Projection of primary and revision hip arthroplasty surgery in Denmark from 2020 to 2050
Mathias B RASMUSSEN 1, Anders EL-GALALY 1, Louise DAUGBERG 1,2, Poul T NIELSEN 1, and Thomas JAKOBSEN 1,2
1 Interdisciplinary Orthopedics, Aalborg University Hospital , Aalborg; 2 Department of Clinical Medicine, Aalborg University, Aalborg, Denmark
Background and purpose — The incidence of primary and revision total hip arthroplasty (THA) has increased over the last decades. Previous forecasts from different healthcare systems have predicted a continuous increase. We present a forecast of both primary and revision surgery from 2020 to 2050 based on 25 years data from the healthcare system in Denmark.
Patients and methods — We retrieved data from the Danish Hip Arthroplasty Register on 198,835 primary and 29,456 revision surgeries. Historical censuses and population forecasts were retrieved from Statistics Denmark. Logistic and Gompertz regression analysis was used to forecast incidence rates (IR) and total numbers in the next 30 years.
Results — Our forecast predicts an increase in IR of 3–9% and an increase in total numbers of primary THA of between 12% and 19% in 2050. For revision THA the IRs have reached a plateau but total numbers are predicted to increase by 19% in 2050.
Conclusion — Our forecast shows that both primary and revision THA will increase in total numbers in the next decades, but the IR for primary THA is near its plateau and for revision THA the plateau has already been reached. The forecast may aid in healthcare resource planning for the decades to come.
Citation: Acta Orthopaedica 2022; 93: 849–853. DOI http://dx.doi.org/10.2340/17453674.2022.5255.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-03-02. Accepted: 2022-09-29. Published: 2022-11-22.
Correspondence: Mathias.rasmussen@rn.dk
All authors were involved in planning the study. MBR, LD, and AEG retrieved and analyzed the data. MBR wrote the manuscript, and all authors revised and accepted the final manuscript before submission.
Handling co-editors: Bart Swierstra and Jonas Ranstam
Acta thanks Szilard Nemes and Marieke Ostendorf for help with peer review of this study.
There has been an increase in the incidence of total hip arthroplasty (THA) within the Scandinavian countries, and in Denmark, with an estimated population of 5.8 million (1), 10,413 primary THA surgeries and 1,225 revision surgeries were performed in 2018 according to the annual report from the Danish Hip Arthroplasty Register. Studies from Germany (2), the United Kingdom (3), Australia (4), and Sweden (5) have reported an increase historically, and projected a future increase in both incidence rate (IR) and total numbers. This would also be expected to cause an increase in revision surgery.
An expected increase in both primary surgeries and revision surgeries will require more resources in healthcare. Reliable mid- and long-term forecasts for the annual number of primary and revision procedures is important for political and clinical decision-makers in order to allocate sufficient economical and surgical resources. The latest study covering Danish conditions only covers primary THA and forecasts up to 2020 (6). As more historical data is now available for analysis we find the need for new forecasts for both primary and revision surgery, the latter being fewer in absolute numbers but requiring more resources and longer hospital stay than primary procedures. The Danish healthcare system is an obvious source for data for such analysis due to unrestricted healthcare access and a high degree of data reliability, yielding reliable forecasts (7). We made forecasts for the development in incidence rate and total numbers of primary and revision hip arthroplasty from 2020 through 2050.
Patients and methods
Data source
The study was conducted as a register study based on data from the Danish Hip Arthroplasty Register (DHR). The DHR collects data from the Danish healthcare system on primary and revision surgery. The Danish healthcare system comprises primarily tax-paid public clinics but also private clinics. The system is based on free access to healthcare for all patients regardless of socioeconomic status. Treatment and healthcare services are free of charge for the patient.
The DHR has collected data on primary and revision hip arthroplasty since 1995. All public and private orthopedic departments performing hip arthroplasty in Denmark report to the register. The register has been reported as suitable for epidemiological studies with a positive predictive value of 84% and a completeness of 97.8% (8,9). The data from the DHR is combined with data from the Danish National Patient Register to provide data on data completeness for each year.
