Risk of reoperation due to surgical site infection in 74,771 hip fracture patients: a Danish nationwide cohort study
Nicolai K KRISTENSEN 1,3, Jeppe LANGE 1,3, Trine FRØSLEV 2, and Alma B PEDERSEN 2,3
1 Department of Orthopaedic Surgery, Horsens Regional Hospital; 2 Department of Clinical Epidemiology, Aarhus University Hospital, Aarhus; 3 Department of Clinical Medicine, Aarhus University, Aarhus, Denmark
Background and purpose — Surgical site infection (SSI) after hip fracture surgery is a feared condition. We examined the trend in incidence of reoperation due to SSI up to 1 year following hip fracture surgery from 2005 to 2016 and risk factors of SSI by age, sex, comorbidity, type of fracture, and surgery.
Patients and methods — We conducted a population-based, nationwide cohort study using data from the Danish Multidisciplinary Hip Fracture Register (DMHFR). We included 74,771 patients aged 65 and up who underwent surgery from 2005 to 2016 for all types of hip fracture. We calculated net risk of reoperation using Kaplan–Meier method, and, with Cox regression, adjusted hazard ratios (HRs) with a 95% confidence interval (CI) for reoperation due to SSI.
Results — Overall, the 1-year net risk of reoperation due to SSI was 2.7%. The HR was lower for patients undergoing total/hemiarthroplasty surgery versus internal fixation (HR = 0.6; 95% CI 0.5–0.6) and for patients with per-/subtrochanteric fracture versus femoral neck fracture (HR = 0.7; CI 0.6–0.8). The risk of reoperation due to SSI decreased over time; HR was 0.6 (CI 0.5–0.7) for 2015–2016 compared with 2005–2006. Risk of reoperation decreased with increasing age; the HR was 0.6 (CI 0.6–0.7) in the more than 85-year-olds compared with 65–74-year-old patients.
Interpretation — The net risk of reoperations due to SSI in our study was higher than previously assumed. We identified several risk factors for increased risk of reoperation due to SSI, most noticeably treatment with internal fixation vs. arthroplasty, as well as younger age and femoral neck fracture diagnosis.
Citation: Acta Orthopaedica 2022; 93: 760–766. DOI http://dx.doi.org/10.2340/17453674.2022.4580.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-02-20. Accepted: 2022-08-31. Published: 2022-09-21.
Correspondence: nicokris@rm.dk
NKK contributed to the study design, data interpretation and writing of the article, review, and revision of the article. JL contributed to the study design, data interpretation, and writing of the article, review, and revision of the article. TF contributed to the study design, data analysis, and revision of the manuscript, review, and revision of the article. ABP initiated the study, contributed to the study design, data interpretation, and writing of the article, review, and revision of the article.
Acta thanks Jan-Erik Gjertsen and Lars Gunnar Johnsen for help with peer review of this study.
Surgical site infection (SSI) following hip fracture surgery results in pain, prolonged hospital stay, additional surgical procedures, and increased socioeconomic costs (1). Moreover, mortality rates in patients with a reoperation due to SSI have been reported to be 2.9 times higher than in patients with no SSI event (2,3). In Denmark, almost 7,000 patients suffer a hip fracture every year (4).
Studies have indicated an increase in SSI in primary arthroplasties over a 10-year period (5), but to our knowledge data on time-trend in reoperation due to SSI after hip fracture is lacking. A recent review from 2020 (6) found an overall incidence of 2.1% reoperation due to SSI (varying from 1% to 12%). The review included hip fracture patients from 20 studies of which most were retrospective, single-center studies, and only of UK origin, with considerable inter-study differences, including SSI definitions.
We investigated the risk and time-trend in reoperation due to SSI following hip fracture surgery and evaluated specific risk factors of SSI.
Patients and methods
Study design and setting
This was a population-based, nationwide cohort study.
The study was based on routinely collected data from national medical databases, which encompass the entire Danish population, and are well proven in epidemiologic research (7).
The Danish National Health Service provides tax-supported healthcare for the entire population, guaranteeing universal access to all hospitals and primary medical care.
Data sources
The Danish Multidisciplinary Hip Fracture Register (DMHFR) is a nationwide, clinical, quality assessment database on all hip fracture patients aged 65 or older undergoing surgery for proximal femoral fractures (4,8). The database was established in 2003 with the intention to improve the quality of treatment and care of hip fracture patients. Reporting to the DMHFR has been mandatory by law for all hospitals from 2006 (9). During the period from 2006 to 2016, all hospitals nationwide treating hip fracture patients were reporting to the registry.
