Impact of the Nordic Arthroplasty Register Association (NARA) collaboration on demographics, methods and revision rates in knee arthroplasty: a register-based study from NARA 2000–2017
Tero IRMOLA 1, Ville PONKILAINEN 2, Keijo T MÄKELÄ 3,4, Otto ROBERTSSON 5, Annette W-DAHL 5, Ove FURNES 6,7, Anne M FENSTAD 6, Alma B PEDERSEN 8, Henrik M SCHRØDER 9, Mika J NIEMELÄINEN 1, and Antti ESKELINEN 1
1 Coxa Hospital for Joint Replacement, and Faculty of Medicine and Health Technologies, University of Tampere, Tampere, Finland; 2 Department of Orthopaedics and Traumatology, Central Finland Hospital Nova, Jyväskylä, Finland; 3 Finnish Arthroplasty Register, National Institute for Health and Welfare, Helsinki, Finland; 4 Department of Orthopaedics and Traumatology, Turku University Hospital, and University of Turku, Turku, Finland; 5 The Swedish Knee Arthroplasty Register, Department of Orthopedics, Skane University Hospital, Lund, Sweden, and Department of Clinical Sciences, Orthopedics, Lund University, Sweden; 6 The Norwegian Arthroplasty Register, Department of Orthopaedic Surgery, Haukeland University Hospital, Bergen, Norway; 7 Department of Clinical Medicine, University of Bergen, Bergen, Norway; 8 Department of Clinical Epidemiology, Aarhus University Hospital, Denmark, and the Danish Knee Arthroplasty Registry; 9 Department of Orthopaedic Surgery, Naestved Hospital, Denmark, and the Danish Knee Arthroplasty Register
Background and purpose — We have previously observed differences in treatment and outcome of knee arthroplasties in the Nordic countries. To evaluate the impact of Nordic collaboration in the last 15 years we aimed to compare patient demographics, methods, and revision rates in primary knee arthroplasties among the 4 Nordic countries.
Patients and methods — We included 535,051 primary knee arthroplasties reported 2000–2017 from the Nordic Arthroplasty Register Association (NARA) database. Kaplan–Meier analysis (KM) and restricted mean survival time (RMST) analysis were used to evaluate the cumulative revision rate (CRR) and RMST estimates with 95% confidence intervals (CI) and to compare countries in relation to risk of revision for any reason.
Results — After 2010, the increase in incidence of knee arthroplasty plateaued in Sweden and Denmark but continued to increase in Finland and Norway. In 2017 the incidence was highest in Finland with 226 per 105 person-years, while it was less than 150 per 105 in the 3 other Nordic countries. In total knee arthroplasties performed for osteoarthritis (OA), overall CRR at 15 years for revision due to any reason was higher in Denmark (CRR 9.6%, 95% CI 9.2−10), Norway (CRR 9.1%, CI 8.7−9.5), and Finland (CRR 7.0%, CI 6.8−7.3) compared with Sweden (CRR 6.6%, CI 6.4−6.8). There were differences among the countries in use of implant brand and type, fixation, patellar component, and use of unicompartmental knee arthroplasty.
Interpretation — We evinced a slowing growth of incidence of knee arthroplasties in the Nordic countries after 2010 with Finland having the highest incidence. We also noted substantial differences among the 4 Nordic countries, with Sweden having a lower risk of revision than the other countries. No impact of NARA could be demonstrated and CRR did not improve over time.
Citation: Acta Orthopaedica 2022; 93: 866–873. DOI http://dx.doi.org/10.2340/17453674.2022.5256.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-05-03. Accepted: 2022-10-11. Published: 2022-11-28.
Correspondence: tero.irmola@coxa.fi
Design and drafting of the work: AE, MN, TI, VP. Final approval of the version to be published and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: TI, VP, KM, OR, AW-D, OF, AF, AP, HS, AE, MN.
Handling co-editor: Søren Overgaard and Philippe Wagner
Acta thanks Anders El-Galaly and Brian Hallstrom for help with peer review of this study.
A pilot study based on the Nordic Arthroplasty Register Association (NARA) knee database (1997–2007) demonstrated a continuous increase in the incidence of knee arthroplasty, but also marked differences in fixation methods, implant brands, the use of patellar buttons, total knee arthroplasties (TKA) and unicompartmental knee arthroplasties (UKA), and risk of revision after knee arthroplasty in the Nordic countries (1).
