Epidemiology and trends in management of acute proximal humeral fractures in adults: an observational study of 137,436 cases from the Danish National Patient Register, 1996–2018
Stig BRORSON 1, Bjarke VIBERG 2, Per GUNDTOFT 3, Bamo JALAL 4, and Søren OHRT-NISSEN 5
1 Centre for Evidence-Based Orthopaedics, Zealand University Hospital and Department of Clinical Medicine, University of Copenhagen; 2 Department of Orthopaedic Surgery and Traumatology, Hospital Lillebaelt, University Hospital of Southern Denmark and Department of Orthopaedic Surgery and Traumatology, Odense University Hospital; 3 Department of Orthopaedic Surgery, Aarhus University Hospital and Department of Orthopaedic Surgery, Kolding Hospital; 4 Department of Orthopaedic Surgery, Zealand University Hospital; 5 Spine Unit, Department of Orthopaedic Surgery, Rigshospitalet, University of Copenhagen, Denmark
Background and purpose — Proximal humeral fractures (PHF) can be managed surgically or non-surgically. Locking plates have been the preferred head-preserving surgical technique while hemiarthroplasty (HA) or reverse shoulder arthroplasty (RSA) have been used in joint replacement surgery. We describe the epidemiology and trends in management of acute PHF in Denmark with a focus on (i) changes in the incidence of PHF; (ii) changes in the proportion of surgical cases; and (iii) changes in preferred surgical techniques.
Patients and methods — Data on diagnoses and interventions was retrieved from the Danish National Patient Register. Patients aged 18 years and above were included. Surgical treatment was defined as the diagnosis of PHF combined with a predefined surgical procedure code within 3 weeks of injury. Data on plate osteosynthesis, HA, RSA, and “other techniques” was retrieved. Non-surgical treatment was defined as no relevant surgical procedure code within 3 weeks.
Results — We identified 137,436 PHF (72% women) in the Danish National Patient Register. The overall mean incidence was 138/100,000/year (500 for women 60 years or above). Non-surgical treatment accounted for 119,966 (87%). The 17,470 surgical procedures included 42% locking plates, 34% arthroplasties, and 25% other techniques. The rate of surgery declined from 17% in 2013 to 11% in 2018.
Interpretation — The overall incidence of PHF remained stable between 1996 and 2018 but the absolute number increased. The approach to PHF remains predominantly non-surgical. The number of surgeries in Denmark have decreased since 2013, especially for locking plates and HA, while RSA is increasingly used.
Citation: Acta Orthopaedica 2022; 93: 750–755. DOI http://dx.doi.org/10.2340/17453674.2022.4578.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-05-19. Accepted: 2022-09-05. Published: 2022-09-20.
Correspondence: sbror@regionsjaelland.dk
SB had the idea for the study. All authors participated in the planning of the study. BV and PG provided the dataset. Data analysis was performed by PG, BV, and SO. SB drafted the manuscript. All authors participated in revision.
Acta thanks Carl Bergdahl and Elina Ekman for help with peer review of this study.
Proximal humeral fractures (PHF) are the third most common non-vertebral osteoporosis-related fractures (1). The fracture is closely related to age and sex with a lifetime risk of suffering a PHF in women aged 50 or above being 13% (2). PHF can be managed surgically or non-surgically. Modern surgical treatment includes head-preserving techniques with locking plates or locking intramedullary nails, while joint replacement with hemiarthroplasty (HA) or reverse shoulder arthroplasty (RSA) is used when head-preserving techniques are not amenable (3).
A growing number of high-quality randomized clinical trials (4-11) and meta-analyses (12) have been unable to demonstrate superiority of any surgical treatment modality compared with non-surgical management, thus challenging the operative approach to these fractures. In Denmark, an evidence-based national guideline recommending non-surgical management of displaced 2-, 3-, and 4-part fractures in the elderly was first published in 2015 (13). The impact of high-quality evidence and guidelines on clinical practice has only sporadically been studied (14) and national data on epidemiology and trends of management of PHF is sparse except for head replacements (15).
