Spinal surgery and the risk of reoperation after total hip arthroplasty: a cohort study based on Swedish spine and hip arthroplasty registers
Ted ENEQVIST 1,2, Louise PERSSON 1,2, Emma KOJER 1, Linus GUNNARSSON 1, and Paul GERDHEM 3-5
1 Department of Clinical Sciences, Södersjukhuset, Karolinska Institutet, Stockholm; 2 Department of Orthopaedics, Södersjukhuset, Stockholm; 3 Department of Clinical Science, Intervention and Technology (CLINTEC), Karolinska Institutet, Stockholm; 4 Department of Orthopaedics and Hand Surgery, Uppsala University Hospital; 5 Department of Surgical Sciences, Uppsala University, Uppsala, Sweden.
Background and purpose — Studies suggest increased revision risk of total hip arthroplasty (THA) in individuals with lumbar spinal fusion, but studies including non-fused individuals are lacking. We aimed to investigate whether individuals undergoing lumbar spinal stenosis surgery with or without fusion are at an increased risk of reoperation before or after THA.
Patients and methods — The Swedish Spine Register and the Swedish arthroplasty register were searched from 2000 through 2021. Chi-square, Kaplan–Meier and binary multivariate logistic regression were used to compare reoperation rates up to 10 years after THA surgery
Results — 7,908 individuals had undergone lumbar spinal stenosis surgery (LSSS) (fusion n = 1,281) and THA. LSSS before THA compared with THA-only controls was associated with a higher risk of THA reoperations: 87 (2%) out of 3,892 vs. 123 (1%) out of 11,662 (P < 0.001). LSSS after THA compared with THA-only controls was not associated with a higher risk of reoperation, confirmed by Kaplan– Meier analyses and binary multivariate logistic regression. Mortality was lower in individuals undergoing both LSSS and THA, regardless of procedure order. There was no difference in THA reoperations in individuals who had undergone LSSS before THA without fusion or with fusion. The individuals who had undergone LSSS after THA with fusion had an increased risk of THA reoperation compared with those without fusion.
Conclusion — LSSS with or without fusion before THA is associated with an increased risk of THA reoperation. Spinal fusion increased the risk of reoperation of THA when performed after THA.
Citation: Acta Orthopaedica 2024; 95: 12–18. DOI https://doi.org/10.2340/17453674.2024.35228.
Copyright: © 2024 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2023-08-20. Accepted: 2023-12-05. Published: 2024-01-18.
Correspondence: paul.gerdhem@uu.se
TE and PG conceived the idea, designed and directed the study, and are accountable for all aspects of the work. LP, EK, and LG drafted the manuscript with input from TE and PG. All contributed with interpretation of the results. PG edited the final manuscript before submission. PG is the corresponding author. PG supported the study with grants for the ethical application, data retrieval, and statistical analysis.
Joakim Ruist, Registercentrum Västra Götaland, is thanked for statistical expertise, and Carina Blom, Swespine, for help with data extraction.
Handling co-editor: Ilkka Helenius
Acta thanks Benny Dahl, Filip C Dolatowski and Samo Karl Fokter for help with peer review of this manuscript.
The coexistence of lumbar spinal stenosis and hip osteoarthritis is common, and an estimated 18% of individuals with total hip arthroplasty (THA) have a concurrent lumbar spine disorder [1]. In Sweden, 3.5% of individuals with THA have had previous lumbar spine surgery [2]. It is likely that THA and surgery for lumbar spinal stenosis will increase in the future, increasing the number of individuals that undergo both procedures [3,4].
Due to the overlap of symptoms in degenerative hip and lumbar spine conditions, correct diagnosis and treatment is a challenge for clinicians [5]. Identifying the condition that primarily drives the pain, and the surgical treatment that has priority, may be difficult [5,6]. Pre-existing lumbar surgery in THA individuals may also result in worse patient-reported outcomes than in those without any spinal surgery [2].
Recent studies have reported an increased risk of dislocation and revision of THA in individuals with a prior or subsequent spinal fusion [7-9].
Previous studies on dislocation and revision risk of THA in individuals with prior or subsequent lumbar spine surgery have not included individuals without fusion. This is an important knowledge gap to fill, as only a minority of the patients with the most common reason for spine surgery, lumbar spinal stenosis, need a spinal fusion [10,11].
