Efficacy of adding an interspace block to the posterior knee for perioperative pain in total knee arthroplasty: a randomized controlled trial
Swist CHATMAITRI 1, Suwimon TANGWIWAT 2, Pathom HALILAMIEN 2, Pakpoom RUANGSOMBOON 1, Chaturong PORNRATTANAMANEEWONG 1, Keerati CHAREANCHOLVANICH 1, and Rapeepat NARKBUNNAM 1
1 Department of Orthopaedic Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok; 2 Department of Anesthesiology, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand
Background and purpose — The interspace between the popliteal artery and the capsule of the posterior knee (IPACK) block is a novel anesthetic technique for total knee arthroplasty (TKA). Our objective was to compare the effect of IPACK and adductor canal block (ACB) and periarticular injection (PAI), relative to ACB and PAI only, from baseline to postoperative day 3, in patients undergoing unilateral primary TKA.
Patients and methods — This was a single-center, double-blinded, randomized controlled trial. Adults over the age of 50 who were scheduled for unilateral primary TKA were enrolled. They were randomly assigned to ACB and PAI block (control group), or ACB, PAI, and IPACK block (IPACK group). The primary outcome was mean pain at rest during 24–48 hours post-operation using a numerical rating scale (0–10). We also investigated opioid use and ambulation pain.
Results — 89 patients were evaluated, 45 from the control group and 44 from the IPACK group. Despite slightly higher mean pain score at rest in the control group, no statistically significant difference was found during 0–24 hours (0.13; 95% CI –0.19 to 0.46), 24–48 hours (0.42; CI –0.06 to 0.89), and 48–72 hours (0.35; CI 0.00 to 0.69) postoperatively as well as in maximum pain scores at rest. Neither pain during ambulation nor the number of opioids used differed between the trial groups at any given time point.
Conclusion — The addition of the IPACK block to ACB and PAI did not reduce postoperative pain intensity or opioid usage. Therefore, IPACK block may not offer any benefit for pain management in patients undergoing unilateral primary TKA who are already receiving ACB and PAI.
Citation: Acta Orthopaedica 2022; 93: 894–900. DOI http://dx.doi.org/10.2340/17453674.2022.5257.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: Accepted: Published: 2022-11-30.
Correspondence: Rapeepat Narkbunnam, mai_parma@hotmail.com
SC provided the research questions, conducted data collection, analyzed data, and wrote the manuscript. ST, PH, and PR conducted data collection, analyzed data and discussion, and developed the full manuscript. CP and RN examined all data analysis, detailed the results, undertook statistical calculation, and monitored data and discussion. KC also provided useful advice and finalized the manuscript.
The authors acknowledge the assistance of Mr. Suthipol Udompunthurak, Ms. Nichakorn Khomawut, and Ms. Piyawadee Rungmongkolsab for their contributions to this study. We thank Onlak Ruangsomboon for her assistance in editing the manuscript.
Handling co-editors: Nils Hailer and Robin Christensen
Acta thanks Martin Sundberg for help with peer review of this study.
One of the most common concerns following total knee arthroplasty (TKA) is perioperative pain. Currently, there are several analgesic methods for perioperative pain control, 2 of which are adductor canal blocks (ACB) and periarticular injections (PAI). These 2 methods can either be performed separately or combined. They are among the most used methods, and they have been shown to result in favorable outcomes (1-3). Although their comparative effects for pain control have been controversial, the combined method tended to provide at least equivalent or better pain control compared with either single method alone (4-8).
During the last few years, a novel technique whereby an anesthetic agent is infiltrated into the interspace between the popliteal artery and the capsule of the posterior knee, or IPACK block, has become increasingly popular in TKA (9). It has been claimed to deliver additional pain relief when administered in addition to other standard procedures. In fact, this benefit may partly occur because ACB could not yield adequate pain control around the posterior knee (10). There have been many studies demonstrating the benefits of the IPACK block for TKA patients (11-13).
