Correction of post-traumatic lower-limb discrepancy with Precice intramedullary lengthening nails: a review of 34 adults with an average follow-up of 2 years
Christof RADLER, Gabriel T MINDLER, Alexandra STAUFFER, Carina WEIß, and Rudolf GANGER
Department of Pediatric Orthopaedics, Orthopaedic Hospital Speising, Vienna, Austria
Background and purpose — We report results and complications of gradual bone lengthening for post-traumatic lower-limb length discrepancy (LLD) with Precice intramedullary lengthening nails in 34 adults.
Patients and methods — Inclusion criteria were lowerlimb lengthening using the Precice nail, posttraumatic etiology, age older than 18 years, and minimum follow-up of 12 months after implantation. 34 patients met the inclusion criteria. Radiological and clinical outcome data were collected.
Results — Precice lengthening was performed in the femur in 28 patients (21 antegrade, 7 retrograde) and in the tibia in 6. Mean patient age at time of surgery was 32 years (18–72). Mean preoperative LLD was 31 mm (20–71). Acute correction of axial or rotational malalignment was performed in 11 segments. At final follow-up (mean 2 years [1.1–3.6]), 33 of 34 nails had been removed. All lengthening sites were healed, and all patients mobilized with full weight-bearing. 14 adverse events occurred in 11 patients and were categorized as problems (n = 5), obstacles (n = 3), and complications (n = 6). Unplanned surgery was necessary in 7 patients, 3 of whom did not complete treatment with Precice.
Interpretation — Correction of posttraumatic LLD with or without axial malalignment using Precice intramedullary lengthening nails is associated with a low number of complications and good functional outcome. However, one-fifth of patients in this series needed further unplanned surgery for revision of obstacles or complications.
Citation: Acta Orthopaedica 2022; 93: 696–702. DOI https://doi.org/10.2340/17453674.2022.4513.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-04-21. Published: 2022-09-02.
Correspondence: christof.radler@oss.at
CR: study design, data analysis, preparation of manuscript; GTM: data acquisition; AS: data acquisition; CW: data acquisition; RG: manuscript review. All authors contributed to data analysis and writing of the manuscript.
The authors thank Dori Kelly, MA, for professional manuscript editing.
Acta thanks John Gerard Birch and Ulrik Kähler Olesen for help with peer review of this study.
Intramedullary (IM) limb lengthening has become increasingly popular because of faster rehabilitation, less pain, and higher patient comfort compared with external fixation (1). In our department, correction of post-traumatic shortening and malalignment was traditionally performed with hexapod external fixation frames (2). Although the overall outcome and anatomic results were encouraging, complications included pin infection, delayed ossification, limited range of motion (ROM), late bowing, nerve injury, and axial deviation (2). In 2013, we started using the Precice intramedullary lengthening nail in adults and children for various indications, including post-traumatic shortening.
Substantial deformity, narrow IM canal, and active infection are contraindications for the use of IM lengthening nails (3), limiting IM lengthening to more benign indications compared with external fixation. Associated problems with vascularity, reduced bone quality, and possible bacterial colonization might further complicate lengthening (4).
Previous reports on the use of IM lengthening nails often included small numbers of post-traumatic cases (5-7). Case series on post-traumatic lengthening are also limited (8-11), with only 1 recent study reporting a larger series of patients (12). We report the results of, and complications associated with, IM lengthening with the Precice nail to treat posttraumatic lower-limb length discrepancy (LLD) in 34 adult patients.
Patients and methods
We performed a single-center retrospective analysis of radiological and clinical data from a prospective consecutive patient database for lower-limb lengthening. Inclusion criteria were bone lengthening of the lower limb using a Precice IM lengthening nail, post-traumatic etiology, age older than 18 years, and minimum follow-up of 12 months after implantation. 161 patients underwent lengthening with a Precice nail at our institution between March 2013 and March 2020, of whom 34 patients met the inclusion criteria.
