Design attributes
The design attributes investigated were stem size, caput-collum-diaphyseal (CCD) angle (i.e., neck angle), offset, head length, head size, head material, and cup material.
Confounders
Age, sex, year of surgery, and surgical approach were used as confounders as these variables have previously been demonstrated to influence implant survival (Hailer et al. 2012, Skoogh et al. 2019).
Outcome
The outcome of interest was 1st-time stem revision defined as the removal or exchange of the stem for all non-infectious reasons listed in Table 1. Patients were followed until death, emigration, any type of revision, or at the end of the study on December 31, 2018, whichever came first.
Statistics
We used IBM SPSS version 25 (IBM Corp, Armonk, NY, USA). Design-specific characteristics were analyzed using Cox regression analysis with adjustment for age, sex, and incision. Survival curves, log minus log plots, and Schoenfeld residuals were calculated. The residuals were tested (global test: p = 0.5, test of individual covariates: p = 0.05–0.9), plotted and graphically inspected in order ensure that model assumptions were met. We performed 2 additional sensitivity analyses. In the 1st analysis we included only the first operated hip (n = 65,225). In this analysis the hazard rates changed marginally (0.2 or less) without any change in the results according to previous findings (Robertsson and Ranstam 2003, Lie et al. 2004). In the 2nd analysis we stratified data into 2 periods, 2000–2008 and 2009–2018 and included both hips.
We computed life tables to study the probability rate of non-infectious stem revision. Hazard rates (HR) are presented with 95% confidence intervals (CI). All design parameters were classified using the group with highest number of observations as reference.
Ethics, funding, data sharing, and potential conflicts of interests
This study was approved by the Regional Ethical Review Board in Gothenburg, entry number 804-17. All patients included in the registry are informed prior to operation that reported data will be used for research purposes and the patients are able to withdraw their consent at any time.
Funding was received from the Swedish State under the agreement between the Swedish government and the county councils, the ALF agreement (721791). No other funding was provided for this study. The authors report institutional support provided by LINK for other studies performed at Sahlgrenska University Hospital.
Aggregated data are presented in the manuscript; individual data cannot be shared.
Our institution has received funds from Link, Germany for other purposes not related to this study. The authors declare no conflicts of interest.
Results
Mean and median follow-up were 7.6 (SD 4.2) and 7.4 years (0–19).
Descriptive data
76,530 operations were performed on 65,225 patients (58% females). 17% of the males and 18% of the females had bilateral Lubinus SPII prostheses (Table 2). Analyses were based on number of hips and not on number of patients. The cohort was divided into 5 age groups, of which the age group 65–74 years was the largest, including 44% of all hips.
| Factor | Hips included | Revised |
| Sex | ||
| Male | 31,839 (42) | 158 (0.5) |
| Female | 44,691 (58) | 87 (0.2) |
| Age group | ||
| < 55 | 1,413 (1.8) | 20 (1.4) |
| 55–64 | 12,964 (17) | 92 (0.7) |
| 65–74 | 33,100 (43) | 85 (0.3) |
| 75–84 | 25,522 (33) | 46 (0.2) |
| ≥ 85 | 3,531 (4.6) | 2 (0.1) |
| Incision | ||
| Direct lateral | 24,431 (32) | 61 (0.2) |
| Posterior | 52,099 (68) | 184 (0.4) |
| Stem size | ||
| 01 | 7,172 (9.4) | 101 (1.4) |
| 1 | 18,891 (25) | 53 (0.3) |
| 2 | 24,628 (32) | 49 (0.2) |
| 3 | 16,659 (22) | 26 (0.2) |
| 4–6 | 9,180 (12) | 16 (0.2) |
| Stem CCD angle | ||
| 117° | 10,664 (14) | 19 (0.2) |
| 126° | 62,663 (82) | 209 (0.3) |
| 135° | 3,203 (4.2) | 17 (0.5) |
| Stem offset | ||
| Standard | 70,976 (93) | 223 (0.3) |
| Extra offset | 5,554 (7.3) | 22 (0.4) |
| Femoral head size, mm | ||
| 28 | 46,494 (61) | 223 (0.5) |
| 32 | 28,892 (38) | 19 (0.1) |
| 36 | 1,144 (1.5) | 3 (0.3) |
| Femoral head length | ||
| Short | 20,056 (26) | 77 (0.4) |
| Medium | 37,719 (49) | 92 (0.2) |
| Long | 17,872 (23) | 67 (0.4) |
| Extra long | 883 (1.2) | 9 (1.0) |
| Femoral head material | ||
| CoCr | 62,181 (81) | 209 (0.3) |
| Ceramic | 14,349 (19) | 36 (0.3) |
| Cup material | ||
| Older standard a | 56,014 (73) | 238 (0.42) |
| Highly crosslinked b | 20,516 (27) | 7 (0.03) |
| a Gamma irradiated 2.5–4 MRad. b Gamma irradiated 7.5 (SD 1) MRad. |
||
Stem sizes were divided into 5 groups (Figure 2), where size 2 was most frequent (32%). 126° was the most frequently used CCD (82%). The use of 117° increased through the study period (14% for the entire period) while the opposite applied to 135° (4%) (Figure 3). This shift did not result in a negative impact on implant survival in the current analysis.