The Danish Civil Registration system (DCRS) was established in 1968 and contains electronic records on vital status (date of death or emigration) for the entire Danish population; it is updated daily. The DCRS assigns a unique civil registration number to every Danish citizen, which goes through all Danish registers allowing for unambiguous linkage between registers on an individual level.
The Danish National Patient Register (DNPR) was established in 1977, and has registered all non-psychiatric hospital admissions since 1977 and all hospital outpatient and emergency visits since 1995 (10). It includes dates of admission and discharge, main diagnoses, NOMESCO classification of surgical procedures, and up to 20 secondary discharge diagnosis codes according to ICD-8 until the end of 1993 and ICD-10 thereafter.
Study population
From the DMHFR, we identified the study population consisting of patients 65 years of age or older, who underwent surgery between January 1, 2005 and December 31, 2016. Both primary and secondary inpatient diagnosis were included.
After excluding patients who emigrated (n = 18) or were lost to follow-up (n = 1), we included 74,771 patients from DMHFR in the final study population. Cross-linkage with the remaining study data sources was then made.
Demographic data extracted from the medical databases included vital status, civil status, age, sex, BMI, fracture type, and comorbidity burden measured with the Charlson comorbidity index (CCI) (11).
Surgical procedure type was binary, registered as joint replacement or joint preservation osteosynthesis.
Outcome
The outcome was reoperations due to SSI. We have relied on the SSI definition by the Center for Disease Control, which includes both superficial incisional SSI (involving infection of skin and subcutaneous tissue of the incision), deep incisional SSI (involving deep tissues of the incision such as muscle or fascia layers), and deep open SSI (involving tissues that are deeper than the muscle/fascial layers) (12). The diagnosis and surgery codes, adapted to Danish registration codes used to define SSI in our study, are presented in Table 1.
Risk factors
Risk factors for SSI were assessed among the measured baseline characteristics collected at the time of hip fracture surgery. Risk factors examined were age (in categories 65–74, 75–84, and ≥ 85 year at the time of hip fracture), sex, CCI (in categories low [CCI score 0], medium [CCI score 1 or 2], and high [CCI score of ≥ 3]) in addition to fracture type (fracture of the femoral neck vs. per-/subtrochanteric fracture) and surgery type (internal fixation vs. hemi/total arthroplasty).
Statistics
Patient characteristics were described at the time of hip fracture surgery.
We computed net risk of reoperation using Kaplan–Meier (KM) methods to describe the failure of implants overall and by calendar year periods and other risk factors. In addition, using competing risk method considering death as a competing risk we calculated crude risk of reoperation for resource planning purposes and for communicating with patients regarding their chance of experiencing reoperation due to SSI (13).
The risks of reoperation were calculated for the period of 0–1 year postoperatively, but we also included analyses at 0–15 days, 0–30 days, and 0–90 days postoperatively as they are clinically relevant.
Based on the Cox regression method, hazard ratios (HR) with a 95% confidence interval (CI) were calculated. When looking into the association between calendar time and reoperation due to SSI, we included age, sex, and CCI as confounders based on established impact of these factors on the association of interest, and on the directed acyclic graph (DAG) models. We used calendar period 2005–2006 as a reference.
In addition, we estimated HR by age groups, sex, CCI, fracture type, and surgery type. To avoid Table 2 Fallacy, we have analyzed each risk factor separately, thus we repeated the Cox regression 5 times for each risk factor. When calculating HR for sex, we performed 1 Cox regression to calculate HR for male vs. female, adjusting for age, CCI, BMI, and fracture type. In the analysis of age as a risk factor, we adjusted HR for sex and fracture type, whereas in the analysis of comorbidity as a risk factor, we adjusted HR for age, sex, and fracture type. For fracture type as a risk factor, HR was adjusted for age, sex, CCI, and BMI, whereas for surgery type as a risk factor, HR was adjusted for age, sex, CCI, BMI, and fracture type. Separate DAG models were drawn for each risk factor to decide on confounders.
The proportionality assumption was tested through log–log plots and found to be satisfactory.
Analyses were performed using SAS V. 9.4 (SAS Institute Inc., Cary, NC, USA).
