A comparison study on patient-reported outcome between obese and non-obese patients with central lumbar spinal stenosis undergoing surgical decompression: 14,984 patients in the National Swedish Quality Registry for Spine Surgery
Niyaz HARENI 1,2, Kari GUDLAUGSSON 1, Fredrik STRÖMQVIST 1, Björn E ROSENGREN 1, and Magnus K KARLSSON 1
1 Departments of Clinical Sciences and Orthopedics, Lund University, Skåne University Hospital, Malmö; and 2 Department of Orthopedics, Halland Hospital, Sweden
Background and purpose — Obesity has been associated with inferior outcomes after laminectomy due to central lumbar spinal stenosis (CLSS); we evaluated whether this occurs in surgery on national bases.
Patients and methods — We retrieved pre- and 1-year postoperative data from the National Swedish Quality Registry for Spine Surgery regarding patients aged ≥ 50 with laminectomy due to CLSS in 2005–2018. 4,069 patients had normal weight, 7,044 were overweight, 3,377 had class I obesity, 577 class II obesity, and 94 class III obesity (“morbid obesity”). Patient-reported outcome included satisfaction after 1 year, leg pain (Numerical Rating Scale [NRS], rating 0–10), disability (Oswestry Disability Index [ODI], rating 0–100). Complications were also retrieved.
Results — 1-year postoperatively, 69% of patient of normal weight, 67% who were overweight, and 62% with obesity (classes I–III aggregated) were satisfied (p < 0.001) and 62%, 60%, and 57% in obese groups I–III, respectively (p = 0.7). NRS leg pain improved in normal-weight patients by 3.5 (95% CI 3.4–3.6), overweight by 3.2 (CI 3.1–3.2), and obese by 2.6 (CI 2.5–2.7), and 2.8 (CI 2.7–2.9), 2.5 (CI 2.2–2.7), and 2.6 (CI 2.0–3.2) in obese classes I–III, respectively. ODI improved in normal weight by 19 (CI 19–20), overweight by 17 (CI 17–18), and obese by 14 (CI 13–15), and 16 (CI 15–17), 14 (CI 13–16), 14 (CI 11–18) in obese classes I–III, respectively. 8.1% of normal weight, 7.0% of overweight, and 8.1% of obese patients suffered complications (p = 0.04) and 8.1%, 7.0%, and 17% among obese classes I–III, respectively (p < 0.01).
Conclusion — Most obese patients are satisfied after laminectomy due to CLSS, even if satisfaction rate is inferior compared with normal-weight patients. The morbidly obese have more complications than patients with lower BMI.
Citation: Acta Orthopaedica 2022; 93: 880–886. DOI http://dx.doi.org/10.2340/17453674.2022.5254.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-05-22. Accepted: 2022-10-21. Published: 2022-11-28.
Correspondence: Niyaz.Hareni@med.lu.se
MK, NH, and KG proposed the study. NH wrote the initial manuscript under guidance from MK, BR, and FS. All authors revised the manuscript and contributed to the final manuscript.
Handling co-editors: Bart Swierstra and Philippe Wagner
Acta thanks JLC van Susante and Anne Versteeg for help with peer review of this study.
For central lumbar spinal stenosis (CLSS), primary treatments include patient education, physiotherapy, pain medication, and/or epidural injection (1), while decompressive surgery is advocated with persisting disability (1). Studies, including RCTs (2-5), have reported that laminectomy is followed by a favorable outcome similar to laminectomy with fusion (3). However, a variety of factors, such as old age, chronicity of symptoms, and/or preoperative inferior mental health, also influence the surgical outcome, while the importance of body mass index (BMI) is debated (6-8). Obesity (BMI ≥ 30.0 (9)) is associated with inferior outcomes in a variety of surgical procedures (10-12), and in spine surgery with infection, venous thromboembolism, perioperative blood loss, and prolonged surgical time (13,14). Some studies report inferior clinical outcome also in obese spine-surgical patients (15,16), while others oppose this (7,17-19).
