Activity-restriction only as treatment yields positive outcomes in pediatric spinal compression fractures: a prospective study of 47 patients at medium-term follow-up
Sofia BELOV 1,a, Petra GRAHN 2,a, Reetta KIVISAARI 3, Ilkka HELENIUS 1, and Matti AHONEN 2
1 Department of Orthopaedics and Traumatology, HUS Helsinki University Hospital, University of Helsinki, Helsinki; 2 Department of Pediatric Surgery, Orthopedics and Traumatology, New Children’s Hospital, HUS Helsinki University Hospital, University of Helsinki, Helsinki; 3 Department of Radiology, HUS Diagnostic Center, University of Helsinki and Helsinki University Hospital, Helsinki, Finland
a Shared first authorship
Background and purpose — We aimed to evaluate the clinical outcomes, radiographic results, and health-related quality of life in pediatric AO type A1 spinal compression fractures treated with activity-restriction only.
Patients and methods — All children between 2014 and 2020 with an AO type A1 spinal compression fracture treated with activity-restriction only identified from an institutional fracture registry were invited to a prospective outcomes study. Clinical findings and spinal radiographs were assessed at median 3 years, interquartile range (IQR) 1–4 follow-up from injury. Oswestry Disability Index, Pediatric Quality of Life Inventory Generic Core Scale (PedsQL), and PedsQL Pediatric Pain Questionnaire were compared with reference values. 63 children were identified, of whom 47 agreed to participate. 8 were polytrauma patients.
Results — Age at injury was median 11 (IQR 9–14) years. The number of injured vertebrae was median 2 (IQR 1–3). 82% (94 of 115) were thoracic vertebrae fractures and 70% (33 of 47) of the patients had thoracic vertebrae fractures only. At follow-up all but 2 fractures showed radiographic remodeling. There was no difference from the published reference values in the patient-reported outcome measures. A lower PedsQL physical functioning score was associated with higher patient-reported pain (P = 0.03). At follow-up 12 patients had hyperkyphosis (median difference from the reference values 4°, IQR 3–6, 95% confidence interval [CI] 3–6) and 5 hypolordosis (median difference from reference 8°, IQR 4–11, CI 4–14). None of the patients had surgery for deformity during follow-up.
Conclusion — Clinical, radiographic, and health-related quality of life outcomes were good after activity-restriction treatment in pediatric A1 spinal compression fractures.
Citation: Acta Orthopaedica 2024; 95: 8–13. DOI https://doi.org/10.2340/17453674.2024.35161.
Copyright: © 2024 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2023-06-20. Accepted: 2023-12-03. Published: 2024-01-18.
Correspondence: petra.grahn@hus.fi
Study design: MA, SB, PG, IH, RK. Collecting patient data and data analysis: MA, SB, PG. Writing the manuscript: MA, SB, G, I.H, RK. Radiological assessment: RK.
The authors would like to thank Mitja Lääperi, MSc, for biostatistical expertise in our study.
Handling co-editors: Paul Gerdhem and Philippe Wagner
Acta thanks Mohamed Aly and Johan von Heideken for help with peer review of this manuscript.
Spinal fractures account for 2–5% of all fractures observed in children and adolescents [1-3]. The reported incidence of all pediatric spinal fractures in Finland is 0.66 per 100,000 [2]; however, the incidence of pediatric spinal compression fractures is unknown. The fractures are equally distributed between the sexes with a peak incidence at 12 years and typically affect the thoracolumbar region following a low-energy fall [1-4]. Younger children tend to fracture the lower thoracic spine, whereas in adolescents the thoracolumbar region is more often affected [3]. Recovery from pediatric spinal fractures is perceived as good [5,6]. Recovery may be attributed to the better circulatory properties of the vertebral discs and cartilage as well as apophyseal growth plates providing remodeling [1,6,7]. The more robust structure of the vertebral endplate also makes the pediatric spine stronger to withstand deforming forces in comparison with the adult [7].