Ethics, funding, data sharing, and potential conflicts of interest
The study was approved by the Danish Data Protection Agency (Record number 1-16-02-444-15/ 2012-58-006 in the Central Denmark Region). The study was supported by a grant from Aarhus University Research Foundation. Data was obtained specifically for this project, based on the permissions required by the relevant Danish data authorities, who own the data. The authors are not allowed to share the data with third parties. There are no conflicts of interest in the author group.
Results
Study population (Table 2)
The proportion of patients aged 65–74, as well as those older than 85 years of age, increased during the study period from 2005 to 2016. Likewise, the proportion of patients with comorbidity increased during the study period. There was an increase over time in patients registered with lymphomas, any tumor, diabetes I and II, moderate to severe renal disease, chronic pulmonary disease, dementia, and peripheral vascular disease (Table 3, see Supplementary data) More patients with femoral neck fracture were treated over time, and use of total or hemiarthroplasty increased over time. Most patients with per-/subtrochanteric fracture were treated with internal fixation (98%), whereas patients with femoral neck fracture were treated with internal fixation in 42% of cases, and with total/hemiarthroplasty in 58% of cases.
Reoperation due to SSI: time trend
Within 1 year of primary surgery, 1,688 of 74,771 hip fracture patients had undergone reoperation due to SSI, corresponding to a net risk of reoperation of 2.7%. During the study period, the net risk of reoperation due to SSI decreased from 3.4% in 2005–2006 to 2.1% in 2015–2016, corresponding to an adjusted HR of 0.6 (CI 0.5–0.7) (Table 4) and absolute reduction of 1.3%. A similar decrease in adjusted HRs was observed for follow-up periods 0–15, 0–30, and 0–90 days after hip fracture surgery. Overall, crude risk of reoperation was 2.3%, decreasing from 2.8% to 1.8% over the study period (Table 4).
| Follow-up period Calendar period of diagnosis | No. of patients | No. of % infections | Cumulative incidence, % (95% CI) | Kaplan-Meier risk, (HR) (95% CI) | Crude hazard ratio (HR) (95% CI) | Adjusted a hazard ratio(95% CI) |
| 0–15 days of surgery | ||||||
| 2005–2006 | 12,453 | 37 | 0.30 (0.21–0.41) | 0.32 (0.23–0.43) | Reference | Reference |
| 2007–2008 | 13,236 | 25 | 0.19 (0.13–0.28) | 0.20 (0.13–0.29) | 0.63 (0.38–1.05) | 0.63 (0.38–1.05) |
| 2009–2010 | 12,724 | 19 | 0.15 (0.09–0.23) | 0.16 (0.10–0.25) | 0.50 (0.29–0.87) | 0.50 (0.29–0.87) |
| 2011–2012 | 12,706 | 22 | 0.17 (0.11–0.26) | 0.18 (0.12–0.28) | 0.59 (0.35–0.99) | 0.58 (0.34–0.98) |
| 2013–2014 | 12,285 | 28 | 0.23 (0.16–0.33) | 0.24 (0.16–0.35) | 0.76 (0.47–1.25) | 0.75 (0.46–1.23) |
| 2015–2016 | 11,367 | 19 | 0.17 (0.10–0.26) | 0.18 (0.11–0.27) | 0.56 (0.32–0.97) | 0.55 (0.32–0.96) |
| 2005–2016 | 74,771 | 150 | 0.20 (0.17–0.23) | 0.21 (0.18–0.25) | ||
