Impact of the COVID-19 lockdown on patient-reported outcome measures in Dutch hip and knee arthroplasty patients
Joshua M BONSEL 1, Lichelle GROOT 1,2, Abigael COHEN 1, Jan A N VERHAAR 1, Maaike G J GADEMAN 2,3, Anneke SPEKENBRINK-SPOOREN 4, Gouke J BONSEL 5, and Max REIJMAN 1
1 Department of Orthopaedics and Sports Medicine, Erasmus Medical Center, University Medical Center Rotterdam; 2 Department of Orthopaedics, Leiden University Medical Center; 3 Department of Clinical Epidemiology, Leiden University Medical Center; 4 Dutch Orthopaedic Registry (Landelijke Registratie Orthopedische Interventies [LROI]); 5 Department of Public Health, Erasmus Medical Center, University Medical Center Rotterdam, The Netherlands
Background and purpose — During the first COVID-19 lockdown elective surgery was greatly reduced. Prioritization of patients with greater need and expected benefit in terms of quality of life was advised. The lockdown also potentially affected follow-up outcomes. Therefore, our study compared patient-reported outcome measures (PROMs) retrieved during the lockdown of Dutch primary total hip and knee arthroplasty (THA, TKA) patients with previous years.
Patients and methods — We performed cross-sectional analyses using national data from the Dutch Orthopaedic Registry (LROI). All primary elective THA and TKA patients with preoperative or postoperative PROMs (EQ-5D-3L index, OHS/OKS) during the first COVID-19 lockdown between March and July 15, 2020 were included. Patients with PROMs during the same months in 2018 plus 2019 were used as control. Finally, 33,453 THA and 27,335 TKA patients were included. Patient characteristics were compared during versus before the lockdown. Subsequently, the lockdown effect on PROMs scores was analyzed with multivariable linear regression.
Results — During the COVID-19 lockdown, THA and TKA patients had a lower age and BMI preoperatively, and more often had surgery in private clinics. Both preoperative PROMs in THA patients, but not in TKA patients, were worse (EQ-5D: Adjusted mean difference (AMD) –0.021, p < 0.001) during the lockdown compared with prior years. Both postoperative PROMs in THA and TKA patients were better during the lockdown (12-month EQ-5D in THA: AMD 0.010, p = 0.003; and in TKA: AMD 0.013, p < 0.001).
Interpretation — During the COVID-19 lockdown, THA patients had slightly worse preoperative PROMs, suggesting selection of patients with greater urgency. Postoperative PROMs in both THA and TKA patients differed minimally. Overall, the observed differences were likely not clinically relevant.
Citation: Acta Orthopaedica 2022; 93: 808–818. DOI http://dx.doi.org/10.2340/17453674.2022.4856.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-04-04. Accepted: 2022-09-28. Published: 2022-10-14.
Correspondence: j.bonsel@erasmusmc.nl
All authors fulfill the ICMJE authorship criteria. JB: data curation, formal analysis, visualization, writing—original draft, writing—review and editing, funding acquisition, project administration. LG: formal analysis, writing— original draft, writing—review and editing. AC: conceptualization, writing—review and editing. JV: writing—original draft, writing—review and editing, funding acquisition. MG: validation, writing—original draft, writing—review and editing. AS: data curation, writing—original draft. GB/MR: conceptualization, validation, writing—original draft, writing— review and editing, funding acquisition, supervision.
The authors would like to thank Dr S Baart for her help designing the analytical strategy.
Acta thanks Eric Richard Bohm and Keijo T Mäkelä for help with peer review of this study.
In response to the SARS-CoV-2 (COVID-19) pandemic, extreme measures have been taken to contain the virus, most notable being national lockdowns and quarantine policies (1). Several studies noted an increase in psychological distress symptoms of, e.g., feelings of anxiety, and a decrease in quality of life in the general population following the pandemic and the measures taken (2-4). This effect increased with lower age, female sex, poor health status, and low socioeconomic status (SES) (5,6). In most countries there were regional variations in infection rates, which were also observed in the Netherlands (7). People inhabiting places with higher infection rates might also experience increased effects on mental and physical health (8).
In the Netherlands the first lockdown was instigated on March 16, 2020, which was relaxed on June 1, 2020. During the lockdown, large events were prohibited, and people were advised to stay at and work from home if possible. Also, nonessential shops and places including outpatient healthcare facilities such as physical therapists’ premises were closed.
