Outcomes of trabecular metal total ankle replacement: a longitudinal observational cohort study of 239 consecutive cases from the Swedish Ankle Registry
Anders HENRICSON 1, Alexandra UNDÉN 2,3, Åke CARLSSON 3,4*, Lars JEHPSSON 3,4, and Björn ROSENGREN 3,4
1 Department of Orthopedics, Falu Central Hospital and Center of Clinical Research Dalecarlia, Falun; 2 Department of Radiology, Skåne University Hospital, Malmö; 3 Department of Clinical Sciences Malmö (IKVM), Lund University; 4 Department of Orthopedics, Skåne University Hospital, Malmö, Sweden
Background and purpose — Information on outcomes after some modern total ankle replacement (TAR) designs is scarce. We therefore examined outcomes after trabecular metal (TM) TAR in Sweden by use of data from the national registry.
Patients and methods — On December 31, 2020, 239 primary TM TARs had been reported to the Swedish Ankle Registry. We analyzed prosthesis survival probability, using exchange or permanent extraction of components as endpoint for 239 protheses with mean follow-up of 2.2 years (0.1–6.6), risk of revision, as well as patient-reported outcome measures (SEFAS/EQ-5D/EQ-VAS) and satisfaction with surgery.
Results — 7/239 prostheses (3%) had been revised by December 31, 2020. We found an overall prosthesis survival probability of 95% (95% CI 89–98) after 3 years. 2 years after surgery 81% of the answering patients were satisfied or very satisfied with surgery and patients reported median SEFAS 36 (max 48), EQ-5D 0.90 (max 1), and EQ-VAS 80 (max 100).
Interpretation — We found short- to mid-term outcomes after TM TAR to be at least as good as after other TAR designs regarding prosthesis survival and patient-reported satisfaction.
Citation: Acta Orthopaedica 2022; 93: 689–695. DOI https://doi.org/10.2340/17453674.2022.4387.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2021-11-06. Accepted: 2022-06-21. Published: 2022-07-27.
Correspondence: anders.henricson@regiondalarna.se
AH and BR designed the study, AH, BR, and ÅC collected data, AH, LJ, and BR interpreted data and performed statistical analyses, AH and BR wrote the first version; all authors together finalized the manuscript.
Acta thanks Helkka Koivu, Markus Knupp, and Jan Willem Louwerens for help with peer review of this study.
Results of total ankle replacement (TAR) have gradually improved (1,2) but remain inferior to those after total hip and knee replacement (3). The most common cause of TAR revision is aseptic loosening (2,4,5). Trabecular metal (porous tantalum) coating has been used to improve fixation for various implants. Ingrowth and sufficient biological fixation in such implants have been shown both experimentally (6) and clinically in human specimens (7-9), and in long-term total knee replacement studies (10,11).
In relatively small short- and mid-term reports from different centers, the trabecular metal ankle (TM Ankle) has shown promising results (12-15). More data, preferably from independent, non-specialist centers is, however, needed.
We present real-world prosthesis survival probability and also PROM results for a large consecutive series of TM Ankles from a national cohort of patients by use of the Swedish Ankle Registry.
Patients and methods
Since 1993, Swedish hospitals performing TARs have reported information on date of index surgery and any revision surgery, together with data on the patient and the procedure, to the Swedish Ankle Registry. Reporting is made by the surgeon, except for PROMs and PREMs, which are reported by the patient. The current procedure-based coverage and completeness are both estimated at close to 100%.
The TM Ankle is a fixed-bearing 2-component total ankle prosthesis. The tibial and talar surfaces are coated with trabecular metal (porous tantalum). The surgical approach is transfibular, meaning that the fibular osteotomy must be fixated at the end of the procedure.