Surgical procedures
Precice nail implantation was performed according to predominant segment shortening and deformity. A femoral antegrade approach was considered for femoral LLD of 20 mm or more without relevant frontal plane knee deformity. Retrograde femoral nail implantation was considered in cases with femoral LLD and frontal or sagittal plane deformity; the reverse planning method presented by Baumgart (13) was performed for each case. Tibial nail implantation was performed for tibial shortening with and without deformity. For retrograde femoral and tibial nail implantation, blocking screws were used to stabilize acute correction or to prevent deformity during lengthening.
Postoperative physical therapy with hip, knee, and ankle mobilization started on the 1st postoperative day for all patients. Until consolidation of 2 to 3 cortices, touch-down to partial weight-bearing mobilization using 2 crutches was allowed, largely depending on patient weight, nail diameter, and compliance. Using Precice Stryde nails, partial weightbearing was allowed as soon as tolerated and full weight-bearing was allowed from consolidation of 1 to 2 cortices.
Full-length anteroposterior (AP) view radiographs (hip to ankle) of both lower limbs in standing position with a calibration marker and lateral view radiographs of the femur or tibia in standing and non-standing positions with a magnification marker were obtained preoperatively and at various times during follow-up. Radiographs of the bone lengthened, including the adjacent joints, were obtained every 1 to 2 weeks and every 6 weeks at the end of distraction. Deformity analysis included standard measurements (14) using only full-length standing radiographs. The residual LLD and mechanical axis deviation (MAD) were measured. Complications were extracted from the database and categorized into problems, obstacles, and complications according to Paley (15). The weight-bearing index (WBI), defined as days from surgery to full weight-bearing per centimeter of lengthening, and the healing index (HI), defined as days from surgery to full bone healing per centimeter of lengthening, were calculated. ROM data were extracted from the patient file and had been collected with the use of a hand-held goniometer during clinic visits.
34 patients were treated with 34 Precice nails (28 femoral and 6 tibial nails). The 6 female and 28 male patients had a mean age of 32 years (18–72). In the 28 femoral cases, the nail was inserted from an antegrade approach in 21 and from a retrograde approach in 7.
Age at time of trauma was available for 31 patients: average, 20 years (0.9–59). Details on severity or classification of the initial fracture were not available. However, 20 patients presented with changes to the bone structure and/or bone integrity visible on plain radiographs and 9 patients underwent removal of fixation simultaneously with implantation of the Precice nail. 3 patients were previously treated with external fixation. 8 of 34 patients were known smokers.
Mean preoperative LLD was 31 mm (20–71). Additional acute correction of axial or torsional malalignment was planned in 11 segments (8 frontal plane malalignment, 1 maltorsion, 2 combined corrections). Frontal plane axial correction was performed in the tibia in 5 patients and in the femur with a retrograde approach in 5 patients. Correction of torsional malalignment was performed in 1 femur using an antegrade approach.
For antegrade femoral lengthening, 12 trochanteric entry nails with a 10° bend and 9 piriformis entry straight nails were used. 2 of the 34 nails were Precice Stryde nails.
Ethics, funding, and potential conflicts of interest
Ethical approval was granted by the local ethics committee (EK02/2020). Written informed consent was received from patients before inclusion. No outside funding was received for this study. CR and RG have received personal fees from Smith & Nephew Europe and from NuVasive Inc for professional consulting and presentations. No potential conflicts of interest are declared by the other authors.
Results
At final follow-up (mean, 2 years [1.1–3.6]), 33 of 34 nails had been removed; 1 patient died before nail removal as the result of an unrelated cause. All lengthening sites were healed, and all patients mobilized with full weight-bearing.
Problems, obstacles, and complications
14 adverse events occurred in 11 of the 34 patients and were categorized as problems (n = 5), obstacles (n = 3), and complications (n = 6) (Figure 1). The 5 problems comprised delayed consolidation, all treated nonoperatively. 1 patient with delayed consolidation also encountered an obstacle: a migrated most proximal locking screw in an antegrade nail, which became painful and had to be removed. Another patient experienced loosening and migration of a retrograde femoral nail distal locking screw in soft bone, which was secured by adding a small plate (Figure 2). In another, a painful transmalleolar screw had to be removed before nail removal.