Large shifts in healthcare resources were needed and most elective orthopedic care was reduced to a minimum (9). The Dutch Orthopaedic Society issued a statement on May 1, 2020, to restrict elective arthroplasty to patients who have the largest need and expected benefit in terms of quality of life (10). Also, to minimize COVID-19 infection risks, healthier patients eligible for day treatment were preferred (11).
The lockdown in combination with the pandemic also likely resulted in a lower grade of physical activity and postoperative rehabilitation, negatively influencing the postoperative patient-reported outcome measures (PROMs) of these patients (12,13). Reporting this impact has important implications regarding the assessment of effectiveness of interventions during a pandemic and the resulting lockdown.
This study compared PROMs retrieved during the COVID-19 lockdown of primary THA and TKA patients registered in the Dutch Orthopaedic Registry (Dutch abbreviation: LROI) with previous years. We had the following hypotheses. First, preoperative PROMs are lower due to a selection effect based on urgency assessment. Second, early postoperative PROMs in particular are lower due to the impaired rehabilitative process. Third, at all follow-up points the lockdown negatively affect PROMs, e.g., through feelings of anxiety. Specific subgroups that were possibly more affected by the COVID-19 lockdown were also analyzed.
Patients and methods
Dutch Orthopaedic Registry (LROI)
We used data from the LROI, which prospectively collects data on orthopedic interventions in the Netherlands. The LROI contains demographic and surgical information, and for arthroplasties additionally prosthesis characteristics. Data completeness is over 95% for primary THA and TKA patients (14). Since 2014 the Dutch Orthopaedic Society has strongly recommended the collection of internationally validated general health and disease-specific PROMs in elective arthroplasty. PROMs are retrieved before surgery (at max. 182 days before surgery), at 3-month follow-up (63–110 days) in THA and at 6-month follow-up (154–210 days) in TKA, and at 12-month follow-up (323–407 days) in both. Preoperative PROMs are mostly completed at the outpatient clinic, whilst postoperative PROMs are completed either electronically after invitation via email, or with pen and paper. In 2018 and 2019, 63–66% of THA patients for osteoarthritis completed preoperative PROMs, whilst 34–42% completed both preoperative and postoperative PROMs. In TKA these rates were 55–61% and 30–40% respectively. During COVID-19 in 2020 response rates were in the same ranges (9).
Study design
We performed a retrospective cross-sectional study, and adhered to the STROBE guidelines. Primary THA and TKA patients for any elective indication were selected. Patients who filled out either pre- or postoperative PROMs between March 23 and July 15, 2020 were included. This window allowed for any potential impact of the lockdown to reach its full extent. THA and TKA patients were analyzed separately. This resulted in 6 COVID-19 lockdown groups (THA: preoperative, 3-, and 12-month follow-up; TKA: preoperative, 6-, and 12-month follow-up). Using the same inclusion window patients from 2018 plus 2019 were selected as control groups. COVID-19 groups were compared with the respective control groups, resulting in 6 cross-sectional comparisons.
Data
The following patient characteristics were obtained: age, sex, BMI, Charnley score, ASA score, previous surgery on the joint, indication for joint replacement (osteoarthritis or non-osteoarthritis such as post-traumatic), and type of hospital (general, academic, or private). Additionally, data on COVID-19 infection rate and SES was linked to registry data using patients’ 4-digit postal codes. The Dutch Institute for Health and Milieu published COVID-19 infection rates in the Netherlands bi-weekly (15). The Netherlands is divided into 12 “provinces.” Each province was given an infection rate score of 1 through 5 calculated at 2-week intervals (1: ≤ 24, 2: 25–49, 3: 50–74, 4: 75–99, 5: ≥ 100 infections per 100,000 inhabitants). This score was assigned to records based on the date the PROMs were filled in. Data on SES was obtained from the Dutch Institute of Social Research (16). For each 4-digit postal code area with more than 100 inhabitants, a numeric SES score was created. The SES score is calculated with multiple variables from a postal code area: mean income per household, % households with a low income, % unemployed inhabitants, and % households with an average low education. This method to approximate the individual SES score is considered a validated technique (17). The SES score was categorized into 5 groups based on the quantiles. These groups were referred to as quintiles.
