Anterior cruciate ligament reconstruction and concomitant procedures in Finland between 2004 and 2018 based on national registers
Anssi ARIMAA1, Tommi SALMINEN1, Jani KNIFSUND1, Ville KYTÖ2-5, Petteri LANKINEN6, and Inari LAAKSONEN1
1Department of Orthopedics and Traumatology, Turku University Hospital and University of Turku, Turku; 2Heart Center, Turku University Hospital and University of Turku, Turku; 3Research Center of Applied and Preventive Cardiovascular Medicine, University of Turku, Turku; 4Center for Population Health Research, Turku University Hospital and University of Turku, Turku; 5Clinical Research Center, Turku University Hospital, Turku; 6Satakunta Central Hospital, Pori, Finland
Background and purpose — We aimed to assess the incidence of anterior cruciate ligament reconstruction (ACLR) and concomitant procedures in Finland.
Patients and methods — We identified all the patients who underwent ACLR between 2004 and 2018 in Finland using national registry data. Patients with an ICD-10 diagnosis code S83.5 and the NOMESCO operation codes NGE30 or NGE35 were included. We recorded the patient’s age, sex, Charlson comorbidity index, and concomitant procedures. NGE30 or NGE35 was defined as the main procedure and all other procedures attached to this procedure were included as concomitant procedures.
Results — Our study included 37,224 ACLRs. The overall incidence of ACLR was 46 (95%CI 34–62) per 105 person-years. This increased from 38 per 105 person-years in 2004 to its peak of 53 in 2014 before decreasing to 47 by 2018. Male patients had a higher overall incidence of ACLR than female patients (61 [CI 47–78] vs. 32 [CI 22–45] per 105 person-years, respectively). However, this difference changed over time: for the males, a decrease in ACLR incidence was observed after 2014, whereas for the females, the trend increased throughout the study period. For both sexes, the highest incidence of ACLRs was in the age group 16–29 years (159 and 71 per 105 person-years, respectively). Concomitant procedures were performed at the time of ACLR in 32% of cases.
Conclusion — While the total incidence of ACLR decreased slightly from 2014 to 2018, it increased among women over the full study period, which might be due to increased female participation in contact sports. Special attention should be given to girls’ and women’s ACL rupture prevention and treatment.
Citation: Acta Orthopaedica 2023; 94: 45–50. DOI https://doi.org/10.2340/17453674.2023.8481.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-06-10. Accepted: 2022-12-13. Published: 2023-02-02.
Correspondence: anssi.arimaa@tyks.fi
AA, JK, PL, VK, and IL designed the work. AA, TS, VK, and IL wrote the manuscript. All the authors analyzed and interpreted the data, edited the manuscript, and approved the final version of the manuscript. All the authors agree to be accountable for all aspects of the work to ensure that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Handling co-editors: Li Felländer-Tsai and Philippe Wagner
Acta thanks Alejandro Marcano and Ville Mattila for help with peer review of this study.
The incidence of anterior cruciate ligament (ACL) rupture is reportedly 78 per 105 person-years and 1 per 10,000 athlete exposures (1,2). Based on current evidence, the first-line treatment of ACL rupture is conservative, and surgical treatment is considered if instability remains after rehabilitation (3). After adequate rehabilitation, approximately half of all patients require later ACL reconstruction (ACLR) (4,5). Nevertheless, surgical treatment is considered the first-line treatment in the presence of concomitant injuries such as dislocated buckethandle meniscal tears needing immediate surgical intervention, or in patients with high functional demands, such as professional athletes.
The incidence of ACLR has been widely reported as varying between 30 and 74 per 105 person-years, but the numbers have been rising (6-12). Women are at a higher risk of both ACL rupture and ACLR; however, the total number appears to be higher among men, likely due to their greater participation in contact sports (11,13,14). The peak age for ACL rupture and ACLR among females is slightly earlier, between 11 and 20 years of age, whereas the incidence of ACLR peaks in males in the third decade of life (1,6). Among Finnish adolescents the incidence of ACLR has been reported to rise with age, being highest at 17 years of age (15).