Even though several studies have demonstrated the effects of the IPACK block on TKA patients, to date no randomized controlled trials have evaluated the benefits of adding the IPACK block to combined ACB and PAI. We hypothesized that the addition of the IPACK block to ACB and PAI could reduce postoperative pain levels during the first 72 hours after TKA. Therefore, we conducted this study to evaluate whether adding the IPACK block could yield further beneficial effects for patients undergoing unilateral primary TKA.
Patients and methods
Study design and setting
This study was a single-center, double-blinded, randomized controlled trial conducted between July 2019 and May 2021 at the Department of Orthopaedic Surgery, Siriraj Hospital, Bangkok, Thailand. This is the largest tertiary university hospital in Thailand. All participants provided written informed consent prior to their enrollment in the study.
Participants
Included patients were those aged 50 years or older who were scheduled for unilateral primary TKA. Patients were excluded if they had contraindications to any of the anesthetic methods or analgesic drugs used in the study, e.g., infection at the site of injection, coagulopathy or drug allergy, chronic kidney disease with creatinine clearance < 50 mL/minute, BMI of > 35 or < 18, any previous ipsilateral knee surgery, severe medical conditions defined as American Society of Anesthesiologists (ASA) class IV or higher, and unwillingness to participate.
Allocation and randomization
On the day of hospital admission, TKA-eligible individuals were screened. If inclusion and exclusion criteria were met and patients agreed to participate, informed consent was obtained. Using a computer-generated sequence, participants were randomly assigned to the control (ACB + PAI) or IPACK group (ACB + PAI + IPACK). The randomization sequence was hidden in sealed envelopes. Before the operation, the anesthesiologists in charge opened these sealed packets. Surgeons were blinded to participant interventions.
Interventions and procedures
Before and during the operation, all patients received standard spinal block, PAI, and ACB. Only patients in the IPACK group also received the IPACK block.
Adductor canal block (ACB)
Before the operation, in the regional anesthesia block room the patients were placed in a supine position for anesthetic procedures. Anesthetic drugs, which were 15 mL of 0.33% bupivacaine and 5 mg of dexamethasone, were injected into the adductor canal identified under the layer of the sartorius muscle at midthigh using ultrasound guidance (USG). The USG-adductor canal block technique was performed with an in-plane needle approach from lateral to medial direction using 8 cm, 22 G Stimuplex Ultra (B. Braun [Thailand] Ltd, Bangkok, Thailand). Successful USG-adductor canal block was confirmed by observing the local anesthetic spread in the adductor canal under ultrasound and palpating the cold sensation on the medial side of the leg.
IPACK block
After the USG adductor canal block was completed, the curvilinear ultrasound transducer (2–5 MHz) was applied while the patient was in a supine position. 20 mL of 0.25% bupivacaine was injected into the space between the femur and popliteal artery above the level of the popliteal crease. The needle was inserted from anterior to posterior direction, using an in-plane approach. The procedure was ultrasound-guided and performed under a sterile technique by one of 2 anesthesiologists experienced in ultrasound-guided peripheral nerve block (ST, PL).
Periarticular injection (PAI)
During the operation, a solution composed of 0.5% levobupivacaine 20 mL (100 mg), ketorolac 30 mg, and adrenaline 0.5 mg diluted with normal saline to 100 mL was injected around the knee equally at the anterior, medial, lateral, and posterior aspects.
Operative procedures
After the anesthetic procedures were completed according to the assigned group of each study participant, the operation was initiated. 1 of the 3 orthopedic surgeons at our institution performed all operations using the same surgical technique.
For every patient who underwent primary TKA, a pneumatic tourniquet with 300 mmHg pressure was applied. 2 grams of intravenous cefazolin (or 900 mg of clindamycin in the case of penicillin allergy) was given prior to making a skin incision. Tranexamic acid was administered intravenously in all cases to reduce blood loss. A midline skin incision was performed with medial parapatellar arthrotomy. The lengths of the incision and arthrotomy depended on the surgeon to allow for adequate exposure. Patellar denervation was done by electrical cauterization 1–2 mm around the patella without patellar resurfacing. Only cemented posterior-stabilized prostheses were used, but the selected prosthesis brand for each patient was at the surgeon’s discretion. A drain was placed postoperatively for 24–48 hours and was clamped during the first 3 hours. All surgeons obtained the same PAI protocol. Subcutaneous and subcuticular skin closures were performed by using Vicryl 3-0 and Monocryl 4-0, respectively. No Jones bandage or slab was applied after the surgery.