Patient-reported outcome measures
The EuroQol 5-Dimensions (EQ-5D-3L) questionnaire, visual analogue scale (EQ-VAS), and 2 disease-specific questionnaires were obtained (18). For THA the latter were the Oxford Hip Score (OHS) and the short version of the Hip disability and Osteoarthritis Outcome Score (HOOS-PS), and for TKA these were the Oxford Knee Score (OKS) and the short version of the Knee disability and Osteoarthritis Outcome Score (KOOS-PS) (20-22). We selected the EQ-5D-3L and the Oxford set as our main outcome measures. For the EQ-5D-3L an overall index score was calculated using the Dutch National Value set (19).
Statistics
Patient characteristics of the COVID-19 groups were compared with the respective control groups using the chi-square and Student’s t-test. The representativeness of responders was assessed by also comparing patient characteristics of each COVID-19 group with non-responders operated on during the same period based on the inclusion window. The pattern of representativeness was compared with previous years (2018 plus 2019). Duplicate cases, i.e., patients who had their contralateral joint replaced as well, made up a small number of patients (THA: 5%, TKA: 6%) in the entire cohort. Given the present study design, they were not expected to affect results, therefore they were not removed.
Subsequently, PROMs retrieved during the COVID-19 lockdown were compared with control groups using multivariable linear regression analysis. Potential confounders were included based on the theoretical association with the exposure (COVID-19 lockdown) and the known association with outcomes (PROMs) (23). The analyses were adjusted for sex, BMI, ASA score, Charnley score, previous surgery on the joint, indication for joint replacement, type of hospital, and SES (24-27). If a PROM was statistically significantly associated with the COVID-19 group, interaction terms between this group and specific high-risk subgroups were used to explore whether the COVID-19 lockdown had a different effect in these subgroups. The subgroups that we explored were BMI > 30, ASA ≥ 3, age > 70, non-osteoarthritis indication for joint replacement, female sex, and SES quintile ≤ 2. Similarly, we investigated the effect of inhabiting a region with ≥ 50 COVID-19 infections per 100,000 inhabitants. Each interaction term was added individually to the regression analysis, which was then assessed for fit and significance. If interaction terms were not relevant, i.e., resulted in a lower R2 (worsened model fit) and/or did not reach statistical significance, they were removed from the analyses. Robust 95% confidence intervals (CIs) were calculated to account for heteroscedasticity of the PROMs outcomes. The differences are presented as adjusted mean differences (AMDs) with robust CIs and p-values. Clinical relevance was determined by comparing AMDs of the main analyses with currently accepted minimal clinically important differences (MCIDs). These have been reported to be 0.03 for the EQ-5D-3L index in musculoskeletal patients, 5.2 for the OKS, and 4.8 for the OKS in arthroplasty patients (28,29). Potential clinical relevance was confirmed if the CIs’ bounds exceeded the defined MCIDs. A p-value < 0.05 was considered significant. All analyses were performed using SPSS (version 25; IBM Corp, Armonk, NY, USA).
Ethics, funding, and potential conflicts of interest
This study was based on registry data with an extensive protocol for legally conforming data access, therefore no ethical approval additional to LROI permission was required. One of the authors (JB) has received funding from EuroQol for a PhD project including this study. The views expressed by the authors in this manuscript do not necessarily reflect the views of the EuroQol group.
Results
Included patients
There were 33,453 elective THA and 27,335 elective TKA patients eligible for inclusion (Figure 1). The number of patients at 6-month follow-up (TKA) and 12-month follow-up during the COVID-19 lockdown was similar to prior years. There were 35–50% fewer preoperative and 3-month followup (THA) patients.
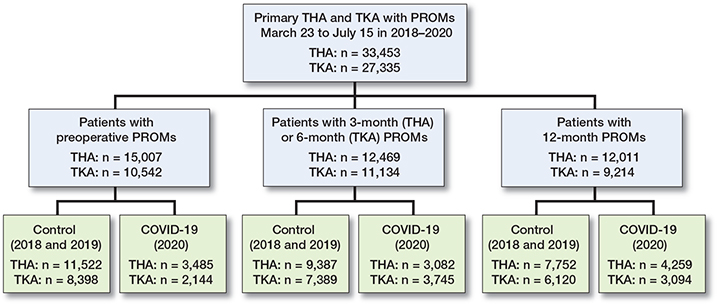
Figure 1. Flowchart of included primary THA and TKA patients with completed PROMs during defined inclusion windows. In a small number of patients with PROMs at multiple measurement points the postoperative follow-up PROM falls in an inclusion window in the subsequent year.