The incidence of knee arthroplasties is rising, but not at the rate previously predicted (2,3). In addition, differences in TKA patient demographics and clinical outcomes exist internationally (4). In the Nordic countries, the lifetime risk of TKA for osteoarthritis (OA) increased from 2003 until 2013, with the highest rate for women in Finland (22.8%) and lowest in Norway (9.7%) (5).
The present study is an update on a study from 2010 (1), with longer follow-up and with the addition of Finland to the 3 previously studied Nordic countries. The aim of our study was to compare patient demographics, incidences, methods, fixation concepts, implant brands, and risk of revision in primary knee arthroplasties among the 4 Nordic countries based on the collaboration and the NARA database.
Patients and methods
Data sources
The data was obtained from the NARA common knee database. All primary knee arthroplasties recorded between January 1, 2000 and December 31, 2017 were included. The NARA gathers data from 4 Nordic countries and datasets include only variables that all countries can deliver (minimal dataset), currently including 20 variables (6). The present study was collaborated by the Swedish Knee Arthroplasty Register (SKAR), the Danish Knee Arthroplasty Register (DKR), the Norwegian Arthroplasty Register (NAR), and the Finnish Arthroplasty Register (FAR). All registers use individual-based registration of operations. The selection and transformation of the particular datasets and de-identification of the patients were performed within each national register. The de-identified data was then pooled into a common database. Data was treated with full confidentiality, according to the rules of each country respectively.
The quality of data in the Nordic registers is high, including both 100% coverage of hospitals and the following completeness of patients for primary knee arthroplasties: SKAR 97%, DKR 97%, NAR 97%, FAR 96% and for revision knee arthroplasties: SKAR > 95% (estimate, OR, personal communication), DKR 94%, NAR 93%, FAR 80% (7-10). Coverage refers to the proportion of those hospitals (of all hospitals performing TKAs) that deliver data into national registers. The completeness is overall for the entire study period and refers to the proportion of operations (of all primary/revision TKAs) that have been recorded in the national arthroplasty register. The study follows the RECORD and STROBE guidelines (11,12).
Outcome
The incidence of knee arthroplasties per 105 person-years was calculated for each country using the country-specific population information available. Revision performed for any reason was the endpoint in the revision analyses, with revision being defined as exchange, removal, or addition of one or more prosthetic components. The fixation methods of knee arthroplasties were divided into 4 groups: cemented, uncemented, hybrid (uncemented femur with cemented tibia), and inverse hybrid (cemented femur with uncemented tibia). Age was divided into age groups younger than 45 years, and groups of 10 years until aged 85 years and older. TKA, UKA, and patellofemoral arthroplasty (PFA) were evaluated as well as level of prosthetic constraint. Standard implants, minimally stabilized cruciateretaining (CR) and posterior stabilized (PS) were analyzed separately and fully stabilized constrained condylar knee (CCK) and rotating-type hinge knee (RHK) separately.
NARA
The NARA was founded in 2007 to produce and analyze a combined dataset from the knee and hip arthroplasty databases in Denmark (DK), Norway (NO), and Sweden (SE). In 2010, Finland (FI) also joined this collaboration. The NARA collaboration among the Nordic registers and national research units facilitates gathering national datasets together and provides a higher quality of the analyses performed. Improved quality of research could enhance the possibility of quality improvements for knee arthroplasty. The NARA is organized in collaboration with Nordic registers and representatives from each member country have annually face-to-face meetings, regular teleconferences, and web meetings (6).
Statistics
Descriptive statistics were presented as numbers with percentage, as mean with standard deviation (SD), or as median with interquartile range (IQR) based on the distribution. Incidences were calculated for each corresponding country using the total annual population obtained from the national official statistics websites from each country (www.dst.dk, www.ssb.no, www.scb.se, www.stat.fi). The population was obtained from the last day of the year, except for Denmark, for which the population was from the first day of the year.
Kaplan–Meier (KM) survival analysis was used to assess implant cumulative revision rate (CRR) with 95% confidence intervals (CI). Curves were cut off when 40 knees remained at risk. When comparing the risk of revision among countries, a Cox regression model resulted in serious violations of the proportional hazards assumption, and thus restricted mean survival time (RMST) analysis was used. The results of the analysis were interpreted as restricted mean survival time at 10-year time point with 95% CI. The 10-year time point was chosen as it was the last time point to contain at least 10% of all included patients in each model. The model was adjusted by relevant covariates (either shown in the previous studies or hypothesized by the authors and selected by using directed acyclic graphs [DAGs]) to control for confounding and to estimate the total effect of country on revision risk. Covariates included in the analysis were sex and age at surgery (Figure 1, see Supplementary data). Age was included as a continuous variable. CRRs were also assessed separately for 2 time periods: 2000 to 2007 (early) and 2008 to 2017 (late), to evaluate the possible effect of the NARA collaboration on country-wise results. Statistical analyses were performed using R 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria).