We studied whether both obese and non-obese patients who undergo laminectomy due to CLSS achieve improvement of clinical relevance and whether clinical outcomes are inferior, and risks for complications higher, in obese than in non-obese patients.
Patients and methods
In Sweden, 95% of the departments that perform spine surgery register procedure-specific data in the Swedish National Quality Registry for Spinal Surgery (SweSpine) (20). The registry has a completeness of 85% and a participation rate of patient follow-up of 75% 1 year after surgery (20). Preoperatively, patients complete a questionnaire regarding patient demographics such as height, bodyweight, and smoking status as well as patient-reported outcome measures (PROMs) to characterize clinical symptoms. The PROMS include Numeric Rating Scale (NRS) pain for leg and back pain and Oswestry Disability Index (ODI). Postoperative questionnaires, identical to the preoperative, are sent to the patients 1, 2, 5, and 10 years after surgery. At follow-up, grade of satisfaction is also registered on a 3-point Likert scale, using satisfied, uncertain, or dissatisfied.
Variables
We regarded an improvement in NRS leg pain of ≥ 40%, NRS back pain of ≥ 33%, and ODI ≥ 30% as clinically important differences based on previous research on minimal clinically important difference (MCID) (21). Perioperative data (acute or elective surgery, diagnosis, type of procedure, level(s) of surgery) and incidence of complications before hospital discharge (death, dural tear, injury of a nerve root, postoperative hematoma, urinary retention, urinary tract infection, pulmonary embolism, wound infection, cauda equina syndrome, thrombosis, and “other complication,” all answered dichotomously [Yes or No]) are reported by the operating surgeon.
Participants
We retrieved data from SweSpine for patients who underwent surgery for CLSS without degenerative spondylolisthesis between November 2005 and December 2018 and had preoperative data (n = 29,237). Surgery types were decompression (with or without microscope) in the old version of SweSpine and laminectomy (total or midline sparing) in the new SweSpine version. We excluded patients with missing sex information, age < 50, missing information on height and/or weight, BMI < 18.5 (i.e., underweight), improbable values for height (< 140 cm or > 210 cm), improbable values for bodyweight (< 40 kg or > 200 kg), missing data on type of surgery, procedures other than laminectomy without fusion, previous spine surgery, and missing PROMs at the 1-year follow-up. This resulted in 14,984 patients with preoperative data and at least 1 PROM at the 1-year follow-up (Figure 1). According to the WHO definition (9), the study included 4,069 patients of normal weight (BMI 18.5 to < 25.0), 7,044 who were overweight (BMI 25.0 to < 30.0), 3,377 with obesity class I (BMI 30.0 to < 35.0), 577 with obesity class II (BMI 35.0 to < 40.0), and 94 with obesity class III (“morbid obesity”) (BMI ≥ 40.0) (Table 1). Preoperative data in patients who responded to both the preoperative and the 1-year postoperative questionnaire (responders) and in those who answered the preoperative but not the 1-year postoperative questionnaire (non-responders) are presented in Table 2 (see Supplementary data).
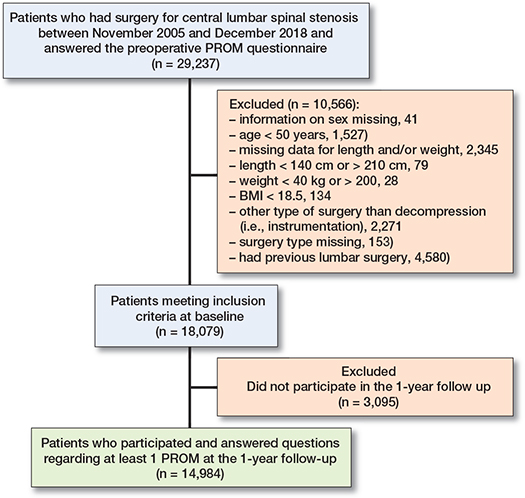
Figure 1. Flow chart of patient inclusion from SweSpine.
