Evaluation of simultaneous bilateral femoral distraction osteogenesis with antegrade intramedullary lengthening nails in achondroplasia with rhizomelic short stature: a retrospective study of 15 patients with a minimum follow-up of 2 years
Björn VOGT 1,2,a, Andrea LAUFER 1,2,a, Georg GOSHEGER 2, Gregor TOPOROWSKI 1,2, Carina ANTFANG 1,2, Jan Duedal RÖLFING 3, Robert RÖDL 1,2, and Adrien FROMMER 1,2
1 Pediatric Orthopedics, Deformity Reconstruction and Foot Surgery, Muenster University Hospital, Muenster, Germany; 2 General Orthopedics and Tumor Orthopedics, Muenster University Hospital, Muenster, Germany; 3 Children’s Orthopedics and Reconstruction, Aarhus University Hospital, Aarhus, Denmark
a Shared first authorship
Background and purpose — Bilateral femoral distraction osteogenesis in patients with achondroplasia is insufficiently reported. We aimed to perform the first study that exclusively analyzed simultaneous bilateral femoral distraction osteogenesis with motorized intramedullary lengthening nails via an antegrade approach in patients with achondroplasia focused on reliability, accuracy, precision, and the evolving complications.
Patients and methods — In this retrospective singlecenter study we analyzed patients with achondroplasia who underwent simultaneous bilateral femoral lengthening with antegrade intramedullary lengthening nails between October 2014 and April 2019. 15 patients (30 femoral segments) of median age 14 years (interquartile range [IQR] 12–15) were available for analysis. The median follow-up was 29 months (IQR 27–37) after nail implantation.
Results — The median distraction length per segment was 49 mm (IQR 47–51) with a median distraction index of 1.0 mm/day (IQR 0.9–1.0), and a median consolidation index of 20 days/cm (IQR 17–23). Reliability of the lengthening nails was 97% and their calculated accuracy and precision were 96% and 95%, respectively. The most common complication was temporary restriction of knee range of motion during distraction in 10 of 30 of the lengthened segments. 1 patient was treated with 2 unplanned additional surgeries due to premature consolidation.
Conclusion — The method is reliable and accurate with few complications.
Citation: Acta Orthopaedica 2024; 95: 47–54. DOI: https://doi.org/10.2340/17453674.2024.35226.
Copyright: © 2024 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-03-10. Accepted: 2023-11-07. Published: 2024-01-30.
Correspondence: bjoern.vogt@ukmuenster.de
BV, AL, and AF contributed to acquisition, analysis, and interpretation of data, drafting of the paper, approval of the submitted, and final version. GG, GT, CA, JDR, and RR contributed to research design, interpretation of data, and revising the paper and approval of the submitted and final versions. All authors have read and approved the final submitted manuscript. BV and AL contributed equally to this work.
The authors would like to thank the patients and their families for their support of this work and acknowledge the physicians, nurses, and support staff who contributed to the treatment of the patients included in this study. The help of Maike Niemann and Dominik Turkowski for data acquisition is much appreciated. Julia Frommer and Lilian Vogt are thanked for their support. We acknowledge support from the Open Access Publication Fund of the University of Muenster.
Handling co-editors: Ivan Hvid and Robin Christensen
Acta thanks Joachim Horn and Søren Kold for help with peer review of this manuscript.
Achondroplasia with rhizomelic shortening of the limbs is the most common dwarfing disorder in humans, with an estimated prevalence of 3–5 per 100,000 births [1,2]. Lower limb lengthening to increase average adult height and minimize functional impairment during daily living is controversially discussed [3-5]. If patients and their families desire limb lengthening, a thorough evaluation together with all involved parties should be conducted to discuss the possible benefits and short- and long-term complications of such treatment. If significant height gain is strongly desired, repeated limb lengthening involving bilateral lower leg and femoral lengthening might be performed [6-8]. Lengthening can be conducted with either external fixators or intramedullary lengthening nails [6,9,10]. Distraction osteogenesis with intramedullary lengthening nails provides an equally safe, but more comfortable option compared with treatment with external fixators, avoiding complications such as pin site infection or soft tissue tethering [11-13]. However, due to relatively small dimensions and open growth plates of the respective bone, lengthening procedures in children are commonly performed with external fixators [6,10]. Nonetheless, previous studies have shown that femoral lengthening with intramedullary lengthening nails implanted via an antegrade approach can be applied in children starting at the age of 8 years [14-16].
Earlier studies on intramedullary lengthening nails are heterogeneous in terms of underlying etiologies, approaches employed, and implants [16-19].
