Lower mortality in distal femoral fractures in the presence of a knee arthroplasty: an observational study on 2,725 fractures from the Swedish Fracture Register
Björn HERNEFALK 1, Anders BRÜGGEMANN 1, Jabbar MOHAMMED 2, Sebastian MUKKA 2, and Olof WOLF 1
1 Department of Surgical Sciences, Orthopaedics, Uppsala University, Uppsala; 2 Department of Surgical and Perioperative Sciences at Umeå University, Umeå, Sweden
Background and purpose — Distal femoral fractures (DFF) in older patients have mortality rates comparable to fractures of the proximal femur. An ageing population combined with an increasing number of patients undergoing total knee arthroplasty (TKA) will make periprosthetic distal femoral fractures (pDFF) more common. We investigated whether a pre-existing TKA influences mortality rates.
Patients and methods — All patients ≥ 60 years registered in the Swedish Fracture Register with a DFF sustained between March 20, 2011 and December 31, 2020 were included. The study cohort comprised 2,725 patients, of which 650 had a pDFF. Unadjusted 90-day and 1-year mortality was estimated via Kaplan–Meier survival curves. A Cox regression model adjusted for age, sex, and treatment modality was used to investigate the association between DFF or pDFF and mortality.
Results — Mean age was 80 years and 82% were females. The most common injury mechanism was a simple fall (75%). The pDFF and DFF group were similar with regards to age, sex, and trauma mechanism. Unadjusted 90-day and 1-year mortality was 11% (95% CI 10–12) and 21% (CI 19–23), respectively. Kaplan–Meier survival analysis demonstrated a slightly lower mortality for pDFFs, especially in patients ≤ 70 years. The Cox regression model showed a lower hazard ratio (HR) for mortality in the pDFF group (HR 0.82, CI 0.71–0.94).
Interpretation — In a large cohort of patients ≥ 60 years with a distal femoral fracture, mortality rates at 90 days and 1 year post-injury were 11% and 21%, respectively. Periprosthetic fractures were associated with a lower mortality.
Citation: Acta Orthopaedica 2022; 93: 684–688. DOI http://dx.doi.org/10.2340/17453674.2022.4376.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-03-13. Accepted: 2022-06-28. Published: 2022-07-22.
Correspondence: bjorn.hernefalk@surgsci.uu.se
BH, JM, SM, AB, and OW planned the study. BH wrote the initial draft. AB performed the analyses. All authors contributed to the interpretation of the data and revision of the manuscript.
Acta thanks Esa Jämsen for help with peer review of this study.
In older patients, fractures of the distal femur share many of the characteristics and challenges in management with those of hip fractures. They are both typically fragility fractures resulting from low-energy trauma in patients with several comorbidities and comparable mortality rates (1-3). However, distal femoral fractures (DFF) have been studied to a far lesser extent than their proximal counterparts.
The incidence for DFFs has been reported to be 8.7 per 100,000 per year, with a rapid increase in patients above 60 years, and a majority (> 80%) of fractures occur in elderly women (2,4).
As the number of patients receiving a total knee arthroplasty (TKA) increases, combined with an ageing, frailer population, periprosthetic distal femoral fractures (pDFF) will become more common in years to come. The prevalence of pDFF after TKA has been reported to be 0.2–1.8% (5). These fractures mandate evaluation of remaining bone stock, implant integrity, and fixation, all factors that could limit surgical options (5,6).
In the current literature on pDFFs, which is sparse and based on limited cohorts, there are reports of mortality rates between 13% and 17% at 1 year post-treatment (7,8). A tendency towards a less favorable outcome in patients with periprosthetic fractures compared with patients with fractures of the native femur has been described (8). Risk factors include female sex, age above 70 years, and revision arthroplasty (9).
We compared, based on data from the Swedish Fracture Register (SFR), mortality after DFF in patients with and without pre-existing total knee arthroplasty and describe the demography, fracture characteristics, and treatment given.