Ethics, funding, data sharing, and disclosures
The ethical approval process of each national register granted formal approval for the study. Permission numbers from each country were: the Danish Data protection agency (1-16-02-54-17), Denmark, the National Institute of Health and Welfare (Dnro THL/1743/.5.05.00/2014), Finland, the Norwegian Data Inspectorate (ref 24.1.2017: 16/01622-3/CDG), Norway and the Ethics Board of Lund University (LU20-02), Sweden. This work was supported by the competitive research funds of Pirkanmaa Hospital District, Tampere, Finland, representing governmental funding. The authors have no conflicts of interests to declare. The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Results
535,051 primary knee arthroplasties were reported in the 4 Nordic countries in the study period (2000−2017) (Table 1).
Between 2000 and 2009, the incidence of knee arthroplasty increased in all 4 countries, but most dominantly in DK (Figure 2). Since 2009, the increase in incidence plateaued in SE and in DK, while it continued to increase in FI (especially from 2014 onwards) and in NO (Figure 2). At the end of our study, the incidence was highest in FI (226 per 105) and lowest in NO (125 per 105) (Figure 2).
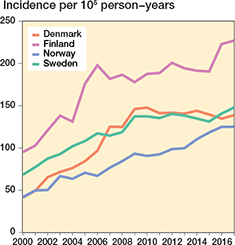
Figure 2. Overall incidence of primary knee arthroplasties.
In all 4 countries, the proportion of patients aged 55−64 years increased slightly over the study period. The proportion of patients 75 years and older decreased slightly. The age group 65−74 years remained the largest in all Nordic countries throughout the study period (Figure 3).
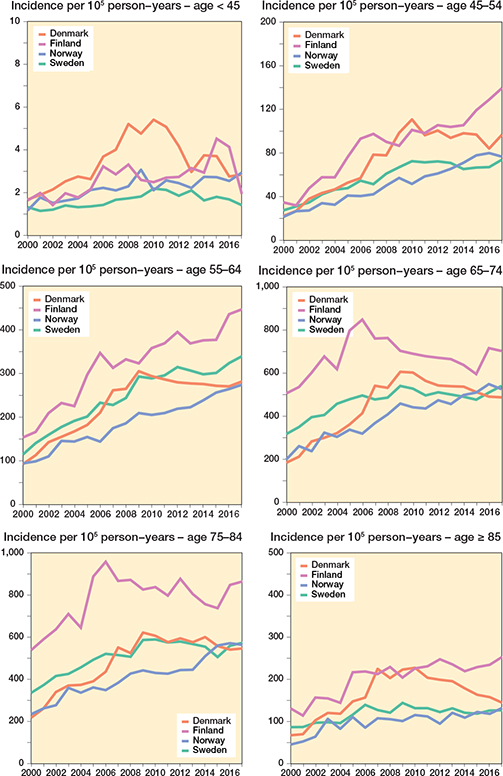
Figure 3. Incidence in different age groups in primary knee arthroplasty.
62% of the operations were in women, with the highest proportion found in FI (Table 1). The proportion of women was highest for isolated PFA (74%) (Table 1). The mean age at surgery was higher for TKA than for UKA and PFA (Table 1). OA was the indication for surgery in 91% of all cases. The incidence of arthroplasty for rheumatoid arthritis (RA) decreased during the period in all 4 countries (Figure 4).
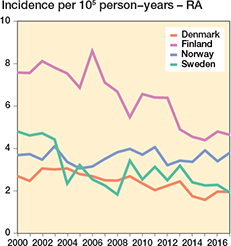
Figure 4. Incidence of knee arthroplasty for rheumatoid arthritis.
In the study period, a vast majority (92%) of the arthroplasties were TKAs (Table 1 and Figure 5). Increasing usage of UKA was noted in DK and in NO and recently also in SE (Table 1 and Figure 5). PFA was uncommon, accounting for only 0.3% of all the primary arthroplasties; the highest proportion was in NO (0.6%) and DK (0.5 %) (Table 1 and Figure 5).