Hence, the number of patients in the defined groups exceed the total number of patients.
Patient characteristics and representativeness
Characteristics of patients during the lockdown were compared with the control groups for THA and TKA separately (Tables 1–2, see Supplementary data). Most notable differences occurred before surgery: during the lockdown both THA and TKA patients had a lower age and BMI, and more often had surgery in private clinics. THA patients slightly more often had a non-osteoarthritis indication, and TKA patients slightly more often were male and had a Charnley score of A/B1/B2 during the lockdown. At 6- and 12-month follow-up in TKA, and at 12-month follow-up in THA, patients more often had an ASA score of III–IV. Other characteristics of patients with postoperative PROMs were comparable during the lockdown.
Characteristics of responders were also compared with non-responders for THA and TKA separately at each follow-up point (Tables 3–6, see Supplementary data). The comparison of patterns confirmed that elective care was reduced during the lockdown and also confirmed the above-mentioned differences in patient characteristics. Responders at all followup points were slightly younger, more often were male, more often had joint replacement for the indication osteoarthritis, and had better orthopedic (i.e., Charnley score) and general vitality (i.e., ASA score) scores. During the lockdown similar patterns emerged, except for type of hospital. In control years, preoperative responders had surgery in general hospitals more often, whilst during the lockdown they were more likely to have had surgery in private clinics.
PROMs
The estimated mean EQ-5D index for each comparison between PROMs retrieved during the COVID-19 lockdown and control groups is presented in Figure 2. In THA patients, the adjusted EQ-5D index and OHS were slightly worse during the COVID-19 lockdown (Table 7, see Supplementary data). In TKA patients, both PROMs were unchanged during the lockdown. For adjusted mean differences in EQ-VAS and HOOS-PS/KOOS-PS see Table 8 in Supplementary data.
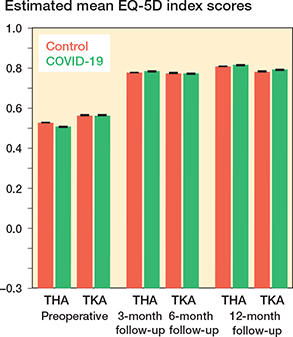
Figure 2. Estimated mean EQ-5D index scores for COVID-19 and control groups, for primary THA and primary TKA separately. A higher EQ-5D index score represents better health status. The error bars represent the 95% confidence intervals of the predicted mean; the upper and lower limit are very close to each other due to the large number of patients for each bar
In THA patients, at 3-month and 12-month follow-up the EQ-5D index and OHS were slightly better during the lockdown. In TKA patients, the EQ-5D index and OKS did not differ at 6-month follow-up, whilst at 12-month follow-up they were slightly better. All identified differences and CI bounds did not exceed predefined MCIDs.
Subgroup analyses
Several interaction terms reached significance; however, they were not consistent across PROMs or follow-up points. Only in THA patients at 12-month follow-up did the term for inhabiting a region with ≥ 50 infections per 100,000 inhabitants reach statistical significance in both PROMs. Higher EQ-5D index and OHS scores (EQ-5D AMD 0.014, CI 0.007 to 0.022; OHS AMD 0.93, CI 0.60 to 1.27) were counteracted (EQ-5D interaction term –0.012, CI –0.022 to –0.001; OHS interaction term –0.58, CI –1.03 to –0.13).
Discussion
Our study demonstrated only small differences in preoperative and postoperative PROMs retrieved during the COVID-19 lockdown compared with previous years in Dutch THA and TKA patients. In THA patients most preoperative PROMs were slightly worse during the lockdown, which was not the case in TKA patients. This suggests a selection effect based on urgency assessment reflected in preoperative PROMs in THA. In both THA and TKA patients, most postoperative PROMs were slightly better during the lockdown. Contrary to our hypotheses, this suggests that the rehabilitation process remained mostly unaffected, and that an overall negative lockdown effect was not observed. Identified differences and CI bounds of all PROMs used in this study did not exceed predefined MCIDs, and are likely not clinically relevant.
This study had several strengths. 2 additional area-based variables were linked to the LROI data set, namely SES and COVID-19 infection rate. Also, multiple PROMs were used at 3 measurement moments, and an extensive set of potential confounders was included. Finally, given the study design (national registry study) the results can be considered generalizable for Dutch orthopedics.
