The relationship between hip displacement, scoliosis, and pelvic obliquity in 106 nonambulatory children with cerebral palsy: a longitudinal retrospective population-based study
Terje TERJESEN 1, Svend VINJE 2, and Thomas KIBSGÅRD 2
1 Section of Children’s Orthopedics and Reconstructive Surgery, Oslo University Hospital, Oslo; 2 Section of Spinal Surgery, Division of Orthopaedic Surgery, Oslo University Hospital, Rikshospitalet and Institute of Clinical Medicine, University of Oslo, Oslo, Norway
Background and purpose — The relationship between hip displacement (HD), pelvic obliquity (PO), and scoliosis in nonambulatory children with cerebral palsy (CP) has not been clearly elucidated. The aims of this population-based study were to examine the prevalence and temporal sequence of these deformities in nonambulatory children with CP and to evaluate how probable it is that severe unilateral HD contributes to development of scoliosis.
Patients and methods — This longitudinal study comprised 106 nonambulatory children, enrolled in a surveillance program. Pelvic radiographs for measurements of migration percentage (MP) and PO were taken once a year from the diagnosis of HD. Spine radiographs were taken in patients with clinically detected scoliosis. Radiographic follow-up continued until skeletal maturity.
Results — Clinically significant scoliosis (Cobb angle ≥ 40°) occurred in 60 patients at a mean age of 11.8 years. 65 patients developed clinically significant HD (MP ≥ 40%) at a mean age of 4.8 years. 24 patients had no significant hip or spine deformities, 22 had HD only, 17 had scoliosis only, and 43 had both deformities. HD was diagnosed before scoliosis in all except 1 of the patients with both deformities. 14 of 19 patients with severe unilateral HD (MP ≥ 60%) had scoliosis convexity to the opposite side of the displaced hip.
Conclusion — The combination of scoliosis and HD was frequent, and HD was diagnosed first in almost all the patients. HD might be a contributory cause of scoliosis in patients with severe, unilateral HD, PO, and later scoliosis with convexity to the opposite side.
Citation: Acta Orthopaedica 2024; 95: 55–60. DOI https://doi.org/10.2340/17453674.2024.39915.
Copyright: © 2024 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2023-09-23. Accepted: 2023-12-29. Published: 2024-01-30.
Correspondence: terje.terjesen@rikshospitalet.no
All the authors planned and designed the study. TT analyzed the data and wrote the initial manuscript. TT, SV, and TK revised the manuscript.
The authors thank NorCP (Norwegian Quality and Surveillance Registry for Cerebral Palsy) for access to patient data used in this study. The authors would also like to thank the photographer Øystein Horgmo for help with the illustrations and the statistician Are Hugo Pripp for help with the statistics.
Handling co-editor: Ilkka Helenius
Acta thanks Matti Ahonen, Julia F Funk, and Unni Narayanan for help with peer review of this manuscript.
Hip displacement (HD) and scoliosis are common in nonambulatory children and adolescents with cerebral palsy (CP) [1-4]. These deformities can occur as isolated or in conjunction and can be combined with pelvic obliquity (PO). Severe degrees of deformities can cause clinical problems like sitting difficulties, decubitus ulcers, gastrointestinal problems, and pain [5-7].
Although scoliosis, HD, and PO often coexist, the relationship between them has not been clearly explored [8-10]. In nonambulatory children with unilateral hip dislocation, Letts et al. [11] found that the most common temporal pattern was hip dislocation first, followed by PO, and finally scoliosis. Others reported that scoliosis PO, and HD tended to begin at the same time [8].
Regarding the association between unilateral HD, the high side of PO, and convex side of scoliosis, previous literature has shown divergent results, indicating that further studies with sufficient follow-up time are required [8,9,11-13]. Such studies should be population-based to avoid the possible coincidences that could occur in hospital-based cohorts. During the last decades, surveillance programs for children with CP have become a useful source of information and research [4,14,15].
The aims of this longitudinal, population-based study were to examine the prevalence of scoliosis, HD, and PO in non-ambulatory children with CP, look at the temporal sequence of the deformities, and to study whether severe unilateral HD can be a contributory factor in the development of scoliosis.