Other pain control protocol
Pre-emptive analgesia consisted of paracetamol and etoricoxib was prescribed as preoperative medication. For postoperative pain control, fentanyl intravenous patient-controlled analgesia (IV-PCA) was provided during the first 72 hours and then switched to morphine syrup. Postoperative oral medications included paracetamol, etoricoxib, and gabapentin. Prescribed home medications were Ultracet (paracetamol/acetaminophen + tramadol), gabapentin, and etoricoxib.
Postoperative procedures
The same postoperative protocol was applied to all participants. They also received the same in-hospital rehabilitation protocol provided by the hospital’s physical therapy team. Also, early knee range of motion (ROM) exercises and ambulation with supporting devices were encouraged for all patients.
Outcome measurement
The primary outcome of the study was the postoperative pain score at rest 24–48 hours following surgery. We expected that the spinal block’s effect would have diminished, whereas the IPACK block’s effect could still be in effect at this time interval; hence, we chose this time interval as the primary outcome. The secondary outcomes were average and maximum postoperative pain scores at rest and during ambulation during the initial 72 hours postoperatively, the dominant location of pain, time to the first dose of opioid, the amount of opioid consumption, knee ROM, and length of hospital stay.
Postoperative pain was measured using the numerical rating scale (NRS), a scale ranging from 0 (no pain) to 10 (the worst pain). The NRS and visual analog scale (VAS) are among the most common methods for pain evaluation and are highly correlated (13). We used the NRS as it was the standard method for pain evaluation in our institution. Participants were asked to rate their NRS scores verbally. NRS at rest was recorded every 4 hours for 72 hours by the ward nurses, and the scores were verified daily by the nurses from the acute pain service (APS) team. The mean pain score for each 24-hour interval during the first 72 hours after the operation was then calculated. The patient identified the dominant location of pain and classified it as (1) anterior, (2) posterior, (3) generalized and/or unidentified, or (4) no pain. NRS during ambulation was recorded once daily during the physical therapy session. Knee ROM was measured on the third day after the operation by a research coordinator. The APS team recorded the time to the first dose of fentanyl (IV-PCA) and the total amount of opioid consumption.
All participants were reassessed at 2 and 6 weeks after the operation. Knee ROM was reassessed and recorded at those visits by the research coordinator. The research coordinator and the nurses who assessed the outcomes were all blinded to knowledge of the study group.
Statistics
According to the study by Grosso et al. (4), the mean VAS for pain in the control group was 3.0/10 points (standard deviation [SD] 2.1). A study by Danoff et al. (15) suggested that the minimum detectable change (MDC) for pain in VAS after TKA was approximately 16/100 points. With an assumption that the IPACK block could further reduce at least 1.5/10 points of pain, and with type 1 and type 2 errors of 0.05 and 0.1, respectively, a total of 42 participants per group was required. To cover a dropout rate of 10%, the total sample size of the study was 94.
SPSS software version 18 (SPSS Inc, Chicago, IL, USA) was employed for all statistical analyses of the study. For demographic data, descriptive statistics were employed. Categorical data is reported as number and percentage. Continuous variables are reported as mean and standard error of mean or median with interquartile range for normally distributed and non-normally distributed data, respectively.
Categorical data was compared using the chi-square test for inferential statistics, and continuous data was compared using Student’s t-test (data aligned with Kolmogorov–Smirnov normality test) or the Mann–Whitney U test (data with non-normal distribution). Comparisons of the mean and maximum NRS scales measured during each 24-hour interval were performed using repeated measures analysis. Results are presented as means with 95% confidence intervals (CI) or medians with interquartile ranges. The estimated marginal means was calculated and presented with standard error of means (SEM). A p-value < 0.05 was considered statistically significant. Analysis of covariance (ANCOVA) was used to compare knee ROM between the 2 groups using preoperative ROM as covariates.