We aimed to analyze simultaneous bilateral femoral distraction osteogenesis with motorized intramedullary lengthening nails via an antegrade approach in patients with achondroplasia. Reliability, accuracy, precision, and the evolving complications of treatment were evaluated to increase knowledge concerning the treatment and to improve patient counseling.
Patients and methods
Study design and setting
The longitudinally maintained database of our orthopedic teaching hospital was analyzed retrospectively to identify patients with rhizomelic short stature who underwent distraction osteogenesis between 2014 and 2019. Those who underwent simultaneous bilateral femoral distraction osteogenesis with magnetically driven motorized antegrade femoral lengthening nails were eligible for this study. Patients with a distal femoral deformity were treated via a retrograde femoral nail approach or with external fixator and were not included in this study. Intramedullary lengthening nails were not considered for patients with deep tissue infection, bone dimensions too small in relation to the available implants, and patients under the age of 8 years. No patient was excluded or lost before the minimum follow-up of 2 years. The study findings are reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (Figure 1) [20]. We would like to underline that all patients included in this study had a strong desire for this treatment to be performed and that lengthening surgery was not recommended during pediatric orthopedic consultation.
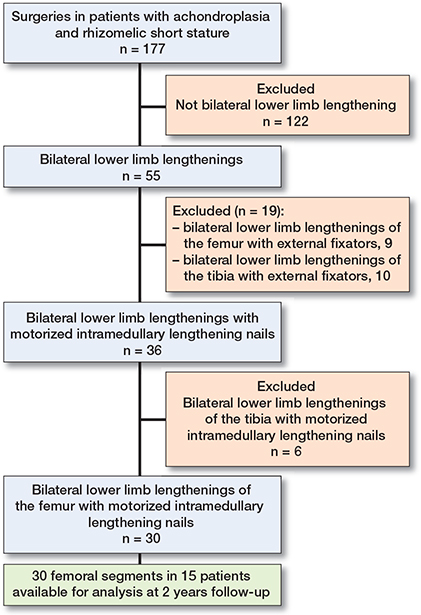
Figure 1. Patient flow diagram detailing the inclusion and exclusion criteria of the study.
Patients
15 patients with rhizomelic short stature (9 females, 30 femoral segments) with a median age of 14 years (interquartile range [IQR] 12–15) were available for analysis. At the time of surgery, the youngest patient was 10 and the oldest was 19 years old. In 11 patients lengthening of the femur with an intramedullary lengthening nail was the last part of a treatment concept for extensive lower limb lengthening to achieve a total length gain of 20–30 cm [8]. This is usually achieved by, first, simultaneous bilateral lengthening of the femur by 5–8 cm with a unilateral monorail external fixator (Limb Reconstruction System [LRS], Orthofix, Verona, Italy) at the age of 3–4 years and a second simultaneous bilateral lengthening of the tibia of 5–7 cm with a circular hexapod external fixator (Taylor Spatial Frame [TSF], Smith + Nephew, Watford, UK) before patients start their first year of school. Next, simultaneous bilateral lengthening of the tibia with a distraction goal of 5–7 cm is scheduled between the ages of 8 and 12 years and conducted with a circular hexapod external fixator. The last simultaneous bilateral lengthening is then planned with an intermedullary lengthening nail inserted via an antegrade femoral entry (lateral trochanteric approach) once the size of the bone is suitable for the available implants. The timing of the last lengthening is left to the patients and families’ preferences depending on their individual situation, but not before the age of 8 years for girls and 10 years for boys. If patients decided in favor of humerus lengthening due to functional impairment regarding daily activity and perineal hygiene this was usually performed simultaneously bilaterally with a unilateral monorail external fixator between 6 and 10 years, aiming to achieve a lengthening of 8–10 cm.
Lengthening of the femur was conducted using an antegrade intramedullary lengthening nail without additional deformity correction. Of the studied cohort, 11 had undergone previous bilateral lengthening of the femur with a unilateral external fixator (median distraction: 60 mm [IQR 60–65]) and 2 consecutive bilateral lengthening procedures of the tibia with circular external fixators (first lengthening: median distraction 60 mm [IQR 60–65], second distraction: median distraction 60 mm [IQR 60–70]) (Table 1). Bilateral lengthening of the humerus with external monorail fixator was conducted in 10 patients with a median distraction of 79 mm (IQR 56–99) at the age of 9.0 (IQR 8–11) years.
| Factor | Lengthening | |||
| 1st | 2nd | 3rd | 4th | |
| Patients, n | 11 | 11 | 9 | 15 |
| Segments, n | 22 | 22 | 18 | 30 |
| Segment | Femur | Tibia | Tibia | Femur |
| Device | Unilateral | Hexapod | Hexapod | Intra- |
| external | external | external | medullary | |
| fixator | fixator | fixator | lengthening | |
| nail | ||||
| Age at treatment | 4.0 (3–5) | 5.0 (4–6) | 8.0 (6–9) | 14 (12–15) |
| Achieved distraction per segment, mm | 60 (60–65) | 60 (60–65) | 60 (60–70) | 49 (47–51) |
| Total gain of length a | / | / | / | 220 (88–238) |
| a per leg after serial lengthening in mm | ||||
The median follow-up duration of the studied cohort was 29 months (IQR 27–37). After successful completion of femoral lengthening with intramedullary lengthening nails all 15 patients had all implants retrieved after a median of 17 months (IQR 15–20).