Patients and methods
Study design
This is a longitudinal, retrospective study based on the Norwegian surveillance program for children with CP (NorCP). Inclusion criteria were nonambulatory children with bilateral CP, born during the period 2002–2006 and living in 1 of the 10 counties of southeast Norway. Data on diagnosis and classification of CP according to international consensus [16] and on ambulation according to the Gross Motor Function Classification System (GMFCS) [17] was retrieved from the NorCP register. GMFCS distribution was level IV in 33 children and level V in 73.
The study was reported according to the STrengthening the Reporting of OBservational studies in Epidemiology guidelines (STROBE).
Surveillance program
The hip surveillance program includes a pelvic radiograph at the time of diagnosis of CP and then radiographs once a year in children at GMFCS levels IV and V. An anteroposterior (AP) radiograph of the pelvis and hips was taken with the child in the supine position, taking care to avoid rotation of the legs and pelvis and to keep the legs parallel (Figure 1A). The femoral head displacement was measured as the migration percentage (MP) according to Reimers [18]. MP is the percentage of the femoral head lateral to the acetabulum (lateral to Perkin’s line). The hip is termed located if MP is < 33%, subluxated if MP is 33–89%, and completely dislocated if MP is ≥ 90%. The age at MP ≥ 40% was noted.
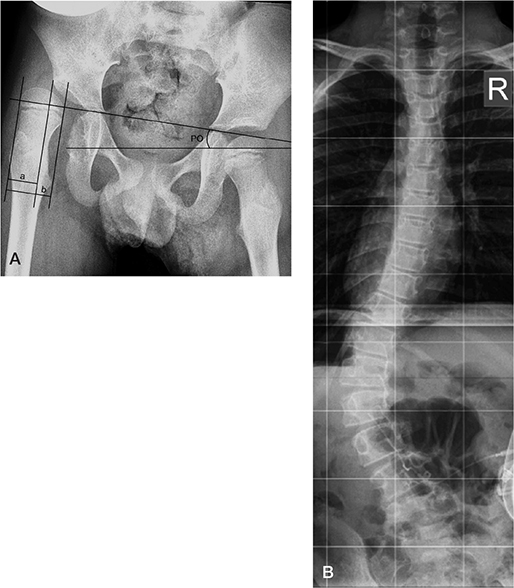
Figure 1. Radiographs of a boy with all 3 deformities: hip displacement, pelvic obliquity, and scoliosis.
A. AP pelvic radiograph in the supine position at the age of 7 years, showing the measurement of migration percentage (MP = a/b x 100) and pelvic obliquity (PO). MP was 67% in the right hip and 9% in the left. PO was 9° with the right side highest.
B. PA spine radiograph in the sitting position of the same boy at age 12.7 years, showing a thoraco-lumbar scoliosis of 56° with convexity to the left side, the opposite side of HD and high PO (R, right side).
Pelvic obliquity (PO) was measured in the supine position on the same pelvic radiographs as used for MP, as the angle between the horizontal line and Hilgenreiner’s line (Figure 1A).
Assessment of scoliosis was based on clinical examination and radiography. Clinical examination was performed once a year by a physiotherapist at the Child Rehabilitation Service, one in each county. The examination was done with the patient in the sitting position, if necessary, supported by a caregiver. The grade of scoliosis was subjectively assessed using the following classification: no scoliosis, mild scoliosis, moderate scoliosis, and severe scoliosis. If the scoliosis was found to be moderate or severe on clinical examination, a radiograph of the spine was taken.
Posteroanterior and lateral radiographs of the whole spine were taken with the patient in the sitting position (Figure 1B). The scoliosis was described by location in the spine (thoracolumbar or lumbar), shape of the curvature (C- or S-shaped), and the Cobb angle. If the curve was S-shaped, only the lumbar component was used for the analyses. All the spine radiographs that had been performed from the beginning of 2004 to 2021 were assessed. Only spine radiographs taken at the university hospital or at a local hospital and stored in our PACS system were evaluated. The age at scoliosis ≥ 40° was noted.
Because mild deformities have little clinical significance, only moderate and severe hip and spine deformities were used in most of the statistical analyses. The following cutoffs for clinically significant deformities were chosen: a Cobb angle ≥ 40° for scoliosis and MP ≥ 40% for hip displacement.