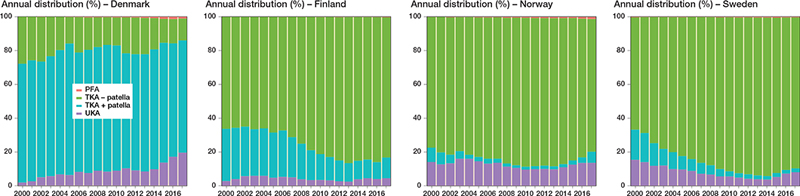
Figure 5. Proportion of arthroplasty types used for primary knee arthroplasty.
The use of patellar resurfacing in TKA was most common in DK (79%) but only used in 4%, 6%, and 19% of the TKAs in NO, SE, and FI, respectively (Table 1). A slight increase in patellar resurfacing was seen in NO and a decrease in FI (Table 1 and Figure 5).
In TKA, cement was used as fixation for both the tibial and femoral components in 74–98% of cases, least often in DK and most often in FI (Table 1). Uncemented and hybrid fixation were more common in DK and NO than in FI and SE (Table 1). In UKA, uncemented fixation was used more often in FI (30%) and DK (27%) than in SE (11%) and NO (6%) (Table 1).
In TKAs, cruciate retaining (CR) designs including mobile bearing implants clearly dominated in all 4 countries with the proportion ranging from 87% to 98% of all TKAs. The posterior stabilized (PS) knees were most steadily used in DK and less frequently in SE and NO (Table 1). The most frequently used TKA designs were NexGen, PFC, and Triathlon (Table 2). In UKAs, the Oxford implant accounted for 98%, 91%, and 88% UKAs in FI, NO, and DK, respectively, while it accounted for only 35% in SE (Table 3).
Including all TKA models performed for primary OA, the overall CRR at 15 years was higher in DK 9.6% (CI 9.2−10) and in NO 9.1% (CI 8.7−9.5) than in FI 7% (CI 6.8−7.3) and SE 6.6% (CI 6.4−6.8), respectively (Figure 6). Using RMST analysis and adjusting for differences in age and sex, the RMST at 10 years was lower in DK 9.52 (CI 9.50−9.53), NO 9.54 (CI 9.52−9.55), and FI 9.65 (Cl 9.65−9.66) compared with SE 9.69 (Cl 9.68−9.70).
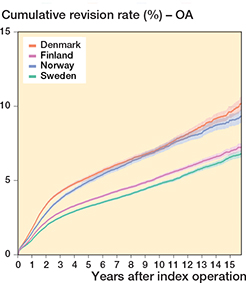
Figure 6. Cumulative revision rate (CRR = lines) with 95% CI (colored areas) after total knee arthroplasty performed for osteoarthritis.
The same tendency was also seen in the 2 time periods assessed (2000–2007 and 2008–2017). The overall CRRs for total knee arthroplasties among Nordic countries remained at the same level in both periods (Figure 7).
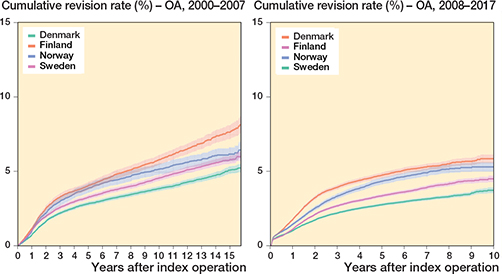
Figure 7. Cumulative revision rates (CRR = lines) with 95% CI (colored areas) in 2000–2007 and 2008–2017 after total knee arthroplasty performed for osteoarthritis.
Regarding UKAs performed for OA, the CRR at 15 years was comparable between FI (26%, CI 24−28), NO (24%, CI 22−25) and DK (23%, CI 20−26), while the CRR were lowest in SE (19%, CI 18−20) (Figure 8). The corresponding RMSTs at 10 years were 9.17 (CI 9.13−9.21) in SE, 8.98 (CI 8.92−9.04) in NO, 8.99 (CI 8.92−9.05) in FI, and 9.00 (CI 8.93−9.06) in DK.
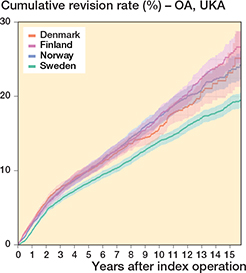
Figure 8. Cumulative revision rate (CRR = lines) with 95% CI (colored areas) after unicompartmental knee arthroplasty for osteoarthritis.
When only the Oxford UKA was examined, the CRR at 15 years followed a similar trend in the 4 countries, being highest in FI (26%, CI 25−28), followed by SE (24%, CI 21−27) and NO (23%, CI 21−25), and was lowest in DK (23%, Cl 20−25) (Figure 9). In addition, there was no difference in RMST, which at 10 years was 9.17 (CI 9.09−9.25) in SE, 8.98 (CI 8.92−9.04) in NO, 8.98 (CI 8.92−9.05) in FI, and 9.00 (CI 8.93−9.06) in DK.