Clinical and radiographic evaluation
Clinical and radiographic information were acquired from hospital records. Anteroposterior (AP) long standing radiographs and bilateral radiographs of the femur with adjacent joints of all patients were analyzed preoperatively and after consolidation. All measurements were conducted on calibrated radiographs using the PACS® system (GE Healthcare, Chicago, IL, USA) and the postprocessing software TraumaCad (Brainlab, Munich, Germany).
Preoperative planning, surgical technique, and perioperative parameters
First, radiographs of all patients were analyzed preoperatively in order to assure that the bone dimensions were suitable for lengthening nail insertion (Table 2). A minimum femoral length of 19 cm (measured from the tip of the greater trochanter to the distal femoral growth plate) and a minimum outer cortical bone diameter of 16.5 mm, calculated by adding 2 mm of additional reaming to the diameter of 8.5 mm of the smallest available nail while leaving a cortical thickness of 3 mm on each side, was required to insert a lengthening nail with minimum lengthening capacity (stroke) of 50 mm (Tables 2 and 3). When planning the osteotomy site, a minimum of 4 cm of the female (thicker) part of the nail should remain in the distal fragment after full distraction to not compromise stability. Therefore, a rather proximal osteotomy should be chosen, whilst still preserving a sufficiently long proximal bone segment to permit stable fixation (Table 2). All femoral lengthening procedures were conducted with the magnetically driven motorized second-generation PRECICE P2 limb lengthening system (NuVasive Specialized Orthopedics, Inc, San Diego, CA, USA). The TraumaCad software was used for preoperative planning to ensure that the bone length and diameter were feasible for nail insertion and that the telescopic junction remains within the intramedullary canal of the distal fragment even after distraction.
| Nail length: 190 / 215 / 245 mm | 8 / 10 / 12 |
| Nail diameter: 8.5 / 10.7 mm | 26 / 4 |
| Nail stroke: a 50 / 80 mm | 18 / 12 |
| Proximal locking: 1 bolt / 2 bolts | 10 / 20 |
| Distal locking: AP or lateral / 2 lateral | 11 / 19 |
| a Distraction potential of the lengthening nail. AP = anteroposterior | |
For lengthening nail implantation patients were placed in a supine position using a minimally invasive antegrade technique as previously described [18]. All nails were inserted via a trochanteric entry established at the very tip of the trochanter [14,15] and without concomitant soft tissue release. All implanted nails had 2 locking options in the proximal and 3 in the distal part of the nail. Whenever anatomically possible, 2 proximal locking bolts were applied. In patients with an open trochanteric apophysis, a nail cap was used or the nail was positioned proximal enough to bridge the physeal defect caused by the approach. In this case, proximal locking was performed with only 1 bolt [18] (Table 3). Correct function of the implant was verified intraoperatively by means of an image intensifier after distraction of 1 mm of each nail.
Postoperative lengthening and follow-up protocol
The postoperative latency period was 7 days, and the initial distraction rate was set to 1 mm/day. Patients relied on wheelchair mobility during the distraction and consolidation period as the bilaterally applied implants do not enable full weightbearing. Physiotherapy at least once per week under professional supervision and additional self-exercises on a daily basis were recommended so that distraction could be conducted without external bracing. Patients were followed up every second week during distraction in the outpatient clinic including biplanar radiographs of the lengthened segments. According to our established protocols [18], once the lengthening goal was achieved, a consolidation period of 6 weeks was initiated. Full weight-bearing was allowed after consolidation of at least 3 of 4 cortices was confirmed on biplanar radiographs. Implant removal was routinely scheduled 1 year after consolidation (Figure 2).