As at December 31, 2020, 239 TM Ankle (Zimmer Biomet, Warsaw, IN, USA) primary procedures in 233 patients were registered in the Swedish Ankle Registry. 6 patients underwent bilateral procedures, none simultaneously (Table 1). The procedures were performed at 11 different hospitals, 9 at 5 high-volume centers. In the 2 low-volume centers, most procedures were performed by, or with the aid of, a surgeon from a high-volume center.
| Category | N (%) | Mean (SD) or n (%) |
| Age | 239 (100) | 65 (11) a |
| Sex | 239 (100) | |
| Female | 109 (46) | |
| Male | 130 (54) | |
| BMI | 204 (85) | 28 (4.4) a |
| ASA | 237 (99) | |
| 1 | 57 (24) | |
| 2 | 149 (63) | |
| 3 | 31 (13) | |
| Side | 239 (100) | |
| Right | 121 (51) | |
| Left | 118 (49) | |
| Diagnosis | 239 (100) | |
| Post-traumatic osteoarthritis | 108 (45) | |
| Primary osteoarthritis | 72 (30) | |
| Rheumatoid arthritis | 38 (16) | |
| Psoriatic arthritis | 7 (3) | |
| Other | 14 (6) | |
| a Mean (SD) | ||
Preoperatively most patients were invited to answer PROM questionnaires (SEFAS and EQ-5D/EQ-VAS) at the location of their caregiver. At 3 time points after surgery including 2 years postoperatively questionnaires for SEFAS, EQ-5D/EQ-VAS, and satisfaction with surgery were sent to all patients. The validated SEFAS score has 12 questions, each graded by the patient from 0 to 4 (16). A total score of 0 points represents the most severe disability and 48 points represents normal function. EQ-5D has 5 dimensions: mobility, hygiene, main activities, pain, and anxiety/depression, each graded by the patient on a scale from 1 to 3: no problem (1), some problems (2), and severe problems (3). The answers are converted to an overall score between 1 and 0, where 1 is full health and 0 is dead. EQ-VAS records the patient’s self-rated health on visual analogue scale (0–100), with the endpoints “The worst health you can imagine” and “The best health you can imagine.” Satisfaction with surgery was graded on a Likert scale with 5 levels: very satisfied, satisfied, neither satisfied or dissatisfied, dissatisfied, and very dissatisfied.
We chose to analyze the number of prostheses rather than the number of patients (including bilateral cases), in line with our previous study (17), as this approach has been found to have a negligible effect on the survival estimates (18).
We defined revision as exchange or removal of 1 or more components except incidental exchange of the polyethylene insert (19). Follow-up started on the day of primary TAR and ended on the day of revision, death, or December 31, 2020, whichever came first.
Statistics
Even though the data is collected from a complete or almost complete National Quality Registry (NQR) we chose to consider the study as sample based. We thus present measures of uncertainty to facilitate generalization to probable future outcomes in Sweden and to other similar populations.
We used the Kaplan–Meier estimator to visualize the prosthesis survival probability and used 95% confidence intervals (CI) to describe uncertainty.
For estimation of risk of revision, cases that underwent surgery at least 1, 2, or 3 years before end of study were used as population at risk and revision cases within 1, 2, or 3 years as events (disregarding deaths).
As PROM scores were not normally distributed, they are presented as medians with interquartile ranges (IQR). Changes in scores were, however, approximately normally distributed (with some ceiling effects). We therefore (under the central limit theorem) used a t-test (with non-parametric bootstrapping, using simple case resampling with 10,000 iterations) to estimate mean changes with 95% confidence intervals (interval percentiles from the ordered bootstrap values).
Ethics, data sharing, funding, and potential conflicts of interest
The study protocol was approved by the Ethical Review Board of Lund University (Dnr 2009:698, 2014/448) and the study was conducted in accordance with the Helsinki Protocol.
The registration of data and the study was performed confidentially and according to Swedish and EU data protection rules. All authors had access to the anonymous database delivered by Register Centrum Syd, Region Skane Sweden. This study is based on sensitive individual-level data protected by the Swedish personal data act. Data sharing is not possible according to Swedish law.
This work was supported by grants from ALF and FoUU of Region Skåne, Greta Koch, Herman Järnhardt, Maggie Stevens, Skåne University Hospital foundations, and the Swedish Association of Local Authorities and Regions. The funders had no influence on the design of the study, the collection, analysis, or interpretation of data, on writing the manuscript, or on any other part of the study.