This study had the following limitations. First, in this crosssectional study we did not explore the effect of the lockdown on the longitudinal change scores (i.e., difference between pre- and postoperative PROMs). These analyses would provide information on a different hypothesis, i.e., whether a lockdown effect before surgery could persist into recovery. Furthermore, due to privacy laws the area-based variables were not allowed to contain patient-identifiable information. Therefore, we could not study whether regional differences in PROMs response percentage and representativeness occurred. Additionally, the response rate of PROMs is relatively low in the LROI. However, response rates remained unchanged during the lockdown. Lastly, although the lockdown in the Netherlands shared many similarities with other countries during the first COVID-19 wave, certain differences may still influence the generalizability of results to other countries.
Our study confirms the reduction in elective joint replacements during lockdown, and that a shift of orthopedic care from general hospitals to private clinics occurred during the first COVID-19 lockdown. Furthermore, younger patients with a lower BMI were selected for arthroplasty during the lockdown. Early on in the pandemic focus had shifted towards how to prioritize treatment with reduced capacity for elective surgery (30-32). As the formal announcement of the Dutch Orthopaedic Society was made public halfway through the first lockdown, it could reflect a shift in the collective clinical opinion of Dutch orthopedic surgeons. They may have been aware of risk factors for worse COVID-19 infections such as high age and BMI, and (sub-)consciously selected candidates with a lower risk. A limitation of registry data is that we are unable to discern to what extent self-selection played a role, e.g., patients delaying the procedure themselves because of fear of becoming infected in the hospital.
Besides selection based on characteristics, we additionally found evidence of selection based on urgency. Even after adjustment, THA patients had worse preoperative EQ-5D index and disease-specific PROMs during the COVID-19 lockdown compared with previous years. In TKA patients similar PROMs scores during COVID-19 were observed compared with control years; we do not have a definite explanation for this contrast with THA patients.
We noted no difference or, rather, a slight improvement in most PROMs scores in both THA and TKA patients compared with previous years, an unexpected finding. This was already apparent in the short term (3- and 6-month for THA and TKA respectively), which indicates that rehabilitation success was unaffected. All arthroplasty patients in the Netherlands receive an unsupervised exercise schedule after surgery, and generally receive postoperative outpatient exercise therapy subsequently. It is possible that unsupervised therapy was sufficient, a notion supported by contemporary systematic reviews (12,13). However, this finding should be interpreted with caution. Although during the lockdown physical therapists had to close their physical practice, in approximately 25% of patients they continued via telemedicine, which is not recorded in the LROI (33). Moreover, many patients included in the short-term cross-sectional comparison will have had surgery sometime before the lockdown, and thus might have already initiated physical therapy.
A global scientific body reported severe psychological stress during the COVID-19 pandemic. This is also reflected in studies using the EQ-5D, where lower scores are found in different populations from different nationalities including Dutch, mainly driven by poorer scores for pain/discomfort and anxiety/depression (3,4). The slightly higher postoperative PROMs indicate there was no direct negative effect of the lockdown in this Dutch orthopedic population. In THA patients, inhabiting a region with a COVID-19 high infection rate appeared to negate the improvement in EQ-5D and OHS during the lockdown. However, this effect was minimal and resulted in approximately equal scores compared with prior to the lockdown, which we do not believe provides sufficient evidence of an effect of this interaction term. These findings are in line with a recent study on the impact of COVID-19 on PROMs in hand–wrist patients, which had a similar cross-sectional study design (34). Combined, these results attest to the fact that the general and the orthopedic population do not necessarily experience the same impact of the COVID-19 lockdown.
A potential explanation for the discrepancy in EQ-5D index between the Dutch arthroplasty patient group and the general population is “response-scale heterogeneity,” which refers to the difference in the way individuals interpret a response scale, i.e., a PROM. For instance, if a difference in health occurs between two groups, this may reflect a true difference in health or that the groups perceive the response scale differently due to psychological mechanisms (35). In this population, this may have been caused by feeling privileged during the lockdown: patients considered themselves lucky to have already had their hip or knee replacement before the pandemic hit.
In conclusion, we demonstrated that PROMs scores in Dutch primary THA and TKA patients during the COVID-19 lockdown were hardly affected. Orthopedic surgeons were forced to delay elective surgery due to COVID-19 and also to identify the best candidates for surgery. The observed lower preoperative PROMs scores of THA patients during the COVID-19 lockdown could indicate a (sub-)conscious selection effect based on urgency. Postoperative PROMs in both THA and TKA patients differed minimally. Overall, differences found were likely not clinically relevant.
