Inducible displacement CT increases the diagnostic accuracy of aseptic loosening in primary total hip arthroplasty
Olof SANDBERG 1, Sofia CARLSSON 2, Ellen HARBOM 3, Vendela CAPPELEN 3, Simon THOLÉN 2, Henrik OLIVECRONA 5, and Per WRETENBERG 4
1 Sectra AB, Linköping; 2 Department of Radiology, Örebro University Hospital; 3 School of Medical Sciences, Örebro University; 4 Department of Medical Sciences, Section of Orthopaedics, Örebro University Hospital; 5 Department of Molecular Medicine and Surgery, Karolinska Institutet, Sweden
Background and purpose — Inducible displacement CT compares 2 CTs acquired in series but with alternated rotation of the femur. This provides visual and quantitative clues as to the mechanical situation, i.e., loosening, of a total hip arthroplasty. We report the accuracy of this method as well as the experience of integrating it into a clinical workflow.
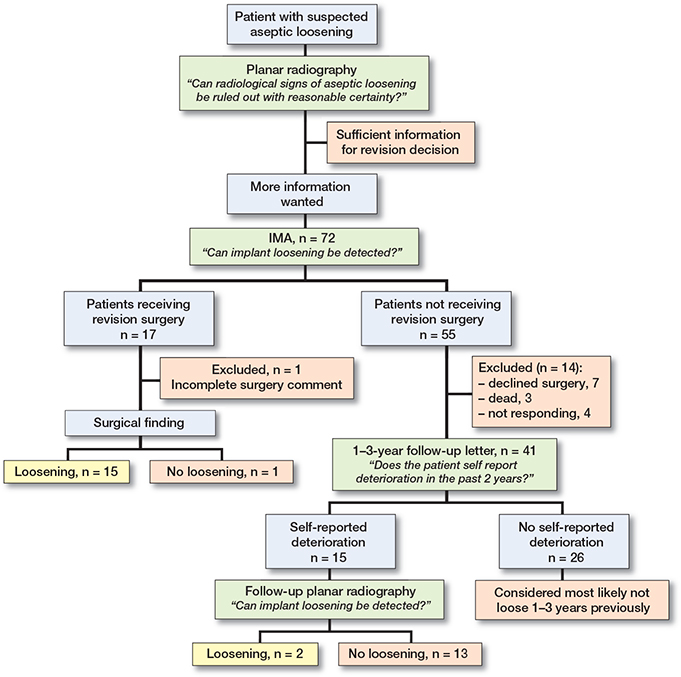
Patients and methods — This was a retrospective single centre study of 72 cases of suspected aseptic loosening were the surgeon after reviewing a standard plain radiograph saw a need for more information. The displacement CT and plain radiograph were compared either to intraoperative findings or a 1–3 year follow up questionnaire for patients that did not have revision surgery. Patients reporting degradation in status since the time of the displacement CT were called for a follow up plain radiograph. Sensitivity and specificity were assessed, and user experience gathered.
Results — Of 72 enrolled patients 15 were lost to follow-up. Of the remaining 57, 17 were judged by in-traoperative findings or follow-up to have had loose implants. For plain radiography the sensitivity and specificity were 59% (95% CI 35–82) and 85% (74–96). For displacement CT the corresponding values were 77% (56–97), and 100% (100–100) respectively. The tool was adaptable to clinical routine.
Conclusion — Displacement CT with alternated rotations of the femur is a viable option to improve the diagnostic process for identifying aseptic loosening in a total hip arthroplasty.
Citation: Acta Orthopaedica 2022; 93: 831–836. DOI http://dx.doi.org/10.2340/17453674.2022.5240.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-04-13. Accepted: 2022-09-30. Published: 2022-10-31.
Correspondence: olof.sandberg@sectra.com
EH, planned, performed, analyzed, interpreted, and wrote the first draft. VC planned and performed the follow-up. ST and SC took part in the data collection; PW and HO planned the design and interpreted data. OS merged the first manuscript with the follow-up data. Everyone took part in the manuscript revision.
Handling co-editorS: Bart Swierstra and Jonas Ranstam.
Acta thanks Bart Pijls and Stephan Röhrl for help with peer review of this study.