The aim of our study was to investigate whether individuals undergoing lumbar spinal stenosis surgery with or without fusion are at an increased risk of THA reoperation compared with controls with THA only, and whether the risk is dependent on the order of the procedures.
Patients and methods
Sources of data
Data collection has been done prospectively, but the study design is retrospective. The study was designed before data retrieval. Data from the Swedish Spine Register (Swespine), the Swedish Hip Arthroplasty Register (SHAR), and the National Board of Health and Welfare Mortality register was used. The coverage of Swespine is 95% [12] and of SHAR 98% [13]. Between 93% and 96% of reoperations are registered in SHAR [13]. Mortality data is considered complete in Sweden. All registers use the same unique personal identification number (PIN) for data linkage.
The checklist STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) has been used when preparing this manuscript.
Selection of cases and controls
The selection process for cases and controls is shown in Figure 1. The Swedish Spine Register and the Swedish Arthroplasty Register were searched from 2000 through 2021 as follows.
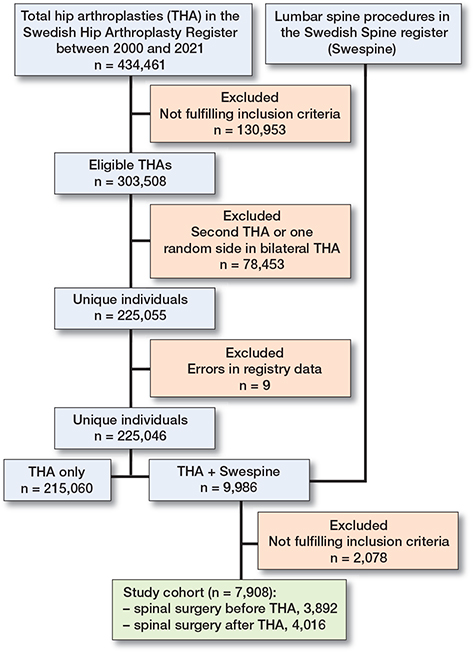
Figure 1. Flowchart. Selection from the Swedish Hip Arthroplasty Register and the Swedish Spine Register. THA = total hip arthroplasty.
Cases: were individuals that had undergone both lumbar spinal stenosis surgery and primary total hip arthroplasty at any time from 2000 through 2021.
We included individuals 40 years of age or older at the time of the primary THA with surgery performed with only lateral or posterior surgical approaches. If an individual were to receive 2 primary THAs, only the first prosthesis was included. If both THAs were inserted at the same time 1 of them was included randomly.
Individuals in Swespine had to have 1 of the following diagnoses at surgery: central spinal stenosis with or without degenerative olisthesis, lateral spinal stenosis, recess stenosis, or foraminal stenosis. Surgery had to be decompression only (any type), or decompression with fusion (instrumented or non-instrumented, with or without interbody fusion) limited to any segment(s) between the first lumbar vertebra and the sacrum.
The cases were grouped together or subdivided into those that had undergone lumbar spinal stenosis surgery, with or without fusion, before or after the THA.
Controls: were individuals who had undergone THA with the same inclusion criteria as the cases but lacked a record of lumbar spine surgery (of any type) in Swespine.
Cases and controls were for some analyses matched for age, sex, and year of THA surgery. For each case that underwent lumbar spinal stenosis surgery before THA we were able to identify 3 controls. For each case that underwent lumbar spinal stenosis surgery after THA we were able to identify 5 controls. Matched controls had neither undergone a THA reoperation nor were deceased at the time of the second surgery (lumbar spinal stenosis surgery or THA, depending on order) of its matched case.
Follow-up
The follow-up period ended with the first reoperation on the THA and was limited to a maximum of 10 years starting from the time of the second surgical procedure (lumbar spinal stenosis surgery or THA, depending on order).
Outcome
The outcome was THA reoperation due to any cause, with the exception of metastasis or infection.
Statistics
Means and standard deviation (SD) were used to present continuous variables and numbers (%) were used for categorical variables. P values for categorical values were calculated with chi-square tests.