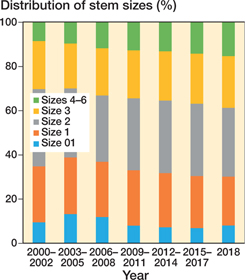
Figure 2. Distribution of stem sizes.

Figure 3. Distribution of usage of CCD angle
An increase in the use of extra-offset stems (10.5 mm longer neck than the standard version) was observed during the study period and reached 13% in 2018 (7% for the entire period).
Medium long (0 mm) was the most common (49%) and extra-long the least common (+10.5 mm for 28 mm head Ø, +8.5 mm for 32 mm head, and + 8 mm for 36 mm head) (1.2%) head length used. No clear change of trend in the use of head length was observed through the progress of the study period.
A shift in using head sizes was observed with the progress in time. 61% of the 28 mm heads were used in the earlier period of the study. By the end of the study period, the 28 mm heads accounted for approximately 2% of all heads used in this cohort.
32 mm head size was the most commonly used head size throughout the study (38%) and dominated the later portion of the study period. In 2011, the first 36 mm heads were used. 36 mm head size was used in only 1.5% of the cases and in about 100 to 200 operations per year from 2011.
Lubinus eccentric cups made of highly cross-linked polyethylene were introduced in Sweden in 2010. Their use increased during the following years to reach 84% in 2018.
Stem survival and risk factors for revision
The overall stem survival at 18 years was 99.0 (CI 98.8–99.2). The most common reason for stem revision was aseptic loosening (79% of all non-septic stem revisions, Table 1). Males had a higher risk of revision when compared with females (adjusted HR = 4.3). Age below the reference group also implied increased hazard rate (adjusted HR, age < 55 and 55–64 = 2.5 and 1.8 respectively; Table 3).