Ethics, registration, data sharing, funding, and disclosures
The study was approved by the Siriraj Institutional Review Board (ID 265/2562 (EC2)) and prospectively registered in www.thaiclinicaltrials.org (TCTR20190715001). No changes to the study protocol were made after the study commenced. Data is available from the Siriraj Institutional Data Access/Ethics Committee (contact via orthoresearch.si@gmail.com) for researchers who meet the criteria for access to confidential data. This work was funded by the Faculty of Medicine Siriraj Hospital, Mahidol University (grant numbers 126/2562). The authors have no competing interests as defined by Acta Orthopaedica, or other interests that might be perceived to influence the results and/or discussion reported in this paper. All authors declare no personal or professional conflicts of interest, and no financial support from the companies that produce and/or distribute the drugs, devices, or materials described in this report.
Results
A Consolidated Standards of Reporting Trials (CONSORT) flow diagram is presented in Figure 1. 139 patients underwent unilateral primary TKA by the participating surgeons at our hospital between August 2019 and April 2021. Of these, 98 patients were eligible for the study. 1 patient declined to participate, and another 3 refused to receive spinal block; they were thus excluded. Moreover, 5 patients dropped out of the study due to complications or deterioration of cognitive function that raised concerns about IV-PCA use and the credibility of self-reported NRS scores. These patients had faced complications causing their dropouts early, within 24 hours postoperation, thereby not being able to follow the postoperative protocol, and thus were unable to provide relevant data for the study. Consequently, we excluded them from the analysis. 89 participants were included in the analysis: 44 in the IPACK group and 45 in the control group. There was no missing data on the variables collected during the participants’ hospital admission. However, there were 7 patients in whom the data on knee ROM at 6 weeks postoperatively was missing. This missing data was considered missing at random and was imputed using the last observation carry-forward method.
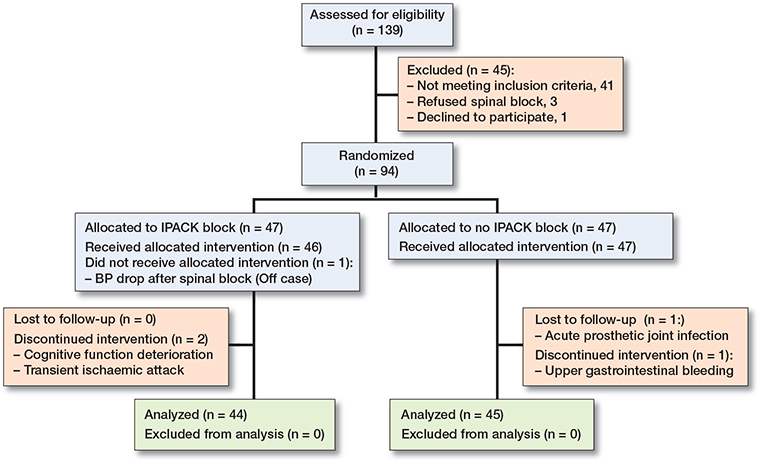
Figure 1. Flowchart of the study
More females than male patients underwent TKA (Table 1). BMI, the side of surgery, ASA classification, knee alignment, and history of previous contralateral knee surgery were comparable between the 2 groups (Table 1). The median length of stay was 5 days in both groups (p = 0.5), and the median operative time was 88 minutes in the IPACK group and 80 minutes in the control group (p = 0.5).