Spinal compression fractures are generally stable and treated non-surgically [1-6]. However, there is no consensus among pediatric orthopedic surgeons regarding the optimal treatment strategy and little is known about the natural history [5]. Immediate mobilization with thoracolumbosacral orthosis (TLSO) is a common treatment option with treatment duration ranging from 4 to 8 weeks [4]. Strong evidence supporting this treatment modality is lacking [6]. Other treatment options include bed rest with or without TLSO or activity-restriction including cessation of sports and excess physical activity for 12 weeks [5,6,8].
At Helsinki University Hospital (HUS) New Children’s Hospital pediatric compression fractures have been treated with restraint from excess physical activity and return to sports at 3 months from injury.
We aimed to evaluate the clinical outcomes, radiographic results, and health-related quality of life in pediatric AO type A1 spinal compression fractures treated with activity-restriction only.
Patients and methods
HUS New Children’s Hospital is a primary care center for pediatric trauma treating children ≤ 16 years of age. We conducted a study based on prospectively collected data from all patients identified from the institutional fracture registry (Kids Fracture Tool, BCB Medical, Turku, Finland). The STROBE guidelines were followed (https://www.strobe-statement.org/). Our prospective fracture registry collects data regarding the injury and its treatment (age of patient at time of injury, mechanism of injury, type of fracture, international classification of diseases 10th revision [ICD-10] code, treatment of fracture, complications of treatment, number of follow-up visits). Our treatment protocol for spinal compression fractures is restraint from sports with follow-up radiographs (anteroposterior and lateral view) taken 1–2 weeks from injury. If no progression of compression is observed children are allowed to return to sports 12 weeks from injury.
Data collection
The follow-up (FU) evaluation included neurologic examination of the lower limbs, evaluation of spinal mobility using the modified Schober’s test, and measurement of rib hump using a scoliometer in a forward bending test [9,10]. In addition, all participants were asked to complete patient-reported outcome measures (PROM), Oswestry Disability Index (ODI), Pediatric Quality of Life Inventory (PedsQL) Generic Core Scale (PedsQL), and PesdQL Pediatric Pain Questionnaire (PedsQL Pain); 1 declined. The ODI and the PedsQL Pain scores are calculated from 0–100 with 0 indicating no disability/pain and 100 indicating the highest level of disability/pain [11-13]. The PedsQL total score as well as its subscore of physical health is similarly calculated from 0 to 100 with a higher score representing a better outcome [14]. Section 8 (question about sex life) was removed from the ODI questionnaire used in the study.
Radiographic evaluation (Figure 1)
All radiographs were assessed by a musculoskeletal radiologist with over 10 years’ experience of pediatric trauma for initial fracture classification (Genant grade) and progression or correction of initial deformity. The Genant classification grades spinal compression fractures from 0 to 3 based on the vertebral shape, with respect to vertebral height loss involving the anterior, posterior, and/or middle vertebral body with a higher grade indicative of a more severe compression [15]. The degree of vertebral body compression was measured as the ratio between the anterior height and the posterior height of the fractured vertebrae from the lateral radiograph (Figure 1) [5,6]. Thoracic kyphosis (T2–T12) and lumbar lordosis (T12–L5) were measured using Cobb’s method [16]. Hypolordosis (T12–L5) was defined as < 35° at the age of < 12 years and < 40° at the age of 12–16 years. Hyperkyphosis (T2–T12) as >38° at the age of <12 years and >39° at age of 12–16 years [17].
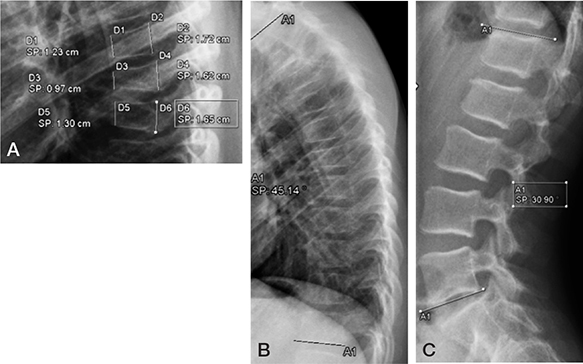
Figure 1. A. Compression was calculated as the ratio between the anterior and posterior height of the vertebrae.
