The indication for aseptic revision TKA does not influence 1-year outcomes: an analysis of 178 full TKA revisions from a prospective institutional registry
Siri B WINTHER 1, Gøril Lund SNORROEGGEN 1, Jomar KLAKSVIK 1, Olav A FOSS 1,2, Tarjei EGEBERG 1, Tina Strømdal WIK 1,2, and Otto S HUSBY 1,2
1 Department of Orthopaedic Surgery, St Olav’s Hospital HF, Trondheim; 2 Department of Neuromedicine and Movement Science, Faculty of Medicine and Health Science, Norwegian University of Science and Technology, Trondheim, Norway
Background and purpose — Outcomes following revision total knee arthroplasty (TKA) may depend on the indication for revision surgery. We compared pain, patientreported outcome measures (PROMs), and patient satisfaction among different indications for an aseptic TKA revision.
Patients and methods — This was a retrospective study of prospective data from an institutional registry of 178 primary TKAs revised between 2012 and 2020. Patients were grouped by the main reason for their revision: loosening, malposition, instability, or stiffness. Pain during mobilization and at rest (NRS 0–10), physical function (KOOS-PS and KSS), and quality of life (EQ-5D) were surveyed preoperatively and at 2 months and 1 year postoperatively. Patient satisfaction was evaluated through questions related to knee function and their willingness to undergo the same surgery again at 1-year follow-up.
Results — Pain and PROMs improved in all groups and did not differ statistically significantly between the 4 groups at 1-year follow-up, but equivalence for pain was not confirmed between groups. Overall, pain during mobilization improved by 2.4 (95% CI 1.9–3.0) at 1-year followup, which was both clinically and statistically significant. Improvements were seen within 2 months of surgery, with no further improvements seen 1 year postoperatively. Approximately 2/3 of patients reported that their knee function had improved and would undergo the same surgery again, at 1-year follow-up.
Conclusion — Statistically significant and clinically relevant improvements in pain and PROMs were seen in all 4 revision groups 1 year after revision TKA. These results may assist clinicians and patients during preoperative counselling.
Citation: Acta Orthopaedica 2022; 93: 819–825. DOI http://dx.doi.org/10.2340/17453674.2022.4878.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-03-25. Accepted: 2022-09-20. Published: 2022-10-19.
Correspondence: siri.bjorgen@ntnu.no
All authors contributed to study planning and data interpretation. TE and OSH performed the surgeries. GL and SBW contributed to data registration. JK and OF performed the data analyses. All authors contributed to revising the draft manuscript written by SBW.
Acta thanks Henrik Husted for help with peer review of this study. Handling co-editors: Nils P Hailer and Philippe Wagner
As the number of total knee arthroplasties (TKA) performed per year worldwide increases, so has the demand for revision TKA (1). Although the clinical outcomes following revision TKA are good, they are inferior to those after primary TKA (2). The main goal of both primary and revision arthroplasty surgery is a satisfied patient. This goal can be accomplished by setting realistic expectations for clinical improvement, and achieving an acceptable level of postoperative pain and function (3). Preoperative patient counseling on expected outcomes is important to setting realistic recovery goals (4,5), and is central to the preoperative shared decision-making process (6,7).
Excluding infections and acute events, the main indications for revision TKA are implant loosening, instability, pain, polyethylene wear, stiffness, implant failure, and implant malposition (8). Previous studies have presented different conclusions as to whether the reason for a TKA revision influences clinical postoperative outcomes (9-13). Although it is difficult to compare studies on revision TKA due to methodological discrepancies and the use of diverse outcome measures, a recent review reported a tendency toward revision TKA due to stiffness yielding the lowest outcome scores (14).
The extent to which the indication for the revision TKA influences clinical outcomes is unclear. Therefore, we evaluated the results of several different domains in a standardized fast-track clinical setting with a few highly skilled revision TKA surgeons. More specifically, we evaluated how pain, function, quality of life, and patient satisfaction at 1-year follow-up were related to the indication for an aseptic revision TKA using a registry-based cohort at a single large-volume hospital department.
Patients and methods
Design
This was an observational cohort study using prospectively recorded data from an institutional quality registry for hip and knee arthroplasty patients who underwent a fast-track clinical course at our orthopedic department. Some of the results from the first 16 revision total TKAs included in the registry have previously been published in a study that describes the establishment of the fast-track patient course (15). 2 senior orthopedic surgeons operated or assisted on all revision procedures.