Reference
- Lai C C, Shih T P, Ko W C, Tang H J, Hsueh P R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents 2020; 55(3): 105924.
- Brooks S K, Webster R K, Smith L E, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 2020; 395(10227): 912-20.
- van Ballegooijen H, Goossens L, Bruin R H, Michels R, Krol M. Concerns, quality of life, access to care and productivity of the general population during the first 8 weeks of the coronavirus lockdown in Belgium and the Netherlands. BMC Health Serv Res 2021; 21(1): 227.
- Hay J W, Gong C L, Jiao X, Zawadzki N K, Zawadzki R S, Pickard A S, et al. A US population health survey on the impact of COVID-19 using the EQ-5D-5L. J Gen Intern Med 2021; 36(5): 1292-301.
- Horesh D, Kapel Lev-Ari R, Hasson-Ohayon I. Risk factors for psychological distress during the COVID-19 pandemic in Israel: loneliness, age, gender, and health status play an important role. Br J Health Psychol 2020; 25(4): 925-33.
- Ping W, Zheng J, Niu X, Guo C, Zhang J, Yang H, et al. Evaluation of health-related quality of life using EQ-5D in China during the COVID-19 pandemic. PLoS One 2020; 15(6): e0234850-e.
- Hoekman L M, Smits M M V, Koolman X. The Dutch COVID-19 approach: regional differences in a small country. Health Policy Technol 2020; 9(4): 613-22.
- Santomauro D F, Mantilla Herrera A M, Shadid J, Zheng P, Ashbaugh C, Pigott D M, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021; 398(10312): 1700-12.
- Dutch Orthopaedic National Quality Registry (LROI). Annual report 2021. Available at: www.lroi-rapportage.nl.
- Nederlands Orthopaedische Vereniging (NOV). Statement on how to reinitiate orthopedic care during the COVID-19 lockdown 1st of May, 2020. Available at: https://bit.ly/2yjf0UN.
- Dutch Cooperating Quality Registries (SKR). Impact Report 2021. Available at: https://skr-zorg.nl/impact-report/.
- Hansen S, Aaboe J, Mechlenburg I, Overgaard S, Mikkelsen L R. Effects of supervised exercise compared to non-supervised exercise early after total hip replacement on patient-reported function, pain, health-related quality of life and performance-based function: a systematic review and meta-analysis of randomized controlled trials. Clin Rehabil 2019; 33(1): 13-23.
- Wang D, Wu T, Li Y, Jia L, Ren J, Yang L. A systematic review and meta-analysis of the effect of preoperative exercise intervention on rehabilitation after total knee arthroplasty. Ann Palliat Med 2021; 10(10): 10986-96.
- van Steenbergen L N, Denissen G A W, Spooren A, van Rooden S M, van Oosterhout F J, Morrenhof J W, et al. More than 95% completeness of reported procedures in the population-based Dutch Arthroplasty Register. Acta Orthop 2015; 86(4): 498-505.
- National Institute for Public Health and the Environment (RIVM). COVID-19 actual report. Accessed October 23, 2020. Available at: https://www.rivm.nl/coronavirus-covid-19/actueel.
- Dutch Institute of Social Research (SCP). Socioenomic status score per postal code area. Retrieved October 20, 2020. Available by request at: https://bronnen.zorggegevens.nl/Bron?naam=Sociaal-Economische-Status-per-postcodegebied.
- Subramanian S V, Chen J T, Rehkopf D H, Waterman P D, Krieger N. Comparing individual- and area-based socioeconomic measures for the surveillance of health disparities: a multilevel analysis of Massachusetts births, 1989–1991. Am J Epidemiol 2006; 164(9): 823-34.
- Brooks R. EuroQol: the current state of play. Health Policy 1996; 37(1): 53-72.
- Lamers L M, McDonnell J, Stalmeier P F, Krabbe P F, Busschbach J J. The Dutch tariff: results and arguments for an effective design for national EQ-5D valuation studies. Health Econ 2006; 15(10): 1121-32.
- Murray D W, Fitzpatrick R, Rogers K, Pandit H, Beard D J, Carr A J, et al. The use of the Oxford hip and knee scores. J Bone Joint Surg Br 2007; 89(8): 1010-14.