Patients and methods
Study design and variables
This is an observational cohort study based on data obtained from the SFR (10). The register started in Gothenburg, Sweden in 2011. It was introduced stepwise in Sweden and by January 2021 all 54 orthopedic departments in Sweden participated (11). Orthopedic surgeons register data prospectively on basic patient characteristics, data on injury mechanism, fracture classification, and treatment. Fractures are classified according to the AO/OTA classification system (12). Since December 2015, classification of periprosthetic fractures is done according to the Unified Classification System (UCS) (13).
Completeness of femoral fracture registration in 2020 in the SFR was 81% when compared with the National Patient Register (NPR). However, as the NPR has demonstrated a tendency to overestimate the number of acute fractures (14), the true completeness of the SFR is likely higher. Data on mortality, the primary endpoint of this study, is obtained by real-time linkage to the Swedish Tax Agency.
Patient selection
Data was retrieved on all patients ≥ 60 years registered with a distal femoral fracture (ICD S72.0–S72.4) with an injury date between March 20, 2011 and December 31, 2020. Patients with missing data, i.e., incomplete information regarding treatment modality or with a treatment date of more than 30 days after the registered injury date (n = 205), were interpreted as invalid registrations and excluded.
Outcome measures
Unadjusted 90-day and 1-year mortality was determined for patients with DFF and pDFF. Associations between mortality and absence or presence of a TKA (DFF or pDFF), patient age, sex, and type of treatment were also examined. Patient age was treated as a categorical variable and stratified into 4 groups: ≤ 70 years, 71–80 years, 81–90 years, and > 90 years.
Statistics
Baseline variables are presented as means (SDs) and proportions. Differences between observed counts were analyzed using the chi-square test. Follow-up mortality data was retrieved for 1 year for all patients. Unadjusted cumulative mortality and 95% confidence intervals (CI) were estimated using the Kaplan–Meier method. The association between mortality and investigated group (DFF or pDFF), age, sex, and treatment modality were examined via a Cox regression model. Bilateral observations were excluded in this model. To ensure that the underlying assumptions of Cox regression were met, Schönfeld residuals were calculated and plotted. Statistical analyses were performed using the R software package (R Development Core Team 2021; R Foundation for Statistical Computing, Vienna, Austria).
Ethics, funding, data sharing, and potential conflicts of interest
The study was conducted following the ethical principles of the Helsinki Declaration and was approved by the Regional Ethical Committee in Uppsala (Dnr 2015/510 and 2021/02560). In accordance with Swedish law, individual consent was not required.
Any person interested in the data set may contact Uppsala University and the corresponding author to find ways to share data according to Swedish law and regulations. It is also possible for individuals interested in this data to apply directly to the Center of Registers, Västra Götaland (URL: http://registercentrum.se/), a process that involves approval from the Swedish Ethical Review Authority.
The authors declare no competing interests in relation to this study.
Results
The final study cohort comprised 2,725 patients, of whom 2,075 had a DFF and 650 a pDFF. Mean age was 80 (SD 10) years and 1,840 patients (82%) were female. The most common trauma mechanism was a simple fall (75%). Trauma energy was considered low in 84% of cases. No statistically significant differences were observed between the DFF and pDFF groups with respect to these variables. For both DFFs and pDFFs, osteosynthesis using either plates or intramedullary nails was the most common treatment modality (72% and 77% respectively). Nonoperative management was undertaken in 26% of DFFs and 17% of pDFFs (Table 1).
The most common fractures in the DFF group were extraarticular AO/OTA type A (n = 1,226, 61%). The majority of pDFFs where simple fractures around well-fixed implants (Table 2).
Mortality
At 1-year post-injury, the unadjusted mortality was 21% (CI 19–23) for the entire cohort. Mortality was slightly lower in the pDFF group (19%, CI 16–22) than in the DFF group (22%, CI 20–24).
The unadjusted 90-day mortality was 11% (CI 10–12) for the entire cohort, and comparable estimates were found for the DFF group (11%, CI 10–13) and pDFF group (10%, CI 8–12) respectively (Figure 1).