The authors declare no conflict of interest.
Results
Before the end of follow-up, 5 of the 233 patients died (mean 24 months [range 11–52)] after surgery) and 7 (3%) underwent revision (mean 13 months [4–28] after surgery). The mean follow-up was 26 months [1–79].
Of the 7 patients who underwent revision, 4 were due to deep infection; of these 3 were treated with removal of components and arthrodesis in a 2-stage procedure and 1 with arthrodesis in a 1-stage procedure. 2 patients with valgus malalignment after fracture close to the prosthesis both underwent ankle fusion, and 1 patient with medial pain underwent cleaning of the medial gutter and change to a higher meniscal bearing.
During the 239 TM Ankle procedures 86 concomitant procedures were performed in 85 patients. Calcaneal osteotomy was the most common (Table 2).
Postoperative major complications occurred in 7 patients. 6 of these were related to infection; 1 was treated with debridement, antibiotics, and implant retention (DAIR), and the other 5 with removal of the lateral plate. 1 patient suffered a fracture and underwent a re-osteotomy of the fibula.
10 patients underwent secondary non-revision surgery, 2 due to valgus malalignment (1 of these underwent calcaneal osteotomy, FDL transfer, and deltoid reconstruction, and the other underwent navicular–cuneiform arthrodesis and tibial osteotomy). 1 patient, due to varus malalignment, underwent osteotomy of both tibia and fibula. Due to medial pain 4 patients underwent cleaning of bony overgrowth in the medial gutter and insertion of an augmenting screw in the malleolus. The 3 remaining patients for unspecific reasons underwent talo-navicular arthrodesis (1 patient), TMT I arthrodesis (1 patient), and extraction of a medial screw (1 patient).
Preoperatively, 168/239 completed the SEFAS questionnaire, 165 (69%) the EQ-5D, and 160 (67%) completed the EQ-VAS. 149 patients were available (≥ 1.5 years’ follow-up, alive and unrevised) for the 2-year questionnaires and 107 (72%), 106 (71%), and 107 (72%) completed the respective above-mentioned questionnaire. Median scores were higher after surgery. Not all patients answered all questionnaires but for those that reported both pre- and 2-year postop scores, changes were statistically significant. 108 (72%) patients also reported their satisfaction with surgery in the 2-year questionnaires; 81% were very satisfied or satisfied with their prosthesis (Tables 3 and 4).
| Individuals answering preoperative questionnaire | Individuals answering postoperative a questionnaire | |||
| n (%) | median (IQR) b | n (%) | median (IQR) b or n (%) | |
| SEFAS | 168 (70) | 15 (10–19) | 107 (72) | 36 (26–43) |
| EQ-5D | 165 (69) | 0.68 (0.58–0.73) | 106 (71) | 0.90 (0.83–0.97) |
| EQ-VAS | 160 (67) | 60 (40–76.5) | 107 (71) | 80 (70–90) |
| Satisfaction | 108 (72) | |||
| Very satisfied | 61 (5) | |||
| Satisfied | 27 (25) | |||
| Neither satisfied nor dissatisfied | 12 (11) | |||
| Dissatisfied | 3 (3) | |||
| Very dissatisfied | 5 (5) | |||
| a ≥ 1.5 years’ follow-up, alive and unrevised, n = 149 eligible patients. b See Statistics. |
||||
| n (%) | Preoperative median (IQR) b | Postoperative a median (IQR) b | Change from pre- to postoperative mean (95% CI) b | |
| SEFAS | 79 (53) | 16 (10–20) | 35 (25–41) | 18 (15–20) |
| EQ-5D | 77 (51) | 0.68 (0.58–0.73) | 0.83 (0.83–0.96) | 0.19 (0.15–0.22) |
| EQ-VAS | 76 (51) | 65 (46–80) | 80 (70–90) | 15 (9.6–20) |
| a ≥ 1.5 years’ follow-up, alive and unrevised, n = 149 eligible patients. b See Statistics. |
||||
The estimated prosthesis survival probability was 95% (CI 89–98) after 3 years (Figure 1, Table 5). The risk for revision was 3% at 3 years (Table 6).