| 0–30 days of surgery | ||||||
| 2005–2006 | 12,453 | 94 | 0.75 (0.61–0.92) | 0.82 (0.66–0.99) | Reference | Reference |
| 2007–2008 | 13,236 | 87 | 0.66 (0.53–0.81) | 0.71 (0.58–0.88) | 0.87 (0.65–1.16) | 0.87 (0.65–1.16) |
| 2009–2010 | 12,724 | 79 | 0.62 (0.50–0.77) | 0.68 (0.54–0.84) | 0.82 (0.61–1.11) | 0.82 (0.61–1.11) |
| 2011–2012 | 12,706 | 84 | 0.66 (0.53–0.81) | 0.72 (0.58–0.89) | 0.88 (0.66–1.18) | 0.88 (0.65–1.18) |
| 2013–2014 | 12,285 | 100 | 0.81 (0.67–0.99) | 0.88 (0.72–1.07) | 1.08 (0.81–1.43) | 1.07 (0.81–1.42) |
| 2015–2016 | 11,367 | 61 | 0.54 (0.42–0.69) | 0.58 (0.45–0.74) | 0.71 (0.51–0.97) | 0.70 (0.51–0.97) |
| 2005–2016 | 74,771 | 505 | 0.68 (0.62–0.74) | 0.73 (0.67–0.80) | ||
| 0–90 days of surgery | ||||||
| 2005–2006 | 12,453 | 208 | 1.67 (1.46–1.91) | 1.87 (1.63–2.14) | Reference | Reference |
| 2007–2008 | 13,236 | 181 | 1.37 (1.18–1.58) | 1.54 (1.33–1.77) | 0.82 (0.67–1.00) | 0.82 (0.67–1.00) |
| 2009–2010 | 12724 | 176 | 1.38 (1.19–1.60) | 1.56 (1.34–1.80) | 0.83 (0.68–1.02) | 0.83 (0.68–1.01) |
| 2011–2012 | 12706 | 178 | 1.40 (1.21–1.62) | 1.59 (1.37–1.84) | 0.85 (0.69–1.04) | 0.84 (0.69–1.03) |
| 2013–2014 | 12,285 | 174 | 1.42 (1.22–1.64) | 1.58 (1.36–1.82) | 0.85 (0.69–1.04) | 0.84 (0.69–1.03) |
| 2015–2016 | 11,367 | 123 | 1.08 (0.90–1.29) | 1.20 (1.01–1.43) | 0.64 (0.52–0.80) | 0.64 (0.51–0.80) |
| 2005–2016 | 74,771 | 1040 | 1.39 (1.31–1.48) | 1.56 (1.47–1.66) | ||
| 0–365 days of surgery | ||||||
| 2005–2006 | 12,453 | 352 | 2.83 (2.55–3.13) | 3.36 (3.03–3.72) | Reference | Reference |
| 2007–2008 | 13,236 | 305 | 2.30 (2.06–2.57) | 2.76 (2.47–3.08) | 0.82 (0.70–0.95) | 0.82 (0.70–0.96) |
| 2009–2010 | 12,724 | 287 | 2.26 (2.01–2.52) | 2.70 (2.41–3.03) | 0.80 (0.69–0.94) | 0.80 (0.68–0.94) |
| 2011–2012 | 12,706 | 286 | 2.25 (2.00–2.52) | 2.71 (2.41–3.03) | 0.81 (0.69–0.94) | 0.80 (0.68–0.93) |
| 2013–2014 | 12,285 | 262 | 2.13 (1.89–2.40) | 2.51 (2.22–2.82) | 0.76 (0.64–0.89) | 0.75 (0.64–0.87) |
| 2015–2016 | 11,367 | 196 | 1.77 (1.54–2.03) | 2.10 (1.82–2.40) | 0.62 (0.52–0.73) | 0.60 (0.51–0.72) |
| 2005–2016 | 74,771 | 1688 | 2.26 (2.16–2.37) | 2.70 (2.57–2.83) | ||
| a Hazard ratio adjusted for age, sex, and comorbidity by the Charlson comorbidity index; CI = confidence interval; Cumulative incidence = crude risk of reoperation; Kaplan–Meier risk = net risk of reoperation. | ||||||
Risk factors for reoperation due to SSI (Figures 1 and 2)
Sex and CCI were not risk factors for reoperation due to SSI within 1 year of hip fracture surgery. The HRs for reoperation due to SSI within 1 year decreased with increasing age. Thus, the HRs were 0.6 (CI 0.6–0.7) and 0.8 (CI 0.7–0.8) for patients aged above 85 and patients aged 75–84 years compared with the youngest age group (65–74 years), respectively. Similar results were obtained within 90 days of surgery.
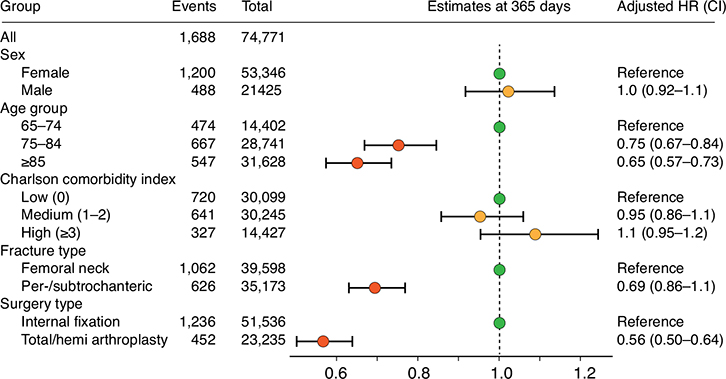
Figure 1. Risk factors for reoperation due to SSI within 1 year of hip fracture surgery.