B. Thoracic kyphosis was measured from the superior endplate of the T2 vertebra to the lower endplate of the T12 vertebra.
C. Lumbar lordosis was measured from the superior endplate of the T12 vertebra to the lower endplate of the L5 vertebra.
Statistics
We describe the data using the median and the interquartile range (IQR) for continuous variables and as counts and percentages for categorical data. The comparisons have been done using the Mann–Whitney U test for the continuous variables (PROMs, modified Schober, scoliometer) and Fisher tests for the categorical data. Due to our small sample size, we calculated the 95% confidence intervals (CI) for the medians using bootstrapping. We used a 1,000 bootstrap sample to calculate the CI using percentiles. Statistical analysis was carried out using R 4.2.3 (R Foundation for Statistical Computing, Vienna, Austria) and SPSS (SPSS Statistics 29 v100; IBM Corp, Armonk, NY, USA). An external biostatistician was consulted.
Ethics and disclosures
Written informed consent was gathered from guardians and participants. The study protocol was approved by HUS Regional Committee on Medical Research Ethics (approval number: HUS-1902-2020). The authors report no conflict of interest. Complete disclosure of interest forms according to ICMJE are available on the article page, doi: 10.2340/17453674.2024.35161
Results
Patients and recruitment
Between 2014 and 2020, 83 patients treated for a spinal fracture in the thoracolumbar region (ICD-10 search codes: S22.0, S22.1, S32.0, and S32.7) were identified from the registry. A spinal compression fracture was defined as a vertebral body fracture with one or both endplates involved but the fractures not connecting with one another (AO type A1, https://surgeryreference.aofoundation.org/). A musculoskeletal radiologist re-evaluated the initial radiographs of all 83 patients; 72 fulfilled the radiographic criteria. Of the 72 patients, 7 were excluded due to pre-existing risk of fractures and 2 due to TLSO treatment started elsewhere. Any concomitant injuries (polytrauma) were documented. Altogether 63 patients (38 male) were invited to participate in the study of whom 47 agreed (28 male) (Figure 2).
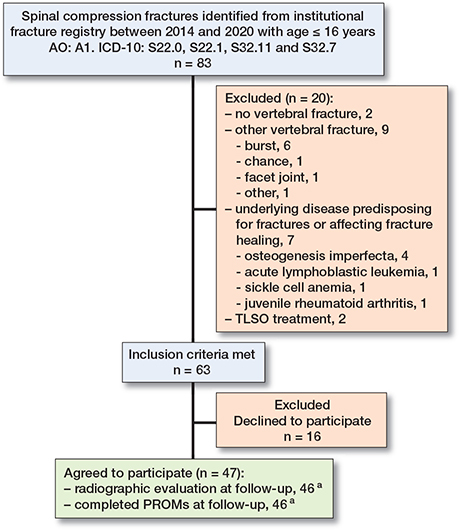
Figure 2. Flowchart of participants selection. a 1 patient declined radiographic evaluation at follow-up visit, and 1 other patient’s patient-reported outcome measures (PROMs) were excluded due to compliance issues. AO = https://surgeryreference.aofoundation.org/, ICD-10 = International Classification of Diseases 10th revision, TLSO = thoracolumbosacral orthosis.