Statistics
SPSS (version 29, IBM Corp, Armonk, NY, USA) was used for the statistical analysis. Categorical variables were analyzed with the Pearson chi-square test. Continuous variables were analyzed with Student’s t-tests for independent samples. All tests were 2-sided and differences were considered significant when the P value was < 0.05. Correlation between parameters was evaluated by Pearson’s correlation coefficient (r). Univariable logistic regression was used to identify risk factors for scoliosis with Cobb angle ≥ 40°. Variables with P value < 0.05 were evaluated with multivariable logistic regression.
Local linear smooth plots (lowess) illustrated development of migration percentage, pelvic obliquity, and Cobb angle with age. It is a tool in regression analysis to create a smooth line through a timeplot to see relationships between variables and foresee trends. We used Stata/SE 18.0 for windows (StataCorp LLC, College Station, TX, USA) for making lowess plots. The plots were based on 690 pelvic radiographs (MP and PO) and 211 spine radiographs (Cobb angle).
Ethics, funding, and disclosures
The study protocol was approved by the Regional Committee of Medical Research Ethics, REC (ref. 2020/107726) and our institutional review board. The study was not funded by any external or internal party. There are no conflicts of interest. Complete disclosure of interest forms according to ICMJE are available on the article page, doi: 10.2340/17453674.2024.39915
Results
106 children met the inclusion criteria, 69 boys and 37 girls. None were excluded or lost to follow-up (Figure 2).
Hip and pelvis screening
The mean MP of the worst hip (greatest MP) on the initial radiograph of the 106 patients at a mean age of 3.0 years (range 0.7–9.5) was 28% (0–100) and the mean contralateral MP was 19% (0–100). MP increased almost linearly during the first years of follow-up, and the increase was greatest in children who underwent hip surgery to improve femoral head coverage (Figure 3). 78 patients (74%) developed hip subluxation (MP ≥ 33%), and 65 patients (61%) deteriorated to MP ≥ 40%. There were 25 girls and 40 boys at GMFCS level IV in 15 patients and level V in 50 patients. Unilateral HD occurred in 46 patients and bilateral HD in 19.
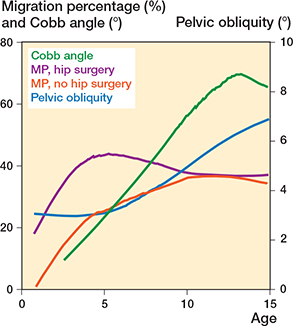
Figure 3. Local linear smooth plots (lowess) showing the development of migration percentage, pelvic obliquity, and Cobb angle in all the patients from age 1 to 15 years. The plots were based on 690 pelvic radiographs (MP and PO) and 211 spine radiographs (Cobb angle).
During the follow-up period, 59 of the 65 patients had undergone surgical treatment to improve their femoral head coverage (23 bilateral adductor and psoas releases and 36 pelvic osteotomies and/or varus femoral osteotomies in addition to the adductor/psoas releases). The mean age at surgery was 6.5 years (2.7–14.9). The mean age was lower in patients with soft tissue releases only compared with those who had osteotomies (5.1 and 7.0 years, respectively; P < 0.001). The outcome of surgery was graded according to Shore et al. [19] as “good” when the final MP was < 50% and the patient had not undergone subsequent bony surgery and “poor” if these demands were not met. The outcome was good in 41 patients and poor in 18. After hip surgery, the mean MP showed a moderate decrease, whereas there was a continuing increase, although at a slower rate, in the nonoperated hips until the age of 11–12 years (Figure 3).
The mean initial PO in the supine position in the 106 patients was 2.6° (range 0–13). PO was almost unchanged up to patient age 5 years and thereafter showed a moderate and almost linear increase up to age 15 years (Figure 3). The mean value at the last pelvic radiograph was 5.9° (0–30). When all the pelvic radiographs were analyzed, there was a significant correlation between MP of the worst hip (highest MP) and PO (r = 0.25; P < 0.001). In patients with severe unilateral HD (MP ≥ 60%), the sides of high PO and HD were the same in all patients except for 3, where PO was 0°.
Scoliosis screening
Radiographic scoliosis with Cobb angle ≥ 10° was diagnosed in 76 of the 106 patients (72%) at a mean age of 9.9 years (3–18). The mean initial Cobb angle was 35° (10–79). The Cobb angle increased almost linearly with age from 3 to 13 years (Figure 3). 71 children (67%) developed a Cobb angle ≥ 20°. Age at the first radiograph with Cobb angle ≥ 20° is shown in Table 1. At the age of 7–8 years, 21% of the children had a Cobb angle ≥ 20°.