| Factor | Unadjusted HR (95% CI) | Adjusted HR (95% CI) |
| Sex | ||
| Male | 2.6 (2.0–3.4) | 4.3 (3.2–5.7) |
| Female (ref.) | 1 | 1 |
| Age group | ||
| < 55 | 3.5 (2.2–5.8) | 2.5 (1.5–4.1) |
| 55–64 | 2.1 (1.6–2.9) | 1.8 (1.3–2.4) |
| 65–74 (ref.) | 1 | 1 |
| 75–84 | 0.8 (0.6–1.2) | 1.0 (0.7–1.4) |
| ≥ 85 | 0.4 (0.1–1.6) | 0.5 (0.1–2.1) |
| Incision | ||
| Direct lateral | 0.8 (0.6–1.1) | 0.9 (0.7–1.2) |
| Posterior (ref.) | 1 | 1 |
| Stem size | ||
| 01 | 6.0 (4.3–8.5) | 9.7 (6.8 -14) |
| 1 | 1.3 (0.9–2.0) | 1.7 (1.1–2.5) |
| 2 (ref.) | 1 | 1 |
| 3 | 0.8 (0.5–1.3) | 0.7 (0.5–1.2) |
| 4–6 | 1.1 (0.6–1.9) | 0.8 (0.5–1.5) |
| Stem CCD angle | ||
| 117° | 1.1 (0.7–1.7) | 0.7 (0.5–1.2) |
| 126° (ref.) | 1 | 1 |
| 135° | 1.0 (0.6–1.6) | 0.9 (0.6–1.5) |
| Stem offset | ||
| Standard (ref.) | 1 | 1 |
| Extra offset | 1.7 (1.1–2.7) | 2.0 (1.2–3.1) |
| Femoral head size, mm | ||
| 28 (ref.) | 1 | 1 |
| 32 | 0.5 (0.3–0.8) | 0.8 (0.5–1.3) |
| 36 | 2.1 (0.7–6.5) | 4.4 (0.9–22) |
| Femoral head length | ||
| Short | 1.4 (1.0–1.9) | 1.2 (0.9–1.7) |
| Medium (ref.) | 1 | 1 |
| Long | 1.6 (1.2–2.2) | 1.6 (1.2–2.2) |
| Extra long | 4.2 (2.1–8.4) | 3.2 (1.6–6.4) |
| Femoral head material | ||
| CoCr (ref.) | 1 | 1 |
| Ceramic | 0.8 (0.6–1.2) | 0.7 (0.5–1.0) |
| Cup material | ||
| Older standard a (ref.) | 1 | 1 |
| Highly crosslinked b | 0.4 (0.2–0.9) | 0.4 (0.1–1.2) |
| a,b See Table 2 | ||
CCD angles used did not statistically significantly alter the survival probabilities for the Lubinus stem. Stems with extra offset had an increased hazard rate as had stems below size 2, with the highest rate for the smallest size. Stem size 01 had an almost 10 times increased rate relative to the reference stem size 2 (Table 3). The survival probabilities for the different stem sizes are illustrated in Figure 4. A higher rate was also found when long and extra-long head lengths were used (HR = 1.6 and 4.2 respectively; Table 3).

Figure 4. Survival probabilities.
In the stratified analysis we observed a higher stem survival during the later period (2009–2018, log-rank test: p < 0.001). Separate analyses of the influence of design variations showed rather similar results between the 2 periods with 1 exception. Use of a stem with extra offset increased the adjusted rate of non-infectious revision for stems operated on during the first but not during the second period (HR 1st period: 2.4 (CI 1.4– 3.9); 2nd period: 1.0 (CI 0.3–3.5). Cups made of highly cross-linked polyethylene were used only during the later period. During this period use of these cups seemed to be protective, and statistically significantly so in the adjusted analysis (unadjusted HR 0.6 (Cl 0.3–1.5); adjusted HR 0.3 (CI 0.1–0.9).
Discussion
We studied design the influence of design variations of the Lubinus SPII stem on implant survival. The Lubinus SPII stem is the most frequently used cemented stem in Sweden.
In 2018 its share regardless of fixation was 34%, followed by Corail (26%) and Exeter (18%), and the Lubinus SPII accounted for 58% of all cemented stem fixations (Kärrholm et al. 2018). During the period for our study (2000–2018) the SPII cemented stem constituted 40%. This decline over almost 2 decades is caused by an increasing use of uncemented fixation and the introduction of the cemented and polished MS30 stem.
During the observation period, the Lubinus SPII did not undergo any modifications. It was used for a wide spectrum of patients and numerous orthopedic surgeons with varying experience were involved in these operations. We did try to reduce this variability by exclusion of other diagnoses than primary osteoarthritis and focused on only the most commonly used stem length. The overall high survival rate of the Lubinus SPII stem in our follow-up is in line with published studies (Espehaug et al. 2009, Prins et al. 2014, Junnila et al. 2016).