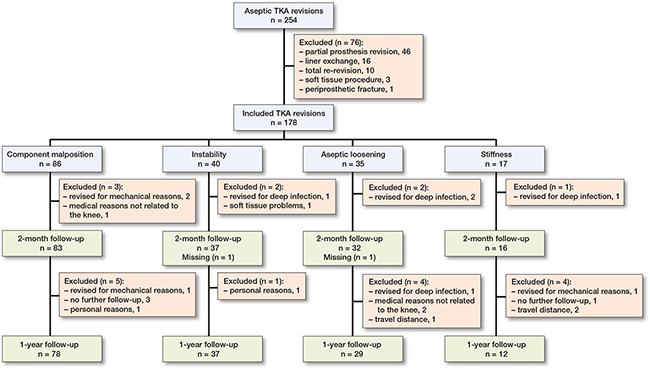
Patients (Figure 1, Table 1)
All elective aseptic revision TKA surgeries performed at St Olav’s University Hospital between March 2012 and May 2020 were screened for study eligibility. Inclusion criteria were TKA revisions that required replacement of both the tibial and femoral components. TKA re-revisions were excluded. Infections and periprosthetic fractures were not included due to the elective nature of the fast-track clinical course.
Patients were allocated into groups based on the 4 most frequent indications for aseptic revision surgery: loosening, component malposition, instability, and stiffness, based on previously publicized work (11). We consider pain to be a symptom caused by the underlying indication for revision surgery. Aseptic loosening was defined as loosening without signs of infection or polyethylene wear with emerging bone loss. Malalignment was defined as the indication if there were a malposition or malrotation of 1 or both components. Instability was the main indication when patients experienced instability without any signs of component malposition. Stiffness was the main indication if the knee flexion was < 90° without any other reasons present, or if the knee flexion was < 70°, even if the stiffness was caused by any of the 3 other indications. Patients were placed into groups based on the main reason for their revision. For patients with more than 1 indication for surgery, a group of experienced orthopedic knee surgeons discussed and agreed on the main indication.
Fast-track clinical pathway
All patients were treated according to a well-established standardized clinical fast-track patient course. Pain treatment consisted of spinal anesthesia, local infiltration, and systemic analgesics. For details see Winther et al. (15).
Surgical procedures and implants
Three levels of constrained implants from the same revision knee system were used for the revision surgeries (NexGen, Zimmer Biomet, Warsaw, IN, USA). Preoperative planning included an evaluation of stability demands in order to select a posterior stabilized (PS), constrained condylar (LCCK), or rotating hinge (RHK) knee. Stem lengths of 100 mm or 150 mm were combined with both the femoral and tibial components.
Data collection and outcomes
Data was prospectively collected at the preoperative outpatient clinic, during hospitalization, and twice after discharge: at 2-months and 1-year follow-up. The primary outcome was pain during mobilization at 1 year, and pain improvement from before surgery to 1-year follow-up.
Pain during mobilization and at rest was reported using the numeric rating scale (NRS 0–10) (0 no pain, 10 worst pain imaginable). Minimal clinically important improvement (MCII) is a threshold that defines the minimum improvement relevant to the patient. Scores above this limit are considered a clinically significant improvement. The patient acceptable symptom state (PASS) is the state beyond which the patient considers the outcome satisfactory (16). The MCII and PASS thresholds for pain were 1.7 and 4.6 based on previous publications (16). Patients achieving these thresholds are referred to as responders. Equivalence tests were performed between groups on pain variables to see if the group differences were small enough to be considered equivalent in a clinical perspective. The specified MCII value of 1.7 was used to define the boundaries of equivalence for both pain at rest and pain during mobilization.
Secondary outcomes were pain at rest, the disease-specific KSS, and KOOS-PS, and the generic EQ-5D.
Self-perceived satisfaction at 1-year follow-up was evaluated using 2 anchor questions: “How does the leg that was operated on work today compared with before surgery?” and “Based on your experience to date, would you go through the surgery again?”.
Time from index surgery, surgery time, length of hospital stay (LOS), knee flexion, and postoperative complications were also registered.