60 patients (57%) developed a clinically significant (severe) scoliosis with Cobb angle ≥ 40°. This Cobb value occurred before 10 years of age in 16 children and before the age of 12 years in 30 children. Scoliosis convexity was on the right side in 24 patients and on the left side in 36. The curve was C-shaped in 47 patients and S-shaped in 13. The apex of the scoliosis was in the thoracic spine (T8–T12) in 18 cases and in the lumbar spine (L1–L4) in 42.
The possible risk factors for scoliosis with Cobb angle ≥ 40° are indicated in Table 2. In univariable analysis, these variables were significant risk factors: GMFCS level, initial MP, HD with MP ≥ 40% and ≥ 60%, hip operation, poor outcome of hip surgery, and intrathecal baclofen treatment. Using multivariable logistic regression, the independent risk factors were GMFCS level V and MP ≥ 60%. There was a significant correlation between the last Cobb angle and the last MP (r = 0.38; P < 0.001).
| Variables | n | Cobb angle | P value | ||
| < 40° | ≥ 40° | uni-variable | multi-variable | ||
| Sex | |||||
| Girls | 37 | 14 | 23 | 0.4 | |
| Boys | 69 | 32 | 37 | ||
| GMFCS level | |||||
| IV | 33 | 24 | 9 | < 0.001 | 0.003 |
| V | 73 | 22 | 51 | ||
| CP type | |||||
| Spastic bilateral | 81 | 31 | 50 | 0.1 | |
| Dyskinetic | 25 | 14 | 10 | ||
| Hip displacement | |||||
| MP < 40% | 41 | 24 | 17 | 0.01 | 0.2 |
| MP ≥ 40% | 65 | 22 | 43 | ||
| MP < 60% | 70 | 40 | 30 | < 0.001 | 0.002 |
| MP ≥ 60% | 36 | 6 | 30 | ||
| Unilateral | 46 | 17 | 29 | 0.4 | |
| Bilateral | 19 | 5 | 14 | ||
| Hip operation | |||||
| No | 47 | 25 | 22 | 0.04 | 0.3 |
| Soft tissue release a | 22 | 11 | 11 | ||
| Osteotomies | 37 | 10 | 27 | ||
| Outcome of hip surgery | |||||
| Good | 41 | 18 | 23 | 0.04 | 0.1 |
| Poor | 18 | 3 | 15 | ||
| Intrathecal baclofen | |||||
| No | 79 | 41 | 38 | 0.003 | 0.4 |
| Yes | 27 | 5 | 22 | ||
| Initial MP | 106 | 21 | 32 | 0.01 | 0.05 |
| Age at MP ≥ 40% | 65 | 4.3 | 5.1 | 0.2 | |
| GMFCS = gross motor function classification system; | |||||
| MP = migration percentage; | |||||
| a bilateral adductor and psoas release. | |||||
During the follow-up period, 32 patients had undergone operative correction and spine fixation at a mean age of 14.3 years (7.6–18.1). The mean Cobb angle at the last spine radiographs in nonoperated patients (the last preoperative radiograph in operated patients) was 73° (11–140).
Temporal sequence of HD and scoliosis
24 patients had no clinically significant spine or hip deformities, defined as MP ≥ 40% and Cobb angle ≥ 40°. The combinations of clinically significant deformities are listed in Table 3. 39 patients had 1 deformity only (HD in 22 patients and scoliosis in 17.). 43 patients had both HD and scoliosis.
The temporal sequence showed a trend to HD occurring before the other deformities (Figure 3). The mean age of clinically significant HD (MP ≥ 40%) was 4.8 years (0.7–12.5) and of scoliosis (Cobb angle ≥ 40°) 11.8 years (5.3–16.3). Of the 43 patients with both HD and scoliosis, HD occurred first in all but 1 patient.
Association between the side of hip displacement and convexity of scoliosis
Of the 43 patients with both HD and scoliosis, 2 patients had the same final MP in both hips. In the remaining 41 patients, the scoliosis was convex to the opposite side of the hip with the highest MP in 27 patients (66%), whereas 14 patients had both deformities on the same side (P = 0.04). When only patients with severe unilateral hip displacement (MP ≥ 60%) were analyzed, the scoliosis was convex to the opposite side of HD in 14 of 19 patients (74%), which was significantly more frequent than the 5 patients with convexity to the same side (P = 0.04).