Concomitant injuries with a traumatic ACL rupture are quite common. The incidence of meniscal tears on magnetic resonance imaging is between 43% and 70%, and bone marrow lesions are even more common (16,17). Based on population data from the USA, as many as 53% of patients undergoing ACLR had a concomitant meniscal procedure (9,12,18). Concomitant collateral ligament or posterior cruciate ligament (PCL) injuries and reconstructions are rare (12). The risk of requiring further surgery following ACLR is also present. While the most common reoperations are meniscal surgeries, the risk of ACLR revision or contralateral ACLR is around 4–5% (19,20). Few population-based studies on the incidence of ACLR and concomitant injuries and procedures have been undertaken during recent years.
We primarily aimed to evaluate the incidence of ACLR in Finland and the association with age and sex on this incidence based on national registry data. Additionally, we determine the concomitant procedures associated with ACLR and the number of patients who underwent more than one ACLR operation during the study period.
Patients and methods
We studied patients with an ACL rupture who underwent ACLR in Finland from 2004 to 2018. All Finnish residents are included in several national databases and identified by a unique and immutable 10-digit national registration number (PIN). This allows the reliable identification of patients from hospital records and administrative databases. To capture new admissions, only those patients treated in surgical units were included in this study.
Patients were identified from the Care Register for Health Care (CRHC) administered by the Finnish Institute for Health and Welfare (THL). The register has high coverage (92%) and accuracy (89%) regarding cruciate ligament rupture (21). All hospitals in Finland are legally obliged to report annually every inpatient treatment period as well as all outpatient contacts with the CRHC (22). Basic baseline data (e.g., age, sex, and specialty of healthcare contact), data on the patient’s length of stay, performed procedures, and International Classification of Diseases 10th version (ICD-10) diagnostic codes are provided for each healthcare contact. Based on this data, all surgical procedures can be identified in the CRHC database. We used the data pertaining to the number of open and arthroscopic ACLRs performed in Finland between January 2004 and December 2018 in this study. The surgical codes applied in our search of the data were NGE35 (arthroscopic ACLR) and NGE30 (open ACLR) based on the NOMESCO Classification of Surgical Procedures version 1.14 by the Nordic Medico-Statistical Committee. The only ICD-10 code included was S83.5 (sprain or strain including [anterior/posterior] cruciate ligament of knee). All other diagnostic codes, including patients with multiligament injury (S83.7, n = 32), were excluded. Only patients who had both surgical code NGE30 or NGE35 and diagnostic code S83.5 were included to exclude patients with surgically treated PCL rupture. All the ACLRs were recorded and linked to the patient’s PIN to assess whether the same patient had undergone more than one operation during the study period. The data does not include nonoperatively treated ACL ruptures. The demographic data of the general population was obtained from Statistics Finland (Helsinki, Finland) (Figure 1).
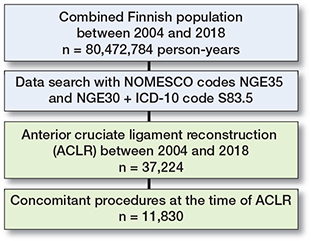
Figure 1. Flowchart of included cases.
In line with previous studies, the Charlson comorbidity index (CCI) score was calculated using a combination of the CRHC, Finnish Cancer registry, and the national registry for special drug reimbursements.
Statistics
The baseline data was analyzed by chi-square test for categorical variables and independent samples t-test for continuous variables. The trends in the dichotomous variables were evaluated via the Cochran–Armitage trend test and the incidence via negative binomial regression (data overdispersion in the Poisson model) with a logarithm of the population at risk as an offset parameter (23). 2-sided tests were used. The standardized incidence was calculated using the European Standard Population 2013. Confidence intervals for incidence were calculated using Poisson distribution. The results are given as the mean, median, percentage, or rate ratio with a 95% confidence interval (CI), interquartile range (IQR), or standard deviation (SD). Incidence is presented as per 105 person-years in the text below. Statistical significance was defined as a p-value < 0.05. The analyses were performed using SAS version 9.4 ( SAS Institute, Inc, Cary, NC, USA ).
