Patient–surgeon sex discordance impacts adverse events but does not affect patient-reported satisfaction after primary total hip arthroplasty: a regional register-based cohort study
Per JOLBÄCK 1,2, Sebastian MUKKA 5, Kristin WETTERLING 1, Maizar MOHADDES 1,6,7, and Anne GARLAND 3,4
1 Department of Orthopaedics, Institute of Clinical Science, The Sahlgrenska Academy, University of Gothenburg, Gothenburg; 2 Department of Orthopaedics, Skaraborg Hospital, Skövde; 3 Department of Surgical Sciences/Orthopaedics, Institute of Surgical Sciences, Uppsala University Hospital, Uppsala; 4 Department of Orthopaedics, Visby Hospital, Visby; 5 Department of Surgical and Perioperative Sciences (Orthopedics), Umeå University, Umeå; 6 Swedish Arthroplasty Register, Gothenburg; 7 Department of Orthopaedics, Sahlgrenska University Hospital, Gothenburg, Sweden
Background and purpose — The sex of the surgeon has been proposed to be associated with a disparity in clinical outcomes after different surgical procedures. We investigated the association between surgeon–patient sex discordance and adverse events (AEs) and surgical AEs (SAEs) within 90 days after primary total hip arthroplasty (THA). We also investigated patient-reported satisfaction with surgical outcomes 1 year after the surgery.
Patients and methods — We conducted a register-based cohort study including primary THAs performed due to osteoarthritis between 2008 and 2016 at 10 publicly managed hospitals in western Sweden. Hospital data was linked to the Swedish Arthroplasty Register and a regional patient register. Logistic regression models investigated discordant sex of patients and surgeons on AEs/SAEs and patient-reported satisfaction with the surgical outcome.
Results — 11,993 primary THAs were included in the study. The proportion of AEs for the concordant group was 7.3% and for the discordant group 6.1%. For SAEs, the proportion was 5.0% for the concordant group and 4.3% for the discordant group. After adjustment the discordant group still had a lower likelihood of an AE or SAE than the concordant group: adjusted odds ratio (aOR) for AE (0.82, 95%CI 0.71–0.95) and for SAE (0.86, CI 0.72–0.99). No association was detected between patient-reported satisfaction and sex discordance.
Conclusion — Sex discordance between surgeons and patients is linked to a decreased risk of an AE but not a lower level of patient-reported satisfaction with the surgical outcome.
Citation: Acta Orthopaedica 2022; 93: 906–913. DOI http://dx.doi.org/10.2340/17453674.2022.5761.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-05-16. Accepted: 2022-11-06. Published: 2022-12-27.
Correspondence: perjo2@icloud.com
PJ had the original idea for the study, processed the data and prepared the first version of the manuscript. SM, MM and AG took part in the planning of the study, analysis, interpretation of the data, and in writing of the manuscript. KW took part in interpretation of the data and writing of the manuscript. All authors read and approved the final manuscript.
Handling co-editors: Søren Overgaard and Robin Christensen
Acta thanks Antti Eskelinen and Henrik Husted for help with peer review of this study.
Orthopedics is still a male-dominated specialty, especially in hip arthroplasty. In Sweden, approximately 17% of all orthopedic surgeons are females (1), compared with 5–6% in the UK or USA (1). The sex of the surgeon is associated with a disparity in clinical outcomes (2,3). This disparity has not yet been shown to impact adverse events (AEs) following primary total hip arthroplasty (THA) (4,5). Sex discordance between physicians/surgeons and patients has negatively affected health care, e.g., increased risk of an inaccurate diagnosis, incorrect assessment of symptom severity, and poor clinical outcomes (6). In a recently published study based on 21 common elective and acute surgical procedures, there was an increased risk of AE and mortality when the sex of the surgeon differed from the sex of the patient (7). The poorest outcome occurred when a male surgeon treated a female patient (7). No study has investigated whether sex discordance between surgeons and patients is related to AEs or patient-reported outcomes in a cohort of primary THAs. We hypothesized that sex discordance contributes to poorer surgical outcomes. We conducted a register-based cohort study to investigate whether the sex of the surgeon and the sex of the patient is related to AEs and surgical AEs (SAEs) 90-days after primary THA surgery. We also examined patient satisfaction with the surgical outcome 1-year after primary THA.