We describe the epidemiology and trends in management of acute PHF in adults in Denmark with a focus on (i) changes in the incidence of PHF; (ii) changes in the proportion of surgical cases; and (iii) changes in preferred surgical techniques.
Patients and methods
Study design
This is a population-based register study on PHF in adults from 1996 to 2018 reported to the Danish National Patient Registry (DNPR). Study reporting is performed according to the STROBE guidelines.
Setting
Approximately 5.9 million inhabitants live in Denmark and, at birth, every Danish citizen is issued a personal, 10-digit identification number. This allows for unambiguous linkage between all Danish medical databases, which ensures that every patient can be traced until death or immigration. The Danish National Health Service provides healthcare for all Danish citizens, guaranteeing free emergency, general hospital care, and outpatient visits (16), which is why the vast majority of patients suffering from a PHF are diagnosed and treated at a public hospital. We cannot rule out that some patients were treated at private facilities, but all fractures diagnosed after radiographic assessment, private or public, are coded for reimbursement and will appear in the DNPR.
Data sources
Patient data was obtained from the DNPR, which is a nationwide administrative database used for reimbursement of healthcare events. It contains individual longitudinal data on all patients discharged from a Danish non-psychiatric hospital both private and public since 1977. As departments are reimbursed for procedures reported to the DNPR the completeness of data is high. The diagnosis and surgical procedure codes for PHF have not been validated but the validity of orthopedic procedures and diagnosis in general have been shown to be high (17). Data is linked to the patient by a unique social security number given at birth or immigration. The DNPR holds data on all hospital admissions since 1977 and on all outpatient and emergency visits since 1995, including dates of admission and discharge and up to 20 diagnoses at discharge recorded according to the ICD (8th Revision until the end of 1993 and 10th Revision thereafter). In addition, the DNPR holds data on all surgical procedure dates and codes according to the Nordic Medico-Statistical Committee classification (18). Population data for incidence calculation was provided by the national registry Statistics Denmark (19).
The authors had complete access to data from the DNRP. This study draws on individual-level record linkage of data from nationwide medical registries using the unique civil registration number assigned to all citizens, which permits unambiguous record linkage between registries (17).
Participants
We included all patients with a PHF (ICD-10 DS42.2) aged 18 or above. We regard the natural history of pediatric fractures to be unique and decided to include only adult cases. The age groups 18–59 and 60 and above were analyzed separately, assuming that the elderly group mainly represented osteoporosis-related fractures, especially in women. The threshold for “acute” surgery was set at 3 weeks post-injury. Unlike some arthroplasty databases (15) we considered procedures performed in the 3rd week (e.g., reverse shoulder arthroplasty) as acute procedures. Consequently, fractures initially treated non-surgically but converted to surgery within the first 3 weeks will be analyzed as “acute” procedures. To reduce possible diagnostic coding errors due to readmissions and other unplanned visits within the first 90 days, a 90-day diagnosis “quarantine” period for DS42.2 was added. As most coding errors are likely to occur within the first 90 days after diagnosis we believe that we are close to the “true rate” or at least that the bias is comparable between the groups.
Variables
Surgical procedures were defined as a relevant surgical procedure code (NOMESCO codes, Table 1, see Supplementary data) within 3 weeks of injury (except closed reduction, KNBJ0*). The surgical procedure codes were further analyzed in 4 major surgical treatment modalities: plate osteosynthesis (KNBJ61), hemiarthroplasty (KNBB0* or KNBB1*), reverse arthroplasty (KNBB20, 30, 40, or 59), and “other techniques” covering K-wires, intramedullary nails, screws alone, cerclage, and combined techniques (KNBL*, KNBG*, and all KNBJ* procedures except KNBJ61 [plate] and KNBJ0* [closed reduction]). Nonoperative treatment was defined as no relevant surgical procedure code within 3 weeks.
Statistics
Descriptive statistics was used for reporting of age, sex, number of PHF, and treatment modalities. Incidences were reported as events/100,000/year based on the relevant yearly population data from Statistics Denmark.
Ethics, funding, and potential conflicts of interest
Data was provided by the DNPR based on diagnosis and procedure codes and was anonymized to the identity of the individual patients. Ethical approval was obtained (Region of Southern Denmark, jr.nr. 20/187). No funding was obtained. The authors have no conflicts of interest to declare.