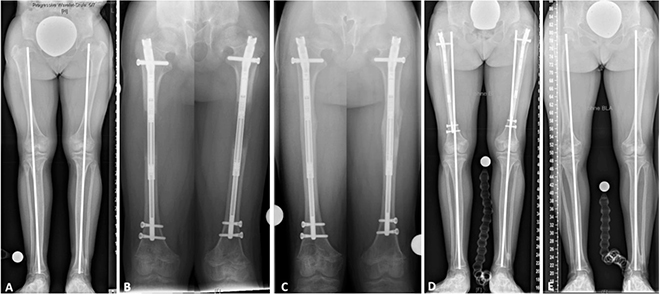
Figure 2. Bilateral femoral distraction osteogenesis with intramedullary lengthening nails
- Preoperative anteroposterior (AP) long standing radiograph of a 10-year-old girl with disproportionate short stature due to achondroplasia.
- Anteroposterior radiographs of the right and left femur during bilateral distraction with intramedullary lengthening nails. Proximal locking was performed with one locking bolt per segment and the nail remained proximal enough to bridge the entry-related defect of the apophysis.
- Bilateral osseous consolidation after having achieved the planned distraction of 5 cm per segment.
- Anteroposterior long standing radiograph at consolidation 3 months postoperatively.
- After implant removal 20 months postoperatively. Due to a slightly different radiographic exposure and posture of the patient the mechanical axis does not appear identical between D and E.
Outcome parameters
The goal of the study was to evaluate disease-specific outcomes and complication rates. Reliability, accuracy, precision, consolidation index, and distraction index were calculated as previously described (Accuracy = (100 – [(achieved distraction in mm – planned distraction in mm) / (planned distraction in mm) x 100]; Precision = 100 – (relative SD of accuracy)) [18]. The length of the femur was determined by measuring the distance from the tip of the greater trochanter to the distal femoral joint line. On the first postoperative radiograph the level of osteotomy (distance from the tip of the greater trochanter to the osteotomy site) was measured. The achieved distraction was determined by an implant-calibrated technique [18]. Lower limb alignment was assessed by measuring the mechanical axis deviation (MAD), the joint line convergence angle (JLCA) and mechanical joint orientation angles of the proximal and distal femur (lateral proximal femoral angle [LPFA] and mechanical lateral distal femoral angle [mLDFA]) according to established methods [21]. All available bilateral radiographs of the hip joint were screened for signs of avascular necrosis.
Complications
Complications were summarized descriptively and characterized as minor complications (events that resolved without additional surgery) and major complications (resulting in unplanned additional surgery, refracture of the regenerate bone, or permanent sequelae) [18]. Pain during lengthening was subclassified according to the required type and frequency of analgesics: no usage of analgesics, pain relief with oral nonsteroidal anti-inflammatory drugs (NSAIDs), or NSAIDs with oral opioid analgesics. Limitations in the range of motion (ROM) were classified as temporary during lengthening and persistent after the end of distraction.
Statistics
Normal distribution was assessed by the Shapiro–Wilk test. Descriptive statistics were performed reporting median values with IQR for continuous variables, and numbers with percentages for binary variables. Median values were compared using the Wilcoxon signed rank test. The level of significance was set at an α value of < 0.05. All statistical tests were conducted using SPSS 27 (IBM Corp, Armonk, NY, USA).
Ethics, funding, data sharing, and disclosures
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the University of Muenster, Germany (registration number: 2019-368-f-S). Written informed consent was obtained from the parents or legal guardians, and all children included in the study gave their verbal assent. Consent to publish was obtained from the parents or legal guardians of those children whose individual data was presented in the article. The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. No external source of funding was used. 3 authors (BV, JDR, and RR) certify receipt of personal payments or benefits, during the study period, in an amount of less than US$ 10,000 from NuVasive Specialized Orthopedics, San Diego, USA. All other authors have no relevant financial or non-financial interests to disclose. Complete disclosure of interest forms according to ICMJE are available on the article page, doi: 10.2340/17453674.2024.35226
Results
Patients were hospitalized for a median of 3 days (IQR 3–8). Surgery parameters and implant type information were acquired from the surgical records. For lengthening nail insertion, a median of 77 minutes per segment (IQR 61–91) with a median fluoroscopy time of 1.5 minutes (IQR 0.7–2.7) and a median blood loss of 0 mL (IQR 0–100) was documented. For lengthening nail removal, a median of 55 minutes per segment (IQR 44–95) with a median fluoroscopy time of 1.0 minute (IQR 0.6–1.3) and a median blood loss of 0 ml (IQR 0–50) was recorded.
Lengthening parameters
Reliability was 97%, as 29/30 lengthening procedures were completed with the initially implanted lengthening nail remaining in situ. One patient required an exchange of the implant during distraction. Implant dysfunction most likely caused premature consolidation. The implant was handed to the patient and no further analysis of the implant was conducted (Table 4).