According to the confidence limits observed in our study the true hazard rates with use of CCD angle 117 or 135 degrees could be up to 50% higher or lower than those hazard rates presented. Further, the number of observations of the 135 stems was comparatively small, with decreasing use over time, which means that these results should be viewed with some caution. We could confirm a negative influence of increased offset and neck length on stem survival as previously reported for the SPII stem by Thien and Kärrholm (2010). Similar findings were reported for the Spectron stems (Johanson et al. 2016). In the stratified analysis the negative effect of increased offset was observed only for hips operated during the 1st period. The reason for this difference is not known, but it could be associated with a longer follow-up of these cases, as increasing revision rate in the group of hips with extra offset did not occur until 5–6 years after the index operation, when compared with standard offset. Furthermore, an even more pronounced negative effect was observed with use of the smallest stem size. In addition, we observed a small but statistically significantly increased rate of stem revision due to non-infectious reasons with the use of size 1. These observations are probably due to longer follow-up time and a larger cohort being studied. Our results are consistent with the findings of Johanson et al. (2016) who also demonstrated an increased revision rate for the 2 smaller sizes of the cemented Spectron stem.
The reasons behind these findings are not known. We speculate that due to the smaller contact area, the smaller sizes of the SPII stems are more prone to debonding from the cement mantle. This will facilitate abrasive wear and particle release. The stem might subside inside the mantle, and result in a more distal fixation and impaired proximal stem support, facilitating stem fracture. This could explain why as many as 0.9% of the size 01 (smallest size) were revised due to stem fracture and 4.2% due to loosening, whereas these complications occurred in only 0.0–0.02% and 0.6–1.5%, respectively, with use of the other sizes. This problem could be expected to become even more pronounced if a small stem is inserted in a narrow canal of a young person with thick femoral cortex and who is supposedly physically active. Small stem sizes and lateralized necks increased the rate of revision in a study by Hallan et al. (2012). Asayama et al. (2005) suggested as an explanation an increased risk of early loosening when small stem sizes are used combined with high offset, generating greater strain on a smaller surface area.
When the problems associated with the size 01 stem became evident its use decreased from a maximum of about 8% down to 4–5% but did not decrease further. Its use in the youngest group (< 55 years) did, however, decrease from 5.9% to 1.9% between the periods 2000–2009 and 2010–2018 among those patients who were operated on with an SPII stem. Based on our observations we think that alternatives other than a cemented matte stem should be used in active patients with a very narrow femoral canal.
Extra offset is used in cases with a long neck but could also be related to the level of neck resection and thus an effect of suboptimal planning or surgical technique. A low neck resection will probably decrease the resistance to rotatory forces and thereby increase the risk of mechanical loosening. These theories will, however, remain as speculations because studies based on register data may be biased in various ways. In cadaver studies, resection of the femoral neck below midshaft markedly decreased the torsional load-bearing capacity of the proximal femur (Whiteside et al. 1995, 1996).
36 mm heads had a higher rate and use of 32 mm had a lower rate of aseptic stem revision, when compared with the reference size 28 mm, but none of these differences reached statistical significance after adjustment. These findings may be surprising, because larger heads are often used to lower the rate of revision, particularly due to dislocation. It should, however, be emphasized that our outcome is stem revision, whereas dislocation problems are commonly addressed with revision of the cup. Our results should also be interpreted with caution as the number of 36 mm heads used in the study is rather low. Furthermore, 36 mm heads may be used in cases where patient and/or surgical factors played a role in the selection of larger head size. Our results are, nevertheless, in line with data from the Nordic Arthroplasty Register Association (Tsikandylakis et al. 2018, 2020), suggesting that there are no additional benefits in using 36 mm heads when compared with 32 mm heads.
Thien and Kärrholm (2010) observed a reduced rate of revision with the use of a ceramic head. In our evaluation the hazard rate was similar between use of cobalt-chromium and ceramic heads. The reason for this discrepancy is not known, but the introduction of a more wear-resistant polyethylene or increasing use of larger heads could have had some influence. It remains unclear whether ceramic heads in general provide better long-term survival than cobalt-chromium with cemented all-poly sockets (Kadar et al. 2011b, 2012, Si et al. 2015, López-López et al. 2017).
Limitations and strengths
The definition of non-infectious stem revisions as the primary outcome in this register-based study may be considered as a disadvantage and limitation. The reasons behind development of a deep infection are, however, multi-factorial and most probably not or very vaguely related to choice of implant components. Exclusions summarized in Figure 1 and exclusion of stem lengths other than 150 mm may be considered as a limitation. These stems are, however, rarely used in Sweden in primary surgery. Our results cannot be generalized to SPII stem variations other than those included in the study design.