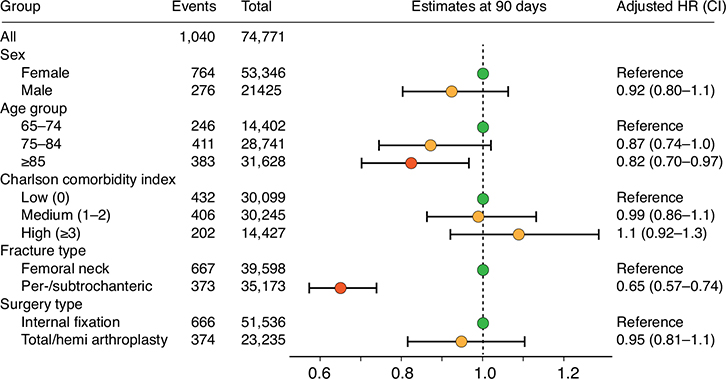
Figure 2. Risk factors for reoperation due to SSI within 90 days of hip fracture surgery.
The HR for reoperation due to SSI within 1 year was 0.7 (CI 0.6–0.8) for patients sustaining the per-/subtrochanteric fracture compared with patients sustaining femoral neck fractures. The HR at 90 days post-surgery was 0.6 (CI 0.6–0.7).
The HR was 0.6 (CI 0.5–0.6) within 1 year for patients undergoing total/hemiarthroplasty compared with patients undergoing internal fixation. However, at 90 days, HR was 0.9 (CI 0.8–1.1) for total/hemiarthroplasty compared with internal fixation.
Discussion
This study shows 1-year net risk of reoperation due to SSI for all types of hip fractures over a 10-year period of 2.7%. There was a 45% decrease in reoperation due to SSI over time with the most recent 1-year net risk of reoperation being 2.1% in 2015–2016. Given the high morbidity and mortality following reoperation due to SSI, further action should be taken to avoid reoperations due to SSI, especially in these high-risk, fragile patients. A Swedish register study showed an SSI rate reduction from 2.5% to 1.1% after implementing the “safe hands” protocol (14), which leads us to believe that focus on infection can improve outcome and reduce the risk of infection.
Comparison with other studies
A systematic review based on 13 papers showed that the SSI rate after hemiarthroplasty for displaced femoral neck fractures varies between 1.7% and 7.3% (15). A multicenter study from France reported a rate of 3.9% of SSI when femoral neck fractures were treated with osteosynthesis compared with 6.9% if the fracture was treated with total/hemiarthroplasty (16). Previous studies were based on small sample sizes contributing to uncertainty regarding the true incidence of reoperation due to SSI.
A recent study from the UK by Masters et al. (6) found an increased number of reoperations due to SSI. The study included SSI with and without operation and was based on 20 studies from 18 UK institutions with vast variations in SSI definition. They found a risk of SSI from 1% to 12% with an average of 2.1%.
Studies showing culture positive findings, or where reoperation is the end point, are at risk of under-reporting as the clinical examinations of SSI are much more difficult to review and do research on, however valid the diagnosis of SSI is. The result is that this study, as well as that by Masters et al., might underreport, no matter the definition of SSI. We believe we contribute to evaluating the “true” SSI rate regarding the exceptional validity of the Danish registers.
Our study finds an almost 50% lower rate of reoperations due to SSI within 1 year when hip fractures are treated with total or hemiarthroplasty compared with osteosynthesis. This somehow contradicts our other finding that per-/subtrochanteric fractures are associated with a lower risk of reoperation due to SSI than femoral neck fractures. However, in Denmark, per-/subtrochanteric fractures are treated with internal fixation, whereas femoral neck fractures are equally treated with osteosynthesis and total/hemiarthroplasty, which might not be the practice in other countries. There are no available comparable studies.