Statistics
A generalized linear mixed model was used to analyze pain during mobilization preoperatively and at 2 months and 1 year after surgery for the 4 revision groups. The time points and 4 patient groups were modelled as fixed factors. Based on clinical considerations, BMI was included as a covariate in the analysis. A random subject intercept was included. The data was modelled with an identity link function and histograms were used to verify residual normality. The numbers presented for mean pain during mobilization are model estimates with 95% confidence intervals (CI). Statistical analyses were performed using SPSS v27 (IBM Corp, Armonk, NY, USA). Equivalence between groups was assumed when the 90% confidence interval of the group differences fell within the interval defined by the MCII boundaries. The aseptic loosening group was used as a reference group.
Ethics, data sharing, funding, and conflicts of interest
The study was approved by the regional ethics committee (REC central) (approval no. 123645) and the National Archive and Center for Research Data (approval no. 480820). All methods accorded with the relevant guidelines and regulations. Patients were informed about the registry and gave written informed consent to allow data related to their knee revision surgery to be used for scientific purposes before they were included. Grouped data or tables of data without possibility of identification are available. The study did not receive any grant or funding and the authors declare that they have no conflicts of interests.
Results
Patients (Figure 1)
178 patients were included, of whom 86 were revised due to malposition, 40 for instability, 35 for aseptic loosening, and 17 due to stiffens. 24 patients had more than 1 reason for failure (22 with 2 reasons and 2 with 3 reasons). 156 (88%) patients completed the 1-year follow-up.
Outcomes
Changes in pain during mobilization from preoperatively to 1-year follow-up (Figure 2)
The mean pain level was statistically and clinically significantly reduced in all groups from preoperatively until 1-year follow-up by 2.4 (CI 1.9–3.0). The mean reduction by group was 3.4 (CI 2.4–4.5) in the aseptic loosening group, 2.4 (CI 1.7–3.0) in the malposition group, 2.2 (CI 1.2–3.1) in the instability group, and 1.8 (CI 0.1–3.5) in the stiffness group. Overall mean pain statistically significantly increased by 0.7 (CI 0.1–1.3) from 2 months postoperatively until 1-year follow-up, but no statistically significant within-group increase was found (p ≥ 0.05).
Pain during mobilization at 1-year follow up (Figure 2)
At 1-year follow-up, the overall mean pain was 4.3 (CI 3.7–4.8). The mean pain by group was 3.4 (CI 2.5–4.4) in the aseptic loosening group, 4.5 (CI 4.0–5.1) in the malposition group, 4.7 (CI 3.9–5.6) in the instability group, and 4.3 (CI 2.8–5.9) in the stiffness group. There were no statistically significant between-group differences, but the equivalence tests (Figure 3) indicate clinically meaningful pain difference in favor of the aseptic loosening group.
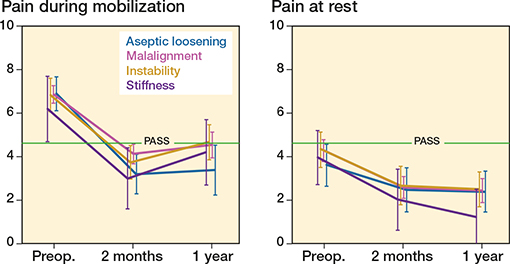
Figure 2. Descriptive values of pain during mobilization and pain at rest of 4 different revision TKA groups preoperatively and at 2-month and 1- year follow-up. PASS = patient acceptable symptom state.
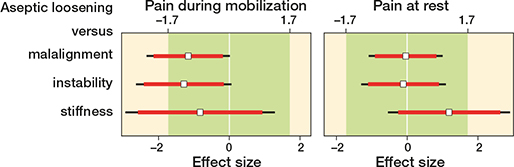
Figure 3. Equivalence plot of pain differences during mobilization and at rest for the groups at 12-month follow-up. Mean differences (white squares) with 90% confidence intervals (red lines) and 95% confidence intervals (black lines). Green area represents equivalence; differences smaller than an effect size considered worthwhile.
Overall, the number of MCII responders was similar with respect to pain during mobilization vs. pain at rest whereas the number of PASS responders was higher for pain at rest than pain during mobilization.
Patient satisfaction at 1-year follow-up (Figure 4)
The overall number of patients who reported improved knee function was between 61% and 76%, and 66–82% reported that they would have the same surgery again based on their experience.