Loosening is the main reason for about 40% of revisions of total hip arthroplasties (THAs) (1). On plain radiography loosening can be detected as bone destruction in the form of radiolucent lines (zones) but in some cases results from plain radiography are inconclusive. Considerable efforts have been put into developing methods to diagnose aseptic loosening with higher accuracy (2-5). While nuclear medicine scans such as PET or SPECT-CT can provide useful information, positive findings are known to be difficult to interpret due to normal bone activity (6). As a comparison, inducible displacement analysis has the advantage of demonstrating and quantifying the implant movement itself rather than inferring its presence from secondary signs. Using inducible displacement to identify loosening has been a research topic since the 1990s. This has been done both by radiostereometry (7-9) and by CT (5,10-13). In the last decade CT image quality, radiation doses, and computer processing power have all improved to a point where the inducible displacement method appears feasible for taking the step from research into clinical practice.
We assessed the sensitivity and specificity of inducible displacement CT as a complementary method to plain radiography in the clinical routine of diagnosing aseptic loosening of THA.
Patients and methods
Patients
This was a retrospective study. Eligible patients were all those who had received a displacement CT scan at Lindesberg Hospital, Region Örebro County between September 2017 and December 2019. The decision to have a displacement CT taken was based on the surgeon deeming that the added information could be of value for the diagnosis of aseptic loosening of a THA. Approximately 1 in every 5 patients considered for such a revision during the period was sent for displacement CT. 72 patients examined with displacement CT consecutively between September 2017 and December 2019 at Lindesberg Hospital were included (Figure 1). Information on age, sex, and dates of examinations was gathered.
Study design
The displacement CT had been acquired as described under “Image acquisition” below. The information provided by the displacement CT analysis had been used in the decision whether to recommend surgery. If revision surgery was done, notes were taken on implant status for stem and cup individually.
For a patient not receiving surgery 1–3 years later a follow-up letter was sent asking for self-reported status. If a decline in hip status was reported the patient was asked to make a follow-up appointment. If the patient did not report a decline (s)he was, for the purpose of this study, considered as most likely not suffering from aseptic loosening at the time of the displacement CT.
Any patient reporting a decline was called for a follow-up examination; if this did not show a decline in bone status as visible on plain radiograph compared with the baseline radiograph the patient was considered, for the purpose of this study, as likely not to have suffered from aseptic loosening at the time of the displacement CT. A patient with a follow-up plain radiograph showing signs of degradation was considered as loose also at the time of the displacement CT.
Image acquisition
Plain radiographic examinations were done according to clinical praxis, i.e., pelvic frontal and axial.
To set up the displacement CT method in our hospital a clinician (HO) with previous experience visited the department. A CT protocol was created by adapting recommended settings to the local equipment, a Siemens Somatom Definition AS (64 slice). The settings on the CT were 120 kV, 180 ref.mAs, slice thickness of 0.6 mm, increment 0.6 mm, pitch 1.2, and rotation time 0.5 seconds. For each scan, 1 axial series with and 1 without iMAR (iterative metal artifact reduction) was saved. The instructor also explained how to do the provocations and participated during the first 2 patient scans. At the following image acquisitions, the provocations were performed by a radiology nurse (Figure 2 and Table 1). The radiation dose of this protocol was about 4.5 mSv per scan—as a reference, about twice the annual background radiation (14).
| Before |
|
| During |
|
| After |
|
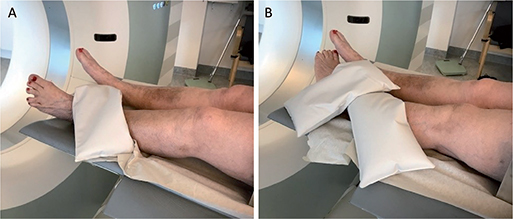
Figure 2. Example of a displacement CT image acquisition with alternated rotation of the left hip. A. The leg is rotated maximally outwards and locked in place with a sandbag at the level of the ankle, thereafter a CT scan is performed. B. The leg is rotated inwards and again locked in place with a sandbag, thereafter the second CT scan is performed.
Producing and analyzing the displacement CT images
The image post-processing was performed using dedicated software, Implant Movement Analysis (IMA, Sectra, Linköping, Sweden), according to methods developed by Olivecrona et al. 2002 (15) and Jedenmalm et al. 2008 (16). The post-processing and analysis was performed by radiologists at Telemedicine Clinic (TMC, Spain), who were specialized in musculoskeletal radiology and in the software used for the displacement CT analysis in this study. The displacement CT analyzer was not blinded to the plain radiographic examinations.