Statistics
We used IBM SPSS version 28 (IBM Corp, Armonk, NY, USA) for statistical calculations. Descriptive data are presented as numbers, proportions (%), means with standard deviations (SD), and inferential data as means with 95% confidence intervals (CI). We utilized chi-square and Fisher’s exact test to examine group differences in categorical data and analyses of variance (ANOVA) and analyses of covariance (ANCOVA), adjusted for age, sex, smoking, and baseline status for the evaluated trait, for continuous data. The model assumptions concerning linear regression models were assessed using residual plots without showing signs of heteroscedasticity. We performed a Kolmogorov–Smirnov test to test the distribution of residuals. We ensured that no Kolmogorov–Smirnov statistics were below 0.05. We performed a Hosmer–Lemeshow test to ensure goodness of fit in the logistic regression models; no significant values were found. We used linear regression to examine the relation between BMI and outcome. For dichotomous outcomes, we utilized logistic regression. We regarded a p-value < 0.05 (2-sided) to indicate a statistically significant difference.
Ethics, data sharing plan, funding, and disclosures
The study was approved by the Lund regional ethical review board (Dnr LU 217/158 allowed inclusion from Swespine years 2000–2016 and additional aplication Dnr 2020-03112 allowed inclusion from 2017-01-01 to 2019-12-31). The data is available from SweSpine upon request and approval by the registry board. No specific funding has been received for this study. NH has received general grants for doctoral studies. No conflicts of interest were declared.
Results
Outcomes in the whole study population
Baseline data are presented in Table 1. For all included patients, 64% were satisfied 1 year after surgery, 7.6% of the patients had sustained any complication, and 5.8% a dural tear. The improvement in NRS leg pain was 3.1 (SD 3.5), in NRS back pain 2.3 (3.1), and in ODI 17 (18). This corresponds to a relative mean improvement in NRS leg pain of 43%, in NRS back pain of 36%, and in ODI of 41%. Among all patients, 60% improved equally or more than MCID (21) in NRS leg pain, 60% in NRS back pain, and 61% in ODI. We found a negative association in the linear regression between BMI and improvement in NRS leg pain (beta value –0.05 [CI –0.06 to –0.03]) and ODI (–0.16 [CI –0.23 to –0.09]) but not for improvement in NRS back pain (–0.01 [CI –0.02 to 0.01]).
Outcomes in normal-weight, overweight, and obese patients (Figure 2 and 3, see Supplementary data)
1 year after surgery, 69% of normal-weight patients, 67% of overweight patients, and 62% of obese patients were satisfied with the surgical outcome (p < 0.001 for group differences). Pre- and postoperative data and improvements in the groups are presented in Table 3.
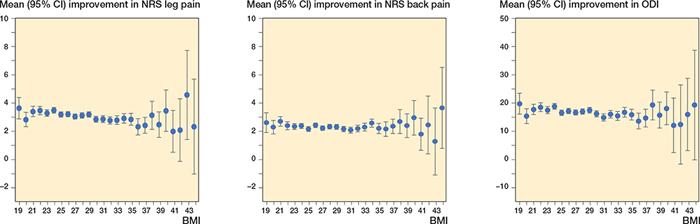
Figure 2. Improvement in Numeric Rating Scale (NRS) leg pain, NRS back pain, and Oswestry Disability Index (ODI) in relation to body mass index (BMI) class. BMI 19 includes patients with BMI 18.5 to <19.5, BMI 20 those with BMI 19.5 to < 20.5 and so on. n = 13,850 for leg pain, 13,849 for back pain and 14,176 for ODI. Data are means with 95% confidence intervals. Patients with BMI ≥ 45 (n = 25) are excluded in the graphs.