Patients and methods
Study design
We conducted a register-based cohort study comprising primary THAs performed due to hip osteoarthritis (OA) as defined by the International Statistical Classification of Diseases and Related Health Problems 10th revision codes (ICD-10, M16.0–M16.7, and M16.9) and the Nordic Medico-Statistical Committee classification (NOMESCO) surgical procedure codes NFB29 (uncemented fixation), NFB39 (hybrid fixation), and NFB49 (cemented fixation). All included surgeries were performed between 2008 and 2016 at 10 publicly managed hospitals in western Sweden.
Hospital data was linked to the Swedish Arthroplasty Register (SAR) and a regional patient administrative register. The linking between hospital records and the SAR was done using the unique 12-digit personal identification number (PIN) issued by the Swedish Tax Agency to all Swedish permanent residents (8), operating unit, and surgery date. The linked dataset was subsequently forwarded to the regional patient register to add all comorbidities and AEs.
Surgeon sex was retrieved from hospital records based on the surgeon’s name and the PIN of each surgeon. The biological sex assigned at birth is represented in the 12-digit PIN (8). For each surgery, the surgeon’s data was retrieved. The primary surgeon (specified in the hospital record) was assigned to the surgery regardless of hierarchical status, i.e., the principal surgeon could be an attending physician or a resident. Approximately 70% of the included THAs were specified with only one surgeon (i.e., no co-surgeon or assistant was listed in the hospital records) and applied to male and female surgeons. Using the PIN, the patient’s sex was retrieved from the SAR.
Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for reporting observational studies were followed (9).
Outcomes
The study outcomes were AE/SAE within 90 days after the index primary THA and patient-reported satisfaction with the surgical outcome 1 year after surgery (hereafter referred to as satisfaction). An AE was defined as readmission for a predefined set of ICD-10 and NOMESCO codes for interventions, or death (10,11). A description of the A, DA, DB/D2, DC, and DM/DM2 categories is given in Table 1. For the outcome AE all categories are included and for the SAE only A, DA, BD, and BD 2 categories are included. All diagnoses to identify AEs were retrieved from the regional administrative patient register and patient satisfaction was recovered from the SARs patient-reported outcomes measures (PROMs) program (11). All publicly managed hospitals in western Sweden have been collecting patient-reported outcomes since the establishment of the PROMs program. The response rate for individual registration at the national level in 2008 was 86% for the preoperative survey and 79% for pooled pre- and 1-year postoperative surveys (12).
| Categories | Description of the AE categories |
| A a | Surgical procedure codes that include reoperations of THA implants and other procedures that may represent a complication |
| DA a | Diagnostic codes that imply surgical complications |
| DB/DB2 a | Diagnostic codes that cover hip-related diseases and that may have been used for complications after THA surgery |
| DC a | Diagnostic codes covering cardiovascular events that may be related to THA surgery |
| DM/DM2 | Diagnostic codes concerning other medical events not related to THA surgery but that may be related to the surgery if they occur shortly afterward |
| a Hip-related complications included in the surgical AE (SAE) | |
During the study period, the PROMs program included the EQ-5D-3L instrument (13), Pain visual analog scale (VAS), Satisfaction VAS, and a question regarding musculoskeletal comorbidity based on the self-administered Charnley classification survey (14). EQ-5D-3L and Pain VAS data was collected before and 1 year after surgery. In 2017, the response scale for the satisfaction VAS was changed from 0 to 100 (0 represents the highest imaginable satisfaction and 100 the worst imaginable satisfaction) to a 5-point Likert scale (very satisfied, satisfied, neither dissatisfied nor satisfied, dissatisfied, and very dissatisfied) in the SAR. All previously collected VAS values were converted to the new scale: very satisfied (0–20), satisfied (21–40), neither dissatisfied nor satisfied (41–60), dissatisfied (61–80), and very dissatisfied (81–100).
Covariates
Based on previous studies, we selected covariates that might affect the outcomes of our study. For the analysis of the AE outcome, the patient’s age (15), the patient’s Elixhauser comorbidity index (ECI) (16), and the annual surgeon volume (17) were included as covariates. The covariates of the patient satisfaction analysis were the patient’s age (15) and the preoperative Charnley classification (18).