The absolute risk and cumulative reoperation rates were used to assess the difference in risk between cases and controls. The cumulative reoperation rate and the cumulative mortality rate were assessed using the Kaplan–Meier method, presented with 95% confidence intervals (CI).
Further comparisons of the risk of reoperation between cases and controls were made using binary multivariate logistic regression models, presented as odds ratio with a CI. The dependent variable was THA reoperation. Independent variables were lumbar spinal stenosis surgery either before or after THA, age (continuous), sex (female/male), and year of surgery. To minimize the influence of death as a confounder in these analyses, regressions results were based on individuals who had a follow-up period of 5 or 10 years.
SAS 15.2 (SAS Institute Inc., Cary, NC, USA) was used for processing data. Calculations were made using R 4.2.0 (R Foundation for Statistical Computing, Vienna, Austria). Statistical significance was set to P < 0.05.
Ethics, registration, data sharing plan, funding, and disclosures
Swespine and the Swedish Hip Arthroplasty Register use opt-out, meaning that patient consent is not needed to be part of the quality register. Information on the registers is given to the individual via signs in the hospitals or handouts. The patient can at any time withdraw their participation in the registers and all data will then be removed.
This study has been approved by the Swedish Ethical Review Authority in Stockholm (2018/2705-31/2). PG was supported by Region Stockholm (ALF), by CIMED, Karolinska Institutet, Sweden, Uppsala University, Sweden, and the Swedish Research Council. The funding sources had no role in the study design, analyses or interpretation of data, in the manuscript writing, or in the decision to submit the paper for publication.
The authors have no conflicts of interest. Complete disclosure of interest forms according to ICMJE are available on the article page, doi: 10.2340/17453674.2024.35228
Results
7,908 individuals had undergone lumbar spinal stenosis surgery, with or without fusion, and THA, and 215,060 individuals had undergone THA only (Figure 1).
Order of lumbar spinal stenosis surgery and THA: matched controls
The absolute risk of reoperation was significantly higher in individuals undergoing lumbar spinal stenosis surgery before THA compared with matched controls, while no significant difference was seen between individuals undergoing lumbar spinal stenosis surgery after THA compared with matched controls (Table 1).
| Factor | LSSS before THA n = 3,892 | Matched controls a n = 11,662 | P value | LSSS after THA n = 4,016 | Matched controls b n = 20,072 | P value |
| Age, mean (SD) | 71.3 (8.3) | 71.3 (8.3) | 66.8 (8.2) | 66.8 (8.2) | ||
| Female | 2,307 (59) | 6,921 (59) | 2,213 (55) | 11,065 (55) | ||
| Reoperatio c | 87 (2) | 123 (1) | < 0.001 | 130 (3) | 549 (3) | 0.08 |
| LSSS = lumbar spinal stenosis surgery, SD = standard deviation, THA = total hip arthroplasty. | ||||||
| a Matched, 3 controls (THA only) per LSSS case. | ||||||
| b Matched, 5 controls (THA only) per LSSS case. | ||||||
| c THA reoperation. | ||||||
The Kaplan–Meier curves of cumulative reoperation rates showed similar findings, with higher reoperation rates in those undergoing lumbar spinal stenosis surgery before THA compared with their matched controls (Figure 2).
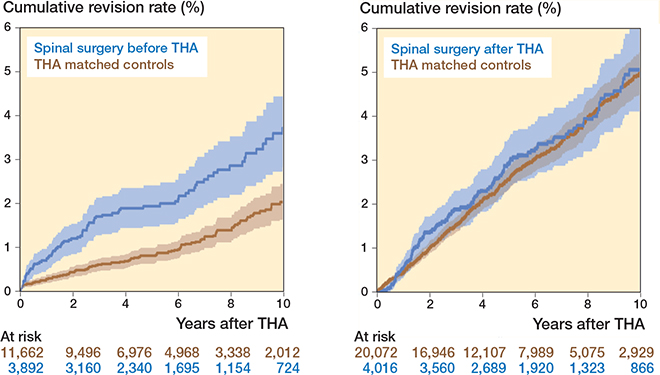
Figure 2. Kaplan–Meier curves of cumulative total hip arthroplasty (THA) reoperation rates, counted once per case, and matched control. CI is presented as shadowed area.