Projections are calculated from historical numbers of primary and revision THAs in Denmark from 1995 to 2019. Data on historical population numbers as well as population projections was retrieved from Statistics Denmark (1). This is the official central authority on Danish statistics, collecting and publishing statistics on Danish society.
The study is presented in accordance with the STROBE statement.
Study population
Data from 1995 to 2019 was retrieved from DHR. 199,356 primary procedures were registered. 521 duplicate entries were excluded, which left 198,835 procedures for analysis. 29,589 revision procedures were recorded. 133 duplicates were identified, leaving 29,456 procedures for analysis. Data for both primary and revision surgery was then divided into annual numbers for each year from 1995 to 2019 and corrected for data completeness to provide accurate numbers of procedures.
Statistics
Annual incidence rates per 105 inhabitants from 1995 through 2019 were calculated for both primary and revision procedures using historical population numbers and numbers of procedures per calendar year. Using logistic and Gompertz regression on historical incidence rates, predictions of future incidence rates from 2020 through 2050 were calculated. Both logistic models assume an upper asymptote representing the maximal incidence rate, as opposed to exponential growth where the incidence will increase unlimited, which is not realistic. Where logistic regression assumes a symmetric growth, Gompertz regression has a more gradual approach towards the upper asymptote.
Combining the predicted incidence rates with the official prediction of future population from Statistics Denmark, predictions of total numbers of both primary and revision surgery procedures were calculated.
Root mean square error (RMSE) was used to detect the difference between the observed and predicted value and R2 was used as a quality estimator to evaluate the prediction models’ fit to the data points. 95% prediction intervals (PI) were calculated for each individual future time point. We assumed a Gaussian distribution while accounting for the prediction noise by adding 1 inside the square root of the expression for confidence interval of the mean. Incidence is reported as events per 105 citizens per year unless otherwise stated.
All analysis were made using JMP Pro 16.0 by SAS (SAS Institute, Cary, NC, USA).
Ethics, data sharing, funding, and disclosures
This study was approved by the North Denmark Region (ID number 2019-121) and by the steering committee of the DHR (ID DHR-2020-06-19). It was financed by Interdisciplinary Orthopedics at Aalborg University Hospital. All data used in this study is available from DHR and Statistics Denmark. None of the authors reported any conflicts of interests.
Results
Primary THA (Table 1, Table 2 and Figure 1)
From 1995 through 2019 the annual number of primary THA increased from 4,118 to 11,711. The incidence similarly increased from 79 to 202. Both regression models showed a continued increase in IR and total number of surgeries. The logistic regression model forecasts an increase in IR, reaching its maximum of approximately 208 (PI 178–251) around 2040. When combining the IR prediction with population forecasts the total number of surgeries is expected to increase to 13,147 in 2050. Gompertz regression model forecasts increasing IR until 2050 with maximum at 220 (PI 212–281) and increase in total numbers to 13,893. The increase in total numbers forecast by the 2 models is between 12% (Logistic) and 19% (Gompertz). RMSE was 8 and R2 was 0.96 for both Logistic and Gompertz, which represent an acceptable fit of the 2 models used in the forecast.
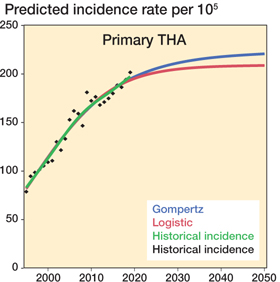
Figure 1. Prediction of incidence rate of primary THA.
Revision THA (Table 3, Table 4 and Figure 2)
Revision surgery increased from 853 in 1995 to 1,447 in 2019. The IR increased from 16 in 1995 to its maximum of 30 in 2009 and 2012, then declining to 25 in 2019. Both the logistic and Gompertz regression predicts that the IR has already reached a maximum of 27 in recent years, and both models have PI of 22–29 in 2020 and PI of 25–33 in 2050. Due to the forecast increase in population, total numbers of revision surgeries are expected to increase to 1,720 according to the logistic regression model and 1,723 according to Gompertz in 2050, representing an increase of approximately 19%. RMSE was 2 and R2 0.71 for both Logistic and Gompertz, which represent an acceptable fit of the 2 models used in the forecast, although not as good as for primary THA
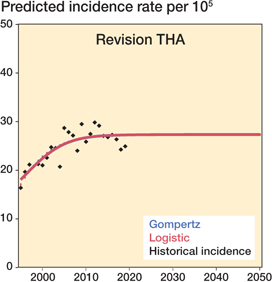
Figure 2. Prediction of incidence rate of revision THA.