Fractures and trauma
The participants were assessed at median 3 years (IQR 1–4) from injury. Altogether 115 compression fractures were identified in the 47 patients. The median age at injury was 11 years (IQR 9–14). 28 patients had 2 or more injured vertebrae. The median number of compression fractures in the participants was 2 (IQR 1–3). Th7 was the most often fractured vertebra (15%, 17/115), while Th1, Th10, and L5 were the least fractured (one each) (Figure 3). 82% of the fractures occurred in the thoracic spine (94/115) and 70% (33/47) of the patients had thoracic vertebrae fractures only (Table 1, Figure 3). Genant grade 0 (47%, 54/115) was the most common fracture grade followed by grade 2 (n = 30), grade 1 (n = 29), and grade 3 (n = 1). Most of the patients (39/47) had isolated spinal compression fractures. In this patient group the median number of fractures was 2 (IQR 1–3). 8 of the participants were polytrauma patients with a median of 3 (IQR 1–5) compression fractures, all sustained from a high-energy injury (fall from 8 meters 3, traffic injury 3, downhill fall with kick scooter 1, and equestrian injury 1). Only 1 of the polytrauma patients had a fracture requiring closed reduction and fixation (metacarpal). All other associated fractures were treated with either casting (metacarpal 2, metatarsal 2, and calcaneus 2), collar and cuff (clavicle 3 and scapula 1) or restriction of weight bearing (pelvis 2).
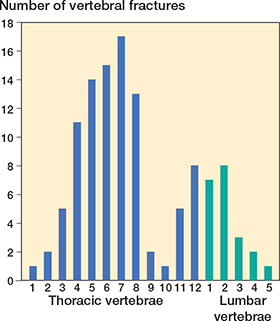
Figure 3. Distribution of the 115 vertebral fractures in the 47 study participants.
Clinical findings and PROMS
All had normal neurological findings of the lower limbs. Modified Schober’s test (median 7 cm, IQR 7–9, CI 7–8) yielded results within the normal range [10]. 5 patients had an increased rib hump as assessed by scoliometer (median 7°, IQR 6–7), while the median rib hump in the whole study population was 3° (IQR 2–5). The mean PROM results showed no disability in the ODI, normal quality of life in the PedsQL, and no pain in the PedsQL Pain scores (Table 2) [11,12,14]. There was no statistically significant difference between the polytrauma and isolated spinal compression fracture patients in the ODI (P = 0.8), or the PedsQL Pain scores (P = 0.9). Nor was there any difference in the PROMS between patients with fractures of the thoracic region and those with fractures in the lumbar spine (P > 0.05 for all).
| PROM type | All (n = 46) a | Isolated spinal fractures (n = 38) | Polytrauma (n = 8) | Thoracic fractures (n = 34) | Lumbar fractures (n = 12) |
| ODI | 0 (0–6) [0–3] | 0 (0–5) [0–4] | 1 (0–9) [0–9] | 0 (0–5) [0–3] | 0 (0–9) [0– 4] |
| PedsQL | 88 (81–96) [87–93] | 89 (85–98) [88–94] | 83 (77–88) [76–88] | 90 (88–91) [86–94] | 88 (83–95) [74–100] |
| PedsQL Function | 94 (87–98) [90–97] | 94 (88–100) [90–97] | 80 (73–91) [71–88] | 94 (83–100) [90–98] | 91 (86–99) [87–95] |
| PedsQL Pain | 1 (0–10) [0–3] | 1 (0–8) [0–3] | 0 (0–13) [0–13] | 0 (0–4) [0–8] | 0 (0–9) [0– 4] |
| The Oswestry Disability Index (ODI) and the Pediatric Quality of Life Inventory pain questionnaire (PedsQL Pain) are calculated from 0–100 with 0 indicating no disability/pain and 100 indicating the highest level of disability/pain. | |||||
| The PedsQL Generic core scale (PedsQL) and the physical health summary score (PedsQL Function) are calculated from 0 to 100 with a higher score representing a better outcome. | |||||
| a 1 patient’s patient-reported outcome measures were excluded due to compliance issues. | |||||
Polytrauma patients reported a lower total PedsQL score than patients with isolated compression fractures (P = 0.05) with a statistically significant difference in the PedsQL subscore of physical functioning (P < 0.01). A lower PedsQL physical functioning score was associated with higher patient-reported pain (P = 0.03).