Order of lumbar spinal stenosis surgery and THA: all controls
Using cases and controls with 5 or 10 years’ follow-up, the reoperation rate was significantly higher at 5 years, but not at 10 years, in individuals undergoing lumbar spinal stenosis surgery before THA compared with individuals undergoing THA only (Table 2, see Appendix). No significant differences were seen in reoperation rate between individuals undergoing lumbar spinal stenosis surgery after THA compared with individuals undergoing THA only (Table 2, see Appendix).
The risk of reoperation was significantly higher for individuals undergoing lumbar spinal stenosis surgery before THA at the 5-year follow-up, but not at 10 years, compared with THA only (Table 3). Older age, more recent surgery, and female sex was associated with a lower risk of reoperation (Table 3). The risk of reoperation was not significantly increased for individuals undergoing lumbar spinal stenosis surgery after THA (Table 3).
Lumbar spinal stenosis surgery with and without fusion
Only in individuals with lumbar spinal stenosis surgery after THR was there a higher risk of reoperation after a decompression and fusion procedure compared with decompression alone (Table 4). The Kaplan–Meier curves showed a similar, but non-significant, trend (Figure 3, see Appendix).
| Factor | No fusion | Fusion | P value |
| LSSS before THA | |||
| No reoperation | 3,060 (97) | 732 (97) | |
| Reoperation a | 79 (3) | 19 (3) | 0.98 |
| LSSS after THA | |||
| No reoperation | 3,379 (97) | 497 (94) | |
| Reoperation a | 107 (3) | 33 (6) | < 0.001 |
| THA = total hip arthroplasty. | |||
| a THA reoperation. | |||
Mortality
Lower mortality rates were seen for individuals undergoing both lumbar spinal stenosis surgery and THA, irrespective of order, compared with controls (Figure 4).
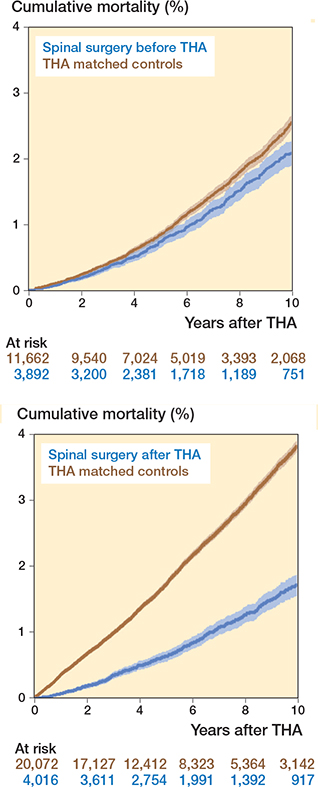
Figure 4. Kaplan–Meier curves of cumulative mortality. CI is presented as shadowed area.
Discussion
We aimed to investigate whether individuals undergoing lumbar spinal stenosis surgery with or without fusion are at an increased risk of reoperation before or after THA. We found an increased risk of THA reoperation in individuals undergoing lumbar spinal stenosis surgery before THA compared with THA-only controls. Our results imply a lower absolute risk of reoperation when lumbar spinal stenosis surgery is performed before THA compared with after.
THA reoperation rates presented in our study were slightly lower than in previous studies [6-9]. One reason could be that this study included lumbar spinal stenosis surgery both with and without fusion [7,9,14], although a larger reoperation risk was noted only for fusion surgery performed after THA in our cohort, which has data spanning more than 20 years. That lumbar spinal stenosis is generally treated without fusion is also reflected in recent figures from Swespine [12].
Previous studies have reported an increased risk of THA reoperations in individuals with spinal fusion [7-9]. This contributes to the hypothesis that a stiff spine can alter the biomechanics of the spinopelvic unit and increase dislocation rates compared with the general THA population. Sing et al. [9] conducted a register study with 589,300 THA patients and 9,695 THA patients with spinal fusion. They showed a 2-year revision rate of THA of 5–7% for spinal fusion compared with 3.4% in the control group. This was in line with the case-control study conducted by Perfetti et al. [8] comparing 934 THA patients with previous spinal fusion with matched controls, reporting a 12-month revision rate of 3.9% and 0.9%, respectively.
