Corrigendum
Risk of reoperation due to surgical site infection in 74,771 hip fracture patients: a Danish nationwide cohort study
Nicolai K KRISTENSEN 1,3, Jeppe LANGE 1,3, Trine FRØSLEV 2, and Alma B PEDERSEN 2,3
1 Department of Orthopaedic Surgery, Horsens Regional Hospital; 2 Department of Clinical Epidemiology, Aarhus University Hospital, Aarhus; 3 Department of Clinical Medicine, Aarhus University, Aarhus, Denmark
Citation: Acta Orthopaedica 2022; 93: 887–893. DOI http://dx.doi.org/10.2340/17453674.2022.5357.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Published: 2022-11-30.
Correspondence: nicokris@rm.dk
Corrigendum of Acta Orthop 2022; 93: 760–766. doi: DOI 10.2340/17453674.2022.4580
The authors have unfortunately discovered that the originally published version of this article contains errors due to an error in inclusion of the specific combination of codes (KNFU 0–99 with T84.1) into definition of reoperation due to surgical site infection. This error leads to changes in most numeric result and in one of the conclusions, and therefore the article needed to be corrected. In this corrigendum, we supply the corrected data in Abstract, Results, Discussion sections, Table 1 and 4, as well as Figure 1 and Figure 2.
The authors apologize for any inconvenience caused.
In the Abstract, the following sentences are changed
Original paragraphs
Results — Overall, the 1-year net risk of reoperation due to SSI was 2.7%. The HR was lower for patients undergoing total/hemiarthroplasty surgery versus internal fixation (HR = 0.6; 95% CI 0.5–0.6) and for patients with per-/subtrochanteric fracture versus femoral neck fracture (HR = 0.7; CI 0.6–0.8). The risk of reoperation due to SSI decreased over time; HR was 0.6 (CI 0.5–0.7) for 2015–2016 compared with 2005–2006. Risk of reoperation decreased with increasing age; the HR was 0.6 (CI 0.6–0.7) in the more than 85-year-olds compared with 65–74-year-old patients.
Interpretation — The net risk of reoperations due to SSI in our study was higher than previously assumed. We identified several risk factors for increased risk of reoperation due to SSI, most noticeably treatment with internal fixation vs. arthroplasty, as well as younger age and femoral neck fracture diagnosis.
Corrected paragraphs
Results — Overall, the 1-year net risk of reoperation due to SSI was 1.6%. The HR was higher for patients undergoing total/hemiarthroplasty surgery versus internal fixation (HR = 1.5; 95%CI 1.3–1.8) and lower for patients with per-/sub-trochanteric fracture versus femoral neck fracture (HR = 0.6; CI 0.6–0.7). The risk of reoperation due to SSI decreased over time; HR was 0.7 (CI 0.5–0.8) for 2015–2016 compared with 2005–2006. Risk of reoperation decreased with increasing age; the HR was 0.8 (CI 0.7–1.0) in the more than 85-year-olds compared with 65–74-year-old patients. Charlson Comorbidity Index of ≥ 3 was associated with a higher risk of reoperation due to SSI, HR was 1.3 (CI 1.1–1.6).
Interpretation — The net risk of reoperations due to SSI in our study was lower than previously assumed. We identified several risk factors for increased risk of reoperation due to SSI, most noticeably treatment with arthroplasty vs. internal fixation, as well as younger age, high comorbidity burden, and femoral neck fracture diagnosis.
In the Results, the following sentences are changed
Original paragraphs
Reoperation due to SSI: time trend
Within 1 year of primary surgery, 1,688 of 74,771 hip fracture patients had undergone reoperation due to SSI, corresponding to a net risk of reoperation of 2.7%. During the study period, the net risk of reoperation due to SSI decreased from 3.4% in 2005–2006 to 2.1% in 2015–2016, corresponding to an adjusted HR of 0.6 (CI 0.5–0.7) (Table 4) and absolute reduction of 1.3%. A similar decrease in adjusted HRs was observed for follow-up periods 0–15, 0–30, and 0–90 days after hip fracture surgery. Overall, crude risk of reoperation was 2.3%, decreasing from 2.8% to 1.8% over the study period (Table 4).
Risk factors for reoperation due to SSI (Figures 1 and 2)
Sex and CCI were not risk factors for reoperation due to SSI within 1 year of hip fracture surgery. The HRs for reoperation due to SSI within 1 year decreased with increasing age. Thus, the HRs were 0.6 (CI 0.6–0.7) and 0.8 (CI 0.7–0.8) for patients aged above 85 and patients aged 75–84 years compared with the youngest age group (65–74 years), respectively. Similar results were obtained within 90 days of surgery.