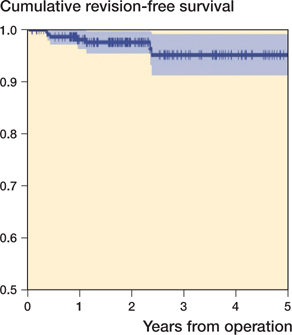
Figure 1. Estimated cumulative prosthesis survival probability for primary TM Ankle procedures in Sweden (N = 239). The purple band represents the 95% confidence interval.
| Interval (year) | Entering interval | Censored a | Exposed to risk | Terminal events | Cumulative proportion surviving at end of interval (CI) |
| 0–1 | 239 | 51 (1) | 213.5 | 4 | 0.98 (0.95–0.99) |
| 1–2 | 184 | 81 (3) | 143.5 | 1 | 0.97 (0.94–0.99) |
| 2–3 | 102 | 43 (0) | 80.5 | 2 | 0.95 (0.89–0.98) |
| 3–4 | 57 | 22 (0) | 46 | 0 | 0.95 (0.89–0.98) |
| 4–5 | 35 | 20 (1) | 25 | 0 | 0.95 (0.89–0.98) |
| For further details see Figure 2 (in Supplementary data). a Deaths or follow-up not long enough. Number of deaths in parenthesis. |
|||||
| TAR performed years before EoS | n | Revisions during follow-up year a | Revisions at EoS | |||
| 1 | 2 | 3 | > 3 | |||
| 0 to < 1 | 50 | (0) a | – | – | 0 | |
| 1 to < 2 | 81 | 1 | (1) a | – | 2 | |
| 2 to < 3 | 48 | 2 | 0 | (1) a | 3 | |
| > 3 | 60 | 1 | 0 | 1 (0) a | (0) a | 2 |
| a Revisons during incomplete follow-up years in parenthesis. EoS = end of study (December 31, 2020). Revision rate within 1 year: (1+2+1) / (81+48+60) = 2% Revision rate within 2 years: (2+1) / (48+60) = 3% Revision rate within 3 years: (1+1) / 60 = 3% Revision rate overall: 7 / 239 = 3% |
||||||
Discussion
In this study, the so far largest published consecutive series of the TM Ankle, we found a 3-year prosthesis survival probability of 95% and a 3-year risk of revision of 3%. After 2 years the satisfaction rate and the clinical score (SEFAS) were high.
Trabecular metal components have properties that seem to facilitate bony ingrowth and stable biological fixation (7,8,10,11). We found no aseptic loosening of components, and few have been reported in the literature. Mosca et al. (15) reported 1 aseptic loosening among 73 cases. This case had, however, already been revised 21 days postoperatively due to malrotation of the tibial component and may thus rather be a technical error than a true aseptic loosening. Barg et al. (12) reported 3 cases of loosening (the tibial component) out of 55 cases. Long-term studies of the Trabecular Metal Tibia in total knee replacement have not shown aseptic loosening (10,11,20).
The complexity of total ankle replacement is well known and is reflected in the high rate of concomitant procedures in this study (86 concomitant procedures during 239 primary TARs). To attain good balancing of the foot and ankle complex during TAR surgery a range of simultaneous procedures may be necessary. DeVries et al. (21) had 7 concomitant procedures in their short-term study, i.e., in nearly half of their patients. Barg et al. (12) reported 58 concomitant procedures in their 55 cases and Bianchi et al. (22) 14 in their study of 30 cases.