In the processing, semi-automated software overlays the pelvis or femur from both CTs (Figure 3). This enables the viewer to achieve an enhanced view (Figure 4, see Supplementary data) of any displacement-induced movement of implant relative to the bone in which it should be anchored. This procedure is carried out in 3D and can be scrolled through by the assessing radiologist in coronal, axial, and sagittal planes. The displacement CT result includes a qualitative assessment of whether loosening can be detected by the radiologist, together with a moving sequence such as the one shown in Figure 4 (see Supplementary data) illustrating the main finding. In addition to this, the result contains assessment of osteolytic zones as in standard static CTs. If movement exists, the text answer also includes a quantification in millimeters and degrees.
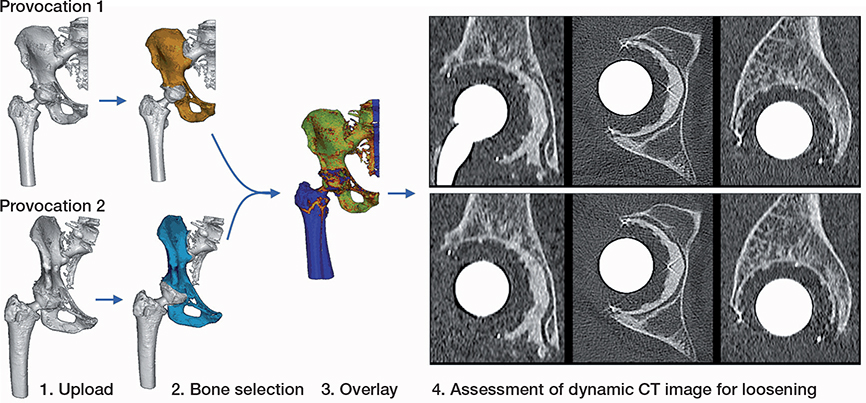
Figure 3. The operating principle of the imaging software. 1. Provocation CT’s are uploaded. 2. The reference body is indicated in both. 3. The software overlays the reference body. 4. The user can assess the overlayed displacement CT video which shows the movement of the implant relative to the reference body. Here, for technical reasons not presented as video overlay but as side by side images. Figure 4 (see Supplementary data) shows an example of actual moving video.
Assessment of sensitivity and specificity
The surgical findings, follow-up questionnaire answer, or follow-up plain radiograph were used as ground truth against which to assess sensitivity and specificity of the displacement CT and baseline radiograph. The surgical findings were classified as negative or positive for loose implant.
The plain radiographs taken at the time of displacement CT were judged as positive or negative for suspicion of implant loosening. The test results from the dynamic CT were not available when this assessment was done.
For the displacement CT results, these were noted as positive or negative for having detected movement relative to the bone. While displacement CT result also include notes on osteolysis and other secondary signs, these were not included in the definition of positive as used in this study.
The follow-up plain radiographic results consisted of the clinical report provided by a radiologist blinded to the displacement CT results. These answers were noted as positive or negative for reporting radiographic signs of progressive implant loosening (deteriorating osteolytic zones, or apparent implant migration) by a researcher blinded to the displacement CT results.
The analysis of sensitivity and specificity was done on the patient level, meaning that the category “loosening detected” could contain both patients with 1 loose implant and patients with 2 loose implants.
Statistics
Sensitivity and specificity were calculated according to standard definitions; sensitivity = found true positives divided by all true positives, and specificity = found true negatives divided by all true negatives. Indeterminate plain radiograph or displacement CT results were categorized as not having found aseptic loosening. The sample size was not based on a power calculation but on previous clinical experience. 95% confidence intervals (CI) were constructed using the simple asymptotic method p±1.96√(p(1–p)/n) where p is the sensitivity and specificity estimate and n is the number of true positives or true negatives for sensitivity and specificity (17).
Likelihood ratios were constructed according to Deeks and Altman (18).
Ethics, funding, data sharing, and disclosures
This study was part of a research project approved by the Regional Ethical Review Board in Uppsala (ref. 2019-00117). It has also been approved as a quality assurance study by the head of operations at the Department of Orthopaedics RÖC. This work was funded by Region Örebro County. Data sharing is not possible. EH, VC, ST, SC, and PW have no conflict of interests to declare. OS works as a full-time employee at Sectra, and HO works as a consultant for Sectra, a company commercializing a tool for assessing displacement CTs.
