Epidemiology and management of proximal tibia fractures in children and adolescents: a population-based study based on the Kids’ Fracture Tool
Sini-Tuuli KOIVISTO 2,4, Topi LAAKSONEN 1,4, Juho-Antti AHOLA 1,4, Ilkka HELENIUS 3,4, and Antti STENROOS 3,4
1 Department of Pediatric Orthopaedics and Traumatology, University of Helsinki and Helsinki New Children’s Hospital, Helsinki; 2 University of Helsinki, Faculty of Medicine; 3 Department of Orthopaedics and Traumatology, University of Helsinki and Helsinki University Hospital, Helsinki; 4 Finnish Pediatric Orthopaedics Research Group (FIPO), Finland
Background and purpose — Proximal tibial fractures are infrequent injuries in children, and the literature on epidemiology, associated injuries, and management is limited. We calculated a population-based incidence and described the characteristics of proximal tibial fractures in children in terms of complications and management.
Patients and methods — This is a retrospective study over a 6-year-period during including 241 children with proximal tibial fractures who presented to our university hospital. Demographic and fracture-related data was collected from the Kids’ Fracture Tool. The number of children during the study period was collected from statistical year-books of the City of Helsinki to estimate annual incidence.
Results — Extra-articular fractures (129/241) peaked at the age of 3 and tibial tubercle (42/241) and intra-articular fractures (70/241) peaked at the age of 15. Annual incidences were estimated to be 3.4/100,000 children and 22/100,000 children in the age group of 13–16 years for ACL avulsions, and 3.8/100,000 children and 21/100,000 children in the age group of 13–16 years for tibial tubercle fractures. The incidence of vascular compromise (0%) and compartment syndrome was low (0.4 %, 1/241).
Conclusion — Proximal tibial fractures present with a bimodal distribution, with extra-articular fractures peaking at the age of 3 years and fractures of the tibial tuberosity and intra-articular fractures peaking at the age of 15 years. Additionally, associated compartment syndrome and vascular compromise was not as common as previously reported.
Citation: Acta Orthopaedica 2022; 93: 826–830. DOI http://dx.doi.org/10.2340/17453674.2022.4879.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-01-04. Accepted: 2022-08-25. Published: 2022-10-20.
Correspondence: antti.stenroos@hus.fi
S-TK: study design, data acquisition, manuscript preparation. TL: study design, data acquisition, manuscript preparation. J-AA: study design, data acquisition, manuscript preparation. IH: study design, manuscript preparation. AS: study design, manuscript preparation, data acquisition.
Handling co-editors: Cecilia Rogmark and Philippe Wagner
Acta thanks Yasmin Denise Hailer and Ole Rahbek for help with peer review of this study.
Proximal tibia fractures are rare in children (1-3). The physeal separations of the proximal tibia account for less than 1% of all physeal fractures in children (1-3). However, proximal tibial fractures are occurring with an increasing frequency due to increased participation of youth in athletics, as well as other high-energy recreational activities (3,4).
Mechanism of injury and the fracture pattern have been observed to be age-dependent. This reflects the different developmental stages of the proximal tibia in the immature skeleton, making it mechanically vulnerable at certain stages of skeletal development, with the location of the fracture shifting more proximally as the age of the child advances (1,5). The choice between operative and nonoperative treatment is based on the type of fracture and associated injuries (3,4).
Premature physeal closure is a complication associated with all epiphyseal fractures with the potential of leading to limblength discrepancy and/or angular deformities (2-4). Rare complications regarding proximal tibial fractures include compartment syndrome and vascular compromise (1,3,4).
The data on the characteristics of proximal tibial fractures and their treatment among children is limited (1-3). We calculated the population-based incidence and describe the complications and characteristics of proximal tibia fractures.