Radiographic findings
Full spinal radiographs (lateral and anteroposterior views) were taken of 46 patients (1 declined) at the FU visit. 12 patients had a remaining hyperkyphosis with a median difference from the reference values of 4° (IQR 3–6, CI 3–6) and 5 hypolordosis with a difference from reference of 8° (IQR 4–11, CI 4–14). The difference between the anterior and posterior height of the fractured vertebrae decreased from an initial anterior–posterior height ratio of median 0.8 (IQR 0.7–0.8, CI 0.7–0.8) to a final 0.9 (IQR 0.8–1.0, CI 0.9–1.0), with delta of 0.12 (IQR 0.1–0.2, CI 0.1–0.2) P < 0.001. There was no difference between the initial compression ratio in the polytrauma patients (median 0.8, IQR 0.7–0.8, CI 0.7–0.8) and the spinal fracture only patients (median 0.8, IQR 0.7–0.8, CI 0.7–0.8, P = 0.7). Nor was there any difference in the remodeling between the 2 groups, with a final anterior–posterior ratio for the polytrauma of median 0.9, IQR 0.8–0.9, CI 0.8–1.0, and 0.9, IQR 0.8–1.0, CI 0.85–0.93 in the spinal fractures only group (P = 0.8). 44 patients (fractures) showed signs of remodeling and only 1 did not (age at fracture 7.5 years, FU 1 year), while 1 more showed progression of deformity (age at fracture 10.5 years, FU 6 years) (Figure 4). Both patients who did not show signs of remodeling had Genant grade 1 fractures. None of the patients in the study required surgery during the FU period.
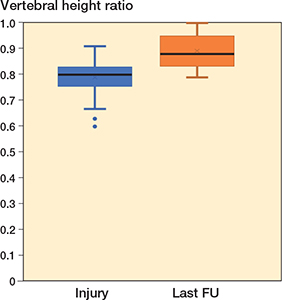
Figure 4. Box plot expressing the ratio between the anterior and posterior height of the vertebrae at the time of injury and at last follow-up (FU). Horizontal line represents the median, box the interquartile range (IQR), whiskers 1.5 x IQR and the dots outliers.
Discussion
We have analyzed the results of activity-restriction only as a treatment modality for pediatric spinal compression fractures (AO type A1), showing good results over mid-term follow-up in terms of radiographic outcomes and health-related quality of life.
Many centers treat spinal compression fractures in children with TLSO even though there is no strong evidence of its superiority as a treatment modality [1,4,6]. In a study of 74 patients with a pediatric spinal compression fracture by Singer et al. [6], half of the fractures were treated with TLSO and the other half by activity-restriction only. The authors found no difference in outcome and reported equal remodeling of the vertebrae in the 2 groups. Karlsson et al. [5] published longterm follow-up (mean 33 years, 21 patients) of pediatric spinal compression fractures using the ODI as an outcome measure. Similar to Singer et al. [6], they reported good remodeling of the fractures and in addition found no increased risk of disc degeneration in adulthood. The ODI score in their study was indicative of no disability (mean 2.3, SD 6.1) [5]. This study reports results in accordance with both aforementioned studies. In addition, general quality of life of the patients is good to excellent suggesting that activity-restriction only is an equal treatment modality to TLSO. As TLSO treatment can be perceived as demanding and more costly we suggest that routine immobilization is not necessary in this stable spinal fracture type in children and young individuals.
In the adult population treatment failure following nonoperative management of spinal compression fractures has been reported to be as high as 39%, mostly being attributed to the progression of deformity [18]. A recent review found that age, lumbar bone mineral density, segmental Cobb angle, and vertebral height loss all were individual risk factors for treatment failure [19]. Although 35% of our patients had a remaining mild deformity, we found no association with the reported health-related quality of life, nor did the deformity correlate with the patient-reported pain. The difference from the adult population most likely can be attributed to the higher metabolic activity of the bone and apophyseal growth plates of the pediatric spine as well as the ability of the intervertebral disc to absorb deforming forces, already leading initially to less severe compression [3,5,6]. In the current study most of our patients showed significant vertebral remodeling (P < 0.01), while only 1 patient showed progression of deformity. As the median follow-up is short (3 years) it is likely that the correction of deformity will further progress in most patients until cessation of growth [5]. Over the study period none of the patients required treatment for residual deformity, suggesting that radiographic follow-up after 1 to 2 weeks with standing radiographs probably is unnecessary.