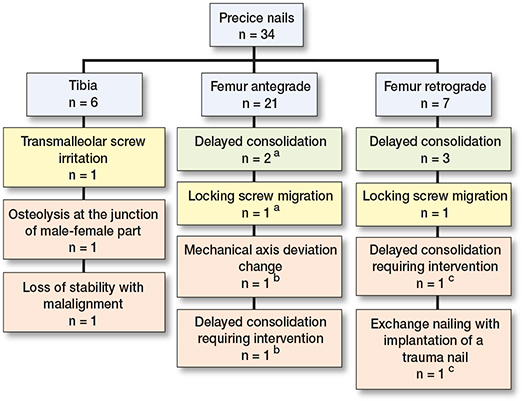
Figure 1. Subclassification of difficulties occurring during limb lengthening into problems (yellow), obstacles (green), and complications (red). a One patient with delayed consolidation encountered an additional obstacle. b Another patient who underwent instillation of BMP showed an increase of medial MAD from –8 to –20 mm and also delayed consolidation. c Delayed consolidation and nail exchange in the same patient.

Figure 2. Postoperative radiographs show that the distal locking screws are in a good position (a). Only 9 days later, the screws were migrating (b). During revision, the bone appeared especially soft and a small plate was added to secure the screws (c). Lengthening of 2 cm was successful, full weight-bearing was possible after 4 months, the bone went on to full healing (d), and the nail was removed 2 years after the index procedure.
6 complications occurred in 4 of 34 patients. 1 patient with delayed consolidation underwent exchange nailing with implantation of a trauma nail and, 18 months later, bone grafting with bone morphogenic protein (BMP-2, InductOs; Medtronic, Minneapolis, MN, USA) to treat lateral callus deficit. Bone grafting with instillation of BMP was necessary in a second case. In that case, the MAD changed from –8 to –20 mm, which was considered a complication. 1 patient presented loss of stability with malalignment and nonunion during distraction, which was treated by nail removal and application of a Taylor spatial frame (TSF; Smith+Nephew, Memphis, TN, USA) within 1 surgery. The 4th patient who encountered a complication presented with painful swelling and osteolysis at the male–female junction of the nail (Stryde nail). Osteomyelitis was suspected, and the nail was removed. Considering that consolidation was not completed and weak callus was present on the anteromedial side, an external fixator was applied for 2 months to prevent fracture. In summary, 7 of 34 patients required unplanned additional surgery.
Radiological outcome
All further analyses were performed for all patients except the 3 with procedural change (exchange nailing, TSF application, external fixator application). Results of the analyses were therefore available for 31 patients.
Mean planned lengthening was 28.3 mm (20–50 mm), and mean achieved lengthening was 27.9 mm (16–55 mm). Mean final residual LLD was 3.8 mm (range, 4 mm over-lengthening to 23 mm residual shortening). 3 patients had residual LLD > 10 mm (15, 16, and 23 mm). They had preoperative LLD > 70 mm with planned lengthening of 50 mm; the planned lengthening was achieved in those 3 (Figure 3). 1 patient had residual LLD of 9 mm. That patient had LLD in the preoperative full-length AP view radiograph in standing position with a calibration marker of 21 mm. The distraction gap measured 20 mm at the time lengthening was stopped, and a distraction gap of 20 mm was found on all subsequent radiographs, which indicates a functional/secondary reason for the residual LLD or inaccurate positioning during the preoperative radiography. All other patients (n = 30) had residual LLD ≤ 7 mm and thereby achieved their lengthening goals.
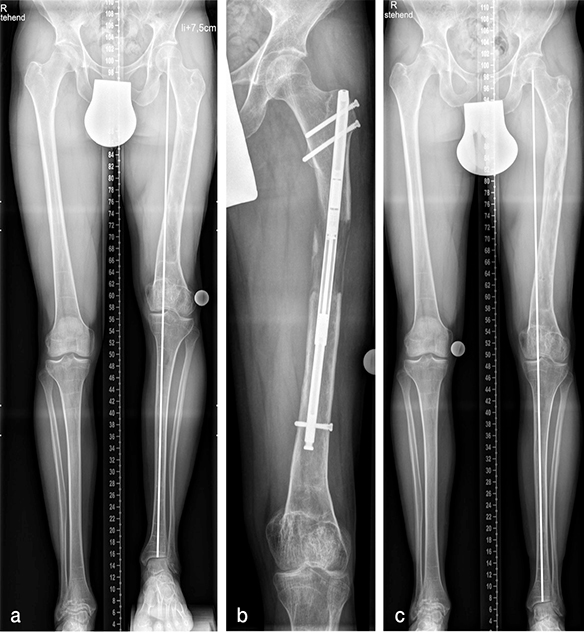
Figure 3. Patient sustained a distal femoral fracture age 8 years, had undergone previous lengthening with external fixation and bone grafting elsewhere, and presented with an LLD of 75 mm (a). Mild varization of the proximal fragment occurred during lengthening, which counteracted the valgus effect of lengthening along the anatomic axis, resulting in a change of the MAD from 16 mm medial to 14 mm medial (b). A final LLD of 16 mm was well accepted, and the planned lengthening of 5 to 6 cm was achieved (c).