The ECI is a comprehensive set of 30 comorbidities associated with a substantial increase in hospital stay, hospital charges, and mortality (19,20). The period used to measure the ECI in this study was 365 days before the index THA. Surgeon annual case volume was defined as the number of primary THAs the main operating surgeons had performed in the 365 days preceding the index THA (17).
Statistics
Descriptive data was presented as mean (SD), numbers, and percentage. Logistic regression was used to investigate the impact of surgeons’ and patients’ sex on AEs/SAEs and patient-reported satisfaction. The 5-point Likert scale was transformed into a binary variable in the logistic regression model: satisfied (very satisfied, satisfied, and neither dissatisfied nor satisfied) and dissatisfied (dissatisfied and very dissatisfied). A sensitivity analysis, including cases performed by attending orthopedic surgeons only, was conducted for AEs, SAEs, and patient-reported satisfaction. Estimates were presented as adjusted odds ratios (aORs) with 95% confidence intervals (CIs). Only the first operation for patients undergoing staged bilateral THAs was included in this analysis (21). Surgeons with an annual case volume of < 5 primary THAs were excluded. Finally, patients with no data on the ECI were assumed to have an ECI equal to 0.
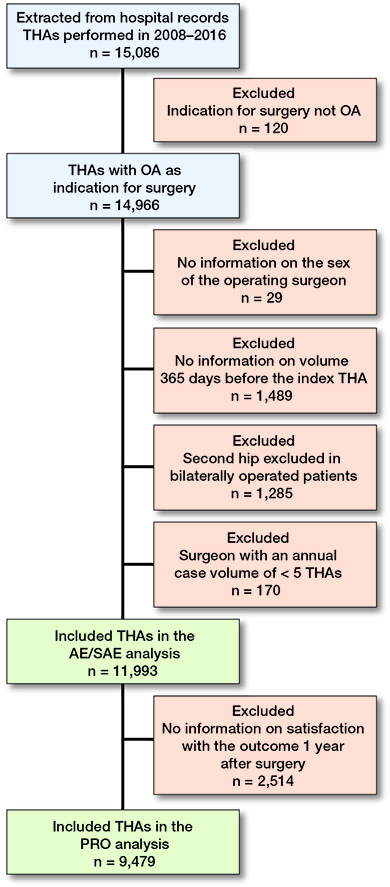
Flowchart of allocation to study groups.
SPSS version 26 (IBM Corp, Armonk, NY, USA) was used for statistical analysis.
Respondents versus non-respondents
To address potential transfer bias due to missing data on PROMs, a respondent versus non-respondent analysis was performed. The analysis evaluated whether non-respondents at 1 year differed from respondents in patient characteristics: age, body mass index (BMI), and the preoperative Charnley classification.
Ethics, funding, data sharing, and disclosures
The study complied with the ethical principles of the Helsinki Declaration and the study was approved by the Swedish Ethical Review Authority (dnr 2022-00358-02). The authors report no conflict of interest.
The dataset analyzed in this study is not publicly available as the study was approved on the grounds of ensuring the confidentiality of data of patients included in the study.
We are positive toward sharing data but are legally restricted from sharing the data publicly according to the law on Public Access and Secrecy, chapter 21, paragraph 7 and chapter 25, paragraph 1 (https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/offentlighets--och-sekretesslag-2009400_sfs-2009-400). Any person interested in the data set may contact Skaraborg Hospital and the corresponding author to find ways to share data according to Swedish laws and regulations.
Results
Characteristics of the study population
Our cohort for the AE/SAE outcome comprised 11,993 patients (57.9% female) operated on by 200 surgeons (82% male). The cohort for the patient satisfaction outcome comprised 9,479 patients (Figure). Of the included cases in the AE/SAE outcome analysis, 5,318 (44.4%) patients were sex concordant with their operating surgeon (male surgeon–male patient or female surgeon–female patient) and 6,675 (55.7%) were discordant (male surgeon–female patient or female surgeon–male patient). A large difference was found in the distribution of the sex of the patients between the concordant and discordant group. In the concordant group most patients were male (86.6%), whereas in the discordant group the dominating sex was female (93.4%). Patients in the sex-discordant group were somewhat older (70 vs. 68 years) and had a higher proportion of Charnley classification group “C” (46.4 vs. 40.6%) compared with the sex-concordant group. Differences in the fixation techniques of implant could also be seen, where the cemented prosthesis was more commonly used in the discordant group (70.2 vs. 65.0%) (Table 2).