Vertebral compression fractures may lead to a progressive kyphotic deformity and global sagittal imbalance, which are known independent predictors of negative quality of life [20,21]. In studies analyzing the impact of Scheuermann’s kyphosis on quality of life, pain has been found to be significantly worse in Scheuermann’s kyphosis patients with moderate hyperkyphosis already, than in controls [21]. In this study 11 patients had a remaining mild hyperkyphosis (< 6°) at follow-up with no association with reported pain or other PROMs, suggesting that a mild thoracic kyphotic deformity is well tolerated. Other studies have reported remodeling of kyphotic deformity following spinal compression fractures over time, with only a very small percentage (< 5%) showing progression of kyphotic angle [5]. In the current study all but 2 patients showed radiographic remodeling of the compressed vertebrae resulting in normal thoracic kyphosis and lumbar lordosis in the majority of our patients.
Limitations
First, our study has relatively short follow-up (median 2.5 years) and limited size of the study population, even though the follow-up rate was good (75%). Second, Genant’s classification was introduced for stable osteoporotic compression fractures in adults but has since been used in children to describe morphological fracture characteristics [15,22]. In the current study its value in predicting fracture remodeling remained limited. Third, the ODI questionnaire has been validated in children and adolescents to evaluate back pain, although it is considered to be less sensitive to identify disability in this population in comparison with adults [23]. With a lack of other suitable PROMs, as well as the use of the ODI in other studies evaluating back pain in children and youth, a choice was made to include this PROM [5,23,24]. Fourth, as nearly half of our patients still have the teenage growth spurt ahead of them, this may accelerate growth and have an influence on the mild residual deformities.
Conclusion
Clinical, radiographic, and health-related quality of life outcomes were good after activity-restriction treatment in pediatric A1 spinal compression fractures.
In perspective, routine immobilization does not seem necessary in the treatment of pediatric spinal compression fractures.
- Akbarnia B A. Pediatric spine fractures. Orthop Clin North Am 1999; 30(3): 521-36, x. doi: 10.1016/s0030-5898(05)70103-6.
- Puisto V, Kääriäinen S, Impinen A, Parkkila T, Vartiainen E, Jalanko T, et al. Incidence of spinal and spinal cord injuries and their surgical treatment in children and adolescents: a population-based study. Spine (Phila Pa 1976) 2010; 35(1): 104-7. doi: 10.1097/BRS.0b013e3181c64423.
- Saul D, Dresing K. Epidemiology of vertebral fractures in pediatric and adolescent patients. Pediatr Rep 2018; 10(1): 7232. doi: 10.4081/pr.2018.7232.
- Carreon L, Glassman S, Campbell M. Pediatric spine fractures: a review of 137 hospital admissions. J Spinal Disord Tech 2004; 17(6): 477-82. doi: 10.1097/01.bsd.0000132290.50455.99.
- Karlsson M, Moller A, Hasserius R, Besjakov J, Karlsson C, Ohlin. A modeling capacity of vertebral fractures exists during growth: an upto-47-year follow-up. Spine (Phila Pa 1976) 2003; 28(18): 2087-92. doi: 10.1097/01.BRS.0000084680.76654.B1.
- Singer G, Parzer S, Castellani C, Wegmann H, Lindbichler F, Till H, et al. The influence of brace immobilization on the remodeling potential of thoracolumbar impaction fractures in children and adolescents. Eur Spine J 2016; 25(2): 607-13. doi: 10.1007/s00586-015-4250-1.
- Boos N, Weissbach S, Rohrbach H, Weiler C, Spratt K, Nerlich A. Classification of age-related changes in lumbar intervertebral discs: 2002 Volvo Award in basic science. Spine (Phila Pa 1976) 2002; 27(23): 2631-44. doi: 10.1097/00007632-200212010-00002.