| Factor | IPACK (n = 44) | Control (n = 45) | |
| Age, mean (SD) | 71 (7.1) | 70 (6.9) | |
| Female sex | 37 | 39 | |
| BMI a | 26 (24–29) | 27 (25–30) | |
| ASA classification: | |||
| 1 | 3 | 3 | |
| 2 | 35 | 38 | |
| 3 | 6 | 4 | |
| Side of knee | |||
| Right | 17 | ||
| Left | 27 | 24 | |
| Knee alignment | |||
| Neutral | 1 | 2 | |
| Varus | 33 | 27 | |
| Valgus | 10 | 16 | |
| Previous contralateral | |||
| knee surgery | 24 | 20 | |
| Length of stay (days) a | 5 (5–6) | 5 (5–6) | |
| Operative time (min) a | 88 (70–105) | 80 (73–95) | |
| Estimated blood loss (mL) a | 10 (10–20) | 10 (5–20) | |
| a mean (range) IPACK = interspace between the popliteal artery and the capsule of the posterior knee; ASA = American Society of Anesthesiologists; BMI = body mass index. |
|||
The IPACK group had a slightly lower mean and maximum level of postoperative pain at rest during the first 72 hours compared with the control group, although the differences failed to reach statistical significance (Table 2, Figure 2). For pain during ambulation, despite generally lower pain levels across the time intervals assessed in the IPACK group, there was also no significant difference between the 2 groups at any given time interval.
| Factor | IPACK (n = 44) | Control (n = 45) | Mean difference Control–IPACK (CI) |
| Average pain at rest | |||
| 0–24 hours | 0.46 (0.12) | 0.59 (0.11) | 0.13 (–0.19 to 0.46) |
| 24–48 hours | 0.55 (0.14) | 0.97 (0.19) | 0.42 (–0.06 to 0.89) |
| 48–72 hours | 0.27 (0.08) | 0.62 (0.15) | 0.35 (0.00 to 0.69) |
| Estimated marginal means | 0.43 (0.11) | 0.73 (0.11) | 0.30 (–0.02 to 0.62) |
| Maximum pain at rest | |||
| 0–24 hours | 1.55 (0.30) | 1.93 (0.30) | 0.39 (–0.46 to 1.24) |
| 24–48 hours | 1.68 (0.36) | 2.64 (0.35) | 0.96 (–0.04 to 1.96) |
| 48–72 hours | 1.00 (0.26) | 1.44 (0.26) | 0.44 (–0.28 to 1.17) |
| Estimated marginal means | 1.41 (0.24) | 2.01 (0.23) | 0.60 (–0.60 to 1.26) |
| Pain during ambulation | |||
| 0–24 hours | 3.30 (0.20) | 3.47 (0.26) | 0.17 (–0.48 to 0.82) |
| 24–48 hours | 3.00 (0.22) | 3.16 (0.25) | 0.16 (–0.51 to 0.82) |
| 48–72 hours | 2.52 (0.21) | 2.56 (0.26) | 0.03 (–0.63 to 0.70) |
| Estimated marginal means | 2.94 (0.19) | 3.06 (0.19) | 0.12 (–0.41 to 0.65) |
| IPACK see Table 1 | |||
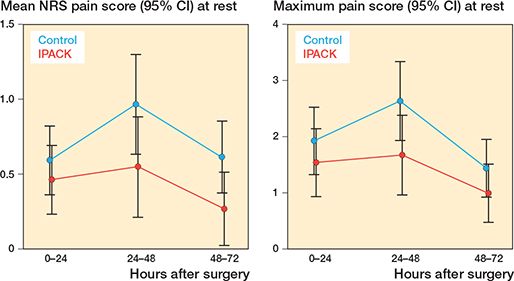
Figure 2. Mean NRS pain (left panel) and maximum NRS pain (right panel) during 0–72 hours after surgery.