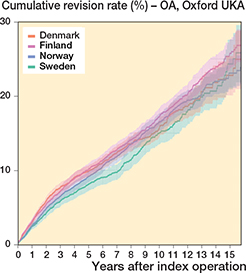
Figure 9. Cumulative revision rate (CRR = lines) with 95% CI (colored areas) for the Oxford unicompartmental implant in patients with primary osteoarthritis
Discussion
We found differences among the 4 Nordic countries in incidence of knee arthroplasty, in use of TKA and UKA, in use of patellar resurfacing, in preferences in implant brands, and also in cumulative revision rates. Even though usage of uncemented and hybrid fixation in TKAs has slightly increased in the study period, cemented TKA still comprised over 83% of all primary TKAs in the Nordic countries. At the beginning of our study, fixations other than cemented TKAs were uncommonly used, but especially in NO and DK a clear increase was noted in the study period. Uncemented fixation in UKAs was used more often in FI and DK. Use of patellar resurfacing in TKA was common and still increasing in DK. Overall, CRR was lowest in Sweden. Preferences in implant brands clearly differed and the revision rates of the contemporary knee designs were low.
There was a continuous increase in the overall incidence of primary knee arthroplasty in 3 of the Nordic countries, the exception being DK. In FI, 2 peaks in 2004 and 2015 are due to legislation, first in 2003 the patient’s right to access specialized medical care within 6 months and second in 2015 the patient’s right to choose freely a specialized medical care provider. In the pilot study (1997−2007), the incidence of TKAs was higher in SE than in DK and NO at the beginning, but the incidences increased in all countries and became higher in DK at the end of the study period (1). Possible reasons for this phenomenon—which have also been reported from other countries—are the increase in the prevalence of symptoms related to knee OA, patients wanting surgical treatment of knee OA even with milder symptoms, access to knee arthroplasty surgery, increased life expectancy, and increased community obesity, which all are slightly confusingly linked with the results of our study (13). The higher incidence of knee arthroplasties in FI may be associated with local patient preferences for surgery, with registry research suggesting that Finnish baby boomers may already opt to undergo knee arthroplasty when their OA symptoms are still relatively mild (14). Access to surgery is not a clear reason either and the waiting times for knee arthroplasty in DK were the lowest among the OECD countries in 2017. The other Nordic countries had longer waiting times, in order, from SE, to FI, to NO (2). In all Nordic countries increased life expectancy at birth was above an average across OECD countries, and it was highest in NO followed by SE, FI, and DK. So, neither access to surgery nor increased life expectancy can lighten the differences among Nordic countries in the incidence of knee arthroplasties. The proportion of overweight adults in 2017 was above average among OECD countries for both sexes only in FI, with 67.6 % of adults being overweight or obese. Also, the proportion of population aged 65 years or older and 80 years or older was above average only in FI, but, besides that, the share of adults aged 65 and above receiving long-term care among the Nordic countries was lowest in FI (2). This could be among other reasons for the substantially higher incidence of knee arthroplasties in FI than in the other Nordic countries.
According to our study, with deceleration in the incidence of knee arthroplasties between the 2 decades in all Nordic countries, the knee arthroplasty incidence is probably not increasing as rapidly as projected (7-10,15). In 2017, the incidence of primary knee arthroplasties per 105 inhabitants was 131 in Sweden, 187 in Kaiser Permanente Joint Replacement Registry (KPJRR) in the United States, and 240 in Australia, and over a 15-year period the incidence had increased in those 3 populations by 79%, 258%, and 102%, respectively (16). Variation in rates of knee arthroplasties among countries may be due to local indications for surgery, local economic concerns and health policy, differences in rates of OA, availability of pre-surgical treatments for OA, and access to TKA, as well as number and distribution of orthopedic surgeons and variation in thresholds for suitability for operative treatment (5,16). In our study, the rate of increase in the incidence of knee arthroplasties has slowed down in 3 of the Nordic countries, and the incidence has actually decreased slightly in DK. The incidence of primary knee arthroplasties per 105 Danes is estimated to plateau within the next 10–15 years with an expected maximal annual incidence between 250 and 260, and the authors thought that might in part be due to the tax-paid healthcare system (17). The number of TKAs implanted per year was also reported to be stabilizing according to the annual report in 2020 of the New Zealand Joint Registry (18).