- Nilsdotter A K, Lohmander L S, Klässbo M, Roos E M. Hip disability and osteoarthritis outcome score (HOOS): validity and responsiveness in total hip replacement. BMC Musculoskelet Disord 2003; 4: 10.
- Roos E M, Roos H P, Lohmander L S, Ekdahl C, Beynnon B D. Knee Injury and Osteoarthritis Outcome Score (KOOS): development of a selfadministered outcome measure. J Orthop Sports Phys Ther 1998; 28(2): 88-96.
- Shrier I, Platt R W. Reducing bias through directed acyclic graphs. BMC Med Res Methodol 2008; 8: 70.
- Garriga C, Leal J, Sánchez-Santos M T, Arden N, Price A, Prieto-Alhambra D, et al. Geographical variation in outcomes of primary hip and knee replacement. JAMA Netw 2019; 2(10): e1914325-e.
- Peters R M, van Steenbergen L N, Stewart R E, Stevens M, Rijk P C, Bulstra S K, et al. Which patients improve most after total hip arthroplasty? Influence of patient characteristics on patient-reported outcome measures of 22,357 total hip arthroplasties in the Dutch Arthroplasty Register. Hip Int 2020; 31(5): 593-602.
- Tolk J J, Waarsing J H, Janssen R P A, van Steenbergen L N, Bierma-Zeinstra S M A, Reijman M. Development of preoperative prediction models for pain and functional outcome after total knee arthroplasty using the Dutch Arthroplasty Register data. J Arthroplasty 2020; 35(3): 690-8.e2.
- Neuburger J, Hutchings A, Black N, van der Meulen J H. Socioeconomic differences in patient-reported outcomes after a hip or knee replacement in the English National Health Service. J Public Health (Oxf) 2013; 35(1): 115-24.
- Beard D J, Harris K, Dawson J, Doll H, Murray D W, Carr A J, et al. Meaningful changes for the Oxford hip and knee scores after joint replacement surgery. J Clin Epidemiol 2015; 68(1): 73-9.
- Coretti S, Ruggeri M, McNamee P. The minimum clinically important difference for EQ-5D index: a critical review. Expert Rev Pharmacoecon Outcomes Res 2014; 14(2): 221-33.
- Logishetty K, Edwards T C, Subbiah Ponniah H, Ahmed M, Liddle A D, Cobb J, et al. How to prioritize patients and redesign care to safely resume planned surgery during the COVID-19 pandemic. Bone Jt Open 2021; 2(2): 134-40.
- Vles G F, Ghijselings S, De Ryck I, Meyfroidt G, Sweeney N A, Oosterlinck W, et al. Returning to elective orthopedic surgery during the COVID-19 pandemic: a multidisciplinary and pragmatic strategy for initial patient selection. J Patient Saf 2020; 16(4).
- Zorzi C, Piovan G, Screpis D, Natali S, Marocco S, Iacono V. Elective orthopaedic surgery during COVID-19: a safe way to get back on track. JB JS Open Access 2020; 5(4).
- Nivel. Use of paramedic care during COVID-19, consequences for first line exercise therapy. Report week 2–22, 2020. Available at: https://www.nivel.nl/nl/publicatie/gevolgen-corona-voor-de-eerstelijns-oefen-enfysiotherapiepraktijk-gebruik-van#:~:text=Na%20vier%20weken%20lag%20het,%2Duitbraak%20(begin%202020).
- Cohen A, Selles R W, De Ridder W A, Ter Stege M H P, Souer J S, Wouters R M, et al. What is the impact of the COVID-19 pandemic on quality of life and other patient-reported outcomes? An analysis of the Hand–Wrist Study cohort. Clin Orthop Relat Res 2021; 479(2): 335-45.
- Knott R J, Black N, Hollingsworth B, Lorgelly P K. Response-scale heterogeneity in the EQ-5D. Health Econ 2017; 26(3): 387-94.