Discussion
Our main finding forecasts increase in primary THA IR between 208 (logistic) and 220 (Gompertz) in 2050 and in absolute numbers an increase to 13,147 (logistic) and 13,893 (Gompertz), representing an increase of 12–19% from 11,300 in 2019. For revision THA, IR reached a plateau of 25–30 around 2010, but due to expected increase in total population total numbers of surgeries are forecast to increase to 1,720–1,723 in 2050, which is an increase of approximately 19%.
From 1995 through 2019, there has been an increase in IR of primary THA in Denmark from 79 to 202. Our prediction models show that the IR is near its plateau of 208–220 , an increase of 3–9%, which it is expected to reach around 2040– 2050. A previous study from Denmark published in 2005 predicted an up to 210% increase in IR from 2002 through 2020, also based on data from the Danish Hip Arthroplasty Register, but only from 1996 to 2002 (6). It forecast a rise in incidence rates to 417 primary procedures in 2020, which is significantly more than the IR of 190 reported in the annual report from DHR in 2019. As the historical data in our study covers 25 years, trends in the development in IR are based on more data points and can therefore be considered as more accurate, i.e., the trend towards a stagnating IR, expected to increase by only 3–9%, in the next decades. Projections of THA surgery in Sweden from 2013 to 2030 have also been published (5). A rise in IR from 332 aged 40 or older to 358 in 2030 were projected, and an upper incidence level of around 400 is projected to be reached in 2107. As this IR is calculated for population aged 40 or above, the IR numbers are not directly comparable to the IR in our projection, but a projected number of approximately 20,000 primary THAs in 2030 and the total population forecast in the article to 10,660,664 equals an IR of 188. This is not very different from our forecast predicting a peak IR of 208–220 around 2040–2050. The Danish and Swedish society and healthcare are similar given that they are tax-paid public healthcare systems with free access for all citizens regardless of socioeconomic status. Given the similarity between the 2 healthcare systems and the 2 projections we find that this further supports our projection.
2 studies projected THA surgery in Germany until 2040. One study used historical data on IR from 2010 to 2016 to project an increase in IR of 38% to 360 and increase in total numbers of 27% from 2010 through 2040 (2). The other used population projection and estimates of future healthcare expenditures as a percentage of GDP to project an increase in IR of 29% to 437 and an increase in total numbers of 23% from 2016 through 2040 (10). These 2 studies project an increase in IR that is approximately twice as high as in our study. A possible explanation for this difference could be that these studies use different methodologies and are based on data from a different healthcare system. This could result in projections that are not directly comparable to the projection in our study. This is generally an issue when comparing predictions with differences in methodology from countries with differences in population and healthcare service. Our study is based on 25 years of data from a socialized healthcare system with free access as previously described. Access to surgery is not dependent on personal economic factors, which means that historical IR used in our projection is expected to be close to the true IR as this is less biased by factors other than the indication for THA.
In the past decades fast track protocols have reduced length of stay and cost of primary THA surgery (11,12). Yet revision surgery still requires longer hospitalization, is more costly and has a higher morbidity and mortality than primary surgery (13). An expected increase in total numbers of THA would be expected to cause an increase in number of revision surgeries. Furthermore, with increasing life expectancy patients will live longer with their arthroplasty, which would also cause an increase in total numbers of revisions. Yet revision surgery seems to have reached its plateau IR of 25–30 around 2010, and the predicted increase in total numbers is due only to the expected increase in population. This is very different from other studies predicting future IR in revision THA. 2 studies from the United States predict increases in IR of 43–70% from 2014 through 2030 (14) and by 137% from 2005 through 2030 (15). This is significantly higher than our prediction, but again, healthcare systems and methodology are very different in the 2 American studies and in our prediction model. A recent study from South Korea predicts an increase in total numbers from 2,870 in 2018 to 3,241 in 2030, which is an increase of 13% (16). The study does not predict development in IR, but the slight increase of 1.1% per year in total numbers is more comparable to our findings than the 2 US studies.