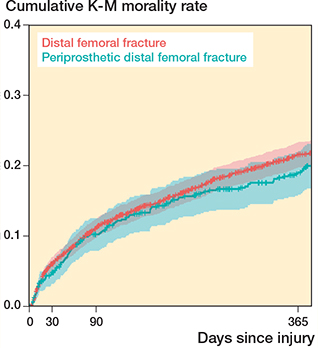
Figure 1. Unadjusted mortality following distal femoral fracture. Kaplan–-Meier survival analysis.
To further examine the influence of patient age, a Kaplan–Meier analysis stratified by age groups was performed. This demonstrated that mortality was lower for the pDFF group in patients ≤ 70 years of age (Figure 2).
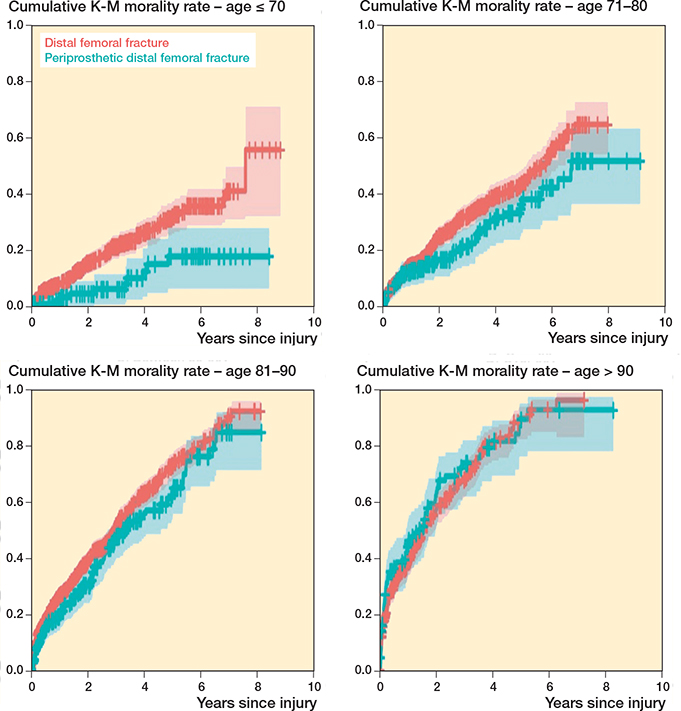
Figure 2. Kaplan–Meier survival analysis for the DFF and pDFF groups stratified by age.
The Cox regression model, adjusted for sex, age group, and treatment modality, showed a lower hazard ratio (HR) for mortality in the pDFF group (HR 0.82, CI 0.71–0.94).
Discussion
In our cohort of 2,725 patients, the unadjusted 90-day and 1-year mortality after a DFF was 11% and 21% respectively, emphasizing the seriousness of these injuries.
Using Kaplan–Meier survival analysis, a tendency toward a more favorable outcome for pDFFs was observed (Figure 1) and the Cox regression model showed a lower HR for mortality in the pDFF group. This association seems to be more pronounced in patients ≤ 70 years of age (Figure 2).
The 1-year mortality for the pDFF group of 19% is similar, with previous reports that have described rates between 13% and 35% (7,8,15-18). The surgical management of periprosthetic fractures is often more complex (19), but this did not translate into higher mortality rates in our study, contradicting earlier findings by Streubel et al. (8). However, they included only surgically treated patients, in contrast to our study where all fractures regardless of treatment modality were included, which makes comparisons difficult. We do acknowledge a potential for selection bias in our study, as patients with a pDFF at least at some point have been evaluated for—and passed the requirements for—elective TKA surgery. Patients with a non-periprosthetic DFF have either not been subject to such an evaluation or have failed it. Our finding of lower mortality in pDFF patients below 70 years of age could simply reflect that they represent a healthier sector of their age group. This is also illustrated by the discrepancy in mortality in patients ≥ 60 years with pDFF (15%) compared with DFF (35%) at 1-year post-injury reported in a Danish study of 304 DFFs (18).