Ethics, registration, funding, data sharing, and disclosures
The CRHC registry data, cancer data in the Finnish Cancer Registry, and data in the national registry for special drug imbursements were obtained from the THL and the Finnish Social and Health Data Permit Authority Findata (permission nos. THL/2245/5.05.00/2019 and THL/164/14.02.00/2021). The background population at risk of ACLR consisted of 80,470,000 person-years. Since this was a retrospective registry study, the requirements for ethical board review and informed consent were waived, and the participants were not contacted. The legal basis for processing the personal data was public interest and scientific research (EU General Data Protection Regulation 2016/679, Article 6[1][e] and Article 9[2] [j]; Data Protection Act, Sections 4 and 6).
This study was based on third-party data. Access to the data is strictly regulated by Finnish law and Findata. The disclosure of this data to third parties without explicit permission from Findata is prohibited. Those fulfilling the requirements established for viewing confidential data may request the relevant data from Findata (www.findata.fi). We confirm that the authors did not have any special access privileges that others would not have.
This research received funding from the Turku University Hospital State Research Funding. No conflicts of interest is declared by any of the authors. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.8481
Results
Based on the CHRC database, 37,256 ACLRs were performed in Finland between 2004 and 2018. We excluded 32 patients from the study due to multiligament injury, and the remaining 37,224 ACLRs in 33,887 individual patients (24,135 [65%] male patients) were included in our study. 33,887 (91%) ACLRs were 1st surgeries, 3,001 (8%) were 2nd ACLRs, and 336 (1%) were 3rd to 5th ACLRs, including both revision and contralateral knee ACLRs. The mean age of the patients was 32 years (males 31 years, females 33 years). 90% of the study population did not have any comorbidities (CCI 0), and 9% had 1 comorbidity (CCI 1). Overall, the female patients had slightly more comorbidities than the male patients (Table 1).
| Factor | All n = 37,224 | Males n = 24,135 | Females n =13,089 | p-valuea |
| Age group | < 0.0001 | |||
| 0–15 | 1,237 (3) | 449 (2) | 788 (6) | |
| 16–29 | 16,086 (43) | 11,273 (47) | 4,813 (37) | |
| 30–39 | 10,045 (27) | 7,015 (29) | 3,030 (23) | |
| 40–49 | 7,071 (19) | 4,032 (17) | 3,039 (23) | |
| 50–59 | 2,419 (7) | 1,213 (5) | 1,206 (9) | |
| 60–69 | 350 (1) | 147 (1) | 203 (2) | |
| ≥ 70 | 16(0.04) | 6 (0.02) | 10(0.08) | |
| Mean age (SD) | 32 (11) | 31 (10) | 33 (13) | < 0.0001 |
| Charlson comorbidity index | < 0.0001 | |||
| 0 | 33,345(90) | 21,845 (91) | 11,500 (88) | |
| 1 | 3,337 (9) | 1,997 (8) | 1,340 (10) | |
| 2 | 430 (1) | 239 (1) | 191 (2) | |
| ≥ 3 | 112 (0.3) | 54 (0.2) | 58 (0.4) | |
| a Between sexes | ||||
Total study population
The overall crude incidence of ACLR was 46 (95%CI 34–62) during the study period. This increased from 38 (CI 27–52) in 2004 to its peak of 53 (CI 40–70) in 2014 before decreasing slightly to 47 (CI 34–62) by 2018. When the incidence was adjusted to the European standard population, the overall incidence was 47 (CI 34–62), and 60 (CI 46–78) and 33 (CI 23–47) for the male and female patients, respectively (Figure 2).
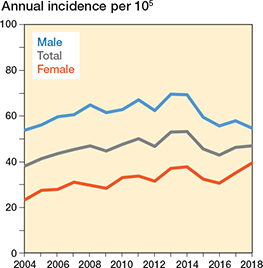
Figure 2. Overall incidence of ACLR per 105 person-years for all patients and by sex.
Sex
The male patients had a higher overall incidence of ACLR than the female patients (61 [CI 47–78] vs. 32 [CI 22–45], respectively). The peak incidence of ACLRs was in 2013 for the male patients (70 [CI 54–88]) and in 2018 for the female patients (39 [CI 28–54]). The increase in ACLR incidence was smaller for the males than the females from 2004 to 2018 at 54 (CI 40–70) to 55 (CI 41–71) and 23 (CI 15–35) to 39 (CI 28 –54), respectively (Table 2, Figure 3).