The dominant pain location, however, was, significantly different between the study groups (p = 0.006). In the IPACK group, pain was located predominantly at the anterior part of the knee in 33 of 44, while no participant reported isolated posterior knee pain (Table 3). Conversely, the most dominant pain location in the control group was the anterior part in only 19 of 45.
| Factor | IPACK (n = 44) | Control (n = 45) | p-value |
| Dominant pain location | 0.003 | ||
| Anterior | 33 | 19 | |
| Posterior | 0 | 6 | |
| Both | 10 | 17 | |
| No pain | 1 | 3 | |
| Time to first dose of fentanyl | 0.4 | ||
| No fentanyl | 0 | 3 | |
| 0–24 hours | 40 | 39 | |
| 24–48 hours | 3 | 3 | |
| 48–72 hours | 1 | 0 | |
| Consumption of IV fentanyl (μg) | |||
| 0–24 hours | 83 (45–195) | 90 (38–218) | 1 |
| 24–48 hours | 105 (45–61) | 120 (45–210) | 0.4 |
| 48–72 hours | 60 (15–173) | 60 (30–135) | 0.5 |
| Total fentanyl (mg) | 0.24 (0.11–0.47) | 0.30 (0.13–0.51) | 0.6 |
| Oral morphine (mg) | 0 (0–0) | 0 (0–4) | 0.1 |
| IPACK see Table 1 | |||
The time to first dose of fentanyl did not differ between the 2 groups. No between-group difference was seen in the amount of opioid consumption, whether calculated as the overall dose or the dosage prescribed within any 24-hour interval. Furthermore, there was no statistically significant difference regarding postoperative ROM measured at 3 days, 2 weeks, and 6 weeks post-operation between the 2 groups (Table 4).
| ROM (°) | IPACK (n = 44) | Control (n = 45) | Mean difference Control–IPACK (CI) |
| Baseline | 117 (2.8) | 112 (2.8) | –4.7 (–12 to 3.2) a |
| Day 3 | 90 (2.2) | 88 (3.1) | 0.1 (–7.1 to 7.3) b |
| 2 weeks | 98 (1.8) | 98 (2.1) | 1.4 (–4.1 to 6.8) b |
| 6 weeks | 112 (1.6) | 109 (2.0) | –2.7 (–7.8 to 2.4) b |
| Estimated marginal means | 104 (1.8) | 101 (1.8) | –3.0 (–8.1 to 2.1) c |
| IPACK see Table 1. a 95% CI by independent t-test. b 95% CI by ANCOVA using range of motion at baseline as covariate. c 95% CI by repeated ANOVA. |
|||
Discussion
The efficacy of the IPACK block has been controversial, as studies evaluating its effect have been limited and have given conflicting results. While some studies have favored its use, others have reported no additional benefits (9,11-13,16). A recently published study by Patterson et al. (16) demonstrated that the addition of the IPACK block to continuous ACB (CACB) could only decrease the average and worst post-operative pain scores at rest in the post-anesthesia care unit (PACU). However, it did not offer additional benefits in terms of pain reduction at rest and during physical therapy on the first day after the operation, opioid consumption, walking distance, or length of stay. With the advantage considered to be minimal, the authors did not recommend routine use of the IPACK block. In contrast, another study by Kertkiatkachorn et al. (9) compared CACB + IPACK block with CACB + PAI and found that the IPACK block was non-inferior to PAI in decreasing the pain score at 12 hours postoperatively and after 24 hours postoperatively. Although the group that received the IPACK block required a significantly higher amount of morphine at 48 hours after the operation, this could have been because of the higher incidence of moderate to severe breakthrough pain in the IPACK than in the PAI group.
Because multimodal anesthetic regimens are recommended as the anesthetic method of choice for TKA, many studies have evaluated the impact of adding the IPACK block to various established regimens. Although ACB + PAI has already been accepted as the standard anesthetic method with proven efficacy in providing adequate pain relief (4-8), the evolution of IPACK has raised the question of whether its addition may provide further clinical benefits. Consequently, we conducted this study to investigate if adding the IPACK block to ACB and PAI could decrease postoperative pain as we hypothesized. To the best of our knowledge, this study was the first randomized controlled trial to compare the effects of adding the IPACK block to ACB and PAI versus ACB and PAI alone for patients undergoing unilateral primary TKA.