With an ongoing increase in IR and numbers of primary THA surgeries during the last decades it would be expected that the number of revision surgeries would also increase. The reason for the stable IR for revision shown in our data is unknown. Factors like increased surgeon training and experience, more wear-resistant articulating surfaces, infection prevention, and improved component fixation might result in lower revision rates. A change in revision strategy towards a more nonoperative approach would also result in lower IR. The increase in IR for primary THA would be expected to affect the IR for revisions due to early revision causes such as early infections or dislocations. Late causes for revision like wear or aseptic loosening would be more affected by the prevalence of THA. If the prevalence of THA has not increased at the same rate as the IR, this could be a contributing factor to the stable IR of revision surgery. We were not able to obtain data from DHR on indications for revision surgery that could show trends in causes for revision such as dislocation, infection, fracture, component failure, or other reasons. This information could help to explain the stable rate of revision surgery.
Strengths
We consider the data in this study reliable, and data from the Danish healthcare system is generally considered to have high external validity (7). It is a socialized system that provides access to medical examination, treatment, and sick leave if needed. This means that a Danish patient needing primary or revision surgery can choose this treatment, regardless of personal socioeconomic factors. We find that this provides a truer incidence of surgery than a private healthcare system where patients might choose not to have surgery because of economic or social factors. Furthermore, The Danish Central Person Registry provides excellent data completeness and follow-up. The data from the DHR has also been shown to have good data validity and to be suitable for epidemiological studies (8,9).
Limitations
Predictions of future demands for medical treatment are uncertain; new treatment options, changes in indications, and changes in demographic factors may influence the result. Events such as a nurses’ strike in 2008 resulted in a drop in surgeries and IR that year, and the recent COVID 19 pandemic also affects surgical capacity. It is likely that there will be a compensatory increase after such events, and there could potentially be an effect on the prediction. Extrapolation of historical medical data can provide estimates but not exact data on the need for primary and revision surgery in the next decades. This is illustrated by the Danish and Swedish studies previously discussed (5,6). The Danish study predicted a rise in IR to 417 in 2020, but the annual report from the DHR in 2019 showed the incidence was 190. Some of the reasons for this overestimation could be that the prediction is based on only 6 years of data, and it predicts a continuous increase without an upper limit, which leads to an unrealistically high IR. The Swedish study predicts an upper limit for the IR, but it underestimates the increase in THA surgeries. It predicts an IR of 339 and total number of 17,588 THAs in 2019, but the Swedish Hip Arthroplasty Register annual report of 2019 (17) shows the IR increased to 373 and total numbers to 19,692, a difference of 10% and 12% only 6 years into the prediction. This emphasizes that predictions and forecasts have limitations.
Our forecast is not stratified into specific age groups. If the older sector of the population increases relatively more than the younger one this would increase the number of surgeries more than if the younger sector of the population increases relatively more. If historical data on surgery and predictions of future developments in population numbers were stratified into different age group intervals, the difference in IR between age groups could be taken into account. This could make the forecast more accurate.
In conclusion our projection shows that the number of primary THA surgeries in Denmark will continue to increase in the years to come, both due to an increase in IR and due to changes in population. The increase in IR seems to be slowing and is predicted to plateau at 208–220 around 2040–2050. For revision THA the IR has been stable for the last 10 years, but the total number of surgeries will increase due to changes in population.
- Statistics Denmark. https://www.dst.dk.
- Pilz V, Hanstein T, Skripitz R. Projections of primary hip arthroplasty in Germany until 2040. Acta Orthop 2018; 89 (3): 308-13. doi: 10.1080/17453674.2018.1446463.