Another limitation is that we have not performed a radio-graphic evaluation. Some unrevised stems might be loose and the decision to revise depends on multiple factors including the symptoms presented by the patient, which may vary depending on choice of stem design. Finally, register studies should be viewed with caution because of other possible residual confounding such as BMI and ASA classification, which were not collected in SHAR before 2015.
The strength of our study is that it is based on data with high validity and high completeness from the Swedish Arthroplasty Register. The sample is probably the biggest so far published, as is the time to follow-up.
Conclusion
Overall, the Lubinus SPII stem is associated with a very low revision rate. Nonetheless, more careful implant selection could probably be applied to reduce the number of revisions due to mechanical problems even further. Based on our results, we would advise surgeons using the Lubinus SPII stems to reflect on alternative solutions if stem size 01, extra offset or extra-long head seems to be the most suitable during preoperative planning.
Asayama I, Chamnongkich S, Simpson K J, Kinsey T L, Mahoney O M. Reconstructed hip joint position and abductor muscle strength after total hip arthroplasty. J Arthroplasty 2005; 20(4): 414-20. doi: 10.1016/j.arth.2004.01.016.
Espehaug B, Furnes O, Engesaeter L B, Havelin L I. 18 years of results with cemented primary hip prostheses in the Norwegian Arthroplasty Register: concerns about some newer implants. Acta Orthop 2009; 80(4): 402-12. doi: 10.3109/17453670903161124.
Hailer N P, Weiss R J, Stark A, Kärrholm J. The risk of revision due to dislocation after total hip arthroplasty depends on surgical approach, femoral head size, sex, and primary diagnosis. An analysis of 78,098 operations in the Swedish Hip Arthroplasty Register. Acta Orthop 2012; 83(5): 442-8. doi: 10.3109/17453674.2012.733919.
Hallan G, Espehaug B, Furnes O, Wangen H, Høl P J, Ellison P, Havelin L I. Is there still a place for the cemented titanium femoral stem? 10,108 cases from the Norwegian Arthroplasty Register. Acta Orthop 2012; 83(1): 1-6. doi: 10.3109/17453674.2011.645194.
Johanson P E, Antonsson M, Shareghi B, Kärrholm J. Early subsidence predicts failure of a cemented femoral stem with minor design changes. Clin Orthop Relat Res 2016; 474(10): 2221-9. doi: 10.1007/s11999-016-4884-2.
Junnila M, Laaksonen I, Eskelinen A, Pulkkinen P, Ivar Havelin L, Furnes O, Marie Fenstad A, Pedersen A B, Overgaard S, Kärrholm J, Garellick G, Malchau H, Mäkelä K T. Implant survival of the most common cemented total hip devices from the Nordic Arthroplasty Register Association database. Acta Orthop 2016; 87(6): 546-53. doi: 10.1080/17453674.2016.1222804.
Kadar T, Hallan G, Aamodt A, Indrekvam K, Badawy M, Havelin L I, Stokke T, Haugan K, Espehaug B, Furnes O. A randomized study on migration of the Spectron EF and the Charnley flanged 40 cemented femoral components using radiostereometric analysis at 2 years. Acta Orthop 2011a; 82(5): 538-44. doi: 10.3109/17453674.2011.618914.
Kadar T, Hallan G, Aamodt A, Indrekvam K, Badawy M, Skredderstuen A, Havelin L I, Stokke T, Haugan K, Espehaug B, Furnes O. Wear and migration of highly cross-linked and conventional cemented polyethylene cups with cobalt chrome or Oxinium femoral heads: a randomized radiostereometric study of 150 patients. J Orthop Res 2011b; 29(8): 1222-9. doi: 10.1002/jor.21389.
Kadar T, Dybvik E, Hallan G, Furnes O, Havelin L I. Head material influences survival of a cemented total hip prosthesis in the Norwegian Arthroplasty Register. Clin Orthop Relat Res 2012; 470(11): 3007-13. doi: 10.1007/s11999-012-2396-2.