13 patients with HD occurring before scoliosis developed severe unilateral HD (MP ≥ 60%), PO > 5° with the high side of PO on the same side as HD, and scoliosis with Cobb angle ≥ 40°. There might be a causal relationship with HD leading to scoliosis in 8 of these patients because the convexity of the scoliosis was to the opposite side of HD. In the remaining patients, scoliosis convexity was to the same side as HD.
Discussion
The aims of this study were to examine the prevalence of scoliosis, HD, and PO in nonambulatory children with CP, to look at the temporal sequence of the deformities, and to study whether severe unilateral HD can be a contributory factor in the development of scoliosis.
We found that the combination of clinically significant HD and scoliosis occurred quite frequently, that HD appeared before scoliosis in the great majority of the patients, and that severe unilateral HD might be a contributory factor in the development of scoliosis in some patients.
Since we intended to analyze only deformities of clinical importance, rather strict definitions were used. A Cobb angle of ≥ 40° was chosen because this was recommended as cutoff for surgical treatment in clinical practice [10,20]. A cutoff of 40% for MP is a commonly used limit for hip displacement that needs surgical treatment to improve femoral head coverage [4,21]. The degree of clinically significant supine position PO is uncertain, and this deformity is usually combined with HD. Thus, no cutoff for PO was used in the present study. Supine position PO is less than sitting position PO measured on spine radiographs because of the effect of gravity. Patel and Shapiro [23] found that supine PO was less than half the PO measured in the sitting position. We tried to measure the sitting PO but found the measurements rather unreliable because the pelvic landmarks were not always clearly depicted on the spine radiographs. Thus, the sitting PO values were not included.
The prevalence of scoliosis in CP increases with decreasing functional level of the patients [2,20,24]. In GMFCS level V, the rates of scoliosis ≥ 40° at or shortly after skeletal maturity was reported to be 48% [25], whereas higher rates were found by Hägglund et al. [2] and in our study (75% and 70%, respectively).
Hip subluxation is common in nonambulatory children, with a prevalence of approximately 70% at GMFCS level V [14,26]. This is in accordance with our prevalence of 70% at level V with MP 40% as cutoff. The prevalence of the combination of scoliosis and HD has, to our knowledge, not been analyzed in previous population-based studies. We found that 41% of the patients had both scoliosis and HD. Of the patients with scoliosis, 72% also had HD, whereas Hadad et al. [27] in a nonpopulation-based study found that 79% had this combination.
The mean supine PO at the initial pelvic radiographs was only 2.6° and at the last radiograph 5.9°, which corresponds with the median supine position PO of 4° reported by Heidt et al. [9]. This indicates that PO is usually moderate in spite of HD and scoliosis. In a Swedish CP register study, the prevalence of supine position PO ≥ 5° increased with increasing GMFCS levels [22], which is in agreement with our results.
Letts et al. [11] reported that the most common temporal sequence of the deformities was dislocation of the hip occurring first, followed by PO, and finally scoliosis. In disagreement with this, Senaran et al. [8] had the impression that scoliosis, PO, and HD tended to begin at the same time and progressed together or with scoliosis preceding the others. However, none of these studies were population-based. In our population-based study the most common pattern was HD, or the combination HD/PO diagnosed first and scoliosis last. One reason could be that hip surveillance begins at age 1–2 years and consists of yearly pelvic radiographs, which contributes to early detection of HD. The scoliosis surveillance involves a yearly clinical examination of the back, which could fail to detect small and moderate degrees of scoliosis [24]. Moreover, a spine radiograph was not taken until the magnitude of the scoliosis was clinically assessed to be moderate or severe.
The relationship between the sides of HD, PO, and scoliosis is controversial [8,11,12]. In unilateral HD, the high side of PO was on the same side as the displaced hip in all the patients in some studies [9,11], as well as in our study. Senaran et al. [8] found this pattern in 67% of patients, whereas no significant correlation between the high side of PO and the side of HD was reported by Lonstein and Beck [12]. In severe unilateral HD, the scoliosis was convex to the opposite side of the high pelvic side in all the patients of Senaran et al. [8] and in 77% in the study by Letts et al. [11], which corresponds well with our findings in severe unilateral HD, where the convex side of the scoliosis was opposite to the high PO side and the displaced hip in 74% of the patients.