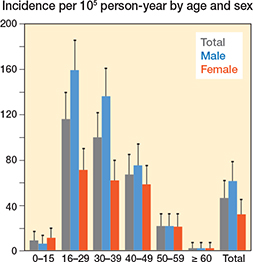
Figure 3. ACLR incidence per 105 person-years by sex and age group with 95%CI levels.
Age
Of all the ACLRs, 43% were performed for patients in the age group 16–29 years (Table 1), and the highest incidence of ACLRs was in the same age group (116 [CI 96–139]) (Table 3, Figure 3). Both the number of ACLRs and the incidence decreased gradually in the older age groups. The highest incidence of ACLRs was in the age group 16–29 years for both males and females (159 [CI 135–186] and 71 [56–90], respectively) (Figure 4). The overall increase in ACLR incidence was most significant in the age group 30–39 years (from 79 [63–99] in 2004 to 106 [87–128] in 2018).
| Age group | Male | Female | Total |
| 0–15 | 6 (2–13) | 11 (6–20) | 9 (4–17) |
| 16–29 | 159 (135–186) | 71 (56–90) | 116 (96–139) |
| 30–39 | 136 (114–161) | 62 (48–79) | 100 (81–122) |
| 40–49 | 75 (59–94) | 58 (44–75) | 67 (52–85) |
| 50–59 | 21 (13–33) | 21 (13–32) | 21 (13–32) |
| ≥ 60 | 2 (0.2–7) | 2 (0.2–7) | 2 (0.2–7 |
| Overall | 61 (47–78) | 32 (22–45) | 46a (34–62) |
| a Standardized incidence is 47 | |||
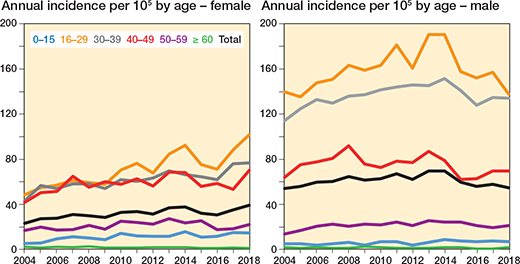
Figure 4. ACLR incidence per 105 person-years during the study period for females and males by age group.
Concomitant procedures
Concomitant procedures were performed at the time of ACLR in 32% of the surgeries (Table 4). Partial meniscal resection was the most common concomitant procedure at 18%, followed by meniscal repair (11%), and chondral microfracturing (1%).
| Meniscal procedures (n = 10,906) | |
| Resection | 6,822 (18) |
| Suture repair | 4,075 (11) |
| Transplantation | 9 (0.02) |
| Collateral repair | 346 (0.9) |
| Chondral procedure | 431 (1.1) |
| Synovial fold resection | 49 (0.1) |
| Osteotomy | 39 (0.1) |
| Patellar procedure | 59 (0.1) |
| Total | 11,830 (32) |
Discussion
The overall incidence of ACLR in Finland was 46 between 2004 and 2018. Our results are in line with earlier international reports. According to registry studies from Sweden and Australia and insurance company data from the USA, the incidence of ACLR was between 30 and 52 from 2004 to 2008 (7-9), which aligns with our result of 46 per 105 person-years.
Previous studies have also reported an increasing trend in ACLR incidence (9,10). During the period of our study, the incidence of ACLR increased between 2004 and 2014 from 38 to 53 before decreasing to 47 in 2018. When the incidence was adjusted to the European standard population to ensure the generalizability of the results, the overall and sex-specific incidences were comparable to those of the Finnish population, which indicates that our results can be extrapolated to other European populations. Mall et al. reported a similar trend in US-based data from the National Discharge Register (9). In their study, the number of procedures increased from 33 in 1994 to 43 in 2006. In comparison, an increase in ACLR incidence from 21 to 34 was reported in the Italian National Discharge registry between 2001 and 2015 (10). Our data range was 2004–2018, which is more recent than the aforementioned studies. The slight decrease in ACLR rates in our study between 2014 and 2018 could be explained by the increasing popularity of non-surgical treatments as a first-line option due to the availability of high-quality research on ACL rupture treatments (24).