Patients and methods
New Children’s Hospital is the only tertiary-level hospital in greater Helsinki and the only hospital providing on-call pediatric orthopedic treatment in Finland. A special electronic pediatric fracture device, Kids’ Fracture Tool (New Children’s Hospital, Helsinki, Finland, and BCB Medical, Turku, Finland), has been used since 2014. When the patient is admitted to the emergency department, the patient’s data is entered into the registry and additional data on treatment and recovery is added at all phases of treatment. All children (< 16 years) diagnosed with proximal tibia fracture (ICD-10 code S82.1) during a 6-year period between 2014 and 2019 were included in the study. The number of under 16-year-olds during the study period was collected from statistical yearbooks of the City of Helsinki to estimate the annual incidence in Helsinki citizens and a subgroup analysis was done for adolescents (13- to 16-year-olds).
Demographic data including age, sex, mechanism of injury, method of treatment, and side of fractures as well as associated injuries was collected from the Kids’ Fracture Tool. The method of treatment was registered in 4 categories: casting in situ (C), closed reduction in an emergency department (ED), manipulation and casting under anesthesia (MUA + C), or surgical treatment (ST) with pins, sutures, screws, plate, or an external fixator.
Fracture morphology and associated fibula fracture type were retrospectively analyzed from primary radiographs of all patients. The Li-La method was used for inclusion criteria for identifying metaphyseal fractures (6). Fractures were divided into 3 categories according to location: intra-articular, tibial tuberosity, and extra-articular fractures. The tibial tuberosity fractures were classified according to Ogden (Figure 1) (7), tibial eminence fractures according to Meyers–McKeever (8), and physeal injuries according to Peterson (9).

Figure 1. Ogden fracture classification.
Statistics
Statistical analysis was performed with the use of SPSS (version 25.0; IBM Corp, Armonk, NY, USA). The Poisson distribution was utilized to calculate the 95% confidence intervals (CI) for the reported incidences. Results are presented as counts, percentages, and medians (range) for continuous, skewed variables.
Ethics, funding, and potential conflicts of interest
The study protocol was approved by the Helsinki University Hospital Review Board (365/13/03/03/2015). The authors received no funding for the research and/or publication of this article, and declare no conflicts of interest.
Results
During the study period (2014–2019), 241 children with a median age of 7.4 years (range 7 months–15.9 years) presented to our clinic with a proximal tibial fracture. Extra-articular fractures peaked at the age of 3 years and fractures of the tibial tuberosity and intra-articular fractures peaked at the age of 15 years (Figure 2). The most common fracture location was extra-articular (54%), followed by intra-articular (29%), and fractures of the tibial tuberosity (17%). 11% had complete closure of the physis, which presented at the time of fracture. Fracture distribution and methods of treatment are presented in Table 1 and Figure 3.
| Fracture types | n (%) |
| Intra-articular fractures | |
| ACL avulsion | 43 (18) |
| PCL avulsion | 6 (2) |
| Peterson IV | 3 (1) |
| Peterson V | 8 (3) |
| Complete articular a | 6 (2) |
| Segond + ACL rupture | 4 (2) |
| Total | 70 (29) |
| Tibial tubercle fractures | |
| Ogden Ia | 3 (1) |
| Ogden Ib | 6 (2) |
| Ogden IIa | 1 (0) |
| Ogden IIb | 8 (3) |
| Ogden IIIa | 3 (1) |
| Ogden IIIb | 5 (2) |
| Ogden IV | 14 (6) |
| Ogden V | 2 (1) |
| Total | 42 (17) |
| Extra-articular fractures | |
| Torus | 45 (19) |
| Greenstick | 35 (15) |
| Peterson I | 31 (13) |
| Peterson II | 13 (5) |
| Complete metaphyseal | 5 (2) |
| Total | 129 (54) |
| Total | 241 ( |
| a Given name for intra-articular fractures with extensively comminuted morphology that did not fit into any pediatric classification systems. | |
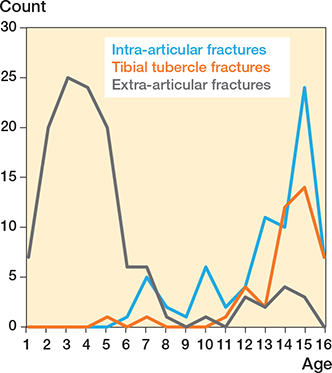
Figure 2. Distribution of fractures according to age.