We found that severe HD was a risk factor for development of scoliosis and there was a significant correlation between the MP and the Cobb angle, indicating a close association between HD and scoliosis. It has been speculated whether severe unilateral HD can cause scoliosis [10,11]. If unilateral HD appears first and is accompanied by PO with the high side on the same side as HD, and scoliosis occurs later and has the convexity on the contralateral side, it might seem probable that HD was a contributory cause of scoliosis. However, this combination was seen in only 8 of the 22 patients with severe, unilateral HD in the present study. This indicates that HD and scoliosis usually develop independently of each other.
Limitation
First, the hip screening with yearly pelvic radiographs was more comprehensive than the scoliosis screening with clinical screening alone. Second, the primary spine radiographs at the local hospitals were probably not always sent to our hospital in cases of mild or moderate scoliosis. This could cause a delay in the registration of radiographic diagnosis of scoliosis and thus reduce the reliability of the temporal sequence of the deformities. Third, the natural history of the relationship between scoliosis and HD could not be fully evaluated because many patients with HD had undergone surgical treatment before scoliosis was detected. The main strength of the study is that it was population-based with follow-up of all the patients, which should imply good generalizability of the results.
What is the clinical relevance of this study?
As HD with MP ≥ 60% was one of the independent risk factors of scoliosis, this severe degree of HD should be avoided by a good hip surveillance program and timely and correct surgical treatment. Our results, especially the relatively late detection of scoliosis, indicate that the surveillance of scoliosis in children with CP needs improvement in order to detect the deformity and consider initiation of treatment at an earlier age. Thus, the initial spine radiographs should be taken earlier, especially in patients at GMFCS level IV/V; in this group it seems rational to take spine radiographs when the patient is aged 7–8 years, at which time approximately 21% of the patients had a Cobb angle ≥ 20°.
Conclusion
The combination of scoliosis and HD was frequent, and HD was diagnosed first in almost all the patients. HD might be a contributory cause of scoliosis in patients with severe, unilateral HD, PO, and later scoliosis with convexity to the opposite side.
- Howard C B, McKibbin B, Williams L A, Mackie I. Factors affecting the incidence of hip dislocation in cerebral palsy. J Bone Joint Surg Br 1985; 67: 530-2. doi: 10.1302/0301-620X.67B4.4030844.
- Hägglund G, Pettersson K, Czuba T, Persson-Bunke M, Rodby-Bousquet E. Incidence of scoliosis in cerebral palsy: a population-based study of 962 young individuals. Acta Orthop 2018; 89: 443-7. doi: 10.1080/17453674.2018.1450091.
- Madigan R R, Wallace S L. Scoliosis in the institutionalized cerebral palsy population. Spine 1981; 6: 583-90. doi: 10.1097/00007632-198111000-00009.
- Terjesen T. The natural history of hip displacement in cerebral palsy. Dev Med Child Neurol 2012; 54: 951-7. doi: 10.1111/j.1469-8749.2012.04385.x.
- Samilson R L, Tsou P, Aamoth G, Green W. Dislocation and subluxation of the hip in cerebral palsy. J Bone Joint Surg Am 1972; 54: 863-73. PMID: 5055174.
- Cooperman D R, Bartucci E, Dietrick E, Millar E A. Hip dislocation in cerebral palsy: long-term consequences. J Pediatr Orthop 1987; 7: 268-76. doi: 10.1097/01241398-198705000-00005.
- Majd M E, Muldowny D S, Holt R T. Natural history of scoliosis in the institutionalized adult cerebral palsy population. Spine 1997; 22: 1461-6. doi: 10.1097/00007632-199707010-00007.
- Senaran H, Shah S A, Glutting J J, Dabney K W, Miller F. The associated effects of untreated unilateral hip dislocation in cerebral palsy scoliosis. J Pediatr Orthop 2006; 26: 769-72. doi: 10.1097/01.bpo.0000242426.60995.29.
- Heidt C, Hollander K, Wawrzuta J, Molesworth C, Willoughby K, Thomason P, et al. The radiological assessment of pelvic obliquity in cerebral palsy and the impact on hip development. Bone Joint J Br 2015; 97: 1435-40. doi: 10.1302/0301-620X.97B10.35390.