Figure 4. Patient satisfaction related to knee function and willingness to have the surgery in the 4 different revision TKA groups at 1-year follow-up.
PROMs (Figures 2, 5–6, see Supplementary data)
Pain at rest, KOOS-PS, KSS knee and function scores, and EQ-5D were improved at 1-year follow-up compared with preoperative scores. No statistically significant differences were noted between the groups in any parameter at 1-year follow up, as demonstrated by overlapping CI. However, the equivalence tests on pain at rest indicate clinically meaningful pain difference in favor of the stiffness group (Figure 3).
Time from primary TKA to revision, surgery time, LOS, preoperative, and 1-year follow-up knee flexion and complications are presented in Table 2.
Discussion
Patient-reported outcomes at 1-year follow-up did not differ significantly among the 4 indication groups, but equivalence testing on pain variables could not rule out clinically significant differences between some groups. Pain was statistically significantly and clinically relevantly decreased, and PROMs improved substantially throughout the cohort at 1-year follow-up. Improvements were primarily seen in the first 2 months after surgery, with no further improvement at 1-year follow-up. The overall mean reduction in pain scores was above the MCII threshold and within the PASS level. Our findings are similar to those that report good results following revision TKA, although they are inferior to outcomes following primary TKA (2,4,13,17,18).
The pain levels seen in our study are in line with prior work that discussed revision TKA (4,11,17), with clinically significant pain reduction and an acceptable patient symptom state. A notable finding is that the overall mean pain during mobilization statistically significantly increased from 2 months to 1 year by 0.7. No statistically significant withingroup increases were observed, but equivalence tests indicate pain levels during mobilization in favor of the aseptic loosening group. Other work has also found that improvements occur in the early phase following revision TKA surgery (11). At 8-week follow-up, the patients are still in an early phase following surgery, which means that they are less active, some might still be using crutches, and some are also probably on pain medication. At 1-year follow-up, the activity level and expectations concerning pain and function are probably higher than at 8 weeks, which might result in a higher self-perceived pain level at 1 year. Stem pain may also be a significant activity-related problem due to mechanical stress between the intramedullary nail in the tibial and femoral components and the bone (19). KSS function increased during the same period, hence the increase in pain from 2 to 12 months postoperatively might be explained by increased physical activity during that period. The pain levels at 1 year correspond well with previous results after TKA revision surgery but are somewhat better for the stiffness group in our study. Other studies suggest that patients with stiffness should lower their expectations for pain relief after revision surgery, as pain has been found to remain high in this group (14,20).
Functional outcome and pain are important factors related to patient satisfaction following TKA, and the latter has been found to be the strongest predictor of dissatisfaction (3). The PASS threshold has previously been found to correspond with satisfaction (21). In our study, 74% of the patients would have undergone the surgery again based on their knowledge of their 1-year follow-up outcome, and 66% were PASS responders when combining pain at rest with pain during mobilization. The overall number of MCII responders was 56% for pain at rest and during mobilization, which is lower than the 66% who reported improved function (Figures 4 and 7). This is similar to previous studies following aseptic revision TKA (11,13,22). Persistent pain following primary TKA is a common reason for patients to consult with an orthopedic surgeon regardless of the underlying reason for their failure (23), and pain has been proposed to be the most important outcome for the patient.
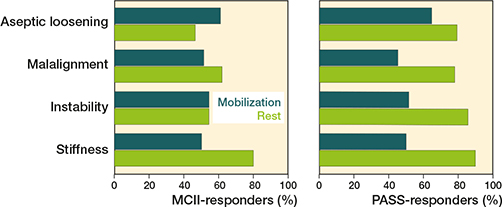
Figure 7. Proportion of MCII- (left) and PASS- (right) responders at 1-year follow-up. Results are stratified into the 4 different revision TKA groups.
Several factors might contribute to further improve the results following revision TKA: first, it is important to inform the patients preoperatively about the expected inferior results following revision surgery and to empower the patients so that they can take an active part in the decision-making. Also, patients should be carefully selected so that patients with minor potential for improvement are advised against having the revision surgery. Decreased time to revision in case of a failed primary TKA due to malposition has previously been demonstrated to yield good results (24). As a part of the follow-up at our orthopedic department, we have recently implemented a routine to identify all patients who are dissatisfied with their outcomes following primary and revision TKA, and thereby we might be able to intervene earlier, which could improve the outcomes. Shorter time to revision might also be important to prevent further deconditioning induced by delayed treatment (25), regardless of indication. An early intensive rehabilitation protocol could have prevented the vicious cycle of inactivity induced by the failed TKA and thus led to improved 1-year outcomes following revision TKA. Increased use of hinged implants in the case of instability and stiffness combined with more coned or shorter stems might also prevent stem pain and improve the outcomes (26-28).