However, there is clearly a lower reoperation risk in elderly patients compared with the younger group. A low virulent infection (e.g., biofilm) could go undetected by the decreased immune response in the elderly (17), explaining the lower risk of reoperation with increasing age. Further, SSI symptoms typically occur within the first 2 years of surgery, and it is likely that older patients die before developing SSI symptoms (18). It is also probable that surgeons are more reluctant to reoperate on elderly patients due to high multimorbidity. This is in line with the latest report from the UK, showing that increased multimorbidity and markers of preoperative poor health are associated with a decreased likelihood to undergo total hip arthroplasty (19). Finally, while some younger hip fracture patients are healthy persons sustaining hip fracture due to high-energy trauma, others who sustain hip fractures due to low-energy trauma, have a biologically advanced age, or have a high prevalence of comorbidities that reduces bone health, making surgery more complicated to perform. A high prevalence of alcohol abuse, smoking, and cognitive impairment, are all negatively associated with surgery outcome (20).
Methodological considerations
The coverage of the DMHFR is 100%, thus, all hospitals that perform surgery for hip fracture report to the register because registration is mandatory. Regarding completeness of hip fracture patient registration, the hospitals are reimbursed for hip fracture treatment only if the diagnosis of hip fracture and surgery code for treatment of hip fracture is reported to the DMHFR. Thus, there is motivation for hospitals to have as complete patient registration as possible since duration of hospitalization and treatment of hip fracture is costly. However, we cannot entirely exclude the possibility that some patients are not caught by the DMHFR. The validity of a hip fracture diagnosis in the DMHFR is high (21), thus the risk of information bias is low.
Regarding registration of reoperation due to SSI, we have previously validated an algorithm for periprosthetic hip joint infection using a combination of diagnosis and surgery codes reported to the Danish National Patient Register with positive predictive value (PPV) of more than 85% (22). In addition, Gundtoft et al. showed a 98% PPV for revision due to deep infection in the Danish Hip Arthroplasty register when crosschecking with the national microbiological database, and completeness of 77% (23). We do not have the same validation study on reoperation due to infection after hip fracture surgery, but we do not have reason to believe that the validity is different since the same departments and surgeons participate in the treatment and registration of patients requiring reoperation surgery.
Strengths and limitations
The large sample size and complete data on 74,771 patients and virtually no loss of follow-up is a study strength. With the use of national databases, there is no loss of patients when a change of hospital or region takes place. As SSI is a rare event at the individual orthopedic centers, register-based studies are the optimal way to thoroughly evaluate SSI occurrence. Misclassification bias is possible, as reoperation due to SSI is dependent on individual assessment and clinical evaluation, but any misclassification is most unlikely related to age, sex, CCI, fracture, and surgery type.
Our results are adjusted for the most important confounders such as age, sex, and CCI score. In addition, in the analyses of risk factors, we used DAG models to establish confounders relevant to specific risk factor-outcome association.
The study includes patients from all hospitals in Denmark, both major trauma centers and traditional district general hospitals. As a result, the findings are very representative of all settings, compared with the review from Masters et al., where most studies included were from 1 single institution and with relatively low patient numbers. The generalizability extends to the patients, as they are all included from 2005 to 2016 irrespective of type of fracture or surgery. It is important to acknowledge that the data are derived from a Danish setting and are likely applicable to the healthcare systems in other high-income Western countries, but the generalizability of data to the non-Western countries or countries where surgery is not the main treatment of hip fracture patients is unclear.
Conclusion
In this large cohort study of 74,771 patients, the net risk of reoperation due to SSI within 1 year for all types of hip fractures treated in the period 2005–2016 was 2.7%. It is noteworthy that the highest risk of revision due to SSI was in the internal fixation group, compared with the arthroplasty-treated patients.
There was a 45% decrease in reoperation due to SSI over time from 2005 to 2016 and we identified several risk factors for increased risk of reoperation due to SSI, including younger age and femoral neck fracture. Given the high mortality following reoperation due to SSI, further focus should be directed towards prevention of SSI in this fragile patient group.
- Burge R, Dawson-Hughes B, Solomon D H, Wong J B, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res 2007; 22(3): 465-75.
- Kjørholt K E, Kristensen N R, Prieto-Alhambra D, Johnsen S P, Pedersen A B. Increased risk of mortality after postoperative infection in hip fracture patients. Bone 2019; 127: 563-70.
- Pollmann C T, Dahl F A, Røtterud J H M, Gjertsen J E, Årøen A. Surgical site infection after hip fracture-mortality and risk factors: an observational cohort study of 1,709 patients. Acta Orthop 2020; 91(3): 347-52.
- Kristensen P K, Röck N D, Christensen H C, Pedersen A B. The danish multidisciplinary hip fracture registry 13-year results from a population-based cohort of hip fracture patients. Clin Epidemiol 2020; 12: 9-21.