Results
Between 1996 and 2018, 137,436 PHF were registered (Figure 1). Women accounted for 72% (Table 2, see Supplementary data). The incidence remained stable over the period (Figure 2) with an overall incidence of 138/100,000/year. An incidence of 500/100,000/year was found in women aged 60 years or above. The total annual numbers of PHF increased during the period following the general growth of the population.
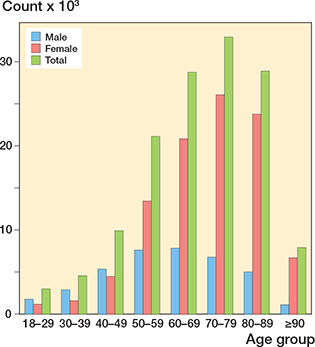
Figure 1. Number of proximal humeral fractures.
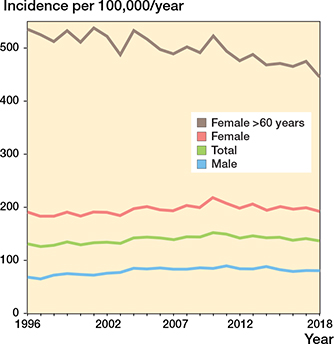
Figure 2. Incidence of proximal humeral fractures per 100,000/year.
17,470 cases (13%) were treated surgically with a peak of 17% in 2013, gradually declining to 11% in 2018 (Figure 3). For all patients aged 60 or above the percentage of surgically treatment declined from 17% in 2013 to 10% in 2018.
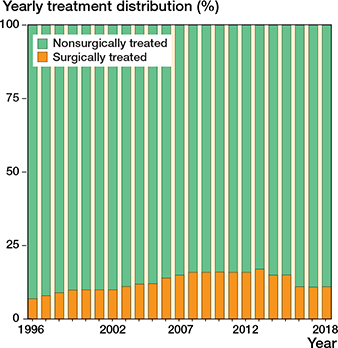
Figure 3. Yearly distribution of proximal humeral fractures.
Among the surgically treated cases, 7,331 (42%) received a locking plate osteosynthesis, and 5,850 (34%) received an arthroplasty (HA or RSA), while 4,289 (25%) were treated with other surgical techniques (Figure 4 and Table 3, see Supplementary data). In the population aged 60 or above the rate of locking plates remained stable from 2013 to 2018 (51% of all cases) while the rate of HA in this group decreased from 38% to 24% and RSA increased from 1% to 13%.
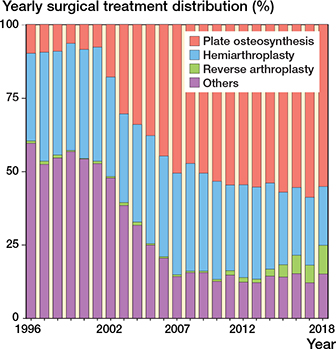
Figure 4. Yearly distribution of surgically treated proximal humeral fractures.
Discussion
Incidence rates
The overall incidence remained stable at around 138/100,000/year between 1996 and 2018, with the highest incidence in women aged 60 or above (500/100,000 per year). A Finnish study based on 79,676 PHF from national registries reported an overall incidence of 105/100,000 per year in a population aged 16 or above between 1997 and 2019. The incidence in the group above 80 years was 405/100,000 per year (both sexes). They further reported an increasing incidence over the period (20). This trend was not found in the Danish data, where incidences remained stable among both men and women during the period. However, a slight decrease was seen in women aged 60 and above. Decreasing incidence rates in Denmark have recently been reported in a registry-based epidemiological study of hip fractures in a population aged 60 and above between 1997 and 2017 (21).
A national study from Scotland collected data on 4,786 fracture patients within a 2-year period and calculated incidences (22). Females aged 65 and above had an incidence of PHF of 392/100,000/year while the incidence in females aged 80 and above was 520/100,000/year.