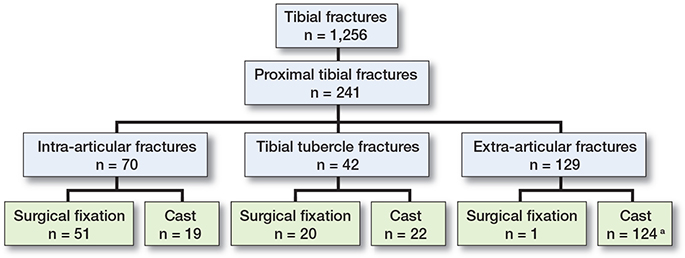
Figure 3. Patient flowchart. Total number of tibia fractures (ICD-10 codes S82.1-3, S82.5, S82.7 and S82.8). a 4 patients with extra-articular fractures were treated with limited weight-bearing only.
Intra-articular fractures
The median age of patients with intra-articular fractures was 13.9 years (range 6.5–15.9 years). There were 48 boys and 22 girls, yielding a ratio of 2.2:1. The most common type of intra-articular fracture was an ACL avulsion (61%, 43/70), with a median age of 13.1 years (range 6.7–15.9 years). This corresponds to a mean annual incidence of 3.4/100,000 children (range 2.5–4.5, CI 0.7–9.3) and 22/100 000 (range 15–25, CI 14–33) children in the age group of 13–16 years.
ACL-avulsion injuries were most frequently sustained in either sports-related accidents (25/43), traffic accidents (11/43), or during random falls (7/43). The most common types of avulsion fractures were Meyers–McKeever type II (11/43) and type IIIb (11/43). 7 patients had an associated meniscus injury. 3 ACL-avulsion patients presented with an associated Segond fracture, while none sustained meniscal and concomitant other ligament injuries simultaneously (Table 2).
| Meyers–McKeever | n | Orthosis | Sutures | Screws | Meniscus injury | Other ligament injury a | Segond fracture |
| I | 6 | 6 | |||||
| II | 11 | 5 | 6 | 2 | 2 | ||
| IIIa | 8 | 8 | 1 | 1 | 1 | ||
| IIIb | 11 | 11 | 1 | 1 | |||
| IV | 7 | 6 | 1 | 3 | 1 | 2 | |
| Total | 43 | 11 | 31 | 1 | 7 | 5 | 3 |
| a Other ligament injuries included: MCL rupture (n = 5) with 1 patient having concomitant MPFL-rupture (n = 1). | |||||||
All patients with Meyers–McKeever type III or IV fractures were treated operatively and all patients with type I fracture nonoperatively, while type II fractures were treated both operatively and nonoperatively (Table 2). Minimally displaced type II fractures (n = 5, ≤ 1 mm) were treated with an orthosis. 2 patients with dislocated type II fractures (5 and 6 mm) had anatomic reduction by hyperextension successfully performed and were treated with an orthosis. The rest of the displaced type II fractures (≥ 3mm) were managed surgically. 31/32 of the operatively treated patients were treated with pull-out sutures and 1 patient with closed physis was treated with cannulated screws. 24/32 patients underwent arthroscopy and mini-arthrotomy fixation and 8 had fixation done using mini-arthrotomy. Reduction of fractures was hampered by the interposition of the anterior horn of the meniscus or the transverse ligament in 6 patients. 4 patients with Segond fracture and ACL rupture initially approached conservatively had ACL reconstruction after physeal closure. 1 patient suffered from deep infection and 1 superficial infection was noted. 1 patient presented with postoperative arthrofibrosis, necessitating arthroscopic resection of excessive scar tissue that limited the patient’s range of motion.
6 patients presented to our clinic with a PCL avulsion fracture. 3 sustained injuries falling with a bike and 3 in motor vehicle accidents. All were treated surgically, 3 of which were treated with screws and the remaining 3 with pull-out sutures. 1 patient presented with concomitant MCL injury and medial meniscal tear, which was sutured.