In 23 patients, no deformity correction and thereby no correction of the mechanical axis was intended. In these patients, the mean change of the mechanical axis was 0.6 mm (from –12 mm [varus direction] to +12 mm [valgus direction]). The mechanical axis remained unchanged (±3 mm) in 14 patients, was improved in 6, and worsened in 3. Those 3 patients had undergone femoral lengthening through an antegrade approach. The MAD changed from –8 mm to –13 mm in 1, from –5 mm to –10 mm in another, and from –8 mm to –20 mm in the 3rd patient. The latter was considered a complication.
Simultaneous mechanical axis correction was performed in 8 patients: 5 femoral corrections (4 retrograde and 1 antegrade approach) (Figure 4) and 3 tibial corrections. In all patients, the desired correction was achieved. In 1 patient, a torsional deformity of 20 degrees was corrected during the insertion of a femoral antegrade nail. In 5 patients, valgus deformity with an average MAD of 16 mm lateral (9–24 mm) was corrected to a MAD of 1.2 mm varus (2 mm residual valgus MAD to 8 mm varus MAD). 2 patients underwent correction of varus MAD of –33 mm and –22 mm to –8 mm and –7 mm, respectively.
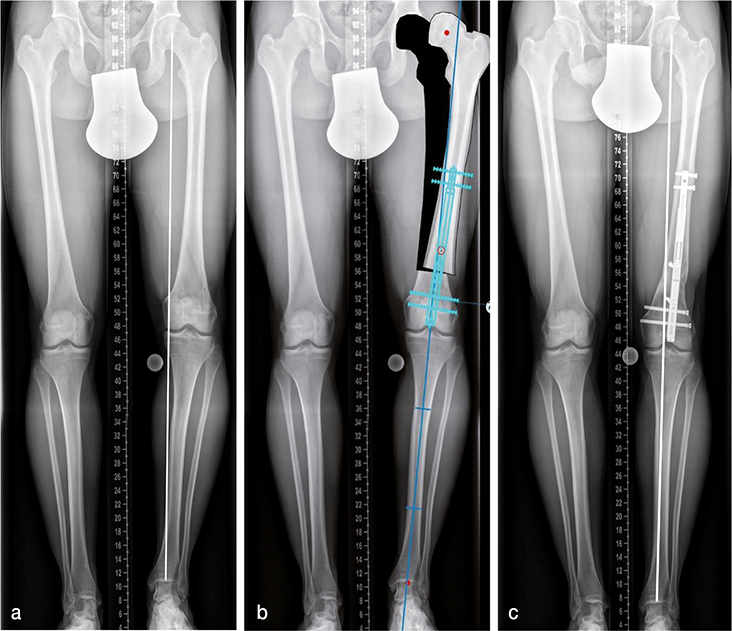
Figure 4. At age 15 years, the patient had an accident snowboarding and sustained a femoral fracture involving the growth plate. At age 25 years, he presented to us with a shortening of 25 mm and a varus deformity that we planned to correct acutely during surgery (a,b). Radiographs obtained before nail removal show no residual LLD and a physiological MAD of 8 mm medial (c).
WBI and HI
The mean WBI, defined as days from surgery to full weightbearing without any aid per centimeter of lengthening, and the average healing index (HI), defined as days per centimeter from surgery to full bone healing (4 cortices), are presented in Table 1.