Adverse events and surgical adverse events
Overall, 794 (6.6%) patients experienced an AE and 551 (4.6%) an SAE. Categorized into concordant/discordant groups, there was a 16.6% difference in AEs and a 24.0% difference in SAEs. The aOR for AEs was 0.82 (95%CI 0.71–0.95) and for SAEs 0.86 (CI 0.72–0.99), both favoring the discordant group (Table 3). When the sex of the patient is the same as the sex of the surgeon (concordant), there was a 28% difference in AEs (aOR 0.55, CI 0.38–0.78) and a 34% difference in SAEs (aOR 0.56, CI 0.36–0.86). In the 2 groups where the sex of the patient differs from the sex of the surgeon (discordant), the difference was 5% for both AEs (aOR 0.96, CI 0.65–1.44) and SAEs (aOR 0.88, CI 0.54–1.44) (Table 4). The distribution of the AE classification is shown in Table 5 (see Supplementary data).
A sensitivity analysis for AEs, SAEs, and patient-reported satisfaction that only included attending surgeons yielded results comparable to the analysis that included attending surgeons and residents (Table 4). Two additional sensitivity analyses were performed: one in which the patient group was restricted to ICD-10 codes M16.0/M16.1 (bilateral/unilateral primary OA of the hip) as the indication for surgery, and one with adjustment for the number of years between the operating surgeon’s specialist certification and time of the index THA together with patient age, patient ECI, and annual surgeon case volume adjusted for in the primary analysis. Adding an extra variable did not improve the primary adjusted logistic regression model fit. The additional analyses yielded results equivalent to the primary analysis (Table 6, see Supplementary data).
Patient-reported outcomes
611 (6.4%) patients reported being dissatisfied or very dissatisfied with the surgical outcome. Female patients reported being more frequently dissatisfied or very dissatisfied than male patients (5.6 male vs. 7.1% female). A higher frequency of dissatisfied/very dissatisfied was reported in both groups of female patients (Table 3). The regression analysis showed no difference in patient-reported satisfaction between the concordant and discordant groups (aOR 0.89, CI 0.74–1.07) (Table 4). Sub-group analyses showed no significant differences among any of the groups.
Respondents versus non-respondents
Approximately 21% of the surgeries had missing satisfaction PROs at 1 year follow-up. There were similar distributions of respondents/non-respondents between the concordant and discordant groups in the 1-year follow-up survey (Table 7, see Supplementary data).
In the 1-year follow-up there was a disparity in mean age, mean BMI, and preoperative Charnley classification. More specifically, non-respondents were younger, slightly more obese, and had a lower proportion of Charnley classification group A (Table 7, see Supplementary data).
Discussion
This study investigated the association between surgeon and patient sex discordance and AEs/SAEs within 90 days after primary THA and patient-reported satisfaction with postoperative results 1 year after primary THA. Our findings show that sex discordance between the operating surgeon and patient is related to a decreased risk of AEs/SAEs but does not affect patient-reported satisfaction. A sub-group analysis showed that male patients operated on by male surgeons had an increased likelihood of AEs and SAEs. This finding contrasts with a previous study showing a composite patient cohort from 21 common elective or acute surgical procedures (7). Wallis et al. (7) found that when the sex of the surgeon and the patient differed, the outcomes were affected negatively, and that female patients operated on by male surgeons had the highest likelihood of a worse outcome. A plausible explanation for the disparity between the studies might be that our study is based on a more uniform cohort of patients sharing the same risk profile for complications.
We elected to present the results for both AEs and SAEs in our analysis. The AEs also include medical complications and might therefore be more related to the “surgery in general” rather than to the operating surgeon’s performance in the operating theater. SAEs might be more directly related to the surgeon’s knowledge, training, and experience in performing surgery and intraoperative decisions.