Problems related to the lateral plate in TM Ankles are not uncommon. Plate removal was undertaken in 5 patients with superficial infections in this study, all of which healed. The most reported complications with the lateral plate are either superficial infection or discomfort and tenderness from the hardware. Tiusanen et al. (14) reported problems with the lateral hardware in 12% of cases and Gagné et al. (23) in 23%. The rate of superficial infections decreased when these authors changed lateral fixation to screws and rods respectively. On the other hand, Usuelli et al. (24) found similar infection rate in 81 TARs through an anterior approach and 69 TARs through a transfibular approach. DeVries et al. (21), in a series of 16 patients, reported 3 cases of non-union after plate fixation of the fibula, and Bianchi et al. (22) had 1 such case in 30 patients. No non-union of the fibular osteotomy was reported to the Swedish Ankle Registry.
On a 5-category scale, 81% of the patients indicated that they were satisfied or very satisfied with the surgical results. Other reports of the TM Ankle have found nine-tenths very satisfied or satisfied patients using a 3-category rating (22) and two-thirds very satisfied patients with a 4-category rating (14). With mobile bearing TARs, Jung et al. (25), in their small short-term study and with a 4-grade score, had nine-tenths very satisfied or satisfied patients with the Hintegra and Mobility prostheses, respectively.
We found a high satisfaction rate and a statistically significant and clinically relevant mean improvement in EQ-5D as well as in the foot- and ankle-specific SEFAS after surgery. The mean increment in SEFAS (max. 48) of 18 points for those who answered both questionnaires was also clinically significant, well beyond the minimal important change (MIC) of 5 points (26). Our results are thus in line with Bianchi et al. (22), who found statistically significant improvements postoperatively using the FFI, the AOFAS, and the VAS pain scores. Mosca et al. (15) used the AOFAS, SF-36, and VAS scale and all improved statistically significantly. In the study by Usuelli et al. (13), the AOFAS, VAS, and Short Form-12 also improved statistically significantly as did the VAS, and the physical and pain domains of the PROMIS scores in the study by Barg et al. (12). Clifton et al. (27) analyzed 55 procedures with Hintegra designs after 7 years and found an AOS score of 35, MOX-FQ score of 36, and EQ-5D score of 0.69, the latter in line with our result of 0.80.
The estimated prosthesis survival probability in this study was 95% after 3 years, which corroborates other mid-term reports of other TAR designs. Sproule et al. (28) found a 90% prosthesis survival probability after 3 years with the Mobility design, and with the same prosthesis Kerkhoff et al. (29) and Lefrancois et al. (30) found 95% and 89% prosthesis survival probabilities respectively. Using the Salto mobile bearing design, Faber et al. (31) and Wan et al. (32) report prosthesis survival probabilities of 94% and 95% respectively. With the TM Ankle, Barg et al. (12) found a prosthesis survival probability after 2 years of 93%, in line with our 2-year results of 97% (CI 0.94–0.99) (Table 5).
2 other fixed-bearing designs have been introduced quite recently, the Cadence and the Infinity. For Cadence, short- to mid-term results are promising but studies are few and small (33,34). For Infinity, promising results have been shown in one mid-term study (35); potential problems around the tibial component have, however, been observed (36,37).
There are some limitations to this study. The proportion of patients completing both measurements could have been higher than the approximately 50% achieved. Even though dropout analyses revealed similar PROMS in those who answered only the baseline or only the 2-year follow-up compared with those who answered both (data not shown) we cannot rule out selection bias. More patient-specific information would also benefit the study, but, due to the registerbased nature, detailed patient-level data was not available. As in all registry studies, there is always uncertainty regarding the completeness and validity of data. The current procedurebased coverage and completeness are, however, both estimated as close to 100% in the register. The registry regularly compares data with the Swedish National Patient Registry and the validity of variables is, due to automatic input controls at registration, high. The strength of the study is that it is the so far largest series published and that it represents non-designer results in a real-world complete national cohort of patients.
In conclusion, this study of TM Ankle outcomes in Sweden found a high prosthesis survival probability (95%) after 3 years without any aseptic loosening, and a high patient satisfaction rate. The results justify further use of this prosthesis but also indicate that studies with head-to-head comparisons with other designs are necessary.