Functional outcome
4 patients had knee extension deficits from 5° to 10°at the end of distraction, 3 having undergone antegrade and 1 having undergone retrograde femoral lengthening. Only 1 tibial lengthening resulted in a substantial limitation of ankle ROM with 10° of equinus at the end of distraction. Knee and ankle ROM had returned to preoperative values in all patients at final follow-up, except in 1 patient who had undergone 5.5 cm of lengthening through an antegrade femoral approach who experienced a decrease of knee flexion from 130° to 90°.
Discussion
Our series includes patients with shortening resulting from childhood trauma and/or physeal damage and patients who sustained fractures in adult life with fixation devices in place and marked changes in bone structure and/or bone integrity. Because of the low number of cases, we were not able to statistically compare those 2 groups.
Complications
4 of the 6 complications encountered occurred in patients who sustained fractures in adult life and were operated on at ages 52 and 54 years, respectively. 1 of these presented with loss of stability of the nail and malalignment during distraction, necessitating nail removal and application of a TSF. He presented initially with shortening of 36 mm, malalignment, and muscle flap after an open tibial fracture sustained in a motor vehicle accident. The second patient had early signs of arthritis and osteoporosis and shortening of 49 mm. The initial fracture type was not clear. Retrospectively, we would refrain from using a lengthening nail in those cases and recommend a hexapod frame. This emphasizes the importance of patient selection, as previously indicated by Teulières et al. (12).
6 complications in 4 of 34 patients compares favorably with complications reported in the literature (10,16,17). Teulières et al. (12) found fewer complications (2 of 34 patients) but more obstacles (14 of 34 compared with our 3 of 34). Screw migration was less common in our series, which might be associated with the different type of implant used. Additionally, we were conservative regarding weight-bearing because the series includes our learning curve with 1st generation nails with possible back-tracking and crown fracture (18). This might have reduced our rate of device-related complications; however, it most likely led to high WBI and HI, a correlation recognized by Calder et al. (19). The number of device-related complications was notably low compared with a systematic review of complications associated with lengthening nails (16). In 1 case, osteomyelitis was suspected because of a severe periosteal reaction and focal lysis at the male–female junction and the nail was removed. This was before we became aware of frequent secondary bone changes at the male–female part of the Precice Stryde nails (20). We cannot determine whether the suspected osteomyelitis or an implant-associated complication occurred; however, cultures and sonication were negative.
Rate of revision surgery
The rate of revision surgery was high in our series, with 7 of 34 patients undergoing an unplanned procedure before nail removal (3 were minor). Frost et al. (16) found complications resulting in substantial change of treatment, such as revision surgery, in 15%. Kirane et al. (21) reported that 7 of 24 patients underwent unplanned revision surgery in an early and mixed series of patients; 2 of the 7 were treated for delayed bone healing, which was also the reason for revision surgery in 2 of our patients. In our series of children and adolescents who had undergone limb lengthening with Precice IM lengthening nails, only 6 of 76 patients required unplanned revision surgery (22). Brinker et al. (11) presented a report of 8 adult patients with post-traumatic LLD, all of which was fully corrected without any unplanned surgery.
Delayed healing
Delayed healing occurred in 6 of our 34 patients, with 1 patient needing bone grafting to achieve union. Delayed healing with a high WBI was mostly associated with short lengthening distances between 2 and 3 cm (Table 2). Small amounts of lengthening are known to produce a higher external fixation index (number of months of external fixation per centimeter of lengthening) (2), which can also be applied to the WBI; neither increases linearly in relation to lengthening (2). However, all 6 patients presented risk factors of smoking, previous delayed union, or comminuted fracture pattern. Additionally, 3 of the 6 underwent acute correction of valgus malalignment, which can delay bone healing through manipulation at the osteotomy site to achieve correction and less bone contact after translation. The comparable series from Teulières et al. (12) included adult patients with post-traumatic shortening. The authors found a similar rate of delayed healing in 5 of 34 cases. The systematic review of complications with IM lengthening nails found bone healing complications in 5% of patients with mixed etiologies (16), again indicating that adult patients with post-traumatic shortening compare less favorably with pediatric patients and with non-post-traumatic cases.