More limited spinopelvic mobility after lumbar spinal fusion surgery has been suggested as the cause of an increased THA dislocation and reoperation risk. However, an individual does not have to undergo a spinal fusion to have a stiff spine. A degenerative spine can be stiff as well, also affecting the stability of the hip joint [15]. Sultan et al. [16] presented an increased risk of THA dislocation and revision in individuals with coexisting sagittal plane spinal deformities.
Our cohort, with 84% of the cases having a decompression only as their spinal stenosis surgery, suggests that the prevalence of lumbar spinal stenosis itself constitutes a risk for THA reoperation, possibly through the same mechanisms as in the setting of spinal deformities. In addition, it seems that lumbar spine decompression without fusion at least does not increase the spinal stiffness, supporting the idea that the spinal pathology itself may increase the risk, and not necessarily only the surgical procedure [17,18].
Surgical order
There is no consensus in the literature on the preferred order of spinal fusion surgery and THA, but a recent systematic review and meta-analysis evaluating the order of lumbar spinal fusion and THA showed no significant differences in THA dislocation or revision irrespective of whether spinal fusion was performed subsequent or prior to THA [6].
Our results imply a lower absolute risk of reoperation when lumbar spinal stenosis surgery is performed before THA as compared with after (Table 2, see Appendix). Also, there were a higher number of reoperations when a spinal fusion procedure was performed after THA. In addition, a previous Swedish study showed better health-related quality of life improvements when lumbar spinal stenosis surgery was performed before THA [19].
This could possibly be supporting spinal surgery as the initial procedure in cases with symptoms of the same magnitude from both the hip and the spine, although there is no need to refrain from lumbar spinal stenosis surgery in general after a previous THA.
Mortality
To our knowledge, no previous studies have assessed mortality in individuals with hip-spine syndrome undergoing both THA and spinal surgery. Other studies have shown decreased mortality rates in individuals with both previous THA [20-22], and previous degenerative spinal deformity surgery [23] compared with nonoperated populations. It is likely that this selection bias is even more evident in individuals undergoing more than one elective surgery.
Strengths and limitations
Data used in this study comes from well-established national quality registers with high coverage rates and long follow-ups giving external validity.
Due to the nature of the observational study, selection bias cannot be excluded and causality between exposure and outcome cannot be revealed. Even though the Swedish national registers have a high degree of coverage with a high number of individuals included, few undergo both THA and lumbar spinal stenosis surgery, of whom a minority undergo spinal fusion. In addition, few of these are undergoing THA reoperation. This makes it impossible to delineate the relationship between different types of spinal procedures and THA reoperation. Coverage is high in the registers, but information not entered cannot be accounted for. Reliable comorbidity data is not available in the registers and could not be controlled for. However, we did include a sub-analysis taking mortality into account, which is arguably a more reliable measure of sickness.
Data on sagittal and coronal alignment is not available for individuals undergoing lumbar spinal stenosis surgery in Swespine, so any relationships between such variables and reoperation risk cannot be determined. However, individuals with a degenerative spinal deformity have not been included in the sample retrieved from Swespine for this specific study.
We used reoperations as outcome. Another tentative outcome would have been dislocations. However, closed reductions are not reported to the Swedish Hip Arthroplasty Register. For the individual, repeated dislocations may ultimately lead to the more important outcome, reoperation, which we chose for this study.
Conclusion
Lumbar spinal stenosis surgery with or without fusion before THA is associated with an increased risk of reoperation compared with controls undergoing THA only. Our results imply a lower absolute risk of reoperation when lumbar spinal stenosis surgery is performed before THA compared with after.
In perspective, doing spinal surgery as the initial procedure should be considered in cases with symptoms of the same magnitude from both the hip and the spine.
- Prather H, Van Dillen L R, Kymes S M, Armbrecht M A, Stwalley D, Clohisy J C. Impact of coexistent lumbar spine disorders on clinical outcomes and physician charges associated with total hip arthroplasty. Spine J 2012; 12: 363-369. doi: 10.1016/j.spinee.2011.11.002.