Trends in surgical management
In the Danish population, 87% of all PHF were managed non-surgically. The highest proportion of surgery was found between 2008 and 2013 (16–17%) with a gradual decline to 11% in 2018 (Figure 3).
About half of all PHF were found to be minimally displaced in a large epidemiological study from Edinburgh (23), leaving the rest for surgical consideration. Assuming this distribution applies to a Danish population, about one-third of all displaced PHF were treated surgically between 2008 and 2013 in Denmark.
Substantial national differences in the use of surgical management of PHF can be found, even in countries geographically and culturally close to Denmark. In Germany, between 2007 and 2016 a 39% increase in surgery for PHF was reported. Among the surgeries 72% were osteosyntheses and 69% of the surgeries were performed in geriatric patients. 35,000 surgeries for PHF were performed in Germany in 2016, with locking plates being the most popular implant (24). The high, and even increasing, number of surgeries is remarkable, as several high-quality randomized trials have been published within the same period, all failing to demonstrate superiority of locking plate osteosynthesis for PHF in the elderly.
From a historical perspective, at the turn of millennium locking plates were developed and manufactured followed by an increase in surgical activity in the following decade. This has been reported in Sweden (25) and Finland (26). Non-locking plates may appear in our material, especially in the first 4–5 years of the study period. Similar, mini-plates and low-profile locking plates are not accounted for separately. The use of locking plates in PHF has still to be supported by strong evidence (27).
In Denmark, the number and proportion of HA decreased from 2013 while RSA increased (Figure 4). The trend of decreasing use of HA is a general trend in the Nordic countries and has been reported in a common dataset from the Nordic shoulder arthroplasty registries covering 6,756 humeral head replacements after PHF between 2004 and 2013 (28). The number of RSA is rapidly increasing, which has been reported for the Nordic countries between 2004 and 2016 (29). In the Danish Shoulder Arthroplasty Registry dismal reports of patient-reported outcome after HA can be found (15). There is hope for improved outcome after RSA but the amount of both registry-based data and randomized trials is still limited.
No safe causal relations can be derived from cross-sectional data. However, a remarkable, albeit small, decrease in surgical activity is noted after the first clinical guideline was published in 2015 by the Danish Orthopaedic Association (13). The guideline recommends a non-surgical approach to 2-, 3-, and 4-part fractures in patients aged 60 and above. It was partly based on the Profher trial (8) and the Cochrane review (12) published in the same year.
In Sweden, between 2001 and 2012 the proportion of surgically treated patients with PHF increased from 12% to 17% in women and from 15% to 17% in men (25). In South Korea, between 2008 and 2016, the overall operative rate for PHF increased from 25% to 37%. In the same period, osteosynthesis increased from 72% to 86% of all surgeries (30). In Finland, a substantial increase in the incidence of surgery and especially in osteosynthesis has previously been reported. Between 1987 and 2009 the incidence of surgery raised from 5.1/100,000/year in 1987 to 19.6/100,000/year in 2016. The use of osteosynthesis became increasingly popular from 2002 with the incidence rising from 4.2/100,000/year in 1987 to 14.5/100,000/year in 2009 (26). However, in 2019 the overall incidence of surgical treatment in Finland decreased to 13/100,000/year with a substantial decrease in plate osteosynthesis (20). In the United States, between 1999–2000 and 2004–2005 a relative increase of 26% in surgery for PHF has been reported (31). The percentage of PHF treated surgically increased from 35% in 2004 to 41% in 2012 (32). In New York State, between 1990 and 2010 a rise in surgery in elderly patients from 20% to 29% was reported (33).
Other trends can be found. In Australia, from 2008 to 2017 operative management of PHF decreased from 33% to 23%. The relative use of osteosynthesis decreased from 77% to 73%, and HA decreased from 19% to 3%, while RSA increased from 4% to 25% (34).
A Swedish single-center study of 4,070 PHF reported an average proportion of surgically treated fractures (2011–2017) of 23%. Among the operated cases, the proportion of locking plates decreased from 47% to 25% while the proportion of RSA increased from 2% to 19% (35).
What is the optimal surgery rate?