The proportions of patients who improved ≥ MCID (21) were different in normal weight, overweight, and obese patients regarding NRS leg pain, NRS back pain, and ODI (all p < 0.001) (Table 4). In analyses adjusted for age, sex, smoking, and baseline status for the evaluated dependent variable, we found that overweight and obese patients had lower odds for improvement: ≥ MCID in NRS leg pain, NRS back pain, and ODI compared with normal-weight patients (Table 4).
| Outcome | Total number | Normal weight BMI 18.5 to < 25.0 | Overweight BMI 25.0 to < 30.0 | Obese BMI ≥ 30.0 | p-value c | ||||||
| n | Improved (%) a | Adjusted OR (CI) b | n | Improved (%) a | Adjusted OR (CI) b | n | Improved (%) a | Adjusted OR (CI) b | |||
| NRS leg pain | 13,313 | 3,529 | 64 | reference | 6,175 | 61 | 0.8 (0.7–0.9) | 3,609 | 55 | 0.6 (0.6–0.7) | < 0.001 |
| NRS back pain | 12,980 | 3,399 | 63 | reference | 5,993 | 61 | 0.9 (0.8, 0.9) | 3,588 | 56 | 0.7 (0.6, 0.8) | < 0.001 |
| ODI | 14,048 | 3,747 | 65 | reference | 6,558 | 62 | 0.9 (0.8, 0.9) | 3,747 | 55 | 0.6 (0.5, 0.7) | < 0.001 |
| a Proportion improved ≥ MCID. | |||||||||||
| b Odds ratio for gaining improvement ≥ MCID. | |||||||||||
| b Group comparison of proportions improved ≥ MCID. | |||||||||||
8% of normal-weight patients, 7% of overweight patients, and 8% of obese patients had any complication (p = 0.04 for group differences) (Table 5). The corresponding proportion of patients with dural tear was 6.0%, 5.2%, and 6.6% (p = 0.01 for group differences) (Table 5).
Outcomes in relation to obesity class
1 year after surgery 62% of patients in obesity class I were satisfied with the surgical outcome. The corresponding proportions of patients in obesity class II and class III were 60% and 57% (p = 0.7 for group differences). Pre- and postoperative data and improvements in relation to obesity class are presented in Table 6.
The proportions of patients who improved ≥ MCID in NRS leg pain, NRS back pain, or ODI were similar in obese classes I, II, and III patients (all p > 0.05) (Table 7). In analyses adjusted for age, sex, smoking, and baseline status, we found similar odds ratios for improvement in patients in the different obesity classes (Table 7).
| Outcome | Total number | Obese I BMI 30.0 to < 35.0 | Obese II BMI 35.0 to < 40.0 | Obese III BMI ≥ 40.0 | p-value c | ||||||
| n | Improved (%) a | Adjusted OR (CI) b | n | Improved (%) a | Adjusted OR (CI) b | n | Improved (%) a | Adjusted OR (CI) b | |||
| NRS leg pain | 3,609 | 3,005 | 55 | reference | 518 | 53 | 0.95 (0.8–1.1) | 86 | 49 | 0.8 (0.5–1.2) | 0.5 |
| NRS back pain | 3,588 | 2,980 | 56 | reference | 522 | 54 | 0.9 (0.8–1.1) | 86 | 62 | 1.3 (0.8–2.0) | 0.4 |
| ODI | 3,747 | 3,128 | 56 | reference | 528 | 51 | 0.8 (0.7–0.99) | 91 | 51 | 0.8 (0.5–1.3) | 0.08 |
| a Proportion improved ≥ MCID. | |||||||||||
| b Odds ratio for gaining improvement ≥ MCID. | |||||||||||
| c Group comparison of proportions improved ≥ MCID. | |||||||||||
8.1% of patients in obesity class I, 7.0% of patients in obesity class II, and 17% of patients in obesity class III had any complication (p < 0.01 for group differences) (Table 8). The corresponding proportions of patients with dural tear were 6.7%, 4.9%, and 15% (p < 0.01 for group differences) (Table 8).