- Dale H, Fenstad AM, Hallan G, Havelin LI, Furnes O, Overgaard S, et al. Increasing risk of prosthetic joint infection after total hip arthroplasty. Acta Orthop 2012; 83(5): 449-58.
- Masters J, Metcalfe D, Ha J S, Judge A, Costa M L. Surgical site infection after hip fracture surgery. Bone Joint Res 2020; 9(9): 554-62.
- Schmidt M, Pedersen L, Sørensen H T. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol 2014; 29(8): 541-9.
- Fracture and dislocation classification compendium—2018. Femur. J Orthop Trauma 2018; 32(1): S33-44.
- Danish health ministry. The Danish health act legislation number 546 from 24 June 2005 - Danish legislation number 546. Vol 546.
- Schmidt M, Schmidt S A J, Sandegaard J L, Ehrenstein V, Pedersen L, Sørensen H T. The Danish National patient registry: A review of content, data quality, and research potential. Clin Epidemiol 2015; 7:449-90.
- Frenkel W J, Jongerius E J, Mandjes-Van Uitert M J, Van Munster B C, De Rooij S E. Validation of the Charlson Comorbidity Index in acutely hospitalized elderly adults: A prospective cohort study. J Am Geriatr Soc 2014; 62(2): 342-6.
- National Healthcare Safety Network. Surgical Site Infection Event (SSI). Centres Dis Control Prev 2021; (January): 1-39.
- Sayers A, Evans J T, Whitehouse M R, Blom A W. Are competing risks models appropriate to describe implant failure? Acta Orthop 2018; 89(3): 256-8.
- Andersson A, Gillespie B, Karlsson M, Malchau H, Nellgård B, Wikström E, et al. Fewer early surgical site infections after hip fracture and lessons learned from the Safe Hands Project: A five-year longitudinal study of 3,553 patients. Antimicrob Resist Infect Control 2022; 11(1): 113.
- Noailles T, Brulefert K, Chalopin A, Longis P M, Gouin F. What are the risk factors for post-operative infection after hip hemiarthroplasty? Systematic review of literature. Int Orthop 2016; 40(9): 1843-8.
- Merrer J, Girou E, Lortat-Jacob A, Montravers P, Lucet J-C. Surgical site infection after surgery to repair femoral neck fracture: a French multicenter retrospective study. Infect Control Hosp Epidemiol 2007; 28(10): 1169-74.
- Montecino-Rodriguez E, Berent-Maoz B, Dorshkind K. Causes, consequences, and reversal of immune system aging. J Clin Invest 2013; 123(3): 958-65.
- Hjelholt T J, Johnsen S P, Brynningsen P K, Knudsen J S, Prieto-Alhambra D, Pedersen A B. Development and validation of a model for predicting mortality in patients with hip fracture. Age Ageing 2022; 51(1): afab233. doi: 10.1093/ageing/afab233.
- Ferguson R, Prieto-Alhambra D, Peat G, Delmestri A, Jordan KP, Strauss V Y, et al. Influence of pre-existing multimorbidity on receiving a hip arthroplasty: Cohort study of 28 025 elderly subjects from UK primary care. BMJ Open 2021; 11(9): 1-7.
- Rogmark C, Kristensen M T, Viberg B, Rönnquist S S, Overgaard S, Palm H. Hip fractures in the non-elderly—Who, why and whither? Injury [Internet]. 2018; 49(8): 1445-50. Available from: https://doi.org/10.1016/j.injury.2018.06.028
- Hjelholt T J, Edwards N M, Vesterager J D, Kristensen P K, Pedersen A B. The positive predictive value of hip fracture diagnoses and surgical procedure codes in the danish multidisciplinary hip fracture registry and the Danish national patient registry. Clin Epidemiol 2020; 12: 123-31.
- Lange J, Pedersen AB, Troelsen A, Søballe K. Do hip prosthesis related infection codes in administrative discharge registers correctly classify periprosthetic hip joint infection? HIP Int 2015; 25(6): 568-73
- Gundtoft P H, Overgaard S, Schønheyder H C, Møller J K, Kjærsgaard-Andersen P, Pedersen A B. The “true” incidence of surgically treated deep prosthetic joint infection after 32,896 primary total hip arthroplasties. Acta Orthop 2015; 86(3): 326-34. doi:10.3109/17453674.2015.1011983