This question can only be addressed in an evidence-based fashion by considering clinical outcome data. Although substantial uncertainty of estimates remains, we have high-quality data from randomized trials unambiguously suggesting non-superiority of surgery in 2-, 3-, and 4-part fractures in the elderly (4-11).
According to the epidemiological study by Court-Brown et al. (23), about half of all PHF are minimally displaced and therefore not considered for surgery. Displaced 2-part surgical neck fractures (mean age 70 years) account for 28% of all PHF, 3-part greater tuberosity fractures account for 9% (mean age 73 years), and 4-part fractures account for 2% (mean age 72 years). If we assume this distribution, current evidence leaves roughly 12% for surgical consideration. Some younger patients are likely to be added and some elderly with isolated tuberosity fractures are likely to be subtracted. We do not have high-quality clinical outcome data for younger patients, fracture-dislocations, articular surface fractures, polytrauma, pathological fractures, and isolated tuberosity fractures.
The current national variations in practice may be influenced by factors such as surgical tradition, education, population characteristics, implant promotion, reimbursement practice, and insurance coverage. A decline in surgical activity can be expected in countries with high rates of surgery with further implementation of evidence-based practice.
Strengths and weaknesses
The strength of the study is the comprehensive dataset derived from national administrative registries. It is the first report of rates of surgery as well as head-preserving surgical techniques for PHF in Denmark adding to data from existing arthroplasty registries.
The cut-off values for age and time to surgery may be discussed. We chose an age limit of 60 years to distinguish mainly osteoporotic fractures from mainly non-osteoporotic fractures. The limit also corresponds to the lower age limit in several randomized trials and guidelines and may therefore add to the comparability of data.
We decided to define “acute” as less than 3 weeks from injury. This reflects the fact that the “window” for surgery has widened since the advent of RSA. Some arthroplasty registries use 2 weeks as the limit because of worsened outcome for HA after 2 weeks. In RSA, however, it is usually possible to perform a stable reconstruction of the tuberosities and the rotator cuff to the prosthesis after 3 weeks. Intramedullary nailing of metaphyseal PHF may also be feasible after 3 weeks.
Bergdahl et al. (35) demonstrated problems with coding in the Swedish National Patient Registry. However, the DNPR differs from the Swedish National Patient Registry in several aspects. In DNPR all healthcare contacts are time coded and there is a possibility for laterality coding. We added a 90-day “quarantine” period for PHF diagnosis code (DS42.2) to reduce possible erroneous coding and to reduce the risk of a fracture being added to the study population more than once. Furthermore, if a fracture was reported to the DNPR within the study period all subsequent reporting of a fracture-related procedure on the same side was regarded as a reoperation and deleted from the study population.
A weakness of this study is the lack of validation for the PHF diagnosis and surgical procedure in the DNPR. However, the validation of orthopedic diagnosis and procedures in the DNPR in general is high (17) and we have no reason to believe that reporting to the register changed during the study period.
In conclusion, the incidence of PHF was stable between 1996 and 2018. The Danish approach to PHF in adults has remained predominantly non-surgical. However, minor temporal trends can be found, including a peak in surgical activity between 2008 and 2013 followed by a decline from 2013 to 2018.
Factors adding to the observed temporal trend may include increasing surgical activity after promotion of locking plates in the first decade followed by a decade of cumulating high-quality evidence failing to demonstrate superiority of surgery.
- Brorson S, Palm H. Proximal humeral fractures: the choice of treatment. In: Falaschi P, Marsh D, editors. Orthogeriatrics: the management of older patients with fragility fractures. Springer 2021: p. 143-53. doi: 10.1007/978-3-030-48126-1.
- Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporos Int 2005; 16(Suppl. 2): S3-7. doi: 10.1007/s00198-004-1702-6.
- Brorson S. Fractures of the proximal humerus. Acta Orthop Suppl 2013; 84: 1-32. doi: 10.3109/17453674.2013.826083.
- Fjalestad T, Hole M, Hovden I A, Blücher J, Strømsøe K. Surgical treatment with an angular stable plate for complex displaced proximal humeral fractures in elderly patients: a randomized controlled trial. J Orthop Trauma 2012; 26: 98-106. doi: 10.1097/BOT.0b013e31821c2e15.