- Helenius I J, Viehweger E, Castelein R M. Cerebral palsy with dislocated hips and scoliosis: what to deal with first? J Child Orthop 2020; 14: 24-9. doi: 10.1302/1863-2548.14.190099.
- Letts M, Shapiro L, Mulder K, Klassen O. The windblown hip syndrome in total body cerebral palsy. J Pediatr Orthop 1984; 4: 55-62. doi: 10.1097/01241398-198401000-00013.
- Lonstein J E, Beck K. Hip dislocation and subluxation in cerebral palsy. J Pediatr Orthop 1986; 6: 521-6. doi: 10.1097/01241398-198609000-00001.
- Garg S, Engelman G, Yoshihara H, McNair B, Chang F. The relationship of gross motor functional classification scale level and hip dysplasia on the pattern and progression of scoliosis in children with cerebral palsy. Spine Deformity 2013; 1: 266-71. doi: 10.1016/j.jspd.2013.05.002.
- Hägglund G, Andersson S, Düppe H, Lauge-Pedersen H, Normark E, Westbom L. Prevention of dislocation of the hip in children with cerebral palsy: the first ten years of a population-based prevention programme. J Bone Joint Surg Br 2005; 87: 95-101. doi: 10.1097/01202412-200507000-00007.
- Soo B, Howard J J, Boyd R N, Reid S M, Lanigan A, Wolfe R, et al. Hip displacement in cerebral palsy. J Bone Joint Surg Am 2006; 88: 121-9. doi: 10.2106/JBJS.E.00071.
- Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl 2007; 109: 8-14. PMID: 17370477.
- Palisano R J, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol 1997; 39: 214-23.
- Reimers J. The stability of the hip in children. Acta Ortop Scand 1980; 51(Suppl. 184): 12-19. doi: 10.3109/ort.1980.51.suppl-184.01.
- Shore B J, Zurakowski D, Dufreny C, Powell D, Mathenay T H, Snyder B. Proximal femoral varus derotation osteotomy in children with cerebral palsy: the effect of age, gross motor classification system level, and surgical volume on surgical success. J Bone Joint Surg Am 2015; 97: 2024-31. doi: 10.2106/JBJS.O.00505.
- Saito N, Ebara S, Ohotsuka K, Kumeta H, Takaoka K. Natural history of scoliosis in cerebral palsy. Lancet 1998; 351: 1687-92. doi: 10.1016/S0140-6736(98)01302-6.
- Hägglund G, Lauge-Pedersen H, Persson M. Radiographic threshold values for hip screening in cerebral palsy. J Child Orthop 2007; 1: 43-7. doi: 10.1007/s11832-007-0012-x.
- Hägglund G. Association between pelvic obliquity and scoliosis, hip displacement and asymmetric hip abduction in children with cerebral palsy: a cross-sectional registry study. BMC Musculoskelet Disord 2020; 21: 464. doi: 10.1186/s12891-020-03484-y.
- Patel J, Shapiro F. Simultaneous progression patterns of scoliosis, pelvic obliquity, and hip subluxation/dislocation in non-ambulatory neuromuscular patients: an approach to deformity documentation. J Child Orthop 2015; 9: 345-56. doi: 10.1007/s11832-015-0683-7.
- Vinje S, Terjesen T, Kibsgård, T. Scoliosis in children with severe cerebral palsy: a population-based study of 206 children at GMFCS levels III-V. European Spine J 2023; Aug 2. doi: 10.1007/s00586-023-07868-1.
- Willoughby K L, Ang, S G, Thomason P, Rutz E, Shore B, Buckland A J, et al. Epidemiology of scoliosis in cerebral palsy: a population-based study at skeletal maturity. J Paediat Child Health 2022; 58: 295-301. doi: 10.1111/jpc.15707.
- Connelly A, Flett P, Graham H K, Oates J. Hip surveillance in Tasmanian children with cerebral palsy. J Paediatr Child Health 2009; 45: 437-43. doi: 10.1111/j.1440-1754.2009.01534.x.
- Hadad M J, Xu A L, Bryant B R, Andrade N S, Hoon A H, Sponseller P D. Why the hips remain stable when the spine strays: a deeper analysis of the relationship between hip displacement and severe scoliosis in patients with cerebral palsy. J Pediatr Orthop 2021; 41: 261-6. doi: 10.1097/BPO.0000000000001765.