The mean age at surgery remained rather steady compared with the NARA knee pilot study (1): for TKA it was 69 years and before 70 years, for UKA 64 and 66 years, and for PFA 57 and 60 years. As in the pilot study, the proportion of females remained higher in NO than in DK and SE, but the highest proportion was now seen in FI, which was not included in the pilot study (1). Obesity among Finnish women may partly be behind this phenomenon. OA still is the main indication for knee arthroplasty. For RA, the number of surgeries was relatively unchanged in DK, as it already was in the pilot study (1). The larger reduction in SE and in FI is unclear. As in the pilot study possible reasons were a change in disease pattern, a change in prevalence, differences in treatment with immunosuppressive and/or biologic drugs, or the longer history of knee arthroplasty in SE (1).
A vast majority of the operations were TKA as in the pilot study (1). The proportion of UKAs increased in DK and in NO and recently also in SE, which was noted already in DK and in NO in the pilot study, while it decreased in SE (1). The influence of marketing of the Oxford brand might have some role in the increasing use of UKAs. UKAs were performed least often in FI, but almost exclusively using the Oxford knee.
Patellar resurfacing was most commonly performed in DK. Difference in the use of patellar resurfacing in DK compared with other Nordic countries might be explained by clinical practices that were derived from historical methods. The same difference was already noted in the pilot study (1). Patellar resurfacing has been reported to reduce the risk of revision, especially in PS knee designs (19). Still, the use of patellar resurfacing remained at the same level in DK despite the decreasing use of PS models there. The decrease in the use of patellar resurfacing was noted in FI, while a slight increase was seen in NO. Also, in the USA, surgeons continue to resurface the patella in over 80% of primary TKAs (20). In our study, the lowest rates of patellar resurfacing were seen in NO and in SE. In Australia, there has been an upward trend in the use of patellar resurfacing with 72% being resurfaced in 2019 (21,22).
Among TKAs, CR designs, including mobile bearing knees (as they could not be distinguished from CR knees), were most used, and most of them with cemented fixation (74–98%). The NARA knee pilot study revealed that cement was used to fix both the tibial and femoral component in 78–98% but did not report the level of constraint of TKAs (1).
NO had a quite different preference in TKA brands with 2 of the 3 the most popular TKA designs (LCS mobile bearing and Profix) being used infrequently in the other Nordic countries. NO was already different in the pilot study regarding the choice of TKA designs (1). A recent NO study showed that a knee prosthesis with a rotating platform (mobile bearing) had a higher risk both for any revision and for aseptic loosening (23).
The CRR at 15 years was highest in DK (9.6%), and lowest in SE (6.6%) and the RMST at 10 years was in DK 9.52 and in SE 9.69, which is in line with the findings in the pilot study (1). When comparing the study period before the NARA was founded (early, 2000–2007) and after establishment of NARA (late, 2008–2017), we found that the CRRs did not improve. Further, the differences between the individual countries that could be seen in the early period also remained rather consistent during the late period. Thus, harmonization efforts of the registers within NARA have not resulted in harmonization of results among the countries. Future studies will show whether such an effect can be seen in the longer term. The 15-year CRR in primary TKAs was 6.4% (6.2–6.5) in the NJR annual report in 2020 and ranged from 4.0% to 15.6% among implant designs in the AOANJRR annual report in 2020 (21,24). Evans et al. (2019) estimated that 82.3% of TKAs last 25 years, using pooled registry data from 14 registers (25). In the pilot study it was assumed that indications for primary arthroplasties and revisions differed among countries. Differences in completeness of reporting had some influence and the fact that knee arthroplasty became common in SE earlier than in DK and NO might indicated that there was a learning curve effect involved, but considering the CRR in FI these may not be the only explanations. Identically to the pilot study, the revision rate after TKA was lowest in SE, both when analyzing all implants and when analyzing the 3 implants commonly used in all countries.
In UKA, the CRR (23−26%) at 15 years was comparable to Australia, where the cumulative percentage revision (CPR) for primary UKA for OA was 14% at 10 years and 30% at 19 years (17). The NJR reported 15-year revision rates for cemented UKA (18%) and cementless or hybrid UKA (14%) (24). The CRR for UKAs was more than 3 times that of the CRR for TKAs.