| WBI days/cm | LLD mm | Age | Approach | Axial correction | Additional factors | |
| 1 | 103 | 25 | 22 | Femur retrograde | Valgus | Smoker |
| 2 | 104 | 20 | 22 | Femur retrograde | Valgus | Smoker |
| 3 | 109 | 27 | 30 | Femur antegrade | a | |
| 4 | 118 | 20 | 18 | Tibia | Valgus | Smoker |
| 5 | 126 | 22 | 31 | Femur antegrade | Smoker | |
| 6 | 137 | 29 | 21 | Femur antegrade | b | |
| a Comminuted fracture; removal of proximal femoral nail simultaneously b TSF lengthening in childhood with delayed union and bone grafting |
||||||
WBI and HI
The WBI seems to be the most practical and clinically relevant bone index for IM limb lengthening. We found a mean WBI of 65 days/cm, with 61 days/cm for antegrade femoral lengthening, 71 days/cm for retrograde femoral lengthening, and 72 days/cm for tibial lengthening. In a series of patients younger than 18 years, we found a mean overall WBI of 45 days/cm with 40 days/cm for antegrade femoral, 48 days/cm for retrograde femoral, and 65 days for tibial lengthening (22), which demonstrates the longer bone healing in adult compared with adolescent patients.
Full weight-bearing without aid was achieved at an average of 168 days (85–396), which falls within the numbers reported in the literature: from an average of 119 days (10) to an average of 226 days (12). Hammouda et al. (10) reported 119 days until regenerate consolidation with full weight-bearing for 8 of 17 patients who were younger than 18 years at time of surgery. Nevertheless, our WBI is high and possibly associated with our weight-bearing recommendations. With the introduction of P2 nails, we changed to a more progressive weight-bearing regime, allowing partial weight-bearing as soon as signs of callus were visible on radiographs. Using the Precice Stryde nail, we recommended partial weight-bearing from day 1 after surgery and full weight-bearing after confirmation of consolidation of 1 or 2 cortices and found a substantial increase in bone healing. However, because of problems with osteolysis and corrosion reported in the literature (20,23,24) and osteolysis possibly being associated with 1 complication in this series, we discontinued using the Stryde nail, which was subsequently taken off the market.
We defined the HI as days from surgery to healing of all 4 cortices and thereby found high numbers compared with mixed case series and with series in which healing was defined as healing of 3 cortices and/or healing until a fixator could be removed (17,19). Compared with the series presented by Teulieres et al. (12), our HI was slightly higher.
Residual LLD and MAD
30 patients had residual LLD ≤ 7 mm, and a final LLD ≤ 5 mm was achieved in 24 of the 31 patients. In another series, only 12 of 34 patients had final LLD ≤ 5 mm, which was attributed to the complexity of the deformities and noncompliance (12). We agree that this is a group of patients less likely to follow weightbearing and distraction recommendations, which highlights the need for preoperative patient selection and counseling.
Accurate lower-limb length equalization is challenging because several factors affect the outcomes and accuracy of radiographic interpretation. Decision-making regarding lengthening is based on preoperative radiographs obtained with both lower limbs in standing position with blocks to compensate for shortening. Lower-limb length measurements might be inaccurate if radiographs are obtained during mild knee flexion, knee hyperextension, or uneven stance. The same radiographic technique cannot define the goal and end of postoperative lengthening. Because of partial weight-bearing, the patient cannot stand evenly, presenting a risk of knee extension or ankle dorsiflexion deficit that can affect measurements. Additionally, antegrade femoral lengthening can lead to an oblique pelvic tilt because of muscle shortening. Measurement of the length from the distraction gap or from the length change of the male distraction rod can also lead to bias. A drill is used for the corticotomy, which removes some bone, and mild acute distraction can occur with nail insertion. To overcome these issues, we measured the male component of the Precice nail system to evaluate the distraction of the nail and the distraction gap in both the AP and lateral planes to measure true lengthening.
An unintentional substantial change to a more unphysiological mechanical axis was observed in 1 patient to a MAD of –20 mm and was considered a complication. A comparable observation was reported by Horn et al. (17), who found a shift of the mechanical axis 10 mm medially in 1 patient in a series that included 20 patients with post-traumatic shortening.