Results
15 patients were excluded, 7 due to declining surgery for suspected loosening, 3 due to death (in no case directly related to the hip), 4 due to not responding to the follow-up, and 1 due to incomplete surgery notes on fixation of the implants at revision surgery.
The average age was 69 (40–85) years and of the 72 patients 42 were women. 37 of the hips were cemented, 13 uncemented, 5 hybrids, and 17 reverse hybrids. Most patients were ASA class 2 or 3. There were no adverse events recorded for performing the displacement CT.
Of the 41 patients who answered the follow-up survey, 10 reported improvement, 16 no change, and 15 patients reported a decline in hip status. 2 out of the 15 reporting a decline were found by a blinded radiologist looking at a follow-up plain radiograph to have a loose implant. The mean follow-up time was 23 (14–40) months.
Most patients who underwent the displacement CT reported a sense of discomfort or a tense feeling in the joint when the leg was in a rotated position, in particular on internal rotation. In no case did this lead to the imaging having to be aborted, or to lasting complaints.
17 of 57 patients were found to have a loose implant as detected by follow-up or findings during surgery (Table 2 for the distribution of plain radiograph and displacement CT results as compared with follow-up or surgery). When sorted per implant type (cup and stem), there were 11 loose cups and 6 loose stems according to the follow-up and intraoperative findings.
For plain radiography the sensitivity and specificity were 59% (95% CI 35–82) and 85% (74–96) and for displacement CT the corresponding values were 77% (56–97), and 100% (100–100), respectively.
While the plain radiograph gave incorrect identification of loose/not loose in 11 cups and 4 stems, the corresponding numbers for displacement CT were 4 cups and 0 stems. All 4 mislabeled cups were labelled as not loose. 1 was a slowly migrating cup, 2 were cups with reported marked osteolytic zones but without movement reported, and 1 was a cup appearing to be loose on the follow-up plain radiograph but having neither mechanical nor secondary signs reported in the displacement CT read. In addition, there was 1 patient without any implants labelled as loose by displacement CT that nevertheless was revised, and no loose implants were found.
The likelihood ratios for respective diagnostic tool are presented in Table 3, providing the likelihood of a loose implant given either a positive or negative method result.
Discussion
We evaluated the role of displacement CT with alternated provocations as a complementary method to plain radiography in the clinical routine of diagnosing aseptic loosening of THA. We found that sensitivity and specificity increased compared with plain radiography. Furthermore, 6 of the 13 patients correctly labelled by displacement CT as loose were mislabeled as not loose by plain radiography. 15 of the 57 patients included in the study received a different result from displacement CT than from plain radiograph; in these cases, displacement CT was 4 times more likely to have given the correct answer (12 out of 15).
We propose an improved patient flow (Figure 5) where, going by our experience, about one-fifth of patients referred for suspicion of aseptic loosening of THA might be expected to go via the displacement CT pathway.
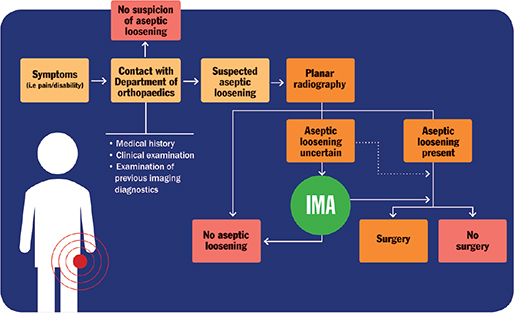
Figure 5. Patient flow chart in cases of suspected aseptic loosening of total hip arthroplasty in Region Örebro County. Dotted line represents flow chart before the introduction of displacement CT. Image from (20) with permission from the author.
The displacement CT method we used is the 1st method capable of showing for both cup and stem the movement of a loose implant via visualization and high-precision quantification in true 3D. The mechanical instability itself is shown rather than inferred by secondary signs such as osteolysis or increased uptake of radioactive compounds. The results we report are in line with findings from smaller cohorts using this method (5,12) and with studies using manual tools and considerably higher radiation doses (10,11). Berger et al. (11) reported a 92% sensitivity and 90% specificity compared with surgical findings for stems. Reinus et al. (10) commented that the precision of the method was likely to increase if an automated tool rather than their manual approach were to be used. In the same study a Newton meter tool was used during revision surgery of femoral stems to measure how much torque was required to move the stem. Lower torque was found in patients where implant rotation at provocation CTs was measured at 5° or higher, strongly indicating that a high rotational value as measured on a provocation CT coincides with low mechanical competence.