The HR for reoperation due to SSI within 1 year was 0.7 (CI 0.6–0.8) for patients sustaining the per-/subtrochanteric fracture compared with patients sustaining femoral neck fractures. The HR at 90 days post-surgery was 0.6 (CI 0.6–0.7).
The HR was 0.6 (CI 0.5–0.6) within 1 year for patients undergoing total/hemiarthroplasty compared with patients undergoing internal fixation. However, at 90 days, HR was 0.9 (CI 0.8–1.1) for total/hemiarthroplasty compared with internal fixation.
Corrected paragraphs
Reoperation due to SSI: time trend
Within 1 year of primary surgery, 996 of 74,771 hip fracture patients had undergone reoperation due to SSI, corresponding to a net risk of reoperation of 1.6%. During the study period, the net risk of reoperation due to SSI decreased from 1.9% in 2005–2006 to 1.3% in 2015–2016, corresponding to an adjusted HR of 0.7 (CI 0.5–0.9) (Table 4) and absolute reduction of 0.6%. A similar decrease in adjusted HRs was observed for follow-up periods 0–15, 0–30, and 0–90 days after hip fracture surgery. Overall, crude risk of reoperation was 1.3%, decreasing from 1.6% to 1.1% over the study period (Table 4).
Risk factors for reoperation due to SSI (Figures 1 and 2)
Sex was not risk factors for reoperation due to SSI within 1 year of hip fracture surgery. High comorbidity burden was a risk factor for reoperation due to SSI within 1 year of hip fracture surgery with an adjusted HR of 1.3 (CI 1.1–1.6) for patients with high CCI (CCI ≥3 points) compared with low CCI. Similar result was seen at 90 days after surgery. The HRs for reoperation due to SSI within 1 year decreased with increasing age. Thus, the adjusted HRs at 1 year was 0.8 (CI 0.7–1.0) for patients aged above 85 years compared with the youngest age group (65–74 years) and 0.9 (CI 0.8–1.1) within 90 days of surgery.
The HR for reoperation due to SSI within 1 year was 0.6 (CI 0.6–0.7) for patients sustaining the per-/subtrochanteric fracture compared with patients sustaining femoral neck fractures. The HR at 90 days post-surgery was 0.6 (CI 0.5–0.7).
The HR was 1.5 (CI 1.3–1.8) within 1 year for patients undergoing total/hemiarthroplasty compared with patients undergoing internal fixation. At 90 days, HR was 2.4 (CI 2.0–3.0) for total/hemiarthroplasty compared with internal fixation.
In the Discussion, the following sentences are changed
Original paragraphs
This study shows 1-year net risk of reoperation due to SSI for all types of hip fractures over a 10-year period of 2.7%. There was a 45% decrease in reoperation due to SSI over time with the most recent 1-year net risk of reoperation being 2.1% in 2015–2016.
Our study finds an almost 50% lower rate of reoperations due to SSI within 1 year when hip fractures are treated with total or hemiarthroplasty compared with osteosynthesis. This somehow contradicts our other finding that per-/subtrochanteric fractures are associated with a lower risk of reoperation due to SSI than femoral neck fractures.
There is clearly a lower reoperation risk in the elderly patients above 85 years of age compared with the younger group. A low virulent infection (e.g., biofilm) could go undetected by the decreased immune response in the elderly (17), explaining the lower risk of reoperation with increasing age. Further, SSI symptoms typically occur within the first 2 years of surgery, and it is likely that older patients die before developing SSI symptoms (18).
In this large cohort study of 74,771 patients, the net risk of reoperation due to SSI within 1 year for all types of hip fractures treated in the period 2005–2016 was 2.7%. It is noteworthy that the highest risk of revision due to SSI were in the internal fixation group, compared with the arthroplasty treated patients.
There was a 45% decrease in reoperation due to SSI over time from 2005 to 2016 and we identified several risk factors for increased risk of reoperation due to SSI, including younger age and femoral neck fracture.
Corrected paragraphs
This study shows 1-year net risk of reoperation due to SSI for all types of hip fractures over a 10-year period of 1.6%. There was a 33% decrease in reoperation due to SSI over time with the most recent 1-year net risk of reoperation being 1.3% in 2015–2016.
Our study finds an almost 54% higher rate of reoperations due to SSI within 1 year when hip fractures are treated with total or hemiarthroplasty compared with osteosynthesis. This is in line with our other finding that per-/subtrochanteric fractures are associated with a lower risk of reoperation due to SSI than femoral neck fractures.