Our findings raise several questions. Are Swedish male surgeons different from Swedish female surgeons? Are Swedish male patients different from Swedish female patients when it comes to preparation before and rehabilitation after surgery? Is there a disparity in indication for surgery between male and female patients in Sweden? Are Swedish male surgeons willing to take higher risks and thus more likely to be an outlier with poor performance (22)? Do Swedish male surgeons have a higher level of self-confidence than Swedish female surgeons (i.e., do women have a higher risk aversion than men)? Is there a disparity in conscientiousness and the willingness to ask for help or/and handle everything yourself between male and female surgeons?
In the economic field several studies indicate that men are more willing to take risks and have a higher level of self-confidence than women (23,24). We can only speculate whether these attributes also apply to the medical field (i.e., THA surgery). A potential higher risk aversion profile of women (surgeon or patient) could protect them from AEs or negative outcomes. The concordant sub-group of female surgeons–female patients had the lowest frequency of AEs followed by the discordant sub-groups in which females are either surgeons or patients. The highest frequency of AEs was found in the male concordant subgroup. Could the interaction between 2 females (surgeon and patient), i.e., a potential risk aversion, contribute to the lowest frequency of AEs in the subgroup containing 2 females?
A disparity between men and women in compliance with recommendations in the preoperative supported OA self-management program given within a physiotherapy context is known (25). There is also a disparity in completing the program (25). The discrepancy in compliance with recommendations shown preoperatively between men and women might also be seen after surgery and contribute to the differences in AEs/SAEs.
In Sweden’s public healthcare system, the ability of each patient to choose a surgeon is limited. In most cases an administrative coordinator selects the surgeon for the operating hospital rather than the patient. This process might be based on random selection depending on the hospital or the surgeon who assessed the patient for THA. This assessment might be a random selection procedure involving scheduling for surgeon availability. Sometimes this selection might be based on the referral’s description to the orthopedic department (i.e., patients at higher risk of technically complex surgery might be assessed by a more experienced surgeon). Previous studies exploring the patient’s preoperative functional status as an indication for surgery show that the functional status seems to be similar between male and female patients (26). Hence, the eventuality of a patient exploring orthopedic departments to avoid specific surgeons or has major variation in preoperative functional status is low and therefore not introducing a selection bias in the study.
We share the same limitations as all studies based on administratively collected data, i.e., the risk of bias because of temporal trends and changes in practice. The ICD-10 codes from the regional patient register in this study were not separately validated. Nevertheless, the register provides data for the Swedish National Inpatient Register, which is part of the National Patient Register administered by the Swedish National Board of Health and Welfare. The Swedish National Inpatient Register has been validated and contains 99% of all hospital discharges (27). Although Sweden is one of the countries with the highest number of female orthopedic surgeons, the uneven distribution of male and female surgeons and the differences in surgical experience increase the risk of bias in the selection of patients. Or patients operated on by female and male surgeons may not be comparable due to residual confounding.
All this suggests that our findings should be interpreted with some caution. Another potential limitation is the lack of information on other health professionals (nurses, other physicians, physio- and occupational therapists, etc.) involved in the care before and after surgery. The variables used for adjustment in the regression analysis are based on previous studies. However, both patient smoking and drinking have been showed to influence AEs negatively but these factors are not included in the analysis. The authors noted a disparity in missing data for smoking in the database with the lowest percentage of smokers in the years with the highest percentage of missing values, which might highlight a collection bias and hence we decided not to include smoking as a covariate. Data on drinking habits is not collected in any of the data sources used.
Strengths in the present study are the 2 additional analyses: one where only bilateral/unilateral primary hip OA was included and one that was adjusted for an additional parameter on surgeon experience. Additionally, the limited ability of patients to select the operating surgeon increases the generalization of our results (i.e., all surgeons are included in the study, not only surgeons with arthroplasty as a sub-specialty). Furthermore, use of the administrative database for western Sweden (registering all healthcare events, including hospital readmissions) increased the chance of collecting virtually all readmissions within 90 days after the index THA. A further strength concerns employing a well-established PROM program from the SAR.
Conclusion
A difference in the sex between surgeon and patient is associated with a decreased risk of an AE but not with a lower level of self-reported patient-reported satisfaction with the surgical outcome after primary THA. There are some indications that the female sex of the surgeons or patients might be associated with a lower risk of AE. Further research is needed to investigate the underlying mechanisms of the present findings.