The median difference between the median preoperatively planned distraction length of 50 mm (IQR 50–50) and the median achieved length of 49 mm (IQR 47–51) was 3 mm (IQR 1–3). The calculated accuracy and precision were 96% and 95%, respectively (Table 4). The median time under distraction was 51 days (IQR 46–65), with a median of 41 days (IQR 26–46) under consolidation. The median time from the date of surgery to full weight-bearing was 99 days (IQR 83–130). The median distraction index was 1.0 mm/day (IQR 0.9–1.0), and the median consolidation index was 20 days/cm (IQR 17–23) (Table 4). The median preoperative MAD was –5 mm (IQR –9 to 5) compared with a median postoperative MAD of –7 mm (IQR –16 to 3). The parameters of pre- and postoperative lower limb alignment and joint orientation are shown in Table 5 and Figure 3. In 3 of 30 operations, concomitant interventions were performed with the index operation: 2 scar excision from previous treatment with external fixator, 1 epiphysiodesis of the distal fibula. Blood transfusion was not necessary in any operation. The median osteotomy level was 81 mm (IQR 72–119) (Table 2).
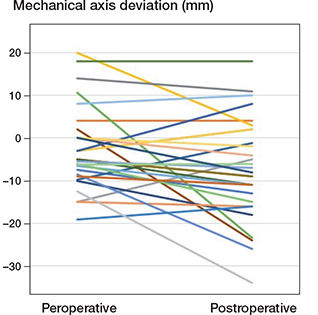
Figure 3. Pre- and postoperative change in the MAD. Spaghetti plot depicting the pre- and postoperative change in the MAD for each lengthened segment. While lengthening resulted in a postoperative MAD > –20 mm in 4 segments, no clear trend towards clinically significant valgus malalignment was observed in the entire cohort.
Complications of treatment
No intraoperative complications occurred during nail implantation or removal. No nail or locking bolt breakage was observed during the study period. No radiographic signs of entry-related avascular necrosis of the femoral head were observed. The median follow-up time between implant removal and subsequent radiographs was 13 months (IQR 6–20). In 5 patients the last radiograph was taken intraoperatively to prove full nail removal. Since then, these patients had only clinical follow-up; these 5 patients had a total follow-up after index surgery of 24, 27, 28, 31, and 37 months respectively and no clinical signs of avascular necrosis of the femoral head. The most common minor complication was temporary restriction of knee ROM during distraction, which occurred in 10 of 30 lengthened limbs, while temporary hip joint limitations were observed in 3 of 30. ROM was restored by intensified physiotherapeutic treatment in all patients. Acceleration of the distraction rate to avoid premature consolidation was required in 5 of 30 segments. Under distraction, 5 patients reported mild tenderness of the distraction site but did not require analgesics while 3 relied on oral NSAIDs to achieve a satisfactory analgesic level. 2 patients achieved a satisfactory analgesic level only by combining oral NSAIDs with oral opioid analgesics.
A major complication was observed in 1 of all lengthened segments. A unilateral premature consolidation of the distraction site was observed 7 weeks postoperatively and this was treated by removal of the distal locking bolts, percutaneous re-corticotomy, and application of torsional stress to the osteotomy site. Intraoperative in situ testing of the nail by distraction of 1 mm proved adequate functioning. However, 2 weeks later biplanar radiographs revealed insufficient distraction, thus the patient was treated by more extensive revision surgery: nail explanation, percutaneous re-osteotomy, application of multidirectional stress to the osteotomy site, spreading of the osteotomy site with a bone spreader, and insertion of a new lengthening nail. Thereafter the planned distraction goal of 7 cm and consolidation was achieved without any further peculiarities.
Complications related to bacterial osteomyelitis, neurovascular damage, joint subluxation, or insufficient bone healing were not observed in the studied cohort.
Discussion
Our study showed that motorized magnetically driven intramedullary lengthening nails can reliably and accurately be employed for simultaneous bilateral femoral lengthening with insertion via an antegrade approach in patients with disproportionate short stature in achondroplasia.
Previous studies have shown promising results of distraction osteogenesis ranging from 33–54 mm per segment in patients who were 7–18 years old [14-16] and evaluation of bilateral lower limb distraction osteogenesis in achondroplasia provided valuable results [6,8,10]. However, to our knowledge, no study has yet solely assessed the application of intramedullary lengthening nails for simultaneous bilateral femoral lengthening in this condition.