Deformity correction
Deformity correction was performed in 8 patients, and the desired correction was achieved in all. Blocking screws were used in these patients to maintain correction and prevent recurrence of malalignment during lengthening. Horn et al. (17) found mild residual deformity in 5 patients who underwent simultaneous axis correction. In a previous series of patients aged 18 years or younger, we encountered malalignment as a result of lengthening or over- and under-correction in 5 of 16 tibial lengthening cases (22), a problem we did not find in the current 6 tibial cases (Figure 5), possibly because larger adult bones allow placement of more blocking screws around the nail. We did not observe any joint contracture, and only 1 patient had limited knee ROM at final follow-up. Physical therapy was initiated on the 1st postoperative day, and a passive motion machine was applied during inpatient treatment and for the 1st 2 weeks after surgery for femoral lengthening. Patients participated in physical therapy at weekly outpatient visits and weekly therapy conducted outside of the hospital. For excessive lengthening or in cases of especially tight iliotibial band, the iliotibial band was cut during surgery as previously recommended (19).

Figure 5. Tibial fracture was treated with a locking nail in Mongolia, which resulted in a good axial alignment but a shortening of 35 mm (a). The nail was removed, and a Precice nail was inserted adding blocking screws and tibia–fibula transfixation proximally and distally. Distraction was started 1 week after surgery at a rate of 0.75 mm per day (b). No residual LLD or malalignment was observed on the radiographs before nail removal (c).
Conclusions
In conclusion, gradual correction of post-traumatic LLD with or without axial malalignment using Precice IM lengthening nails is associated with a low number of complications and good radiological and functional outcomes. However, onefifth of patients needed further unplanned surgery for revisions of obstacles or complications. Although delayed healing was found to occur independent of patient age, the combination of older age and more severe initial injury seems to complicate the lengthening procedure. Prolonged partial weight-bearing might minimize device-related complications but seems to result in slower bone healing.
Reference
- Landge V, Shabtai L, Gesheff M, Specht S C, Herzenberg J E. Patient satisfaction after limb lengthening with internal and external devices. J Surg Orthop Adv 2015; 24(3): 174-9.
- Ganger R, Radler C, Speigner B, Grill F. Correction of post-traumatic lower limb deformities using the Taylor spatial frame. Int Orthop 2010; 34(5): 723-30. doi: 10.1007/s00264-009-0839-5.
- Alrabai H M, Gesheff M G, Conway J D. Use of internal lengthening nails in post-traumatic sequelae. Int Orthop 2017; 41(9): 1915-23. doi: 10.1007/s00264-017-3466-6.
- Axelrod D, Rubinger L, Shah A, Guy P, Johal H. How should we lengthen post-traumatic limb defects? A systematic review and comparison of motorized lengthening systems, combined internal and external fixation and external fixation alone. Eur J Orthop Surg Traumatol 2021; 31(6): 1015-22. doi: 10.1007/s00590-020-02831-y.
- Krieg A H, Lenze U, Speth B M, Hasler C C. Intramedullary leg lengthening with a motorized nail. Acta Orthop 2011; 82(3): 344-50. doi: 10.3109/17453674.2011.584209.
- Thaller P H, Fürmetz J, Wolf F, Eilers T, Mutschler W. Limb lengthening with fully implantable magnetically actuated mechanical nails (PHENIX(®)): preliminary results. Injury 2014; 45(Suppl. 1): S60-5. doi: 10.1016/j.injury.2013.10.029.
- Paley D, Harris M, Debiparshad K, Prince D. Limb lengthening by implantable limb lengthening devices. Tech Orthop 2014; 29(2): 72-85.
- Lenze U, Hasler C C, Krieg A H. Intramedullary motorized nail for equalization of posttraumatic leg length discrepancies [in German]. Unfallchirurg 2011; 114(7): 604-10. doi: 10.1007/s00113-010-1820-x.
- Wang K, Edwards E. Intramedullary skeletal kinetic distractor in the treatment of leg length discrepancy: a review of 16 cases and analysis of complications. J Orthop Trauma 2012; 26(9): e138-44. doi: 10.1097/BOT.0b013e318238b5b1.