Kärrholm J N, Rogemark C, Nauclér E, Vinblad J, Mohaddes M, Rolfson O. Swedish Hip Arthroplasty Register, Annual Report; 2018.
Kärrholm J N, Rogemark C, Nauclér E, Nåtman J, Vinblad J, Mohaddes M, Rolfson O. Swedish Hip Arthroplasty Register, Annual Report; 2019.
Lie S A, Engesaeter L B, Havelin L I, Gjessing H K, Vollset S E. Dependency issues in survival analyses of 55,782 primary hip replacements from 47,355 patients. Stat Med 2004; 23(20): 3227-40. doi: 10.1002/sim.1905.
López-López J A, Humphriss R L, Beswick A D, Thom H H Z, Hunt L P, Burston A, Fawsitt C G, Hollingworth W, Higgins J P T, Welton N J, Blom A W, Marques E M R. Choice of implant combinations in total hip replacement: systematic review and network meta-analysis. BMJ 2017; 359:j4651. doi: 10.1136/bmj.j4651.
Olofsson K, Digas G, Kärrholm J. Influence of design variations on early migration of a cemented stem in THA. Clin Orthop Relat Res 2006; 448:67-72. doi: 10.1097/01.blo.0000224020.73163.28.
Prins W, Meijer R, Kollen B J, Verheyen C C, Ettema H B. Excellent results with the cemented Lubinus SP II 130-mm femoral stem at 10 years of follow-up: 932 hips followed for 5-15 years. Acta Orthop 2014; 85(3): 276-9. doi: 10.3109/17453674.2014.908342.
Robertsson O, Ranstam J. No bias of ignored bilaterality when analysing the revision risk of knee prostheses: analysis of a population based sample of 44,590 patients with 55,298 knee prostheses from the national Swedish Knee Arthroplasty Register. BMC Musculoskelet Disord 2003; 4:1. doi: 10.1186/1471-2474-4-1.
Si H B, Zeng Y, Cao F, Pei F X, Shen B. Is a ceramic-on-ceramic bearing really superior to ceramic-on-polyethylene for primary total hip arthroplasty? A systematic review and meta-analysis of randomised controlled trials. Hip Int 2015; 25(3): 191-8. doi: 10.5301/hipint.5000223.
Skoogh O, Tsikandylakis G, Mohaddes M, Nemes S, Odin D, Grant P, Rolfson O. Contemporary posterior surgical approach in total hip replacement: still more reoperations due to dislocation compared with direct lateral approach? An observational study of the Swedish Hip Arthroplasty Register including 156,979 hips. Acta Orthop 2019; 90(5): 411-6. doi: 10.1080/17453674.2019.1610269.
Thien T M, Kärrholm J. Design-related risk factors for revision of primary cemented stems. Acta Orthop 2010; 81(4): 407-12. doi: 10.3109/17453674.2010.501739.
Tsikandylakis G, Kärrholm J, Hailer N P, Eskelinen A, Mäkelä K T, Hallan G, Furnes O N, Pedersen A B, Overgaard S, Mohaddes M. No increase in survival for 36-mm versus 32-mm femoral heads in metal-on-polyethylene THA: a registry study. Clin Orthop Relat Res 2018; 476(12): 2367-78. doi: 10.1097/corr.0000000000000508.
Tsikandylakis G, Kärrholm J N, Hallan G, Furnes O, Eskelinen A, Mäkelä K, Pedersen A B, Overgaard S, Mohaddes M. Is there a reduction in risk of revision when 36-mm heads instead of 32 mm are used in total hip arthroplasty for patients with proximal femur fractures? Acta Orthop 2020; 91(4): 401-7. doi: 10.1080/17453674.2020.1752559.
Whiteside L A, White S E, McCarthy D S. Effect of neck resection on torsional stability of cementless total hip replacement. Am J Orthop (Belle Mead NJ) 1995; 24(10): 766-70.
Whiteside L A, McCarthy D S, White S E. Rotational stability of noncemented total hip femoral components. Am J Orthop (Belle Mead NJ) 1996; 25(4): 276-80.