While this study used a dichotomous analysis result for displacement CT (mechanical loosening found or not found) the displacement CT results also include a description of the secondary signs such as osteolytic zones. This is similar to regular static CT. During the collection of the patients in this study we realized that it is also important to underline in the communication to the referring surgeon the importance of these indicators of a possible ongoing process that may lead to a mechanical failure.
We perceive the qualitative assessment of the loosening to be a better indicator of overall loosening, as compared with the pure quantification. A purely quantitative assessment is made more problematic as it is not known how many 10ths of a millimeter should be set as a clinically relevant cut-off for aseptic loosening, whereas a qualitative impression of gross movement is more intuitive and corresponded to the intraoperative finding in all 13 positive cases in this study.
While this study focuses purely on THA, displacement CT has also been used successfully for spine and knee patients. Research is ongoing looking at implants in other locations including shoulder and SI joint. The main limiting factor seems to be whether a reliable mode of provocation can be found. Wretenberg et al. reported for the 1st time displacement CT with alternated provocation applied to the knee (13).
We made a number of understandings on how best to adapt the method to clinical practice. 1st, the question in the referral to plain radiography might be better formulated if it makes sure that zones or loosening is mentioned. 2nd, if the displacement CT result also mentions the patient’s ability to comply with the provocation protocol it helps the radiologist to interpret the result. This as too small a provocation makes it hard to draw conclusions. A previous study reported that tremor and reduced range of movement could affect the ability of displacement CT to detect implant loosening (16). 3rd, our study includes 7 cases (all female) where displacement CT showed movement but where the patient did not choose to proceed with revision surgery. If revision surgery is not a conceivable option, it can be argued that no displacement CT examination should be done. However, some benefits may come from getting a diagnosis even if revision is not done, for example not needing to pursue other causes for the individual’s symptoms. 4th, while most patients reported discomfort or a feeling of a tense joint induced by rotation of the leg, the experience of the nurses was that having prepared the patient to expect that the rotation might bring out some of the discomfort for which they sought help meant that all patients were able to go through with the imaging despite the discomfort. In our protocol recommendation we suggest a number of steps meant to minimize the time the patients need to spend with the leg rotated.
This study was designed to analyze the accuracy in identifying implant loosening in patients, rather than for cup or stem separately. The rationale behind this was that while each implant is analyzed individually by the radiologist both for plain radiograph and for displacement CT, the most important decision is that of revision or not revision of the previous surgery. Ergo the most important accuracy to study should be the accuracy in correctly identifying patients with loosening.
While the radiation dose used in this study was around 4.5 mSv per scan, another study has looked at the optimization of lowering the dose while maintaining image quality. That study concluded that a 0.7 mSv dose per scan was an optimal point and that protocol is what is currently recommended to use as a starting point when setting up new sites (19).
It is a limitation of our study that the clinician doing the surgery was not blinded to the displacement CT result, as this could affect the intraoperative finding. This decision was taken due to ethical considerations; we did not want to operate on patients where the displacement CT spoke against surgery. To monitor false negative rates these patients were followed up 1–3 years afterwards. To reduce false positive rates, we kept the group of involved revision surgeons as small as possible and ensured that the department routine to report the absence or presence of loosening was also to be followed for these patients.
In conclusion, displacement CT can provide additional information valuable to the diagnostic process in cases of uncertain aseptic loosening.
- Swedish Arthroplasty Register. Swedish Arthroplasty Register Annual Report 2021. [cited 2022 Apr 13]. Available from: slr.registercentrum.se.
- White L M, Kim J K, Mehta M, Merchant N, Schweitzer M E, Morrison W B, et al. Complications of total hip arthroplasty: MR imaging—initial experience. Radiology 2000; 215(1): 254-62.
- Chew C G, Lewis P, Middleton F, van den Wijngaard R, Deshaies A. Radionuclide arthrogram with SPECT/CT for the evaluation of mechanical loosening of hip and knee prostheses. Ann Nucl Med 2010; 24(10): 735-43.
- Berkowitz J L, Potter H G. Advanced MRI techniques for the hip joint: focus on the postoperative hip. Am J Roentgenology 2017; 209(3): 534-43.