- Fjalestad T, Hole M. Displaced proximal humeral fractures: operative versus non-operative treatment—a 2-year extension of a randomized controlled trial. Eur J Orthop Surg Traumatol 2014; 24: 1067-73. doi: 10.1007/s00590-013-1403-y.
- Olerud P, Ahrengart L, Ponzer S, Saving J, Tidermark J. Internal fixation versus nonoperative treatment of displaced 3-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elbow Surg 2011; 20: 747-55. doi: 10.1016/j.jse.2010.12.018.
- Olerud P, Ahrengart L, Ponzer S, Saving J, Tidermark J. Hemiarthroplasty versus nonoperative treatment of displaced 4-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elbow Surg 2011; 20: 1025-33. doi: 10.1016/j.jse.2011.04.016.
- Rangan A, Handoll H, Brealey S, Jefferson L, Keding A, Martin B C, et al. Surgical vs nonsurgical treatment of adults with displaced fractures of the proximal humerus: the PROFHER randomized clinical trial. JAMA 2015; 313: 1037-47. doi: 10.1001/jama.2015.1629.
- Launonen A P, Sumrein B O, Reito A, Lepola V, Paloneva J, Jonsson K B, et al. Operative versus non-operative treatment for 2-part proximal humerus fracture: a multicenter randomized controlled trial. PLoS Med 2019; 16: e1002855. doi: 10.1371/journal.pmed.1002855.
- Boons H W, Goosen J H, van Grinsven S, van Susante J L, van Loon C J. Hemiarthroplasty for humeral four-part fractures for patients 65 years and older: a randomized controlled trial. Clin Orthop Relat Res 2012; 470: 3483-91. doi: 10.1007/s11999-012-2531-0.
- Lopiz Y, Alcobía-Díaz B, Galán-Olleros M, García-Fernández C, Picado A L, Marco F. Reverse shoulder arthroplasty versus nonoperative treatment for 3- or 4-part proximal humeral fractures in elderly patients: a prospective randomized controlled trial. J Shoulder Elbow Surg 2019; 28: 2259-71. doi: 10.1016/j.jse.2019.06.024.
- Handoll H H, Brorson S. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev 2015; 10.1002/14651858.CD000434.pub4: Cd000434.
- Danish Orthopaedic Association. [Surgical versus non-surgical management of displaced proximal humeral fractures in the elderly]. 2015. Available from: https://www.ortopaedi.dk/wp-content/uploads/2019/10/Prox-humerusfraktur_Final.pdf.
- Jefferson L, Brealey S, Handoll H, Keding A, Kottam L, Sbizzera I, et al. Impact of the PROFHER trial findings on surgeons’ clinical practice: an online questionnaire survey. Bone Joint Res 2017; 6: 590-9. doi: 10.1302/2046-3758.610.BJR-2017-0170.
- Danish Shoulder Arthroplasty Register: Annual Report; 2020. p. 1–101. Available from: https://www.sundhed.dk/content/cms/3/4703_dsr_aarsrapport2020_offentliggoerelse.pdf.
- Schmidt M, Pedersen L, Sørensen H T. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol 2014; 29: 541-9. doi: 10.1007/s10654-014-9930-3.
- Schmidt M, Schmidt S A, Sandegaard J L, Ehrenstein V, Pedersen L, Sørensen H T. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 2015; 7: 449-90. doi: 10.2147/CLEP.S91125.
- NOMESCO Classification of Surgical Procedures. 2009. Available from: http://norden.diva-portal.org/smash/get/diva2:968721/FULL-TEXT01.pdf.
- Statistics Denmark. 2022. Available from: https://www.dst.dk/en.
- Leino O K, Lehtimäki K K, Mäkelä K, Äärimaa V, Ekman E. Proximal humeral fractures in Finland: trends in the incidence and methods of treatment between 1997 and 2019. Bone Joint J 2022; 104-b: 150-6. doi: 10.1302/0301-620X.104B1.BJJ-2021-0987.R1.