Our patients with DFFs and pDFFs were similar with respect to age, sex, injury mechanism, and treatment modality, but data regarding comorbidities would provide more insight on the case-mix of the 2 groups and allow better interpretation of results. Patients with DFFs have been reported to have a lower proportion of high comorbidity than patients with diaphyseal or proximal femoral fractures, although this did not affect mortality up to 1 year post-fracture (4). Boylan et al. and Haughom et al. have demonstrated similar 30-day mortality for native joint hip fractures and periprosthetic fractures of the hip (20,21). The study by Boylan et al., which included 1,655 periprosthetic fractures and 97,231 native hip fractures, found that periprosthetic fractures were associated with a lower risk of mortality at 6 months and 1 year post-injury. These findings are similar to our study of the distal femur, where the pDFF group demonstrated lower mortality.
The vast majority of our patients were female (82%) and a low-energy, simple fall was by far the most common injury mechanism (75%), reinforcing the findings of previous studies (2,4).
There are several limitations to our study. First, as with all register-based studies, completeness, coverage, miscoding, transfer errors, and underreporting is of importance for external validity (22). The stepwise introduction of the national SFR has led to a gradual increase in both completeness and coverage as described above. Missing data regarding treatment and treatment dates registered long after the injury date led to exclusions of patients. The SFR has not undergone validation with respect to distal femoral fractures specifically. However, the classification of femoral fractures overall in the register has been proved to be satisfactory (23). The completeness and accuracy of the register has been successfully tested in the setting of humeral fractures (14).
Second, as previously stated, the potential influence of selection bias must be taken into account. As the SFR in its current form does not register information on confounders for mortality, such as ASA classification, comorbidity scores, e.g., Charlson comorbidity index, dementia, patient dependence on walking aids, and living situation, we were unable to adjust our statistical analysis for these variables. However, a recent study on femoral neck fractures found limited predictive power of Elixhauser and Charlson comorbidity indices for mortality and a model with age and sex was superior to both these indices (24).
Third, residual confounding may affect the results of the regression analysis undertaken. Lastly, the UCS was introduced during the study period, which led to different classification systems for the pDFF group.
The strengths of this study are the large cohort of patients with DFFs combined with full control of the primary outcome mortality through linkage with the Swedish Tax Agency. Owing to the Swedish Personal Identification Number unique to all Swedish citizens, there is no loss to follow-up. The patients included have fractures classified by orthopedic surgeons and classification in the SFR has been proven to be valid as previously mentioned.
In the present study, we chose to focus on mortality. With an ever-increasing number of fractures being included in the register, there will be possibilities for future studies to examine the functional outcome, rates of secondary surgery, and complications following treatment of these injuries.
In conclusion, in a Swedish cohort of 2,725 patients ≥ 60 years old, the 90-day mortality rate after distal femoral fracture was 11%, rising to 21% at 1 year post-injury. The presence of a TKA was associated with lower mortality. DFFs typically occur in female patients as a result of a low-energy simple fall.
- Della Rocca G J, Uppal H S, Copeland M E, Crist B D, Volgas D A. Geriatric patients with fractures below the hip are medically similar to geriatric patients with hip fracture. Geriatr Orthop Surg Rehabil 2015; 6(1): 28-32.
- Elsoe R, Ceccotti A A, Larsen P. Population-based epidemiology and incidence of distal femur fractures. Int Orthop 2018; 42(1): 191-6.
- Jennison T, Divekar M. Geriatric distal femoral fractures: a retrospective study of 30 day mortality. Injury 2019; 50(2): 444-7.
- Wolf O, Mukka S, Ekelund J, Möller M, Hailer N P. How deadly is a fracture distal to the hip in the elderly? An observational cohort study of 11,799 femoral fractures in the Swedish Fracture Register. Acta Orthop 2021; 92(1): 40-6.
- Lombardo D J, Siljander M P, Sobh A, Moore D D, Karadsheh M S. Periprosthetic fractures about total knee arthroplasty. Musculoskelet Surg 2020; 104(2): 135-43.