Supplementary data
| Factor | Preoperative AMD (CI) | p-value | 3-/6-month postoperative AMD (CI) | p-value | 12-month postoperative AMD (CI) | p-value |
| Total hip arthroplasty | n = 15,007 | n = 12,469 | n = 12,011 | |||
| Without interaction terms | ||||||
| EQ-5D index a | –0.021 (–0.029 to –0.013) | < 0.001 | 0.008 (0.001 to 0.015) | 0.03 | 0.010 (0.003 to 0.016) | 0.003 |
| With interaction terms | no relevant interaction terms | |||||
| BMI > 30 | –0.019 (–0.035 to –0.002) | 0.02 | ||||
| EQ-5D index a | 0.012 (0.005 to 0.020) | 0.002 | ||||
| Infections ≥ 50 per 10 5 | –0.012 (–0.022 to –0.001) | 0.03 | ||||
| EQ-5D index a | 0.014 (0.007 to 0.022) | < 0.001 | ||||
| Without interaction terms | ||||||
| OHS a | –0.95 (–1.30 to –0.60) | < 0.001 | 0.44 (0.13 to 0.74) | 0.005 | 0.71 (0.42 to 1.00) | < 0.001 |
| With interaction terms | no relevant interaction terms | no relevant interaction terms | ||||
| Infections ≥ 50 per 105 | –0.58 (–1.03 to –0.13) | 0.01 | ||||
| OHS a | 0.93 (0.60 to 1.27) | < 0.001 | ||||
| Total knee arthroplasty | n = 10,542 | n = 11,134 | n = 9,214 | |||
| Without interaction terms | ||||||
| EQ-5D index a | –0.003 (–0.012 to 0.007) | 0.6 | 0.000 (–0.007 to 0.007) | 1 | 0.013 (0.006 to 0.021) | < 0.001 |
| With interaction terms | – b | – b | no relevant interaction terms | |||
| Without interaction terms | ||||||
| OKS a | –0.03 (–0.36 to 0.41) | 0.9 | 0.12 (–0.22 to 0.47) | 0.5 | 0.45 (0.07 to 0.83) | 0.02 |
| With interaction terms | – b | – b | no relevant interaction terms | |||
| a A higher EQ-5D index, OHS/OKS represents an improvement. b Interaction terms were not analyzed in non-significant associations. |
||||||
| Factor | Preoperative AMD (CI) | p-value | 3-/6-month postoperative AMD (CI) | p-value | 12-month postoperative AMD (CI) | p-value | |
| Total hip arthroplasty | n = 15,007 | n = 12,469 | n = 12,011 | ||||
| Without interaction terms | |||||||
| EQ-VAS a | 0.11 (–0.71 to 0.93) | 0.8 | 2.16 (1.40 to 2.92) | < 0.001 | 3.11 (2.38 to 3.85) | < 0.001 | |
| With interaction terms | – c | no relevant interaction terms | no relevant interaction terms | ||||
| Without interaction terms | |||||||
| HOOS-PS b | 2.15 (1.43 to 2.87) | < 0.001 | –0.38 (–1.00 to 0.24) | 0.2 | –0.77 (–1.35 to –0.20) | 0.009 | |
| With interaction terms | – c | no relevant interaction terms | |||||
| BMI > 30 | –1.88 (–3.60 to –0.16) | 0.03 | |||||
| HOOS-PS b | 2.60 (1.78 to 3.41) | < 0.001 | |||||
| SES 1st–2nd quintile | –1.55 (–3.00 to –0.09) | 0.04 | |||||
| HOOS-PS b | 2.82 (1.88 to 3.76) | < 0.001 | |||||
| Total knee arthroplasty | n = 10,542 | n = 11,134 | n = 9,214 | ||||
| Without interaction terms | |||||||
| EQ-VAS a | 0.76 (–0.20 to 1.73) | 0.1 | 1.82 (1.08 to 2.57) | < 0.001 | 1.92 (1.06 to 2.79) | < 0.001 | |
| With interaction terms | – c | no relevant interaction terms | |||||
| ASA ≥ 3 | 2.74 (0.82 to 4.67) | 0.005 | |||||
| EQ-VAS a | 1.23 (0.42 to 2.05) | 0.003 | |||||
| Age > 70 | 2.47 (0.98 to 3.96) | 0.001 | |||||
| EQ-VAS a | 0.64 (–0.36 to 1.64) | 0.2 | |||||
| Without interaction terms | |||||||
| KOOS-PS b | 0.28 (–0.49 to 1.04) | 0.5 | 0.49 (–0.09 to 1.06) | 0.1 | –0.77 (–1.48 to –0.07) | 0.03 | |
| With interaction terms | – c | – c | no relevant interaction terms | ||||
| a A higher EQ-VAS represents an improvement. b A lower HOOS-PS/KOOS-PS represents an improvement. c Interaction terms were not analyzed in non-significant associations. |
|||||||