It remains difficult to compare the assessed limb lengthening parameters of this study with pre-existing data. Previous studies reported only results of lengthening in patients with achondroplasia conducted with external fixators [4,9,10], or a combination of external fixation and/or lengthening nails [6]. Other studies that reported the outcome of intramedullary femoral lengthening include heterogeneous patient populations [12,14,17-19]. In consideration of these limitations regarding comparability, the observed reliability of 97%, accuracy of 96%, and precision of 95% were similar but slightly above the average of previous studies. Nasto et al. reported an accuracy of 91% compared with Szymczuk et al. and Iliadis et al., who found an accuracy of 95% and 96%, respectively [17,22,23]. In accordance with previous results of our study group, intramedullary lengthening devices seem to be feasible for accurate and precise distraction osteogenesis [18,24]. In this study, the median distraction index was 1.0 mm/day (IQR 0.9–1.0). Previous studies have found similar distraction indices ranging from 0.7 to 0.9 mm/day [17,18,23,25]. Interestingly, the median consolidation index in this study of 20 days/cm (IQR 17–23) was lower than in most precedent studies. Horn et al. (1 month/cm), Szymczuk et al. (35 days/cm), Calder et al. (29 days/cm), Frommer et al. (31 days/cm), Fragomen et al. (1 month/cm), and Radler et al. (63 days/cm) reported consolidation indices ranging from 28 to 63 days/cm [12,16,18,19,23,26]. This could indicate that callus formation and consolidation in patients with achondroplasia occurs at slightly higher rates than in lengthening procedures performed due to other etiologies. As patients relied on wheelchair mobility during lengthening one might assume that, based on the principles described by Ilizarov, the lack of weight-bearing negatively influences the consolidation index [27]. However, the results of our study do not support this theory. The opposite seems to apply, because an acceleration of the distraction rate to avoid premature consolidation was required in 5 lengthened segments, premature consolidation was observed in 1 patient, and no non-union was detected in the studied cohort. In addition, the relatively young median age of this study cohort might have been susceptible to fewer complications than older and less healthy patients. However, a recently published study comparing the treatment outcome and complications of motorized intramedullary nail lengthening in different age groups showed no difference between the older population and the younger cohort [28]. In order to avoid complications during lengthening in relatively young patients with achondroplasia one should be aware of the technical peculiarities of preoperative planning as described in the methods section. 2 recent studies evaluated lower limb lengthening in relatively large cohorts of patients with achondroplasia (n = 50 and n = 66 patients) [6,10]. Lengthening with intramedullary nails was conducted in only a small proportion of patients and the parameters’ accuracy and precision were not provided by the authors [6]. Comparing these parameters with those of our own patient cohort was thus not feasible. Nevertheless, while Paley did not report on lengthening or consolidation indices, Shabtai et al. found a femoral consolidation index of 1 month/cm after lengthening with external fixators, similar to the aforementioned consolidation indices after intramedullary femoral lengthening [6,10].
Complications
Major complications with permanent sequelae were not observed in our patient cohort. The most severe complications were 2 re-osteotomies and exchange of a lengthening nail in 1 segment of the same patient. This complication was most likely due to implant malfunction of unclear origin. However, this is speculative as the device did not undergo further technical analysis. The observed rate of unplanned additional surgery in the studied cohort of 3% is considerably lower than in previous publications [12,16,18,19,23,26]. This could indicate that bilateral femoral distraction osteogenesis with an antegrade intramedullary lengthening nail in patients with achondroplasia bears fewer risks compared with patients treated for leg length discrepancy or short stature due to other etiologies. In particular, severe complications such as joint dislocation or neurovascular damage appear less likely to occur in achondroplasia, presumably due to the relative excess soft tissue conditions [29]. However, this conclusion is limited by the small patient cohort.
Limitations
This study is mainly biased by 2 factors: (1) selection bias versus other treatments, i.e. external fixators and nonoperative treatment, which were used during the same span of time for similar indications, are not reported in this study; (2) although this is presumably the largest patient cohort that has solely been evaluated for this special indication, the number of included patients is still relatively small. Although the minimum follow-up in this study is 2 years after nail insertion, even if rare, complications after implant removal might occur [30]. It should also be emphasized that there is a lack of knowledge concerning long-term side effects of excessive limb lengthening, such as secondary arthritis in adjacent joints of the lengthened segment.
One should consider assessment bias, which is sustained by the following main factors: patient-reported outcomes were not used; ROM was retrospectively acquired from hospital records and could be biased by inconsistency between the examining physician and documentation. Patients relied on wheelchair mobility during lengthening, which possibly delayed their return to work or school and thus reduced functionality and quality of life during the distraction period. Unfortunately, due to the retrospective study design, this study cannot provide reliable information regarding functionality and quality of life during treatment. Furthermore, we would like to point out that changes in the MAD were observed in the study cohort but a clear trend towards valgus malalignment related to lengthening along the anatomical axis of the femur was not found. One might assume that ligamentous laxity of the knee joint, which is a common characteristic of patients with achondroplasia and asymmetric weight-bearing, might have limited comparability of the assessed long standing radiographs [31]. However, this hypothesis could not be confirmed by comparing the pre- and postoperative JLCA, which did not show large variability. A different study design is needed to evaluate the intraindividual reliability of MAD measurements in long standing radiographs of patients with achondroplasia.