In our study, the male patients had an almost 2-fold greater incidence of ACLR than the female patients over the entire study period. However, the difference between the sexes decreased from the start of the study period, with the ACLR incidence among female patients increasing significantly between 2004 and 2018. In contrast, only a small change in the incidence among male patients was noted. Although the overall incidence of ACLR decreased after 2014, the incidence increased slightly between 2014 and 2018 for female patients. The risk of an ACL rupture has been reported as 2–8 times higher for women than for men (13,14). This may be due to anatomical differences as women generally have a higher quadriceps angle, a greater tibial slope, and a smaller intercondylar space (14). However, the overall incidence of ACLR for men in the literature and our study was higher, which could be explained by their greater participation in contact sports, particularly as women are known to have a higher risk of ACL injury than men in the same sports (25-27).
The incidence of ACLR was highest in the age group 16–29 years for both sexes but decreased gradually in the older age groups. The highest incidence was among male patients aged 16–29 years. In other studies, the incidence among males was similar, but for female patients the incidence was greatest for a slightly younger age group (11–20 years) (1,6). Even though the overall ACLR incidence among the females in our study was lower than that of the males, the increase in the former was more apparent, with the incidence in females aged 16–29 years more than doubling during the study period. This may be due to their increased participation in sports that have a high risk of ACL injuries, such as soccer, floorball, and basketball.
ACL rupture is often associated with concomitant injuries in the same knee, which may then need acute surgical care. We found a lower number of concomitant procedures than in the earlier literature (9,12). In Scandinavian ACL registries, meniscectomy was performed in 27–38% of cases and cartilage repair in 6–10% (8). Large registry studies from the USA have reported a higher incidence of concomitant meniscal procedures. In the study by Mall et al., 40% of patients who had an ACLR in 2006 had a concomitant partial meniscectomy (9). Based on data from an insurance company, 50% of the ACLR patients in 2014 received a concomitant meniscal procedure, including both meniscectomies and repairs (12). Further, according to US registry data from 2010 to 2018, 54% of all patients having an ACLR had a concomitant meniscal procedure, of which 73% were meniscectomies and 27% repairs (18). In these studies, concomitant collateral ligament repair was performed in 0.7–1.1% of the ACLRs. When treated non-surgically, concomitant injuries are taken into account in Scandinavian registries (17). Meniscal tears have a reported 43% incidence, with 27% for cartilage damage with an ACL rupture. Our lower number of meniscal procedures (29%) and larger proportion of meniscal repairs (38% of all meniscal procedures) may reflect the more conservative treatment for non-suturable meniscal tears based on data available from high-quality randomized controlled trials (28,29). Concomitant meniscectomy in both primary and revision ACLRs is associated with an increased risk of osteoarthritis. Nonetheless, the differences in the concomitant procedures might be at least partly explained by differences in the registry coverage, as secondary operations might not have been collected as reliably as primary surgical codes.
Strengths and limitations
Our study had several limitations. Our main limitation is that we were unable to evaluate conservatively treated ACL ruptures as our data included only the inpatient data of surgically treated patients. Our registry data therefore did not provide us with the opportunity to evaluate the overall incidence of ACL injuries and the change in the ACLR incidence might also reflect change in the incidence of ACL rupture. Second, as with all registry data, a possibility of bias exists. In registry-based data, there may be some coding errors or missing data. Further-more, a risk of bias is possible in the patient selection as the procedures were performed based on the clinicians’ treatment decisions and not a standardized study protocol. Third, we did not have systematically coded concomitant diagnoses based on MRI findings. Fourth, as is a problem with all retrospective registry data, it may be that not all the concomitant procedures were recorded, and this may have resulted in bias in our data. Additionally, since laterality of procedure is not known, new injury of index knee, revision procedure due to failed graft, or new injury of other knee cannot be distinguished. Notwith-standing, a strength of our study is the use of high-quality data from national registries with excellent coverage, which provided reliable nationwide data regarding the incidence of ACLR. Additionally, our follow-up time was long, and the data was more recent than those in earlier studies.