Discussion
We found that decompression for CLSS is followed by subjective and objective improvement in patients of normal weight, those who were overweight, and obesity grades I, II, and III, and that patients in general are satisfied 1 year after surgery. The improvement and subjective outcomes are lower in overweight than in normal-weight patients, and inferior in the obese to those who are overweight. This is further supported by the lower odds ratio for improvement of at least MCID in both overweight and obese patients compared with those of normal weight.
Several previous studies have reported that obese patients experience similar improvement to normal-weight patients (7,17,18,22). These studies have suggested that this may partly be due to obese patients in general being referred for surgery with a more severe preoperative status than normal-weight patients. It should then be noted that also we found obese grades I–III patients being referred for surgery with more severe symptoms than patients of normal weight.
A recent systematic review supports the view of obese patients having no inferior outcomes to patients with lower BMI, when summarizing that obese patients have similar postoperative outcomes to non-obese patients after non-instrumented lumbar surgery (19). However, this review used a BMI cut-off value 30 when comparing patients, without evaluating the outcomes in each obesity class separately. There are, in contrast, studies that infer obesity to be inversely associated with improvement in ODI and an improvement of MCID or more after non-instrumented CLSS surgery (8,15,16). We support this view, when reporting inferior outcomes in obese to normal-weight patients and in obese grade III to obese grade I patients. However, as most patients in all evaluated groups were satisfied with the surgical outcome, it seems reasonable to postulate that the statistically significant differences were of minor clinical relevance. In a study like this, many other factors such as lifestyle, comorbidity, types of performed surgery, and competence of the operating surgeon may be of importance for the outcome.
Obesity is in spinal surgery associated with a higher risk for surgical site infection, venous thromboembolism, perioperative blood loss, and longer surgery times (13,14). We found in obese patients a higher rate of dural tears than in those of normal weight, this being driven by more tears in class III obese patients. There were also more patients with postoperative hematoma in this group. The risk of sustaining any complication in obese class III patients was therefore 2.5 times higher than in obese class I patients. However, the relevance of patient perception of success ought to be regarded as minor, as satisfaction and improvement were no different in obese grade I or III patients.
The strengths of our study include nationwide prospectively collected data, i.e., outcomes in an unselected national population undergoing CLSS surgery. The results are thus applicable to general healthcare and not only, as in many other studies, to highly specialized spine units with certain inclusion criteria. The other type of studies is very important, but in our view we should rather report what it is possible to achieve than results in general healthcare. To our knowledge this is the largest study so far that has addressed the importance of BMI, obesity, and obesity class—including morbidly obese patients—in terms of outcomes and complications.
Limitations of our study include the inability to draw conclusions concerning causality, whether more obese patients should be operated on or fewer, or when the surgeon should be careful in treating an obese patient with surgery. The study design also renders a risk for selection bias with a dropout of 3,095 patients. However, dropout rates of this magnitude should not affect the outcome (23), and we were also unable to identify any major group differences in the dropout comparisons between participants and dropouts. We must also acknowledge that there may still be confounders that we did not identify and adjust for that may influence the outcome.
In conclusion, the study showed improvement after laminectomy due to CLSS in patients of normal weight, those who were overweight, and obesity classes I–III, and that patients in general are satisfied 1 year after surgery. Most obese patients are satisfied, even if satisfaction rate is inferior compared with normal-weight patients. There was no statistically significant difference in satisfaction rate among patients in different classes of obesity, as the group with morbid obesity is small. The morbidly obese have more complications than patients with lower BMI. Decompression due to CLSS ought also to remain a treatment option in patients with overweight and classes I–III obesity.
- Siebert E, Pruss H, Klingebiel R, Failli V, Einhaupl K M, Schwab J M. Lumbar spinal stenosis: syndrome, diagnostics and treatment. Nat Rev Neurol 2009; 5: 392-403. doi: 10.1038/nrneurol.2009.90.