- Culliford D, Maskell J, Judge A, Cooper, Prieto-Alhambra C D, Arden N K. Future projections of total hip and knee arthroplasty in the UK: results from the UK Clinical Practice Research Datalink. Osteoarthritis Cartilage 2015; 23 (4): 594-600. doi: 10.1016/j.joca.2014.12.022.
- Inacio M C S, Graves S E, Pratt N L, Roughead E E, Nemes S. Increase in total joint arthroplasty projected from 2014 to 2046 in Australia: a conservative local model with international implications. Clin Orthop Relat Res 2017; 475 (8): 2130-7. doi: 10.1007/s11999-0175377-7.
- Nemes S, Gordon M, Rogmark C, Rolfson O. Projections of total hip replacement in Sweden from 2013 to 2030. Acta Orthop 2014; 85 (3): 238-43. doi: 10.3109/17453674.2014.913224.
- Pedersen A B, Johnsen S P, Overgaard S, Søballe K, Sørensen H T, Lucht U. Total hip arthroplasty in Denmark: incidence of primary operations and revisions during 1996–2002 and estimated future demand. Acta Orthop 2005; 76 (2): 182-9. doi: 10.1080/00016470510030553.
- Schmidt M, Schmidt S A J, Adelborg K, Sundbøll J, Laugesen K, Ehrenstein V, et al. The Danish health care system and epidemiological research: from health care contacts to database records. Clin Epidemiol 2019; 11: 563-91. doi: 10.2147/CLEP.S179083.
- Pedersen A B, Johnsen S P, Overgaard S, Søballe K, Sørensen H T, Lucht U. Registration in the Danish Hip Arthroplasty Registry: completeness of total hip arthroplasties and positive predictive value of registered diagnosis and postoperative complications. Acta Orthop Scand 2004; 75 (4): 434-41. doi: 10.1080/00016470410001213-1.
- Gundtoft P H, Varnum C, Pedersen A B, Overgaard S. The Danish hip arthroplasty register, Clin Epidemiol 2016; 8: 509-14. doi: 10.2147/CLEP.S99498.
- Rupp M, Lau E, Kurtz S M, Alt V. Projections of primary TKA and THA in Germany from 2016 through 2040. Clin Orthop Relat Res 2020; 714 (7): 1622-33. doi: 10.1097/corr.0000000000001214.
- Zhu S, Qian W, Jiang C, Ye C, Chen X. Enhanced recovery after surgery for hip and knee arthroplasty: a systematic review and meta-analysis. Postgrad Med J 2017; 93 (1106): 736-42. doi: 10.1136/postgradmedj-2017-134991.
- Petersen P B, Kehlet H, Jørgensen C C. Improvement in fast-track hip and knee arthroplasty: a prospective multicentre study of 36,935 procedures from 2010 to 2017. Sci Rep 2020; 10 (1): 1-9. doi: 10.1038/s41598020-77127-6.
- Bozic K J, Katz P, Cisternas M, Ono L, Ries M D, Showstack J. Hospital resource utilization for primary and revision total hip arthroplasty. J Bone Joint Surg (Am) 2005; 87 (3): 570-6. doi: 10.2106/JBJS.D.02121.
- Schwartz A M, Farley K X, Guild G N, Bradbury T L. Projections and epidemiology of revision hip and knee arthroplasty in the United States to 2030. J Arthroplasty 2020; 35 (6): S79–S85. doi: 10.1016/j.arth.2020.02.030.
- Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg (Am) 2007; 89 (4): 780-5. doi: 10.2106/JBJS.F.00222.
- Park J W, Won S H, Moon S Y, Lee Y K, Ha Y C, Koo K H. Burden and future projection of revision total hip arthroplasty in South Korea. BMC Musculoskelet Disord 2021; 22 (1): 375. doi: 10.1186/s12891-02104235-3.
- Swedish Hip Arthroplasty Register Annual report; 2019. https://registercentrum.blob.core.windows.net/shpr/r/VGR_Annual-report_SHAR_2019_EN_Digital-pages_FINAL-ryxaMBUWZ_.pdf.