There is a lower reoperation risk in the elderly patients above 85 years of age compared with the younger group. A low virulent infection (e.g., biofilm) could go undetected by the decreased immune response in the elderly (17), explaining the lower risk of reoperation with increasing age. Further, SSI symptoms typically occur within the first 2 years of surgery, and it is likely that older patients die before developing SSI symptoms (18). It is also likely that patients who are older than 85 years are somehow selected and our results are due to “healthy survival bias”.
In this large cohort study of 74,771 patients, the net risk of reoperation due to SSI within 1 year for all types of hip fractures treated in the period 2005–2016 was 1.6%. It is noteworthy that the highest risk of revision due to SSI were in the arthroplasty-treated patients, compared with the internal fixation group.
There was a 33% decrease in reoperation due to SSI over time from 2005 to 2016 and we identified several risk factors for increased risk of reoperation due to SSI, including younger age, high CCI (CCI ≥ 3 points), and femoral neck fracture.
In the Tables, the following is changed
Original Table 1
Corrected Table 1
| Operation codes |
| KNFC 0–99 (= secondary arthroplasty in hip joints): Needs to be combined with the ICD-10 codes (minus T84.1) |
| KNFW49 (= reoperation for cicatrice rupture following operation in hip or thigh): Needs to be combined with the ICD-10 codes |
| KNFW59 (= reoperation at superficial surgical site infection following operation in hip or thigh): Does NOT require combination with ICD-10 codes but can be combined with the ICD-10 code |
| KNFW69 (= reoperation at deep surgical site infection following operation in hip or thigh): Does NOT require combination with ICD-10 codes but can be combined with the ICD-10 code |
| KNFU 0–99 (= removal of internal fixation or prosthesis): Needs to be combined with the ICD-10 codes (minus T84.1) |
| KNFG 09–59 (= joint resection, arthroplasties, arthrodesis, in hip joint): Needs to be combined with the ICD-10 codes |
| KNFS19, KNFS29, KNFS49, KNFS59, KNFS99: Does not require combination with ICD-codes |
| Diagnosis codes (based on ICD-10 codes) |
| T84.5 |
| T84.6 |
| T84.1 (not in combination with KNFC 0–99 or KNFU 0–99) |
| T84.7 |
| T81.4 |
| T81.3 |
| ICD codes = International Classification of Diseases codes. |
Corrected Table 4
| Follow-up period Calendar period of diagnosis | No. of patients | No. of infections | Cumulative incidence, % (95% CI) | Kaplan–Meier risk, % (95% CI) | Crude hazard ratio (HR) (95% CI) | Adjusted a hazard ratio (HR) (95% CI) |
| 0–15 days of surgery | ||||||
| 2005–2006 | 12,453 | 30 | 0.24 (0.17–0.34) | 0.26 (0.18–0.36) | Reference | Reference |
| 2007–2008 | 13,236 | 20 | 0.15 (0.10–0.23) | 0.16 (0.10–0.25) | 0.63 (0.36–1.10) | 0.62 (0.35–1.09) |
| 2009–2010 | 12,724 | 16 | 0.13 (0.08–0.20) | 0.13 (0.08–0.21) | 0.52 (0.28–0.96) | 0.52 (0.28–0.95) |