- Weinstein J N, Tosteson T D, Lurie J D, Tosteson A N, Blood E, Hanscom B, et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med 2008; 358: 794-810. doi: 10.1056/NEJMoa0707136.
- Forsth P, Olafsson G, Carlsson T, Frost A, Borgstrom F, Fritzell P, et al. A randomized, controlled trial of fusion surgery for lumbar spinal stenosis. N Engl J Med 2016; 374: 1413-23. doi: 10.1056/NEJMoa1513721.
- Atlas S J, Keller R B, Robson D, Deyo R A, Singer D E. Surgical and nonsurgical management of lumbar spinal stenosis: four-year outcomes from the Maine Lumbar Spine Study. Spine (Phila Pa 1976) 2000; 25: 556-62. doi: 10.1097/00007632-200003010-00005.
- Malmivaara A, Slatis P, Heliovaara M, Sainio P, Kinnunen H, Kankare J, et al. Surgical or nonoperative treatment for lumbar spinal stenosis? A randomized controlled trial. Spine (Phila Pa 1976) 2007; 32: 1-8. doi: 10.1097/01.brs.0000251014.81875.6d.
- Aalto T J, Malmivaara A, Kovacs F, Herno A, Alen M, Salmi L, et al. Preoperative predictors for postoperative clinical outcome in lumbar spinal stenosis: systematic review. Spine (Phila Pa 1976) 2006; 31: E648-663. doi: 10.1097/01.brs.0000231727.88477.da.
- Elsayed G, Davis M C, Dupepe E C, McClugage S G, Szerlip P, Walters B C, et al. Obese (body mass index >30) patients have greater functional improvement and reach equivalent outcomes at 12 months following decompression surgery for symptomatic lumbar stenosis. World Neurosurg 2017; 105: 884-94. doi: 10.1016/j.wneu.2017.06.072.
- Knutsson B, Michaelsson K, Sanden B. Obesity is associated with inferior results after surgery for lumbar spinal stenosis: a study of 2633 patients from the Swedish spine register. Spine (Phila Pa 1976) 2013; 38: 435-41. doi: 10.1097/BRS.0b013e318270b243.
- WHO. Available from: http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi.
- Bookman J S, Schwarzkopf R, Rathod P, Iorio R, Deshmukh A J. Obesity: the modifiable risk factor in total joint arthroplasty. Orthop Clin North Am 2018; 49: 291-6. doi: 10.1016/j.ocl.2018.02.002.
- Chacon M M, Cheruku SR, Neuburger P J, Lester L, Shillcutt S K. Perioperative care of the obese cardiac surgical patient. J Cardiothorac Vasc Anesth 2018; 32: 1911-21. doi: 10.1053/j.jvca.2017.12.025.
- Castle-Kirszbaum M D, Tee J W, Chan P, Hunn M K. Obesity in neurosurgery: a narrative review of the literature. World Neurosurg 2017; 106: 790-805. doi: 10.1016/j.wneu.2017.06.049.
- Jiang J, Teng Y, Fan Z, Khan S, Xia Y. Does obesity affect the surgical outcome and complication rates of spinal surgery? A meta-analysis. Clin Orthop Relat Res 2014; 472: 968-75. doi: 10.1007/s11999-013-3346-3.
- Jackson K L 2nd, Devine J G. The effects of obesity on spine surgery: a systematic review of the literature. Global Spine J 2016; 6: 394-400. doi: 10.1055/s-0035-1570750.
- Giannadakis C, Nerland US, Solheim O, Jakola AS, Gulati M, Weber C, et al. Does obesity affect outcomes after decompressive surgery for lumbar spinal stenosis? A multicenter, observational, registry-based study. World Neurosurg 2015; 84: 1227-34. doi: 10.1016/j.wneu.2015.06.020.