We acknowledge certain strengths and limitations in our study. The major strength of our study is the NARA database covering a high number of knee arthroplasties (populationlevel data) combined with high completeness of reporting for primary knee arthroplasties among Nordic registers. Even if the base of population and healthcare systems include several similarities among the Nordic countries, clear differences were found in this multinational study setting. That the NARA collaboration should influence the surgery in our 4 countries may not be the purpose of NARA, which is, rather, to harmonize the national registers, and it could also affect joint arthroplasty in terms of patients, implant choices, and the revision rates. When comparing the pilot study and 2 consecutive 10-year periods it seems the revision rates were not influenced. There are a few limitations in the current study. First, completeness was lower in all countries for revisions compared with primary surgeries, also 20 years ago compared with the last 10 years. We agree and acknowledge variation in completeness over time and among countries and that differences in completeness affect revision rates. The completeness of revision TKA is lower in FAR than in the other Nordic registries. In Finland, 20% of revisions are missing from the FAR database when compared with the National Patient Discharge Register. This lower revision completeness affects accuracy and reduces the number of revision cases available for analysis. Second, we could not consider polyethylene insert design in analyses, which may have an impact on results, especially for rotating platform TKAs. Third, the patient-reported outcome measures (PROMs) are not yet routinely collected for knee replacements in the Nordic registers.
Regarding the clinical relevance of our results, our study serves as a large-scale benchmarking assessment of outcomes of primary knee arthroplasties in the Nordic countries. It seems that despite the differences in methods and implants used in knee arthroplasty, the overall outcomes, in terms of cumulative revision rates, were good in all 4 Nordic countries. On the other hand, our results indicate that there is still room for further improvement. It is important to continue benchmarking and look for the best practices across countries to further improve the outcomes of primary knee arthroplasty.
To conclude, the incidence of primary knee arthroplasties in the Nordic countries is increasing; however, the previous rapid rate of increase has slowed. Use of patellar resurfacing was more common in Denmark and increasing use of uncemented and hybrid fixation was noted in Denmark and Norway. Preferences in implant designs differed in Norway compared with the other Nordic countries. The CRRs of primary TKAs and UKAs were lowest in Sweden.
- Robertsson O, Bizjajeva S, Fenstad A M, Furnes O, Lidgren L, Mehnert F, et al. Knee arthroplasty in Denmark, Norway and Sweden. Acta Orthop 2010; 81 (1): 82-9. doi: 10.3109/17453671003685442.
- OECD. Health at a glance 2019. doi: 10.1787/4dd50c09-en, Stat-Links https://doi.org/10.1787/888934015942, https://doi.org/10.1787/888934014821, https://doi.org/10.1787/888934015467, https://doi.org/10.1787/888934018260, https://doi.org/10.1787/888934018564.
- Lewis P L, Graves S E, de Steiger R N, Campbell D G, Peng Y, Hatton A, et al. Does knee prosthesis survivorship improve when implant designs change? Findings from the Australian Orthopaedic Association National Joint Replacement Registry. Clin Orthop Relat Res 2020; 478 (6): 1156-72. doi: 10.1097/CORR.0000000000001229.
- Sauder N, Galea V P, Rojanasopondist P, Colon Iban Y E, Florissi I S, Nielsen C S, et al. Regional differences between the US, Scandinavia, and South Korea in patient demographics and patient-reported outcomes for primary total knee arthroplasty. Arch Orthop Trauma Surg 2020; 140 (1): 93-108. doi: 10.1007/s00402-019-03286-5.
- Ackerman I N, Bohensky M A, de Steiger R, Brand C A, Eskelinen A, Fenstad A M, et al. Substantial rise in the lifetime risk of primary total knee replacement surgery for osteoarthritis from 2003–2013: an international, population-level analysis. Osteoarthritis Cartilage 2017; 25 (4): 455-61. doi: 10.1016/j.joca.2016.11.005.
- Mäkelä K T, Furnes O, Hallan G, Fenstad A M, Rolfson O, Kärrholm J, et al. The benefits of collaboration: the Nordic Arthroplasty Register Association. Effort Open Rev 2019; 4 (6): 391-400. doi: 10.1302/2058-5241.4.180058.
- NAR. Norwegian Arthroplasty Register, annual report; 2021. Available from: https://helse-bergen.no/nrl/
- SKAR. Swedish Knee Arthroplasty Register, annual report; 2019 Available from: https://myknee.se
- DKR. Dansk knealloplastikregister, årsrapport; 2019. Available from: https://sundhed.dk
- FAR. Finnish Arthroplasty Register. Available from: https://www.thl.fi/far (last accessed April 24, 2020).
- Benchimol E I, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, et al. The reporting of studies conducted using observational routinely-collected health data (RECORD) statement. PLoS Med 2015; 12 (10): e1001885. doi: 10.1371/journal.pmed.1001885.