- International Orthopaedic Diversity Alliance. Diversity in orthopaedics and traumatology: a global perspective. EFORT Open Rev 2020; 5: 743-52.
- Tsugawa, Y, Jena A B, Figueroa J F, Orav E J, Blumenthal D M, Jha A K. Comparison of hospital mortality and readmission rates for Medicare patients treated by male vs female physicians. JAMA Intern Med 2017; 177(2): 206-13.
- Wallis C J D, Ravi B, Coburn N, Nam R K, Detsky A S, Satkunasivam R. Comparison of postoperative outcomes among patients treated by male and female surgeons: a population based matched cohort study. BMJ 2017; 359: j4366.
- Jolbäck P, Rogmark C, Bedeschi Rego De Mattos C, Chen AF, Nauclér E, Tsikandylakis G. The influence of surgeon sex on adverse events following primary total hip arthroplasty: a register-based study of 11,993 procedures and 200 surgeons in Swedish public hospitals. J Bone Joint Surg Am 2022; 104(15): 1327-33.
- Chapman T R, Zmistowski B, Votta K, Abdeen A, Purtill J J, Chen A F. Patient complications after total joint arthroplasty: does surgeon gender matter. J Am Acad Orthop Surg 2020; 28(22): 937-44.
- Greenwood B N, Carnahan S, Huang L. Patient–physician gender concordance and increased mortality among female heart attack patients. Proc Natl Acad Sci U S A 2018; 15(34): 8569-74.
- Wallis C J D, Jerath A, Coburn N, Klaassen Z, Luckenbaugh A N, Magee D E, et al. Association of surgeon–patient sex concordance with postoperative outcomes. JAMA Surg 2021: e216339.
- Ludvigsson J F, Otterblad-Olausson P, Pettersson B U, Ekbom A. The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol 2009; 24(11): 659-67.
- von Elm E, Altman D G, Egger M, Pocock S J, Gøtzsche P C, Vandenbroucke J P; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg 2014; 12(12): 1495-9.
- Berg U, Bülow E, Sundberg M, Rolfson O. No increase in readmissions or adverse events after implementation of fast-track program in total hip and knee replacement at 8 Swedish hospitals: an observational before-and-after study of 14,148 total joint replacements 2011–2015. Acta Orthop 2018; 89(5): 522-7.
- Jolbäck P, Rolfson O, Cnudde P, Oldin D, Malchau H, Lindahl H, et al. High annual surgeon volume reduces the risk of adverse events following primary total hip arthroplasty: a registry-based study of 12,100 cases in Western Sweden. Acta Orthop 2019; 90(2): 153-8.
- Rolfson O, Kärrholm J, Dahlberg L-E, Garellick G. Patient-reported outcomes in the Swedish Hip Arthroplasty Register: results of a nationwide prospective observational study. J Bone Joint Surg Br 2011; 93(7): 867-75.
- Rabin R, de Charro F. EQ-SD: a measure of health status from the EuroQol Group. Ann Med 2001; 33:(5): 337-43.
- Charnley J. The long-term results of low friction arthroplasty of the hip performed as a primary intervention. J Bone Joint Surg Br 1972; 54(1): 61-76.
- Gagnier J J, Morgenstern H, Kellam P. A retrospective cohort study of adverse events in patients undergoing orthopaedic surgery. Patient Saf Surg 2017; 11: 15.
- Goltz D E, Ryan S P, Howell C B, Attarian D, Bolognesi M P, Seyler T M. A weighted index of Elixhauser comorbidities for predicting 90-day readmission after total joint arthroplasty. J Arthroplasty 2019; 34(5): 857-64.
- Ravi B, Jenkinson R, Austin P C, Croxford R, Wasserstein D, Escott B, et al. Relation between surgeon volume and risk of complications after total hip arthroplasty: propensity score matched cohort study. BMJ 2014; 348: g3284.
- Greene M E, Rolfson O, Gordon M, Garellick G, Nemes S. Standard comorbidity measures do not predict patient-reported outcomes 1-year after total hip arthroplasty. Clin Orthop Relat Res 2015; 473: 3370-79.