- Daniels A, Sobel A, Eberson C. Pediatric thoracolumbar spine trauma. J Am Acad Orthop Surg 2013; 21(12): 707-16. doi: 10.5435/JAAOS-21-12-707.
- Bunnell W. An objective criterion for scoliosis screening. J Bone Joint Surg Am 1984; 66(9): 1381-7.
- Macrae I F, Wright V. Measurement of back movement. Ann Rheum Dis 1969; 28: 584-9.
- Pekkanen L, Kautianen H, Ylinen J, Salo P, Häkkinen A. Reliability and validity study of the Finnish version 2.0 of the Oswestry Disability Index. Spine (Phila Pa 1976) 2011 Feb 15; 36(4): 332-8. doi: 10.1097/BRS.0b013e3181cdd702.
- Fairbank J C, Couper J, Davies J B, O’Brien J P. The Oswestry low back pain disability questionnaire. Physiotherapy 1980; 66: 271-3.
- Varni J, Thompson K, Hanson V. The Varni/Thompson pediatric pain questionnaire. I: Chronic musculoskeletal pain in juvenile rheumatoid arthritis. Pain 1987; 28(1): 27-38. doi: 10.1016/0304-3959(87)91056-6.
- Varni J, Seid M, Kurtin P. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care 2001; 39(8): 800-12. doi: 10.1097/00005650-200108000-00006.
- Genant H, Wu C, van Kuijk C, Newitt M. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 1993; 8(9): 1137-48. doi: 10.1002/jbmr.5650080915.
- Cobb J R. Outline for the study of scoliosis. American Academy of Orthopedic Surgeons Instructional Course Lectures, Vol. 5. Ann Arbor, MI: Edwards; 1948.
- Furlanetto T, Sedrez J, Candotti C, Loss J. Reference values for Cobb angles when evaluating the spine in the sagittal plane: a systematic review with meta-analysis. Motricidade 2018; 14(2-3): 115-28.
- Soultanis K, Thano A, Soucacos P. Outcome of thoracolumbar compression fractures following non-operative treatment. Injury 2021; 52(12): 3685-90. doi: 10.1016/j.injury.2021.05.019.
- Petitt J, Desai A, Kashkoush A, Ahorukomeye P, Potter T, Stout A, et al. Failure of conservatively managed traumatic vertebral compression fractures: a systematic review. World Neurosurg 2022; 165: 81-8. doi: 10.1016/j.wneu.2022.06.053.
- Lonner B, Yoo A, Terran J, Sponseller P, Samdani A, Betz R, et al. Effect of spinal deformity on adolescent quality of life: comparison of operative Scheuermann kyphosis, adolescent idiopathic scoliosis, and normal controls. Spine (Phila Pa 1976) 2013; 38(12): 1049-55. doi: 10.1097/BRS.0b013e3182893c01.
- Petcharaporn M, Pawelek J, Bastrom T, Lonner B, Newton P. The relationship between thoracic hyperkyphosis and the Scoliosis Research Society outcomes instrument. Spine (Phila Pa 1976) 2007; 32(20): 2226-31. doi: 10.1097/BRS.0b013e31814b1bef.
- Mäyränpää M, Helenius I, Valta H, Mäyränpää M, Toiviainen-Salo S, Mäkitie O. Bone densitometry in the diagnosis of vertebral fractures in children: accuracy of vertebral fracture assessment. Bone 2007; 41(3): 353-9. doi: 10.1016/j.bone.2007.05.012.
- Clifford S, Fritz J. Children and adolescents with low back pain: a descriptive study of physical examination and outcome measurement. J Orthop Sports Phys Ther 2003; 33(9): 513-22. doi: 10.2519/jospt.2003.33.9.513.
- MacDonald J, dʼHemecourt P, Micheli L. The reliability and validity of a pediatric back outcome measure. Clin J Sport Med 2016; 26(6): 490-6. doi: 10.1097/JSM.0000000000000282.