Conclusion
In patients with achondroplasia, simultaneous bilateral femoral distraction osteogenesis with motorized magnetically driven antegrade intramedullary lengthening nails seems to be a reliable and accurate treatment with few complications.
Perspective
We argue in favor of close clinical and radiographic follow-ups to detect and treat common complications such as joint stiffness and premature consolidation in a timely fashion. Limb lengthening in patients with achondroplasia is a treatment that addresses only one characteristic of this complex condition. Possible long-term side effects of lengthening and its physical and psychosocial impact remain unclear. Thorough counselling should prioritize limb deformities and follow-up of possible spine complications and lengthening ought only to be an option if explicitly requested by patients and families.
- Foreman P K, van Kessel F, van Hoorn R, van den Bosch J, Shediac R, Landis S. Birth prevalence of achondroplasia: a systematic literature review and meta-analysis. Am J Med Genet A 2020; 182: 2297-316. doi: 10.1002/ajmg.a.61787.
- Coi A, Santoro M, Garne E, Pierini A, Addor M C, Alessandri J L, et al. Epidemiology of achondroplasia: a population-based study in Europe. Am J Med Genet A 2019; 179: 1791-8. doi: 10.1002/ajmg.a.61289.
- Lavini F, Renzi-Brivio L, de Bastiani G. Psychologic, vascular, and physiologic aspects of lower limb lengthening in achondroplastics. Clin Orthop Relat Res 1990: 138-42.
- Kim S J, Balce G C, Agashe M V, Song S H, Song H R. Is bilateral lower limb lengthening appropriate for achondroplasia?: midterm analysis of the complications and quality of life. Clin Orthop Relat Res 2012; 470: 616-21. doi: 10.1007/s11999-011-1983-y.
- Lee R C, Aulisio M, Liu R W. Exploring the Ethics of stature lengthening as treatment for height dysphoria. Strategies Trauma Limb Reconstr 2020; 15: 163-8. doi: 10.5005/jp-journals-10080-1502.
- Paley D. Extensive limb lengthening for achondroplasia and hypochondroplasia. Children (Basel) 2021; 8. doi: 10.3390/children8070540.
- Peretti G, Memeo A, Paronzini A, Marzorati S. Staged lengthening in the prevention of dwarfism in achondroplastic children: a preliminary report. J Pediatr Orthop B 1995; 4: 58-64. doi: 10.1097/01202412-199504010-00009.
- Schiedel F, Rodl R. Lower limb lengthening in patients with disproportionate short stature with achondroplasia: a systematic review of the last 20 years. Disabil Rehabil 2012; 34: 982-7. doi: 10.3109/09638288.2011.631677.
- Venkatesh K P, Modi H N, Devmurari K, Yoon J Y, Anupama B R, Song H R. Femoral lengthening in achondroplasia: magnitude of lengthening in relation to patterns of callus, stiffness of adjacent joints and fracture. J Bone Joint Surg Br 2009; 91: 1612-17. doi: 10.1302/0301-620X.91B12.22418.
- Shabtai L, Jauregui J J, Herzenberg J E, Gesheff M G, Standard S C, McClure P K. Simultaneous bilateral femoral and tibial lengthening in achondroplasia. Children (Basel) 2021; 8. doi: 10.3390/children8090749.
- Hafez M, Nicolaou N, Offiah A, Giles S N, Madan S S, Fernandes J A. Femoral lengthening in children: a comparison between magnetic intramedullary lengthening nails and external fixators. J Pediatr Orthop 2021; 10.1097/BPO.0000000000002039. doi: 10.1097/BPO.0000000000002039.
- Calder P R, McKay J E, Timms A J, Roskrow T, Fugazzotto S, Edel P, et al. Femoral lengthening using the Precice intramedullary limblengthening system: outcome comparison following antegrade and retrograde nails. Bone Joint J 2019; 101-B: 1168-76. doi: 10.1302/0301-620X.101B9.BJJ-2018-1271.R1.
- Laubscher M, Mitchell C, Timms A, Goodier D, Calder P. Outcomes following femoral lengthening: an initial comparison of the Precice intramedullary lengthening nail and the LRS external fixator monorail system. Bone Joint J 2016; 98-B: 1382-8. doi: 10.1302/0301-620X.98B10.36643.
- Hammouda A I, Jauregui J J, Gesheff M G, Standard S C, Herzenberg J E. Trochanteric entry for femoral lengthening nails in children: is it safe? J Pediatr Orthop 2017; 37: 258-64. doi: 10.1097/BPO.0000000000000636.