| 2011–2012 | 12,706 | 18 | 0.14 (0.09–0.22) | 0.15 (0.09–0.24) | 0.59 (0.33–1.06) | 0.58 (0.32–1.04) |
| 2013–2014 | 12,285 | 25 | 0.20 (0.14–0.30) | 0.22 (0.14–0.32) | 0.84 (0.49–1.43) | 0.83 (0.49–1.41) |
| 2015–2016 | 11,367 | 15 | 0.13 (0.08–0.21) | 0.14 (0.08–0.23) | 0.54 (0.29–1.01) | 0.53 (0.29–0.99) |
| 2005–2016 | 74,771 | 124 | 0.17 (0.14–0.20) | 0.18 (0.15–0.21) | ||
| 0–30 days of surgery | ||||||
| 2005–2006 | 12,453 | 72 | 0.58 (0.46–0.72) | 0.63 (0.49–0.78) | Reference | Reference |
| 2007–2008 | 13,236 | 63 | 0.48 (0.37–0.61) | 0.52 (0.40–0.66) | 0.82 (0.59–1.15) | 0.82 (0.58–1.15) |
| 2009–2010 | 12,724 | 62 | 0.49 (0.38–0.62) | 0.53 (0.41–0.68) | 0.84 (0.60–1.18) | 0.84 (0.60–1.18) |
| 2011–2012 | 12,706 | 67 | 0.53 (0.41–0.67) | 0.58 (0.45–0.73) | 0.92 (0.66–1.28) | 0.91 (0.65–1.28) |
| 2013–2014 | 12,285 | 85 | 0.69 (0.56–0.85) | 0.75 (0.60–0.92) | 1.19 (0.87–1.64) | 1.18 (0.86–1.62) |
| 2015–2016 | 11,367 | 47 | 0.41 (0.31–0.55) | 0.45 (0.33–0.59) | 0.71 (0.49–1.03) | 0.70 (0.49–1.02) |
| 2005–2016 | 74,771 | 396 | 0.53 (0.48–0.58) | 0.57 (0.52–0.63) | ||
| 0–90 days of surgery | ||||||
| 2005–2006 | 12,453 | 136 | 1.09 (0.92–1.29) | 1.22 (1.03–1.43) | Reference | Reference |
| 2007–2008 | 13,236 | 116 | 0.88 (0.73–1.05) | 0.98 (0.82–1.17) | 0.80 (0.63–1.03) | 0.80 (0.62–1.03) |
| 2009–2010 | 12,724 | 122 | 0.96 (0.80–1.14) | 1.07 (0.90–1.28) | 0.88 (0.69–1.12) | 0.88 (0.69–1.12) |
| 2011–2012 | 12,706 | 118 | 0.93 (0.77–1.11) | 1.05 (0.87–1.25) | 0.86 (0.67–1.10) | 0.85 (0.67–1.09) |
| 2013–2014 | 12,285 | 129 | 1.05 (0.88–1.24) | 1.16 (0.98–1.38) | 0.96 (0.76–1.23) | 0.95 (0.75–1.21) |
| 2015–2016 | 11,367 | 93 | 0.82 (0.67–1.00) | 0.91 (0.74–1.11) | 0.74 (0.57–0.97) | 0.74 (0.57–0.96) |
| 2005–2016 | 74,771 | 714 | 0.95 (0.89–1.03) | 1.07 (0.99–1.15) | ||
| 0–365 days of surgery | ||||||
| 2005–2006 | 12453 | 199 | 1.60 (1.39–1.83) | 1.87 (1.62–2.14) | Reference | Reference |
| 2007–2008 | 13,236 | 171 | 1.29 (1.11–1.50) | 1.52 (1.31–1.76) | 0.81 (0.66–0.99) | 0.81 (0.66–0.99) |
| 2009–2010 | 12,724 | 169 | 1.33 (1.14–1.54) | 1.56 (1.34–1.81) | 0.84 (0.68–1.03) | 0.83 (0.68–1.02) |
| 2011–2012 | 12,706 | 164 | 1.29 (1.11–1.50) | 1.52 (1.30–1.77) | 0.82 (0.66–1.01) | 0.81 (0.66–0.99) |
| 2013–2014 | 12,285 | 169 | 1.38 (1.18–1.59) | 1.58 (1.36–1.84) | 0.86 (0.70–1.06) | 0.85 (0.69–1.04) |
| 2015–2016 | 11,367 | 124 | 1.11 (0.93–1.32) | 1.28 (1.07–1.52) | 0.69 (0.55–0.86) | 0.67 (0.54–0.85) |
| 2005–2016 | 74,771 | 996 | 1.34 (1.25–1.42) | 1.56 (1.46–1.66) | ||
| a Hazard ratio adjusted for age, sex, and comorbidity by the Charlson comorbidity index; CI = confidence interval; Cumulative incidence = crude risk of reoperation; Kaplan–Meier risk = net risk of reoperation. | ||||||
In the Figures, Events and Adjusted HRs (CI) are changed
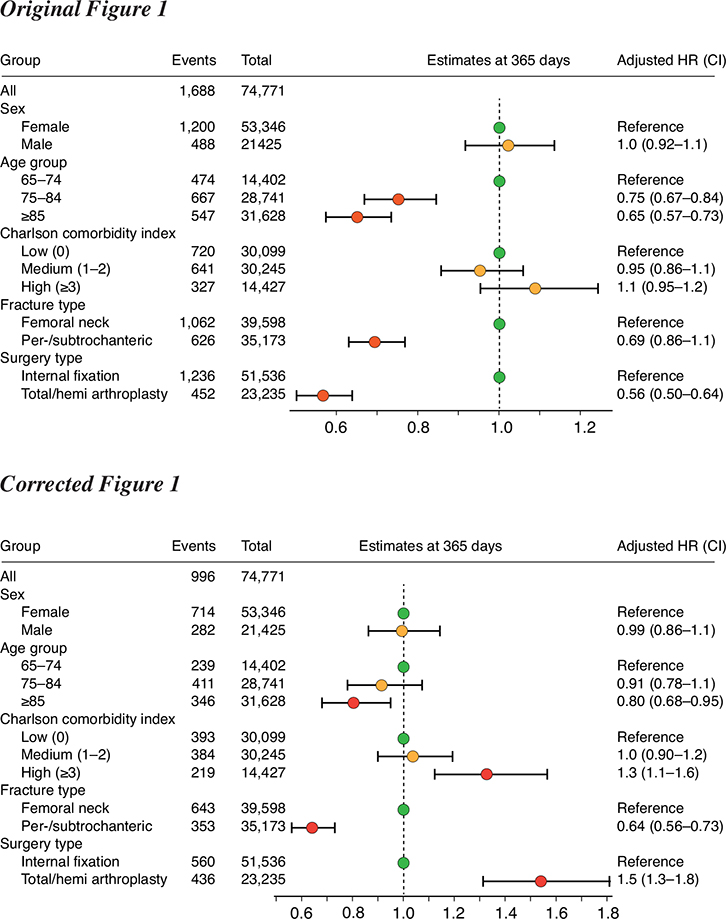
Figure 1. Risk factors for reoperation due to SSI within 1 year of hip fracture surgery.