- Hammouda A I, Jauregui J J, Gesheff M G, Standard S C, Conway J D, Herzenberg J E. Treatment of post-traumatic femoral discrepancy with PRECICE magnetic-powered intramedullary lengthening nails. J Orthop Trauma 2017; 31(7): 369-74. doi: 10.1097/BOT.0000000000000828.
- Brinker M R, Amirian A, O’Connor D P, Laughlin M S. Efficacy of PRECICE nail in treatment of adult patients with posttraumatic femoral leg length discrepancy. J Orthop Trauma 2021; 35(8): e304-8. doi: 10.1097/BOT.0000000000002000.
- Teulières M, Langlais T, de Gauzy J S, Rölfing J D, Accadbled F. Bone lengthening with a motorized intramedullary nail in 34 patients with posttraumatic limb length discrepancies. J Clin Med 2021; 10(11): 2393. doi: 10.3390/jcm10112393.
- Baumgart R. The reverse planning method for lengthening of the lower limb using a straight intramedullary nail with or without deformity correction: a new method. Oper Orthop Traumatol 2009; 21(2): 221-33. doi: 10.1007/s00064-009-1709-4.
- Paley D, Tetsworth K. Mechanical axis deviation of the lower limbs: preoperative planning of uniapical angular deformities of the tibia or femur. Clin Orthop Relat Res 1992; (280): 48–64.
- Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res 1990; (250): 81-104.
- Frost M W, Rahbek O, Traerup J, Ceccotti A A, Kold S. Systematic review of complications with externally controlled motorized intramedullary bone lengthening nails (FITBONE and PRECICE) in 983 segments. Acta Orthop 2021; 92(1): 120-7. doi: 10.1080/17453674.2020.1835321.
- Horn J, Hvid I, Huhnstock S, Breen A B, Steen H. Limb lengthening and deformity correction with externally controlled motorized intramedullary nails: evaluation of 50 consecutive lengthenings. Acta Orthop 2019; 90(1): 81-7. doi: 10.1080/17453674.2018.1534321.
- Paley D. PRECICE intramedullary limb lengthening system. Expert Rev Med Devices 2015; 12(3): 231-49. doi: 10.1586/17434440.2015.1005604.
- Calder P R, McKay J E, Timms A J, Roskrow T, Fugazzotto S, Edel P, et al. Femoral lengthening using the Precice intramedullary limblengthening system: outcome comparison following antegrade and retrograde nails. Bone Joint J 2019; 101(9): 1168-76. doi: 10.1302/0301-620X.101B9.BJJ-2018-1271.R1.
- Rölfing J D, Kold S, Nygaard T, Mikuzis M, Brix M, Faergemann C, et al. Pain, osteolysis, and periosteal reaction are associated with the STRYDE limb lengthening nail: a nationwide cross-sectional study. Acta Orthop 2021; 92(4): 479-84. doi: 10.1080/17453674.2021.1903278.
- Kirane Y M, Fragomen A T, Rozbruch S R. Precision of the PRECICE internal bone lengthening nail. Clin Orthop Relat Res 2014; 472(12): 3869-78. doi: 10.1007/s11999-014-3575-0.
- Radler C, Mindler G T, Stauffer A, Weiß C, Ganger R. Limb lengthening with Precice intramedullary lengthening nails in children and adolescents. J Pediatr Orthop 2022; 42(2): e192-200. doi: 10.1097/BPO.0000000000002016.
- Frommer A, Roedl R, Gosheger G, Hasselmann J, Fuest C, Toporowski G, et al. Focal osteolysis and corrosion at the junction of Precice Stryde intramedullary lengthening device: preliminary clinical, radiological, and metallurgic analysis of 57 lengthened segments. Bone Joint Res 2021; 10(7): 425-36. doi: 10.1302/2046-3758.107.BJR-2021-0146.R1.
- Jellesen M S, Lomholt T N, Hansen R Q, Mathiesen T, Gundlach C, Kold S, et al. The STRYDE limb lengthening nail is susceptible to mechanically assisted crevice corrosion: an analysis of 23 retrieved implants. Acta Orthop 2021; 92(5): 621-7. doi: 10.1080/17453674.2021.1927506.