- Burgstaller J M, Held U, Brunner F, Porchet F, Farshad M, Steurer J, et al. The impact of obesity on the outcome of decompression surgery in degenerative lumbar spinal canal stenosis: analysis of the lumbar spinal outcome study (LSOS): a Swiss prospective multicenter cohort study. Spine (Phila Pa 1976) 2016; 41: 82-9. doi: 10.1097/BRS.0000000000001128.
- McGuire K J, Khaleel M A, Rihn J A, Lurie J D, Zhao W, Weinstein J N. The effect of high obesity on outcomes of treatment for lumbar spinal conditions: subgroup analysis of the spine patient outcomes research trial. Spine (Phila Pa 1976) 2014; 39: 1975-80. doi: 10.1097/BRS.0000000000000577.
- Sielatycki J A, Chotai S, Stonko D, Wick J, Kay H, McGirt MJ, et al. Is obesity associated with worse patient-reported outcomes following lumbar surgery for degenerative conditions? Eur Spine J 2016; 25: 1627-33. doi: 10.1007/s00586-016-4460-1.
- Ghobrial J, Gadjradj P, Harhangi B, Dammers R, Vleggeert-Lankamp C. Outcome of non-instrumented lumbar spinal surgery in obese patients: a systematic review. Br J Neurosurg 2022; 36(4): 447-56. doi: 10.1080/02688697.2021.1885615.
- SweSpine. Available from: www.swespine.se.
- Austevoll I M, Gjestad R, Grotle M, Solberg T, Brox J I, Hermansen E, et al. Follow-up score, change score or percentage change score for determining clinical important outcome following surgery? An observational study from the Norwegian registry for Spine surgery evaluating patient reported outcome measures in lumbar spinal stenosis and lumbar degenerative spondylolisthesis. BMC Musculoskelet Disord 2019; 20: 31. doi: 10.1186/s12891-018-2386-y.
- Azimi P, Yazdanian T, Shahzadi S, Benzel E C, Azhari S, Nayeb Aghaei H, et al. Cut-off value for body mass index in predicting surgical success in patients with lumbar spinal canal stenosis. Asian Spine J 2018; 12: 1085-91. doi : 10.31616/asj.2018.12.6.1085.
- Elkan P, Lagerback T, Moller H, Gerdhem P. Response rate does not affect patient-reported outcome after lumbar discectomy. Eur Spine J 2018; 27: 1538-46. doi: 10.1007/s00586-018-5541-0.
Supplementary data
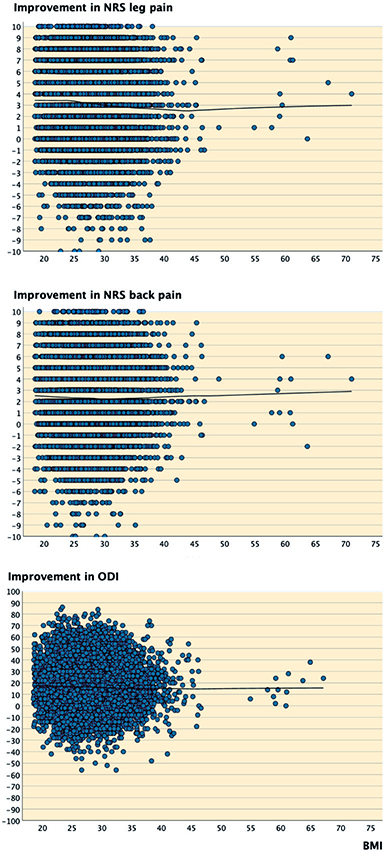
Figure 3. Scatter plots with loess line. Improvement at 1-year follow up in Numeric Rating Scale (NRS) leg pain, NRS back pain, and Oswestry Disability Index (ODI) in relation to body mass index (BMI) class. n = 13,850 for leg pain, 1,3849 for back pain and 14,176 for ODI.