The present study demonstrated that the addition of the IPACK block did not decrease the overall pain at any time point or period following unilateral primary TKA, discordant with some other previous studies (11-13). Because ACB + PAI, the control treatment in the present study, has already been shown to deliver favorable pain relief in many previous studies (4-8), the high efficacy of this treatment received in both the study groups could have explained the insignificant benefit of adding the IPACK block. However, we discovered that the IPACK block could effectively relieve pain predominantly at the posterior knee, which occurred most likely because the IPACK procedure involves infiltrating a local anesthetic agent into the posterior region of the knee, where many articular sensory nerves are situated (17,18). It is worth mentioning that the method we used to measure the dominant pain location was more reliable than the previous study (9). We assessed the outcome by directly asking the patients to locate the area with the maximum pain. The previous study measured pain scales at different areas around the knee, possibly causing confusion and difficulty for the patients to differentiate pain scores in adjacent areas (9).
Nonetheless, the amount of opioid consumption at any time interval did not differ whether the patients received the IPACK block or not. Interestingly, the postoperative pain scores in both study groups in the present study were relatively lower than those reported in previous studies (6-8,9,11-13,16), which could have been due to the use of IV-PCA in our setting. We routinely apply IV-PCA to patients who undergo primary TKA at our institution to eliminate the requirement for rescue analgesia for breakthrough pain. Furthermore, we believe that IV-PCA was effective because the incidence of breakthrough pain was minimal in our study.
From the results of the present study, even though the IPACK block could reduce posterior knee pain, we do not suggest its implementation for primary unilateral TKA if the standard anesthetic method already involves both ACB and PAI, because adding the IPACK block did not deliver additional clinically important benefits as hypothesized, such as overall postoperative pain in the first 72 hours, postoperative ROM, or the amount of opioid consumption. Also, the IPACK block is an operator-dependent intervention that requires the technical expertise of regional pain specialists and may take longer than usual to operate. We believe that our result could suggest institutions that already employ ACB and PAI as their routine anesthetic procedures but are considering whether to implement the IPACK block not pursue such intention.
There are some limitations to our study. First, we did not perform sham procedures for the control group as this might have caused additional unnecessary risks for the patients. Therefore, the participants cannot be blinded to the intervention, probably affecting patient-reported outcomes. Second, anesthetic drugs could have been injected into the interspace between the popliteal artery and the capsule of the posterior knee following PAI. However, we believed that the amount of drugs in the interspace was limited because the technique was done intraoperatively by the surgeon without ultrasound guidance. Third, IV-PCA was provided for all postoperative cases, which might have caused the patients to report very low pain scores, possibly masking statistically significant differences between the 2 groups. Nonetheless, we found no statistically relevant differences in opioid dosage at any of the studied time intervals. Therefore, we believe that there was truly no difference between the 2 interventions, regardless of IV-PCA prescription.
In conclusion, our study showed no decrease in pain or the amount of opioid consumption. There was also no difference in time to the first fentanyl dose, knee range of motion, or duration of hospitalization. The study does not support the addition of the IPACK block in patients already receiving both ACB and PAI as their anesthetic methods for unilateral primary TKA.
- Burkett-St Laurant D, Peng P, Giron Arango L, Niazi A U, Chan V W, Agur A, et al. The nerves of the adductor canal and the innervation of the knee: an anatomic study. Reg Anesth Pain Med 2016; 41(3): 321-7.
- Rasouli M R, Viscusi E R. Adductor canal block for knee surgeries: an emerging analgesic technique. Arch Bone Jt Surg 2017; 5(3): 131-2.
- Chaumeron A, Audy D, Drolet P, Lavigne M, Vendittoli P A. Periarticular injection in knee arthroplasty improves quadriceps function. Clin Orthop Rel Res 2013; 471(7): 2284-95.
- Grosso M J, Murtaugh T, Lakra A, Brown A R, Maniker R B, Cooper H J, et al. Adductor canal block compared with periarticular bupivacaine injection for total knee arthroplasty: a prospective randomized trial. J Bone Joint Surg (Am) 2018; 100(13): 1141-6.