8 patients presented to our clinic with Peterson V type fractures with a median age of 15.1 years (range 12.8–15.9 years). 6 of these patients presented with a distinct fracture morphology characterized by having both PCL and ACL in separate fragments. Of these 6 patients, 2 sustained other fractures and 2 sustained associated Segond fracture, 1 of which had a concomitant meniscal injury. All but 1 was treated surgically, and 1 was treated with manipulation under anesthesia (MUA+C = 1). The 2 patients with conventional Peterson V fractures were successfully treated with casting in situ (C = 2).
Furthermore, 6 polytrauma patients presented with comminuted intra-articular fractures (i.e., “Complete articular fractures,” Table 1), with closed epiphysis. All of these were treated with open reduction and plate fixation (ST = 6).
Tibial tubercle fractures
The median age of the 42 children with tibial tubercle fractures was 14.5 years (range 5.4–15.9 years). 39 were boys and 3 were girls, yielding a ratio of 13:1. A mean annual incidence of 3.8/100,000 children (range 2.1–5.5, CI 0.9–9.8) and 22/100,000 (range 15–25, CI 14–33)in the age group of 13–16 years was determined. Besides 1 moped accident, the mechanism of injury represented sports-related concentric or eccentric contraction of the quadriceps muscle, such as during initiation of a jump or when landing from one. Fractures representing this mechanism of injury were most frequently sustained while playing soccer, accounting for 16/42 of the cases.
The most common type was Ogden IV (14/42). 1 patient had an Ogden IV fracture with an anterior translation of the epiphysis. MRI was taken for 6 patients, 4 of whom presented with associated injuries. 1 Ogden Ib patient had an associated patellar tendon sleeve avulsion and 1 Ogden IV patient had partial ruptures of the popliteus and gastrocnemius muscles. 1 Ogden IIIa patient had a rupture of the MPFL and in addition, the MRI showed interposition of a periosteal sleeve that would have hampered anatomic reduction if treated nonoperatively. Finally, 1 Ogden IIIb patient presented with concomitant proximal PCL avulsion, meniscus injury, and an ACL rupture.
22 of the patients were treated conservatively (C = 20, and MUA+C = 2), with a median initial dislocation of 2 mm (range 0–11 mm). 11 patients were treated with cannulated screws and 9 patients with screws and concomitant sutures (ST = 20), with a median initial dislocation of 14 mm (range 2–75 mm).
None of the patients with tibia tubercle fracture suffered from acute compartment syndrome. During recovery, 1 patient re-fracture, requiring refixation of the avulsion fragment. 1 patient presented with thrombosis and 1 superficial infection was noted. 2 patients had a sore cast and 1 patient had removal of prominent hardware.
Extra-articular fractures
The median age of 129 children with extra-articular fractures was 3.7 years (range 7 months–15.2 years). 75 were boys and 54 were girls, yielding a ratio of 1.4:1. Extra-articular fracture types and distribution are presented in Table 1. The majority of these fractures occurred with younger children (116/129, < 11 years), with a median age of 3.5 years (range 7 months–10.3 years). The older patients (13/129, > 11 years) sustained injuries in more high-energy settings, such as motor vehicle accidents.
The most common mechanisms of injury were trampoline-related accidents (n = 71, 55%), followed by fall on play-ground (n = 20, 16%), and winter activity-related accidents (n = 16, 13%). 8 children sustained injury in miscellaneous falls (n = 8, 6%).
3 patients had other injuries, with 1 having bilateral metaphyseal fractures, and 1 had bilateral distal tibia fractures. 1 patient (15.2 years old) presented with a floating knee with multiple other fractures from a snowmobile accident. The patient underwent fasciotomy and was treated with external fixation. Except for the patient with a floating knee, all patients were treated nonsurgically. 4 patients were treated with limited weight-bearing and 124 patients with cast in situ.