- Jeyaseelan L, Si-Hyeong Park S, Al-Rumaih H, Vejlkovic A, Penner M J, Younger A. Outcomes following total ankle arthroplasty: a review of the registry data and current literature. Orthop Clin N Am 2019; 50: 539-48. doi: 10.1016/j.ocl.2019.06.004.
- Undén A, Jehpsson L, Kamrad I, Carlsson Å, Henricson A, Karlsson M K, et al. Better implant survival with modern ankle prosthetic designs: 1,226 total ankle prostheses followed for up to 20 years in the Swedish Ankle Registry. Acta Orthop 2020; 91(2): 191-6. doi: 10.1080/17453674.2019.1709312.
- Labek G, Thaler M, Janda W, Agreiter M, Stöckl B. Revision rates after total joint replacement: cumulative results from worldwide joint register datasets. J Bone Joint Surg (Br) 2011; 93(3): 293-7. doi: 10.1302/0301-620X.93B3.25467.
- Sadoghi P, Liebensteiner M, Agreiter M, Leithner A, Böhler N, Labek G. Revision surgery after total ankle arthroplasty: a complication-based analysis using worldwide arthroplasty registers. J Arthroplasty 2013; 28: 1329-32. doi: 10.1016/j.arth.2013.01.012.
- Labek G, Todorov S, Iovanescu L, Stoica C I, Böhler N. Outcome after total ankle arthroplasty: results and findings from worldwide arthroplasty registers. Int Orthop 2013; 37(9): 1677-82. doi: 10.1077/s00264-013-1981-7.
- Bobyn J D, Stackpool G J, Hacking S A, Tanzer M, Krygier J J. Characteristics of bone ingrowth and interface mechanics of a new porous tantalum material. J Bone Joint Surg (Br) 1999; 81B: 907-14. doi: 10.1302/0301-620x.81b5.9283.
- D’Angelo F, Murena I, Compagnolo M, Zatti G, Cherobino P. Analysis of bone ingrowth on a tantalum cup. Indian J Orthop 2008; 42: 275-8. doi: 10.4103/0019-5413.39553.
- Sambaziotis C, Lovy A J, Koller K E, Bloebaum R D, Hirsh D M, Kim S J. Histological retrieval analysis of a porous tantalum metal implant in an infected total knee arthroplasty. J Arthroplasty 2012; 27(7): 1413e5-1413e9. doi: 10.1016/j.arth.2011.10.025.
- Epperson R T, Barg A, Williams D L, Salzman C L. Histological analysis of a retrieved porous tantalum total ankle replacement. J Bone Joint Surg (Am) Case Connector 2020; 10(1): 1-6. doi: 10.2106/JBJS.CC.19.00379.
- Henricson A, Nilsson K G. Trabecular metal tibial knee component still stable at 10 years: an RSA study of 33 patients less than 60 years of age. Acta Orthop 2016; 87(5): 504-10. doi: 10.1080/17453674.2016.1205169.
- Wojtowicz R, Henricson A, Nilsson K G, Crnalic S. Uncemented monoblock trabecular metal posterior stabilized high-flex total knee arthroplasty: similar pattern of migration to the cruciate-retaining design—a prospective radiostereometric analysis (RSA) and clinical evaluation of 40 patients (49 knees) 60 years or younger with 9 years follow-up. Acta Orthop 2019; 90(5): 460-6. doi: 10.1080/17453674.2019.1627638.
- Barg A, Bettin C C, Burstein A H, Saltzman C L, Gilliland J. Early clinical and radiographic outcomes of trabecular metal total ankle replacement using transfibular approach. J Bone Joint Surg Am 2018; 100:505-15. doi: 10.2106/JBJS.17.00018.
- Usuelli F G, Maccario C, Granata F, Indino C, Vakhshori V, Tan E W. Clinical and radiological outcomes of transfibular total ankle arthroplasty. Foot Ankle Int 2019; 40(1): 24-33. doi: 10.1177/10711100718798851.