- Elixhauser A, Steiner C, Harris R D, Coffey R M. Comorbidity measures for use with administrative data. Med Care 1998; 36(1): 8-27.
- van Walraven C, Austin P C, Jennings A, Quan H, Forster A J. A modification of the Elixhauser comorbidity measure into a point system for hospital death using administrative data. Med Care 2009; 47: 626-33.
- Ranstam J, Kärrholm J, Pulkkinen P, Mäkelä K, Espehaug B, Pedersen A B, et al. Statistical analysis of arthroplasty data, II: Guidelines. Acta Orthop 2011; 82(3): 258-67.
- Jolbäck P, Nauclér E, Bülow E, Lindahl H, Maziar M. A small number of surgeons outside the control-limit: an observational study based on 9,482 cases and 208 surgeons performing primary total hip arthroplasties in western Sweden. Acta Orthop 2020; 91(5): 581-6.
- Schubert R, Brown M, Gysler M, Brachinger H W. Financial decision making: are women really more risk averse? American Economic Review 1999; 89(2): 381-85.
- Barber B M, Odean T. Boys will be boys: gender, overconfidence, and common stock investment. Q J Economics 2001; 116: 261-92.
- Thorstensson C, Bergsten C. Better management of patients with osteoarthritis (BOA) annual report 2015. Gothenburg: Better Management of Patients with OsteoArthritis (BOA) register; 2016.
- Dust P, Corban J, Sampalis J, Antoniou J, Bergeron S G. Patient functional status as an indication for primary total hip arthroplasty: a systematic review and meta-analysis. J Arthroplasty 2022; 37(2): 390-7.
- Ludvigsson, J F, Andersson E, Ekholm A, Feychting M, Kim J L, Reuterwall C, et al. External review and validation of the Swedish national inpatient register. BMC Public Health 2011; 11: 450.
Supplementary data
| AE a | Concordance | Discordance | Concordance | Discordance | ||
| Surgeon/patient sex | Same | Different | M/M | F/F | M/F | F/M |
| Number of surgeries | 5,318 | 6,675 | 4,606 | 712 | 6,238 | 437 |
| A b | 197 (3.7) | 188 (2.8) | 186 (4.0) | 11 (1.6) | 179 (2.9) | 9 (2.1) |
| DA b | 168 (3.2) | 185 (2.8) | 149 (3.2) | 19 (2.7) | 170 (2.7) | 15 (3.4) |
| DB b | 42 (0.8) | 41 (0.6) | 41 (0.9) | 1 (0.0) | 39 (0.6) | 2 (0.5) |
| DB2 b | 0 (0.0) | 1 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.0) | 0 (0.0) |
| DC | 56 (1.1) | 59 (0.9) | 49 (1.1) | 7 (1.0) | 53 (0.9) | 6 (1.4) |
| DM | 74 (1.4) | 61 (0.9) | 68 (1.5) | 6 (1.0) | 55 (0.9) | 6 (1.4) |
| DM2 | 4 (0.0) | 3 (0.0) | 4 (0.1) | 0 (0.0) | 2 (0.0) | 1 (0.0) |
| a AE = adverse events, see Table 1 for abbreviations. | ||||||
| b SAEs = surgical adverse events. | ||||||
| Note: one patient might have multiple AEs/SAEs. | ||||||
| Factor | Concordance | Discordance | AIC | Concordance | Discordance | ||
| Surgeon/patient sex | Same | Different | Male/male | Female/female | Male/female | Female/male | |
| AEs within 90 days a | Reference | 0.82 (0.70–0.94) | 4,973,988 | Reference | 0.61 (0.42–0.88) | Reference | 0.97 (0.64–1.46) |
| AEs within 90 days b | Reference | 0.80 (0.66–0.93) | 5,678,720 | Reference | 0.58 (0.41–0.83) | Reference | 1.03 (0.69–1.54) |
| AIC = Akaike information criterion. | |||||||
| a Model adjusted for patient age, patient Elixhauser comorbidity index, years between specialist certification and index THA, and annual surgeon case volume. | |||||||
| b Only ICD-10 codes M16.0+M16.1 (bilateral/unilateral primary osteoarthritis of the hip) as an indication for surgery were included. Model adjusted for patient age, patient Elixhauser comorbidity index, and annual surgeon case volume. | |||||||