- Gwam C U, Mistry J B, Khlopas A, Chughtai M, Thomas M, Mont M A, et al. Does addition of multimodal periarticular analgesia to adductor canal block improve lengths of stay, pain, discharge status, and opioid use after total knee arthroplasty? J Arthroplasty 2017; 32(5): 1470-3.
- Ma J, Gao F, Sun W, Guo W, Li Z, Wang W. Combined adductor canal block with periarticular infiltration versus periarticular infiltration for analgesia after total knee arthroplasty. Medicine 2016; 95(52): e5701.
- Nader A, Kendall M C, Manning D W, Beal M, Rahangdale R, Dekker R, et al. Single-dose adductor canal block with local infiltrative analgesia compared with local infiltrate analgesia after total knee arthroplasty: a randomized, double-blind, placebo-controlled trial. Reg Anesth Pain Med 2016; 41(6): 678-84.
- Sawhney M, Mehdian H, Kashin B, Ip G, Bent M, Choy J, et al. Pain after unilateral total knee arthroplasty: a prospective randomized controlled trial examining the analgesic effectiveness of a combined adductor canal peripheral nerve block with periarticular infiltration versus adductor canal nerve block alone versus periarticularinfiltration alone. Anesth Analg 2016; 122(6): 2040-6.
- Kertkiatkachorn W, Kampitak W, Tanavalee A, Ngarmukos S. Adductor canal block combined with iPACK (interspace between the popliteal artery and the capsule of the posterior knee) block vs periarticular injection for analgesia after total knee arthroplasty: a randomized noninferiority trial. J Arthroplasty 2021; 36(1): 122-9.e1.
- Cullom C, Weed J T. Anesthetic and analgesic management for outpatient knee arthroplasty. Curr Pain Headache Rep 2017; 21(5): 23.
- Sankineani S R, Reddy A R C, Eachempati K K, Jangale A, Guava Reddy A V. Comparison of adductor canal block and IPACK block (interspace between the popliteal artery and the capsule of the posterior knee) with adductor canal block alone after total knee arthroplasty: a prospective control trial on pain and knee function in immediate post-operative period. Eur J Orthop Surg Traumatol 2018; 28(7): 1391-5.
- Kim D H, Beathe J C, Lin Y, YaDeau J T, Maalouf D B, Goytizolo E, et al. Addition of infiltration between the popliteal artery and the capsule of the posterior knee and adductor canal block to periarticular injection enhances postoperative pain control in total knee arthroplasty: a randomized controlled trial. Anesth Analg 2019; 129(2): 526-35.
- Kandarian B, Intelli P F, Sinha S, Hunter O O, Wang R R, Kim T E, et al. Implementation of the IPACK (infiltration between the popliteal artery and capsule of the knee) block into a multimodal analgesic pathway for total knee replacement. Korean J Anesthesiol 2019; 72(3): 238-44.
- Bahreini M, Jalili M, Moradi-Lakeh M. A comparison of three self-report pain scales in adults with acute pain. J Emerg Med 2015; 48(1): 10-8.
- Danoff J R, Goel R, Sutton R, Maltenfort M G, Austin M S. How much pain is significant? Defining the minimal clinically important difference for the visual analog scale for pain after total joint arthroplasty. J Arthroplasty 2018; 33(7s): S71-S5.e2.
- Patterson M E, Vitter J, Bland K, Nossaman B D, Thomas L C, Chimento G F. The effect of the IPACK block on pain after primary TKA: a double-blinded, prospective, randomized trial. J Arthroplasty 2020; 35(6s): S173-s7.
- Niesen A D, Harris D J, Johnson C S, Strike D E, Smith H M, Jacob A K, et al. Interspace between popliteal artery and posterior capsule of the knee (IPACK) injectate spread: a cadaver study. J Ultrasound Med 2019; 38(3): 741-5.
- Tran J, Peng P W H, Gofeld M, Chan V, Agur A M R. Anatomical study of the innervation of posterior knee joint capsule: implication for image-guided intervention. Reg Anesth Pain Med 2019; 44(2): 234-8.