- Tiusanen H, Kormi S, Kohonen I, Saltychev M. Results of trabecularmetal total ankle arthroplasties with transfibular approach. Foot Ankle Int 2020; 41(4): 411-19. doi: 10.1177/1071100719894929.
- Mosca M, Caravelli S, Vocale E, Maitan N, Grassi A Q, Massimi S, et al. Clinical–radiological outcomes and complications after total ankle replacement through a lateral transfibular approach: a retrospective evaluation at a mid-term follow-up. Int Orthop 2021; 45: 437-43. doi: 10.1007/s00264-020-04709-4.
- Cöster M, Karlsson M K, Nilsson J-Å, Carlsson Å. Validity, reliability, and responsiveness of a self-reported foot and ankle score (SEFAS). Acta Orthop 2012; 83(2): 197-203. doi: 10.3109/17453674.2012.657579.
- Henricson A, Nilsson J-Å, Carlsson Å. 10-year survival of total ankle arthroplasty: a report on 780 cases from the Swedish Ankle Register. Acta Orthop 2011; 82(6): 655-9. doi: 10.3109/17453674.2011.636678.
- Ranstam J, Robertsson O. Statistical analysis of arthroplasty register data. Acta Orthop 2010; 81: 10-14. doi: 10.3109/17453671003587168.
- Henricson A, Carlsson Å, Rydholm U. What is a revision of total ankle replacement? Foot Ankle Surg 2011; 17: 99-102. doi: 10.1016/j.fas.2010.02.007.
- Niemeläinen M Skyttä E, Remes V, Mäkelä K, Eskelinen A. Total knee arthroplasty with an uncemented trabecular metal component. J Arthroplasty 2014; 29: 57-60. doi: 10.1016/j.arth.2013.04.014.
- DeVries J G, Derksen T A, Scharer B M, Limoni R. Perioperative complications and initial alignment of lateral approach total ankle arthroplasty. J Foot Ankle Surg 2017; 56: 996-1000. doi: 10.1053/j.fas.2017.04.016.
- Bianchi A, Martinelli N, Hosseinzadeh M, Flore J, Minoli C, Malerba F, et al. Early clinical and radiological evaluation in patients with total ankle replacement performed by lateral approach and peroneal osteotomy. BMC Musculoskelet Disord 2019; 20: 132-9. doi: 10.1186/s12891-019-2503-6.
- Gagné O J, Penner M, Wing K, Vejlkovic A, Younger A S. Reoperation profile of lateral vs anterior approach ankle arthroplasty. Foot Ankle Int 2020; 41(7): 834-8. doi: 10.1177/1071100720920276.
- Usuelli F G, Indino C, Maccario C, Manzi L, Liuni F M, Vulcano E. Infections in primary ankle replacement: anterior approach versus lateral transfibular approach. Foot Ankle Surg 2019; 25: 19-23. doi: 10.1016/j.fas.2017.07.643.
- Jung H-G, Shin M-H, Lee S-H, Eom J-S, Lee D-O. Comparison of the outcomes between two 3-component total ankle implants. Foot Ankle Int 2015; 36(6): 656-63. doi: 10.1177/107100715573716.
- Cöster M, Nilsdotter A, Brundin L, Bremander A. Minimally important change, measurement error, and responsiveness for the Self-Reported Foot and Ankle Score. Acta Orthop 2017; 88(3): 300-4. doi: 10.1080/17453674.2017.1293445.
- Clifton L J, Kingman A, Rushton P R P, Murty A, Kakwani R, Coorsh J, et al. The Hintegra total ankle replacement: survivorship, failure modes and patient reported outcomes in seventy cases with a minimum five years follow-up. Int Orthop 2021; 45: 2331-6. doi: 10.1007/s00264-021-05071-9.
- Sproule J A, Chin T, Amin A, Daniels T, Younger A S, Boyd G, et al. Clinical and radiographic outcomes of the Mobility total ankle arthroplasty system: early results from a prospective multicenter study. Foot Ankle Int 2013; 34(4): 491-7. doi: 10.1177/107100713477610.