- Quinzi D A, Childs S, Lipof J S, Soin S P, Ricciardi B F. The treatment of periprosthetic distal femoral fractures after total knee replacement: a critical analysis review. J Bone Joint Surg Rev 2020; 8(9): e20.00003.
- Hoellwarth J S, Fourman M S, Crossett L, Goodman M, Siska P, Moloney G B, et al. Equivalent mortality and complication rates following periprosthetic distal femur fractures managed with either lateral locked plating or a distal femoral replacement. Injury 2018; 49(2): 392-7.
- Streubel P N, Ricci W M, Wong A, Gardner M J. Mortality after distal femur fractures in elderly patients. Clin Orthop 2011; 469(4): 1188-96.
- Meek R M D, Norwood T, Smith R, Brenkel I J, Howie C R. The risk of peri-prosthetic fracture after primary and revision total hip and knee replacement. J Bone Joint Surg Br 2011; 93(1): 96-101.
- Wennergren D, Möller M. Implementation of the Swedish Fracture Register. Unfallchirurg 2018; 121(12): 949-55.
- Möller M, Wolf O, Bergdahl C, Mukka S, Rydberg E M, Hailer N P, et al. The Swedish Fracture Register: ten years of experience and 600,000 fractures collected in a National Quality Register. BMC Musculoskelet Disord 2022; 23(1): 141.
- Meinberg E G, Agel J, Roberts C S, Karam M D, Kellam J F. Fracture and Dislocation Classification Compendium—2018. J Orthop Trauma 2018; 32(Suppl. 1): S1-170.
- Duncan C P, Haddad F S. The Unified Classification System (UCS): improving our understanding of periprosthetic fractures. Bone Joint J 2014; 96-B(6): 713-16.
- Bergdahl C, Nilsson F, Wennergren D, Ekholm C, Möller M. Completeness in the Swedish Fracture Register and the Swedish National Patient Register: an assessment of humeral fracture registrations. Clin Epidemiol 2021; 13: 325-33.
- Shields E, Behrend C, Bair J, Cram P, Kates S. Mortality and financial burden of periprosthetic fractures of the femur. Geriatr Orthop Surg Rehabil 2014; 5(4): 147-53.
- Müller F, Buchner M, Doblinger M, Füchtmeier B. [Distal femoral fractures in geriatric patients: does time to surgery affect revision and mortality?]. Unfallchirurg 2021; 124(7): 568-73.
- Jennison T, Yarlagadda R. A case series of mortality and morbidity in distal femoral periprosthetic fractures. J Orthop 2020; 18: 244-7.
- Larsen P, Ceccotti A A, Elsoe R. High mortality following distal femur fractures: a cohort study including three hundred and two distal femur fractures. Int Orthop 2020; 44(1): 173-7.
- Ricci W M. Periprosthetic femur fractures. J Orthop Trauma 2015; 29(3): 130-7.
- Boylan M R, Riesgo A M, Paulino C B, Slover J D, Zuckerman J D, Egol K A. Mortality following periprosthetic proximal femoral fractures versus native hip fractures. J Bone Joint Surg Am 2018; 100(7): 578-85.
- Haughom B D, Basques B A, Hellman M D, Brown N M, Della Valle C J, Levine B R. Do mortality and complication rates differ between periprosthetic and native hip fractures? J Arthroplasty 2018; 33(6): 1914-18.
- Hailer N P. Orthopedic registry research: limitations and future perspectives. Acta Orthop 2015; 86(1): 1-2.
- Knutsson S B, Wennergren D, Bojan A, Ekelund J, Möller M. Femoral fracture classification in the Swedish Fracture Register: a validity study. BMC Musculoskelet Disord 2019; 20(1): 197.
- Bülow E, Cnudde P, Rogmark C, Rolfson O, Nemes S. Low predictive power of comorbidity indices identified for mortality after acute arthroplasty surgery undertaken for femoral neck fracture. Bone Joint J 2019; 101-B(1): 104-12.