Discussion
241 children with proximal tibial fractures presented with a bimodal fracture distribution in relation to age, with extra-articular fractures peaking at the age of 3 years and tibial tubercle and intra-articular fractures at the age of 15, reflecting the developmental changes in the proximal tibia that alter fracture susceptibility increasingly proximally as osseous maturity proceeds (1,3,5). The fracture distribution is consistent with previously reported findings (5,10).
The risk of developing compartment syndrome has been described with tibial tubercle avulsion patients and proximal physeal fracture patients. Tibial tubercle avulsion patients are predisposed to a risk of developing compartment syndrome as the anterior tibial recurrent artery can be compromised whilst sustaining injury (1,11,12). Occurrences as high as 17%–20% have been reported in some series (13,14); meanwhile, an overall occurrence of 4% was determined by Pretell-Mazzini et al. in their systematic review (1). None of our 42 patients with tibial tubercle avulsion fracture developed compartment syndrome. Regarding proximal tibial physeal fractures according to Peterson classification, the rate of acute neurovascular injury has been reported to be approximately 14% (4), with the popliteal artery being a major concern (2-4). Compartment syndrome may occur with these fractures due to damage to the popliteal artery, mechanical blockage of surrounding vascular structures by a displaced fracture, or collateral damage to soft tissues in high-energy injuries (4). Few examples of compartment syndromes with proximal physeal fractures have been reported (2,5,15,16). In our cohort, the incidence of compartment syndrome was very low (0.4%) in all children with proximal tibia fractures. The only patient who suffered from compartment syndrome among our patients sustained a high-energy injury with a floating knee.
The most common type of intra-articular fracture was an ACL avulsion (43/70), which is seen to occur as the incompletely ossified epiphysis is more prone to failure than the ACL in pediatric patients (3,17). The median age of our patients was 13.1 years, which is similar to figures presented before, as Mubarak et al. reported a mean age of 10 and 12 years for girls and boys (5), and Skak et al. reported a median age of 12 (10).
Tibial tubercle avulsions occurred quite exclusively among boys (39/42), which is consistent with earlier reports, reflecting their higher participation in sports as well as later epiphyseal closure (1,12,18). We were able to determine an annual incidence among Helsinki citizens of 3.8/100,000 children and 21/100,000 children in the age group of 13–16 years, which to the best of our knowledge has not been reported previously. Operative treatment is suggested for all fractures displaced more than 2–3 mm or of an intra-articular nature (4). Our patients did not entirely concur with this, as our nonoperatively treated patients had a dislocation range of 0–11 mm, with 4 patients having initial dislocation exceeding that of 2–3 mm. However, each healed successfully based on clinical evaluation.
Extra-articular fractures constituted 129 patients with a median age of 3.7 years and the most common injury mechanism was trampoline-related accident (70/129). Consistently, Mubarak et al. reported trampoline-related accidents as the prototypic injury mechanism in children with metaphyseal greenstick fractures with a mean age of 3.8 years (5), and Skak et al. described similar age distribution with torus, greenstick, and complete metaphyseal fractures (10). Overall, extra-articular fractures were treated conservatively with one exception.
Limitations
This is a retrospective study, though all data was registered prospectively into the Kids’ Fracture Tool and the results should be interpreted with caution for several reasons. Some children from the Helsinki area might have been treated elsewhere, which may affect the incidence. No studies have been performed to analyze the completeness of the register in comparison with the Care Register for Health Care but we are confident that all patients treated at our clinic are registered in the system. Second, this study represents an epidemiological investigation on the incidence, characteristics, and treatment principles in pediatric proximal tibia fractures and we did not aim to describe treatment outcomes. Third, socioeconomic data on the patients is not included in the register.
Conclusion
Proximal tibial fractures present with a bimodal distribution, with extra-articular fractures peaking at the age of 3 years, and fractures of the tibial tuberosity and intra-articular fractures peaking at the age of 15 years. Additionally, associated compartment syndrome and vascular compromise was not as common as previously reported.