- Eneqvist T, Nemes S, Brisby H, Fritzell P, Garellick G, Rolfson O. Lumbar surgery prior to total hip arthroplasty is associated with worse patient-reported outcomes. Bone Joint J 2017; 99-b: 759-65. doi: 10.1302/0301-620x.99b6.bjj-2016-0577.r2.
- Singh J A, Yu S, Chen L, Cleveland J D. Rates of total joint replacement in the United States: future projections to 2020–2040 using the national inpatient sample. J Rheumatol 2019; 46: 1134-40. doi: 10.3899/jrheum.170990.
- Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ 2016; 352: h6234. doi: 10.1136/bmj.h6234.
- Chavarria J C, Douleh D G, York P J. The hip-spine challenge. J Bone Joint Surg Am 2021; 103: 1852-60. doi: 10.2106/JBJS.20.01728.
- Onggo J R, Nambiar M, Onggo J D, Phan K, Ambikaipalan A, Babazadeh S, et al. Comparable dislocation and revision rates for patients undergoing total hip arthroplasty with subsequent or prior lumbar spinal fusion: a meta-analysis and systematic review. Eur Spine J 2021; 30: 63-70. doi: 10.1007/s00586-020-06635-w.
- Buckland A J, Puvanesarajah V, Vigdorchik J, Schwarzkopf R, Jain A, Klineberg E O, et al. Dislocation of a primary total hip arthroplasty is more common in patients with a lumbar spinal fusion. Bone Joint J 2017; 99-B: 585-91. doi: 10.1302/0301-620X.99B5.BJJ-2016-0657.R1.
- Perfetti D C, Schwarzkopf R, Buckland A J, Paulino C B, Vigdorchik J M. Prosthetic dislocation and revision after primary total hip arthroplasty in lumbar fusion patients: a propensity score matched-pair analysis. J Arthroplasty 2017; 32: 1635-40 e1631. doi: 10.1016/j.arth.2016.11.029.
- Sing D C, Barry J J, Aguilar T U, Theologis A A, Patterson J T, Tay B K, et al. Prior lumbar spinal arthrodesis increases risk of prostheticrelated complication in total hip arthroplasty. J Arthroplasty 2016; 31: 227-232 e221. doi: 10.1016/j.arth.2016.02.069.
- Austevoll I M, Hermansen E, Fagerland M W, Storheim K, Brox J I, Solberg T, et al. Decompression with or without fusion in degenerative lumbar spondylolisthesis. N Engl J Med 2021; 385: 526-38. doi: 10.1056/NEJMoa2100990.
- Forsth P, Olafsson G, Carlsson T, Frost A, Borgstrom F, Fritzell P, et al. A randomized, controlled trial of fusion surgery for lumbar spinal stenosis. N Engl J Med 2016; 374: 1413-23. doi: 10.1056/NEJMoa1513721.
- Fritzell P, Hägg O, Gerdhem P, Abbott A, Skarvinge C, Parai C, et al. Swespine årsrapport 2022. Uppföljning av ryggkirurgi utförd i Sverige år 2021. För Svensk Ryggkirurgisk förening [in Swedish]. Available from: https://swespine.se/page.aspx?id=12&lang=1. 2022.
- W-Dahl A, Kärrholm J, Rogmark C, Mohaddes M, Carling M, Sundberg M, et al. Årsrapport 2022: Svenska Ledprotesregistret [in Swedish]. Available from: https://registercentrum.blob.core.windows.net/slr/r/Svenska-Ledprotesregistret-rsrapport-2022_SE-2--BkxW4idh1s.pdf.2022.
- Eneqvist T, Bulow E, Nemes S, Brisby H, Garellick G, Fritzell P, et al. Patients with a previous total hip replacement experience less reduction of back pain following lumbar back surgery. J Orthop Res 2018; 36: 2484-90. doi: 10.1002/jor.24018.
- Eftekhary N, Shimmin A, Lazennec J Y, Buckland A, Schwarzkopf R, Dorr L D, et al. A systematic approach to the hip–spine relationship and its applications to total hip arthroplasty. Bone Joint J 2019; 101-B: 808-16. doi: 10.1302/0301-620X.101B7.BJJ-2018-1188.R1.