- Wahlsten L R, Palm H, Gislason G H, Brorson S. Sex differences in incidence rate, and temporal changes in surgical management and adverse events after hip fracture surgery in Denmark 1997–2017: a register-based study of 153,058 hip fracture patients. Acta Orthop 2021; 92: 424-30. doi: 10.1080/17453674.2021.1923256.
- Court-Brown C M, Clement N D, Duckworth A D, Aitken S, Biant L C, McQueen M M. The spectrum of fractures in the elderly. Bone Joint J 2014; 96-B:366-72. doi: 10.1302/0301-620X.96B3.33316.
- Court-Brown C M, Garg A, McQueen M M. The epidemiology of proximal humeral fractures. Acta Orthop Scand 2001; 72: 365-71. doi: 10.1302/0301-620x.83b6.11401.
- Klug A, Gramlich Y, Wincheringer D, Schmidt-Horlohé K, Hoffmann R. Trends in surgical management of proximal humeral fractures in adults: a nationwide study of records in Germany from 2007 to 2016. Arch Orthop Trauma Surg 2019; 139: 1713-21. doi: 10.1007/s00402-019-03252-1.
- Sumrein B O, Huttunen T T, Launonen A P, Berg H E, Felländer-Tsai L, Mattila V M. Proximal humeral fractures in Sweden: a registry-based study. Osteoporos Int 2017; 28: 901-7. doi: 10.1007/s00198-016-3808-z.
- Huttunen T T, Launonen A P, Pihlajamäki H, Kannus P, Mattila V M. Trends in the surgical treatment of proximal humeral fractures: a nationwide 23-year study in Finland. BMC Musculoskelet Disord 2012; 13: 261. doi: 10.1186/1471-2474-13-261.
- Brorson S. Locking plate osteosynthesis in geriatric shoulder fractures: why do we continue to perform a low-value procedure? Acta Orthop 2022; 93: 355-7. doi: 10.2340/17453674.2022.2208.
- Brorson S, Salomonsson B, Jensen S L, Fenstad A M, Demir Y, Rasmussen J V. Revision after shoulder replacement for acute fracture of the proximal humerus. Acta Orthop 2017; 88: 446-50. doi: 10.1080/17453674.2017.1307032.
- Lehtimäki K, Rasmussen J V, Kukkonen J, Salomonsson B, Arverud E D, Hole R, et al. Low risk of revision after reverse shoulder arthroplasty for acute proximal humeral fractures. JSES Int 2020; 4: 151-5. doi: http://dx.doi.org/10.1016/j.jses.2019.10.114.
- Jo Y H, Lee K H, Lee B G. Surgical trends in elderly patients with proximal humeral fractures in South Korea: a population-based study. BMC Musculoskelet Disord 2019; 20: 136. doi: 10.1186/s12891-019-2515-2.
- Bell J E, Leung B C, Spratt K F, Koval K J, Weinstein J D, Goodman D C, et al. Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. J Bone Joint Surg Am 2011; 93: 121-31. doi: 10.2106/JBJS.I.01505.
- Sabesan V J, Lombardo D, Petersen-Fitts G, Weisman M, Ramthun K, Whaley J. National trends in proximal humerus fracture treatment patterns. Aging Clin Exp Res 2017; 29: 1277-83. doi: 10.1007/s40520-016-0695-2.
- Khatib O, Onyekwelu I, Zuckerman J D. The incidence of proximal humeral fractures in New York State from 1990 through 2010 with an emphasis on operative management in patients aged 65 years or older. J Shoulder Elbow Surg 2014; 23: 1356-62. doi: 10.1016/j.jse.2013.12.034.
- McLean A S, Price N, Graves S, Hatton A, Taylor F J. Nationwide trends in management of proximal humeral fractures: an analysis of 77,966 cases from 2008 to 2017. J Shoulder Elbow Surg 2019; 28: 2072-8. doi: 10.1016/j.jse.2019.03.034.
- Bergdahl C, Wennergren D, Swensson-Backelin E, Ekelund J, Möller M. No change in reoperation rates despite shifting treatment trends: a population-based study of 4,070 proximal humeral fractures. Acta Orthop 2021; 92: 651-7. doi: 10.1080/17453674.2021.1941629.
Supplementary data