While MCII and PASS evaluate the results of each outcome separately, satisfaction reflects the overall patient experience. Our findings therefore indicate that patient satisfaction is a multifactorial parameter that encompasses more than pain and function, and also includes the patient’s expectations influenced by their involvement in the preoperative planning. Through the fast-track preoperative information, patients are motivated to actively participate in the planning, which has been found to have a positive impact on the results (29). Thereby they are prepared for early mobilization, short LOS, and being discharged to their homes as soon as the specific discharge criteria are fulfilled.
Physical function and health-related quality of life scores as measured by the KSS, KOOS-PS, and EQ-5D in our study are similar to those reported by prior analysis of revision TKAs (4,13,14,22,30). Although all groups showed improvements at their 1-year follow-up that were above the MCII threshold for the outcome scores, neither group reached the PASS level in any outcome other than pain at rest and pain during mobilization (17,21,31) (Figures 2, 5–6, see Supplementary data). Nevertheless, a high number of patients were satisfied with their outcome, which suggests that their expectations were met. All patients in the quality registry and hence in our study went through the fast-track clinical course with thorough preoperative information (15), which could explain these findings.
Stiffness has been associated with the worst outcomes following revision TKA (11,12,14). We did not find any statistically significant between-group differences, but equivalence tests indicate pain levels at rest in favor of the stiffness group. Even though surgery was a reasonable option for most patients with a stiff knee, its benefits have been found to be modest (14,20). The present study reported better pain, KSS functional scores, and patient satisfaction compared with previous studies that evaluated revision due to stiffness (13,14,20). Further, a mean knee flexion of 105° at 1 year is higher than previously reported range of motion, and only 50% of the articles included in a recent review reported average knee flexion of over 90° at final follow-up in patients revised due to stiffness (14). Knee flexion has previously been found to have important functional implications that impact patient satisfaction (20), which is supported by our findings. From the fast-track setting, all patients are well informed about risks and post-operative outcomes. This has especially been emphasized for patients experiencing a stiff knee. The patients are well prepared and motivated to have the revision surgery with the concomitant effort required to make a full recovery. It is highlighted that they must take an active part in the recovery and that their effort is important in order to optimize the outcome. It is emphasized that a lot of work is required in order to regain acceptable function and flexibility, which might have improved the results.
There are limitations to our study. First, more than 1 indication for the revision TKA was present in 24 of the 178 surgeries. Second, the stiffness group is rather small, including only 17 patients. Third, formal tests of equivalence have been conducted only on the pain variables and, consequently, the generalizability of the other PROMs is uncertain. The strength of the study is that a small number of highly experienced orthopedic surgeons performed or assisted on all revisions at a single large-volume hospital department with a standardized fast-track patient course (15). Fast track has previously been demonstrated to improve outcomes following both primary and revision TKA through optimized evidence-based treatment in all aspects of the pathway, from preoperative information until follow-up (29,32). In our orthopedic department, all elective aseptic revisions are implemented on the fast-track patient course, which could explain our findings of a relatively high number of satisfied patients with acceptable pain levels. A wide range of PROMs were also included to provide an extensive description of outcomes following TKA revision in several dimensions. We also had a high response rate of 71–93% in all groups at 1-year follow-up, which is above the acceptable response level of 60–70% when reporting PROMs (4).
Our findings support the importance of increased knowledge through patient counselling, which is the foundation of the informed shared decision-making process and may improve patient satisfaction given the higher likelihood of satisfying their expectations.
In conclusion, all revision TKA groups had statistically significant and clinically relevant improved pain, function, and quality of life at 1-year follow-up. Mean pain after revision TKA was below the PASS limit, and 2/3 of patients reported that they were satisfied with their outcome. These results could be useful in the shared preoperative decision-making of patients who are considering revision TKA.