- Kerkhoff Y R A, Kosse N M, Louwerens J W K. Short term results of the Mobility total ankle system: clinical and radiographic outcome. Foot Ankle Surg 2016; 22(3): 152-7. doi: 10.1016/j.fas.2015.06.004.
- Lefrancois T, Younger A, Wing K, Penner M J, Dryden P, Wong H, et al. A prospective study of four total ankle arthroplasty implants by non-designer investigators. J Bone Joint Surg Am 2017; 99(4): 342-8. doi: 10.2106/JBJS.16.00097.
- Faber W M, Mastboom M J L, van Vliet-Koppert S T, Bouman I C E, van Kamper P M. Outcome of 52 Salto ankle protheses implanted by a single surgeon. Adv Orthop 2018; 2735634. doi: 10.1155/2018/2735634.
- Wan D D, Choi W J, Shim D W, Hwang Y, Park Y J, Lee J W. Short-term clinical and radiographic results of the Salto mobile total ankle prosthesis. Foot Ankle Int 2018; 39(2): 155-65. doi: 10.1177/1071100717737988.
- Fram B, Corr D O, Rogero R G, Pedowitz D I, Tsai J. Short-term complications and outcomes of the Cadence total ankle arthroplasty. Foot Ankle Int 2022; 43(3): 371-7. doi: 10.1177/10711007211043853.
- Kooner S, Kayum S, Pinsker E B, Khalifa A A, Khan R M, Halai M, et al. Two-year outcomes after total ankle replacement with a novel fixed-bearing implant. Foot Ankle Int 2021; 42(8): 1002-10. doi: 10.1077/10711007211005781.
- Penner M, Davis W H, Wing K, Bemenderfer T, Waly F, Anderson R B. The Infinity total ankle system: early clinical results with 2- to 4-year follow-up. Foot Ankle Spec 2019; 12(2): 158-66. doi: 10.1177/1938640018777601.
- Saito G H, Sanders A E, Netto C C, O’Malley M J, Ellis S J, Demetracopoulos C A. Short-term complications, reoperations, and radiographic outcomes of a new fixed-bearing total ankle arthroplasty. Foot Ankle Int 2018; 39(7): 787-94. doi: 10.1177/1071100718764107.
- Cody E A, Taylor M A, Nunley II J A, Parekh S G, DeOrio J K. Increased early revision rate with the INFINITY total ankle prosthesis. Foot Ankle Int 2019; 40(1): 9-17. doi: 10.1177/107110078794933.
Supplementary data
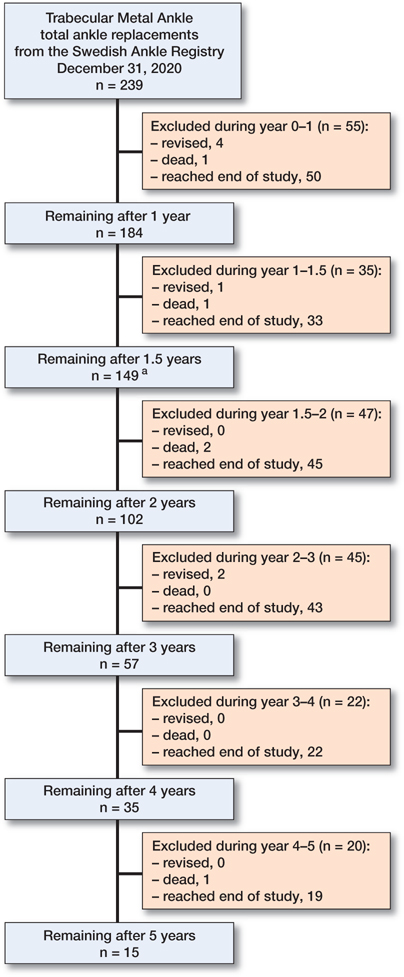
Figure 2. Flowchart of TM Ankle procedures in Sweden with revisions and death. a Available (≥ 1.5 years’ follow-up, alive and unrevised) for the 2-year questionnaires.