- Sultan A A, Khlopas A, Piuzzi N S, Chughtai M, Sodhi N, Mont M A. The impact of spino-pelvic alignment on total hip arthroplasty outcomes: a critical analysis of current evidence. J Arthroplasty 2018; 33: 1606-16. doi: 10.1016/j.arth.2017.11.021.
- Forsth P, Svedmark P, Noz M E, Maguire G Q, Jr, Zeleznik M P, Sanden B. Motion analysis in lumbar spinal stenosis with degenerative spondylolisthesis: a feasibility study of the 3DCT technique comparing laminectomy versus bilateral laminotomy. Clin Spine Surg 2018; 31: E397-E402. doi: 10.1097/BSD.0000000000000677.
- Lener S, Schmolz W, Abramovic A, Kluger P, Thome C, Hartmann S. The effect of various options for decompression of degenerated lumbar spine motion segments on the range of motion: a biomechanical in vitro study. Eur Spine J 2023; 32: 1358-66. doi: 10.1007/s00586-02307587-7.
- Eneqvist T, Bulow E, Nemes S, Brisby H, Fritzell P, Rolfson O. Does the order of total hip replacement and lumbar spinal stenosis surgery influence patient-reported outcomes: an observational register study. J Orthop Res 2021; 39: 998-1006. doi: 10.1002/jor.24813.
- Barrett J, Losina E, Baron J A, Mahomed N N, Wright J, Katz J N. Survival following total hip replacement. J Bone Joint Surg Am 2005; 87: 1965-71. doi: 10.2106/JBJS.D.02440.
- Lie S A, Engesaeter L B, Havelin L I, Gjessing H K, Vollset S E. Mortality after total hip replacement: 0–10-year follow-up of 39,543 patients in the Norwegian Arthroplasty Register. Acta Orthop Scand 2000; 71: 19-27. doi: 10.1080/00016470052943838.
- Paavolainen P, Pukkala E, Pulkkinen P, Visuri T. Causes of death after total hip arthroplasty: a nationwide cohort study with 24,638 patients. J Arthroplasty 2002; 17: 274-81. doi: 10.1054/arth.2002.30774.
- Chen Y C, Huang W C, Chang H K, Lirng J F, Wu J C. Long term outcomes and effects of surgery on degenerative spinal deformity: a 14-year national cohort study. J Clin Med 2019; 8. doi: 10.3390/jcm8040483.
Appendix
| Factor | LSSS before THA | Controls a | P value | LSSS after THA | Controls a | P value |
| 5-year follow-up | 2,028 | 149,113 | 3,723 | 18,235 | ||
| Reoperation b | 36 (2) | 1,781 (1) | 0.02 | 92 (2) | 397 (2) | 0.3 |
| 10-year follow-up | 751 | 83,546 | 2,728 | 12,549 | ||
| Reoperation b | 27 (4) | 2,603 (3) | 0.5 | 110 (4) | 496 (4) | 0.9 |
| LSSS = lumbar spinal stenosis surgery, THA = total hip arthroplasty. | ||||||
| a THA only. | ||||||
| b THA reoperation. | ||||||
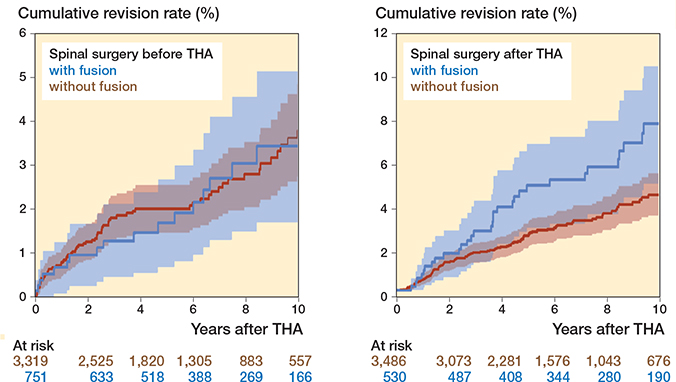
Figure 3. Kaplan–Meier curves of cumulative total hip arthroplasty (THA) reoperation rates, counted once per individual. CI is presented as shadowed area.