- Olivecrona H, Olivecrona L, Weidenhielm L, Noz M E, Hansen J K, Maguire G Q, et al. A new technique for diagnosis of acetabular cup loosening using computed tomography: preliminary experience in 10 patients. Acta Orthop 2008; 79(3): 346-53.
- Pinski J M, Chen A F, Estok D M, Kavolus J J. Nuclear medicine scans in total joint replacement. J Bone Joint Surg Am 2021; 103(4): 359-72.
- Toksvig-Larsen S, Ryd L, Lindstrand A. Early inducible displacement of tibial components in total knee prostheses inserted with and without cement: a randomized study with roentgen stereophotogrammetric analysis. J Bone Joint Surg 1998; 80(1); 83-9.
- Bragonzoni L, Russo A, Loreti I, Montagna L, Visani A, Marcacci M. The stress-inducible displacement detected through RSA in non-migrating UKR. Knee 2005; 12(4): 301-6.
- Lam Tin Cheung K, Lanting B A, McCalden R W, Yuan X, MacDonald S J, Naudie D D, et al. Inducible displacement of cemented tibial components ten years after total knee arthroplasty. Bone Joint J 2018; 100B(2): 170-5.
- Reinus W R, Merkel K C, Gilden J J, Berger K L. Evaluation of femoral prosthetic loosening using CT imaging. Am J Roentgenology 1996; 166(6): 1439-42.
- Berger R, Fletcher F, Donaldson T, Wasielewski R, Peterson M, Rubash H. Dynamic test to diagnose loose uncemented femoral total hip components. Clin Orthop Relat Res 1996; (330): 115-23.
- Sandberg O, Olivecrona H, Gustafson P. Adverse events due to lack of precision in total hip arthroplasty: the potential of provocation-based CT for diagnosis of implant loosening. Scientific World J 2021 2021: 1-6.
- Wretenberg P, Carlsson S, Tholen S, Olivecrona H. Implant movement analysis (IMA), a new CT based technique for diagnosis of aseptic loosening of total knee arthroplasty. Orthop Res Online 2021; 8(3).
- United Nations. Scientific Committee on the Effects of Atomic Radiation. Sources and effects of ionizing radiation: United Nations Scientific Committee on the Effects of Atomic Radiation: UNSCEAR 2008 report to the General Assembly, with scientific annexes. New York: United Nations; 2010.
- Olivecrona L, Crafoord J, Olivecrona H, Noz M E, Maguire G Q, Zeleznik M P, et al. Acetabular component migration in total hip arthroplasty using CT and a semiautomated program for volume merging. Acta Radiol 2002; 43(5): 517-27.
- Jedenmalm A, Noz M E, Olivecrona H, Olivecrona L, Stark A. A new approach for assessment of wear in metal-backed acetabular cups using computed tomography: a phantom study with retrievals. Acta Orthop 2008; 79(2): 218-24.
- Hess A S, Shardell M, Johnson J K, Thom K A, Strassle P, Netzer G, et al. Methods and recommendations for evaluating and reporting a new diagnostic test. Eur J Clin Microbiol Infect Dis 2012; 31(9): 2111-16.
- Deeks J J, Altman D G. Diagnostic tests 4: likelihood ratios. BMJ 2004; 329(7458): 168-9.
- Eriksson T, Maguire G Q, Noz M E, Zeleznik M P, Olivecrona H, Shalabi A, et al. Are low-dose CT scans a satisfactory substitute for stereoradiographs for migration studies? A preclinical test of low-dose CT scanning protocols and their application in a pilot patient. Acta Eadiol 2019; 60(12): 1643-52.
- Harbom E. Evaluation of the role of implant movement analysis in diagnosing aseptic loosening of total hip arthroplasty (Dissertation) Retrieved from http://urn.kb.se/resolve?urn=urn:nbn:se:oru:diva-76218 2019.
Supplementary data
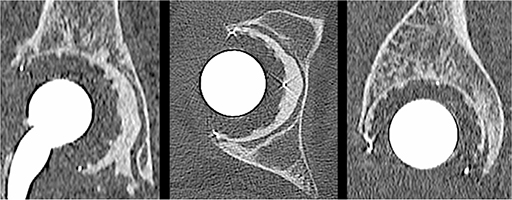
Figure 4. Video with visual representation of displacement CT showing induced movement is linked to the article on ACTAs homepage.