- Hamilton D F, Howie C R, Burnett R, Simpson A H, Patton J T. Dealing with the predicted increase in demand for revision total knee arthroplasty: challenges, risks and opportunities. Bone Joint J 2015; 97-b(6): 723-8.
- Roman M D, Russu O, Mohor C, Necula R, Boicean A, Todor A, et al. Outcomes in revision total knee arthroplasty (Review). Exp Ther Med 2022; 23(1): 29.
- Kahlenberg C A, Nwachukwu B U, McLawhorn A S, Cross M B, Cornell C N, Padgett D E. Patient satisfaction after total knee replacement: a systematic review. HSS J 2018; 14(2): 192-201.
- Piuzzi N S. Patient-reported outcome measures (pain, function, and quality of life) after aseptic revision total knee arthroplasty. J Bone Joint Surg Am 2020; 102(20): e114.
- Baier C, Lüring C, Schaumburger J, Köck F, Beckmann J, Tingart M, et al. Assessing patient-oriented results after revision total knee arthroplasty. J Orthop Sci 2013; 18(6): 955-61.
- Neuprez A, Delcour J P, Fatemi F, Gillet P, Crielaard J M, Bruyere O, et al. Patients’ expectations impact their satisfaction following total hip or knee arthroplasty. PLoS One 2016; 11(12): e0167911.
- Noble P C, Fuller-Lafreniere S, Meftah M, Dwyer M K. Challenges in outcome measurement: discrepancies between patient and provider definitions of success. Clin Orthop Relat Res 2013; 471(11): 3437-45.
- Lewis P L, Robertsson O, Graves S E, Paxton E W, Prentice H A, W-Dahl A. Variation and trends in reasons for knee replacement revision: a multi-registry study of revision burden. Acta Orthop 2021; 92(2): 181-8. 9.
- Hardeman F, Londers J, Favril A, Witvrouw E, Bellemans J, Victor J. Predisposing factors which are relevant for the clinical outcome after revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2012; 20(6): 1049-56.
- Bieger R, Kappe T, Fraitzl C R, Reichel H. The aetiology of total knee arthroplasty failure influences the improvement in knee function. Arch Orthop Trauma Surg 2013; 133(2): 237-41.
- van Kempen R W, Schimmel J J, van Hellemondt G G, Vandenneucker H, Wymenga A B. Reason for revision TKA predicts clinical outcome: prospective evaluation of 150 consecutive patients with 2-years followup. Clin Orthop Relat Res 2013; 471(7): 2296-302.
- van Rensch P J H, Hannink G, Heesterbeek P J C, Wymenga A B, van Hellemondt G G. Long-term outcome following revision total knee arthroplasty is associated with indication for revision. J Arthroplasty 2020; 35(6): 1671-7.
- Baker P, Cowling P, Kurtz S, Jameson S, Gregg P, Deehan D. Reason for revision influences early patient outcomes after aseptic knee revision. Clin Orthop Relat Res 2012; 470(8): 2244-52.
- Cromheecke M, Missinne M, Van Onsem S, Victor J, Arnout N. Efficacy of total knee arthroplasty (TKA) revision surgery depends upon the indication for revision: a systematic review. Acta Orthop Belg 2020; 86(4): 663-77. 15.
- Winther S B, Foss O A, Wik T S, Davis S P, Engdal M, Jessen V, et al. 1-year follow-up of 920 hip and knee arthroplasty patients after implementing fast-track. Acta Orthop 2015; 86(1): 78-85.
- Tubach F, Ravaud P, Martin-Mola E, Awada H, Bellamy N, Bombardier C, et al. Minimum clinically important improvement and patient acceptable symptom state in pain and function in rheumatoid arthritis, ankylosing spondylitis, chronic back pain, hand osteoarthritis, and hip and knee osteoarthritis: results from a prospective multinational study. Arthritis Care Res (Hoboken) 2012; 64(11): 1699-707.
- Stirling P, Middleton S D, Brenkel I J, Walmsley P J. Revision total knee arthroplasty versus primary total knee arthroplasty: a matched cohort study. Bone Jt Open 2020; 1(3): 29-34.
- Postler A E, Beyer F, Wegner T, Lutzner J, Hartmann A, Ojodu I, et al. Patient-reported outcomes after revision surgery compared to primary total hip arthroplasty. Hip Int 2017; 27(2): 180-6.