Conclusion
The total incidence of ACLR decreased slightly from 2014 to 2018 and one-third of the patients had a concomitant procedure. The incidence increased among the female patients in our study over the full study period, which might be due to increased female participation in contact sports. Compared with earlier studies, the lower percentage of meniscal resection and higher percentage of meniscal suturing associated with ACLR may reflect the more conservative treatment of non-suturable meniscal tears based on recent high-quality studies.
- Nordenvall R, Bahmanyar S, Adami J, Stenros C, Wredmark T, Felländer-Tsai L. A population-based nationwide study of cruciate ligament injury in Sweden, 2001-2009: incidence, treatment, and sex differences. Am J Sports Med 2012; 40(8): 1808-13. doi: 10.1177/0363546512449306.
- Parkkari J, Pasanen K, Mattila V M, Kannus P, Rimpelä A. The risk for a cruciate ligament injury of the knee in adolescents and young adults: a population-based cohort study of 46 500 people with a 9 year follow-up. Br J Sports Med 2008; 42(6): 422-6. doi: 10.1136/bjsm.2008.046185.
- Frobell R B, Roos H P, Roos E M, Roemer FW, Ranstam J, Lohmander L S. Treatment for acute anterior cruciate ligament tear: five year outcome of randomised trial. Br J Sports Med 2015; 49(10): 700. doi:10.1136/bjsports-2014-f232rep.
- Frobell R B, Roos E M, Roos H P, Ranstam J, Lohmander L S. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med 2010; 363(4): 331-42. doi: 10.1056/NEJMoa0907797.
- Reijman M, Eggerding V, van Es E, van Arkel E, van den Brand I, van Linge J, et al. Early surgical reconstruction versus rehabilitation with elective delayed reconstruction for patients with anterior cruciate ligament rupture: COMPARE randomised controlled trial. BMJ 2021; 372: n375. doi: 10.1136/bmj.n375.
- Csintalan R P, Inacio M C, Funahashi T T. Incidence rate of anterior cruciate ligament reconstructions. Perm J 2008; 12(3): 17-21. doi: 10.7812/tpp/07-140.
- Janssen K W, Orchard J W, Driscoll T R, van Mechelen W. High incidence and costs for anterior cruciate ligament reconstructions performed in Australia from 2003–2004 to 2007–2008: time for an anterior cruciate ligament register by Scandinavian model? Scand J Med Sci Sports 2012; 22(4): 495-501. doi: 10.1111/j.1600-0838.2010.01253.x.
- Granan L P, Forssblad M, Lind M, Engebretsen L. The Scandinavian ACL registries 2004–2007: baseline epidemiology. Acta Orthop 2009; 80(5): 563-7. doi: 10.3109/17453670903350107.
- Mall N A, Chalmers P N, Moric M, Tanaka M J, Cole B J, Bach B R Jr, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med 2014; 42(10): 2363-70. doi: 10.1177/0363546514542796.
- Longo U G, Nagai K, Salvatore G, Cella E, Candela V, Cappelli F, et al. Epidemiology of anterior cruciate ligament reconstruction surgery in Italy: a 15-year nationwide registry study. J Clin Med 2021; 10(2): 223. doi: 10.3390/jcm10020223.
- Gianotti S M, Marshall S W, Hume P A, Bunt L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: a national population-based study. J Sci Med Sport 2009; 12(6): 622-7. doi: 10.1016/j.jsams.2008.07.005.
- Herzog M M, Marshall S W, Lund J L, Pate V, Mack C D, Spang J T. Trends in incidence of ACL reconstruction and concomitant procedures among commercially insured individuals in the United States, 2002–2014. Sports Health 2018; 10(6): 523-531. doi: 10.1177/1941738118803616.
- Devana S K, Solorzano C, Nwachukwu B, Jones K J. Disparities in ACL reconstruction: the influence of gender and race on incidence, treatment, and outcomes. Curr Rev Musculoskelet Med 2022; 15(1): 1-9. doi: 10.1007/s12178-021-09736-1.
- Sutton K M, Bullock J M. Anterior cruciate ligament rupture: differences between males and females. J Am Acad Orthop Surg 2013; 21(1): 41-50. doi: 10.5435/JAAOS-21-01-41.