- von Elm E, Altman D G, Egger M, Pocock S J, Gøtzsche P C, Vandenbroucke J P; STROBE Initiative. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology 2007; 18 (6): 800-4.
- Hamilton D F, Howie C R, Burnett R, Simpson A H R W, Patton J T. Dealing with the predicted increase in demand for revision total knee arthroplasty: challenges, risks and opportunities. Bone Joint J 2015; 97-B: 723-8. doi: 10.1302/0301-620X.97B6.35185.
- Leskinen J, Eskelinen A, Huhtala H, Paavolainen P, Remes V. The incidence of knee arthroplasty for primary osteoarthritis grows rapidly among baby boomers: a population-based study in Finland. Arthritis Rheum 2012; 64(2): 423-8. doi: 10.1002/art.33367.
- Niemeläinen M J, Mäkelä K T, Robertsson O, W-Dahl A, Furnes O, Fenstad A M, et al. Different incidences of knee arthroplasty in the Nordic countries. Acta Orthop 2017; 88(2): 173-8. doi: 10.1080/17453674.2016.1275200.
- Lewis P L, Graves S E, Robertsson O, Sundberg M, Paxton E W, Prentice H A, et al. Increases in the rates of primary and revision knee replacement are reducing: a 15-year registry study across 3 continents. Acta Orthop 2020; 91(4): 414-19. doi: 10.1080/17453674.2020.1749380.
- Daugberg L, Jakobsen T, Nielsen P T, Rasmussen M, El-Galaly A. A projection of primary knee replacement in Denmark from 2020 to 2050. Acta Orthop 2021; 92(4): 448-451. doi: 10.1080/17453674.2021.1894787.
- NZJR. The New Zealand Joint Registry twenty-one year report; 2020. Available from: https://nzoa.org.nz.
- Comfort T, Baste V, Froufe M A, Namba R, Bordini B, Robertsson O, et al. International comparative evaluation of fixed-bearing non-posterior-stabilized and posterior-stabilized total knee replacements. J Bone Joint Surg Am 2014; 96 (Suppl. 1): 65-72. doi: 10.2106/JBJS.N.00462.
- Fraser J F, Spangehl M J. International rates of patellar resurfacing in primary total knee arthroplasty, 2004–2014. J Arthroplasty 2017; 32: 83-6. doi: 10.1016/j.arth.2016.06.0100.
- AOANJRR. Australian Orthopaedic Association National Joint Replacement Registry, hip, knee & shoulder arthroplasty. 21st annual report; 2020. Available from: https://aoanjrr.sahmri.com.
- NICE. National Institute for Health and Care Excellence .Joint replacement (primary): Hip, knee and shoulder. [L] Evidence review for patella resurfacing. NICE guideline NG157. Intervention evidence review underpinning recommendation 1.7.2 and the research recommendation in the NICE guideline; 2020. Available from: https://www.nice.org.uk/guidance/ng157.
- Gothesen O, Lygre S H L, Lorimer M, Graves S, Furnes O. Increased risk of aseptic loosening for 43,525 rotating-platform vs. fixed-bearing total knee replacements. Acta Orthop 2017; 88(6): 649-56. doi: 10.1080/17453674.2017.1378533.
- NJR. National Joint Registry for England, Wales, Northern Ireland, the Isle of Man and Guernsey, 17th annual report; 2020. Available from: https://reports.njrcentre.org.uk.
- Evans J T, Walker R W, Evans J P, Blom A W, Sayers A, Whitehouse M R. How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet 2019; 393 (10172): 655-63. doi: 10.1016/S0140-6736(18)31665-9.
Supplementary data
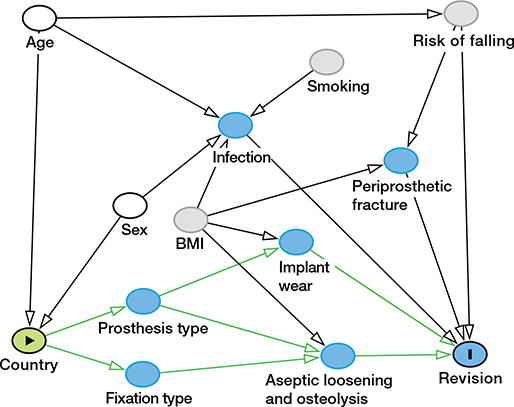
Figure 1. The directed acyclic graph: BMI, body mass index. Measurable (white) factors were included in the multivariable model.