- Albino R B, Santos L S, Gobbi R G, Iamaguchi M, Demange M K, Tirico L E, et al. Pain at the tip of the stem after revision total knee arthroplasty. Rev Bras Ortop 2012; 47(1): 73-6. 20.
- Cohen J S, Gu A, Lopez N S, Park M S, Fehring K A, Sculco P K. Efficacy of revision surgery for the treatment of stiffness after total knee arthroplasty: a systematic review. J Arthroplasty 2018; 33(9): 3049-55.
- Naal F D, Impellizzeri F M, Lenze U, Wellauer V, von Eisenhart-Rothe R, Leunig M. Clinical improvement and satisfaction after total joint replacement: a prospective 12-month evaluation on the patients’ perspective. Qual Life Res 2015; 24(12): 2917-25.
- Luttjeboer J S, Bénard M R, Defoort K C, van Hellemondt G G, Wymenga A B. Revision total knee arthroplasty for instability-outcome for different types of instability and implants. J Arthroplasty 2016; 31(12): 2672-6.
- Mandalia V, Eyres K, Schranz P, Toms A D. Evaluation of patients with a painful total knee replacement. J Bone Joint Surg Br 2008; 90(3): 265-71.
- Lakstein D, Zarrabian M, Kosashvili Y, Safir O, Gross A E, Backstein D. Revision total knee arthroplasty for component malrotation is highly beneficial: a case control study. J Arthroplasty 2010; 25(7): 1047-52.
- Sharma R, Ardebili M A, Abdulla I N. Does rehabilitation before total knee arthroplasty benefit postoperative recovery? A systematic review. Indian J Orthop 2019; 53(1): 138-47.
- van Rensch P J H, Heesterbeek P J C, Hannink G, van Hellemondt G G, Wymenga A B. Improved clinical outcomes after revision arthroplasty with a hinged implant for severely stiff total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2019; 27(4): 1043-8.
- Al-Jabri T, Brivio A, Maffulli N, Barrett D. Management of instability after primary total knee arthroplasty: an evidence-based review. J Orthop Surg Res 2021; 16(1): 729.
- Jacquet C, Ros F, Guy S, Parratte S, Ollivier M, Argenson J N. Trabecular metal cones combined with short cemented stem allow favorable outcomes in aseptic revision total knee arthroplasty. J Arthroplasty 2021; 36(2): 657-63.
- Husted H, Holm G, Jacobsen S. Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop 2008; 79(2): 168-73.
- Larsen J B, Mogensen L, Arendt-Nielsen L, Madeleine P. Intensive, personalized multimodal rehabilitation in patients with primary or revision total knee arthroplasty: a retrospective cohort study. BMC Sports Sci Med Rehabil 2020; 12: 5.
- Walters S J, Brazier J E. Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual Life Res 2005; 14(6): 1523-32.
- Kehlet H, Soballe K. Fast-track hip and knee replacement: what are the issues? Acta Orthop 2010; 81(3): 271-2.
Supplementary data
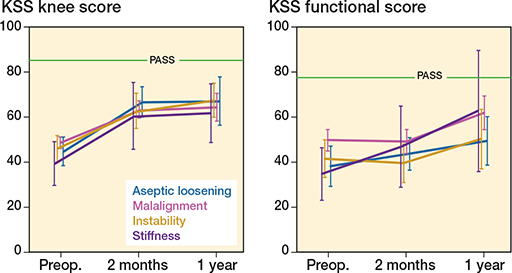
Figure 5. Descriptive values of the KSS knee score and functional score in the 4 different revision TKA groups preoperatively and at 2-month and 1-year follow-up. PASS = patient acceptable symptom state.
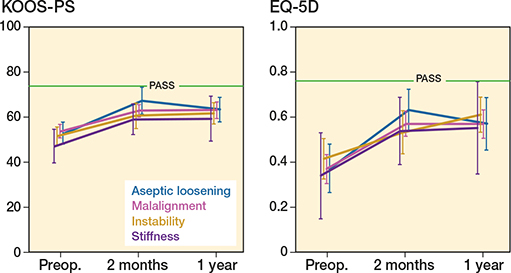
Figure 6. Descriptive values of the KOOS-PS and EQ-5D in the 4 different revision TKA groups preoperatively and at 2-month and 1-year-follow-up. PASS = patient acceptable symptom state.