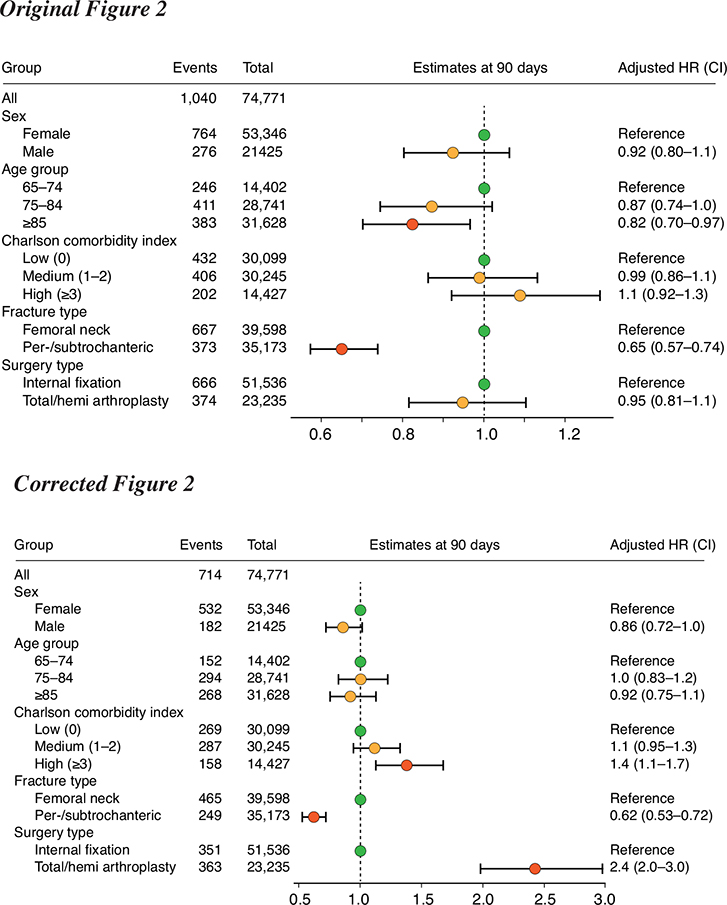
Figure 2. Risk factors for reoperation due to SSI within 90 days of hip fracture surgery.
In the References, the following is changed
Original references
19. Ferguson R, Prieto-Alhambra D, Peat G, Delmestri A, Jordan KP, Strauss V Y, et al. Influence of pre-existing multimorbidity on receiving a hip arthroplasty: Cohort study of 28 025 elderly subjects from UK primary care. BMJ Open 2021; 11(9): 1-7. Deleted reference.
20. Rogmark C, Kristensen M T, Viberg B, Rönnquist S S, Overgaard S, Palm H. Hip fractures in the non-elderly—Who, why and whither? Injury 2018; 49(8): 1445-50. doi: 10.1016/j.injury.2018.06.028
Corrected references
19. Rogmark C, Kristensen M T, Viberg B, Rönnquist S S, Overgaard S, Palm H. Hip fractures in the non-elderly—Who, why and whither? Injury 2018; 49(8): 1445-50. doi: 10.1016/j.injury.2018.06.028. New number.
20. Kjørholt K E, Kristensen N R, Prieto-Alhambra D, Johnsen S P, Pedersen A B. Increased risk of mortality after postoperative infection in hip fracture patients. Bone 2019; 127: 563-70. doi: 10.1016/j.bone.2019.07.023. Added reference.