- Pretell-Mazzini J, Kelly D M, Sawyer J R, Esteban E MA, Spence D D, Warner W C Jr, et al. Outcomes and complications of tibial tubercle fractures in pediatric patients: a systematic review of the literature. J Pediatr Orthop 2016; 36(5): 440-6. doi: 10.1097/BPO.0000000000000488.
- Burkhart S S, Peterson H A. Fractures of the proximal tibial epiphysis. J Bone Joint Surg Am 1979; 61(7): 996-1002. doi: 10.2106/00004623197961070-00005.
- Little R M, Milewski M D. Physeal fractures about the knee. Curr Rev Musculoskelet Med 2016; 9(4): 478-86. doi: 10.1007/s12178-016-93707.
- Rockwood C A, Beaty J H, Kasser J R. Rockwood and Wilkins’ fractures in children. 7th ed. Philadelphia, PA: Wolters Kluwer/Lippincott, Williams & Wilkins; 2010: xiii. 1076 p.
- Mubarak S J, Kim J R, Edmonds E W, Pring M E, Bastrom T P. Classification of proximal tibial fractures in children. J Child Orthop 2009; 3(3): 191-7. doi: 10.1007/s11832-009-0167-8.
- Schneidmuller D, Roder C, Kraus R, Marzi I, Kaiser M, Dietrich D, et al. Development and validation of a paediatric long-bone fracture classification: a prospective multicentre study in 13 European paediatric trauma centres. BMC Musculoskelet Disord 2011; 12: 89. doi: 10.1186/1471-2474-12-89.
- Ogden J A, Tross R B, Murphy M J. Fractures of the tibial tuberosity in adolescents. J Bone Joint Surg Am 1980; 62(2): 205-15.
- Meyers M H, Mc K F. Fracture of the intercondylar eminence of the tibia. J Bone Joint Surg Am 1959; 41-A(2): 209-20; discussion 220-2.
- Peterson H A. Physeal fractures, Part 3: Classification. J Pediatr Orthop 1994; 14(4): 439-48. doi: 10.1097/01241398-199407000-00004.
- Skak S V, Jensen T T, Poulsen T D, Sturup J. Epidemiology of knee injuries in children. Acta Orthop Scand 1987; 58(1): 78-81. doi: 10.3109/17453678709146348.
- Pape J M, Goulet J A, Hensinger R N. Compartment syndrome complicating tibial tubercle avulsion. Clin Orthop Relat Res 1993; (295): 201-4. 12.
- Rodriguez I, Sepulveda M, Birrer E, Tuca M J. Fracture of the anterior tibial tuberosity in children. EFORT Open Rev 2020; 5(5): 260-7. doi: 10.1302/2058-5241.5.190026.13.
- Frey S, Hosalkar H, Cameron D B, Heath A, Horn D B, Ganley T J. Tibial tuberosity fractures in adolescents. J Child Orthop 2008; 2(6): 469-74. doi: 10.1007/s11832-008-0131-z.
- Polakoff D R, Bucholz R W, Ogden J A. Tension band wiring of displaced tibial tuberosity fractures in adolescents. Clin Orthop Relat Res 1986; (209): 161-5.
- Ceylan H, Yildirim C, Korkmaz M, Atlihan D, Cetinus M E. Adolescent proximal tibia physeal injury. J Acad Res Med 2016; 6(3): 196-9. doi: 10.5152/jarem.2015.889.
- Shelton W R, Canale S T. Fractures of the tibia through the proximal tibial epiphyseal cartilage. J Bone Joint Surg Am 1979; 61(2): 167-73. doi: 10.2106/00004623-197961020-00002.
- LaFrance R M, Giordano B, Goldblatt J, Voloshin I, Maloney M. Pediatric tibial eminence fractures: evaluation and management. J Am Acad Orthop Surg 2010; 18(7): 395-405.
- McKoy B E, Stanitski C L. Acute tibial tubercle avulsion fractures. Orthop Clin North Am 2003; 34(3): 397-403. doi: 10.1016/s00305898(02)00061-5.