- Weitz F K, Sillanpää P J, Mattila V M. The incidence of paediatric ACL injury is increasing in Finland. Knee Surg Sports Traumatol Arthrosc 2020; 28(2): 363-8. doi: 10.1007/s00167-019-05553-9.
- Nicholls M, Ingvarsson T, Briem K. Younger age increases the risk of sustaining multiple concomitant injuries with an ACL rupture. Knee Surg Sports Traumatol Arthrosc 2021; 29(8): 2701-8. doi: 10.1007/s00167-021-06538-3.
- Røtterud J H, Sivertsen E A, Forssblad M, Engebretsen L, Arøen A. Effect of meniscal and focal cartilage lesions on patient-reported outcome after anterior cruciate ligament reconstruction: a nationwide cohort study from Norway and Sweden of 8476 patients with 2-year follow-up. Am J Sports Med 2013; 41(3): 535-43. doi: 10.1177/0363546512473571.
- Partan M J, Iturriaga C R, Cohn R M. Recent trends in concomitant meniscal procedures during anterior cruciate ligament reconstruction. Orthop J Sports Med 2021; 9(2): 2325967120984138. doi: 10.1177/2325967120984138.
- Lord L, Cristiani R, Edman G, Forssblad M, Stålman A. One sixth of primary anterior cruciate ligament reconstructions may undergo reoperation due to complications or new injuries within 2 years. Knee Surg Sports Traumatol Arthrosc 2020; 28(8): 2478-85. doi: 10.1007/s001670-20-06127-w.
- Maletis G B, Inacio M C, Funahashi T T. Risk factors associated with revision and contralateral anterior cruciate ligament reconstructions in the Kaiser Permanente ACLR registry. Am J Sports Med 2015; 43(3): 641-7. doi: 10.1177/0363546514561745.
- Mattila V M, Sillanpää P, Iivonen T, Parkkari J, Kannus P, Pihlajamäki H. Coverage and accuracy of diagnosis of cruciate ligament injury in the Finnish National Hospital Discharge Register. Injury 2008; 39(12): 1373-6 . doi: 10.1016/j.injury.2008.05.007.
- Sund R. Quality of the Finnish Hospital Discharge Register: a systematic review. Scand J Public Health 2012; 40(6): 505-15. doi: 10.1177/1403494812456637.
- Musahl V, Karlsson J. Anterior cruciate ligament tear. N Engl J Med 2019; 380(24): 2341-8. doi: 10.1056/NEJMcp1805931.
- Arendt E, Dick R. Knee injury patterns among men and women in collegiate basketball and soccer: NCAA data and review of literature. Am J Sports Med 1995; 23(6): 694-701. doi: 10.1177/036354659502300611.
- Renstrom P, Ljungqvist A, Arendt E, Beynnon B, Fukubayashi T, Garrett W, et al. Non-contact ACL injuries in female athletes: an International Olympic Committee current concepts statement. Br J Sports Med 2008; 42(6): 394-412. doi: 10.1136/bjsm.2008.048934.
- Montalvo A M, Schneider D K, Yut L, Webster K E, Beynnon B, Kocher M S, et al. “What’s my risk of sustaining an ACL injury while playing sports?” A systematic review with meta-analysis. Br J Sports Med 2019; 53(16): 1003-12. doi: 10.1136/bjsports-2016-096274.
- Sihvonen R, Paavola M, Malmivaara A, Itälä A, Joukainen A, Nurmi H, et al; Finnish Degenerative Meniscal Lesion Study (FIDELITY) Group. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med 2013; 369(26): 2515-24. doi: 10.1056/NEJMoa1305189.
- Kise N J, Risberg MA, Stensrud S, Ranstam J, Engebretsen L, Roos E M. Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: randomised controlled trial with two year follow-up. BMJ 2016; 354: i3740. doi: 10.1136/bmj.i3740.
- Borchers J R, Kaeding C C, Pedroza A D, Huston L J, Spindler K P, Wright R W; MOON Consortium and the MARS Group. Intra-articular findings in primary and revision anterior cruciate ligament reconstruction surgery: a comparison of the MOON and MARS study groups. Am J Sports Med 2011; 39(9): 1889-93. doi: 10.1177/0363546511406871.