- Frommer A, Rodl R, Gosheger G, Vogt B. [Application of motorized intramedullary lengthening nails in skeletally immature patients: undications and limitations]. Unfallchirurg 2018; 121: 860-7. doi: 10.1007/s00113-018-0541-4.
- Radler C, Mindler G T, Stauffer A, Weiss C, Ganger R. Limb lengthening with Precice intramedullary lengthening nails in children and adolescents. J Pediatr Orthop 2022; 42: e192-e200. doi: 10.1097/BPO.0000000000002016.
- Iliadis A D, Palloni V, Wright J, Goodier D, Calder P. Pediatric lower limb lengthening using the PRECICE nail: our experience with 50 cases. J Pediatr Orthop 2021; 41: e44-e49. doi: 10.1097/BPO.0000000000001672.
- Frommer A, Roedl R, Gosheger G, Niemann M, Turkowski D, Toporowski G, et al. What are the potential benefits and risks of using magnetically driven antegrade intramedullary lengthening nails for femoral lengthening to treat leg length discrepancy? Clin Orthop Relat Res 2022; 480: 790-803. doi: 10.1097/CORR.0000000000002036.
- Horn J, Hvid I, Huhnstock S, Breen A B, Steen H. Limb lengthening and deformity correction with externally controlled motorized intramedullary nails: evaluation of 50 consecutive lengthenings. Acta Orthop 2019; 90: 81-7. doi: 10.1080/17453674.2018.1534321.
- von Elm E, Altman D G, Egger M, Pocock S J, Gotzsche P C, Vandenbroucke J P, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology 2007; 18: 800-4. doi: 10.1097/EDE.0b013e3181577654.
- Paley D. Normal lower limb alignment and joint orientation: principles of deformity correction. Berlin, Heidelberg: Springer; 2002. p. 1-18.
- Nasto L A, Coppa V, Riganti S, Ruzzini L, Manfrini M, Campanacci L, et al. Clinical results and complication rates of lower limb lengthening in paediatric patients using the PRECICE 2 intramedullary magnetic nail: a multicentre study. J Pediatr Orthop B 2020; 29: 611-17. doi: 10.1097/BPB.0000000000000651.
- Szymczuk V L, Hammouda A I, Gesheff M G, Standard S C, Herzenberg J E. Lengthening with monolateral external fixation versus magnetically motorized intramedullary nail in congenital femoral deficiency. J Pediatr Orthop 2019; 39: 458-65. doi: 10.1097/BPO.0000000000001047.
- Frommer A, Roedl R, Gosheger G, Hasselmann J, Fuest C, Toporowski G, et al. Focal osteolysis and corrosion at the junction of Precice Stryde intramedullary lengthening device: preliminary clinical, radiological, and metallurgic analysis of 57 lengthened segments. Bone Joint Res 2021; 10: 425-36. doi: 10.1302/2046-3758.107.BJR-2021-0146.R1.
- Masci G, Palmacci O, Vitiello R, Bonfiglio N, Bocchi MB, Cipolloni V, et al. Limb lengthening with PRECICE magnetic nail in pediatric patients: a systematic review. World J Orthop 2021; 12: 575-83. doi: 10.5312/wjo.v12.i8.575.
- Fragomen A T, Kurtz A M, Barclay J R, Nguyen J, Rozbruch S R. A comparison of femoral lengthening methods favors the magnetic internal lengthening nail when compared with lengthening over a nail. HSS J 2018; 14: 166-76. doi: 10.1007/s11420-017-9596-y.
- Ilizarov G A. [Basic principles of transosseous compression and distraction osteosynthesis]. Ortopediia travmatologiia i protezirovanie 1971; 32: 7-15.
- Powell K P, Hammouda A I, Hlukha L P, Rivera J C, Patel M, Rozbruch S R, et al. Motorized intramedullary nail lengthening in the older population. J Clin Med 2022; 11. doi: 10.3390/jcm11175242.
- Donaldson J, Aftab S, Bradish C. Achondroplasia and limb lengthening: results in a UK cohort and review of the literature. J Orthop 2015; 12: 31-4. doi: 10.1016/j.jor.2015.01.001.
- Frost M W, Kold S, Rahbek O, Bafor A, Duncan M, Iobst C A. Complications in elective removal of 271 bone lengthening nails (FITBONE, PRECICE and STRYDE). Strategies Trauma Limb Reconstr 2021; 16: 110-15. doi: 10.5005/jp-journals-10080-1529.
- Rozbruch S R, Hamdy R C. Limb lengthening and reconstruction surgery case atlas: adult deformity • tumor • upper extremity. Berlin: Springer International Publishing; 2015.