Previous surgery for instability is a risk factor for a worse patient-reported outcome after anatomical shoulder arthroplasty for osteoarthritis: a Danish nationwide cohort study of 3,743 arthroplasties
Jeppe V RASMUSSEN and Bo S OLSEN
Department of Orthopaedic Surgery, Herlev and Gentofte Hospital, and Department of Clinical Medicine, University of Copenhagen, Copenhagen, Denmark
Background and purpose — Although most patients have good outcomes after shoulder arthroplasty for osteoarthritis, certain risk factors may lead to disappointing outcomes. We assessed risk factors for a worse outcome after anatomical shoulder arthroplasty for osteoarthritis. Our hypothesis was that previous surgery for instability would be a risk factor for a worse outcome independent of age, sex, and arthroplasty type.
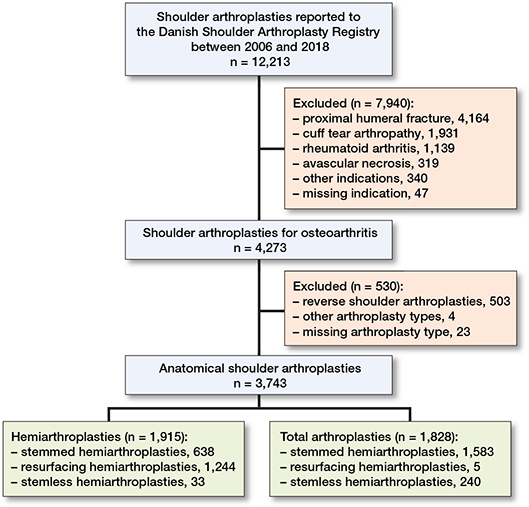
Patients and methods — We included arthroplasties reported to the Danish Shoulder Arthroplasty Registry between 2006 and 2018 (n = 3,743). The Western Ontario Osteoarthritis of the Shoulder (WOOS) index at 1 year was used as outcome. The total score was converted to a percentage of a maximum score. The general linear model was used to analyze differences in WOOS. Age, sex, arthroplasty type, and previous surgery were included in the multivariate model. Estimates were given with 95% confidence intervals (CI).
Results — The mean WOOS score was 78 for patients with no previous surgery and 55 for patients with surgery for instability. The mean difference was –16 (CI –10 to –22) in the multivariate model. Hemiarthroplasty had a worse outcome compared with total shoulder arthroplasty and young patients had a worse outcome compared with older patients. The mean differences in the multivariate model were –12 (CI –10 to –14) and –11 (CI –8 to –14) respectively.
Interpretation — Patients with previous surgery for instability had worse results independent of age, sex, and arthroplasty type and should be informed about their individual risk of a worse outcome.
Citation: Acta Orthopaedica 2022; 93: 588–592. DOI http://dx.doi.org/10.2340/17453674.2022.3419.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-01-25. Accepted: 2022-05-27. Published: 2022-06-21.
Correspondence: jeppe.vejlgaard.rasmussen@regionh.dk
JVR and BSO conceived the study idea and contributed to the design of the study. JVR collected the data and carried out the analysis and wrote the first draft of the manuscript. JVR and BSO participated in the discussion and interpretation of the results. BSO revised the manuscript for intellectual content and approved the final version of the manuscript.
The authors thank the orthopedic surgeons in Denmark for data reporting.
Acta thanks Lars Evert Adolfsson and Björn Salomonsson for help with peer review of this study.
Hemiarthroplasty and total shoulder arthroplasty were previously regarded as equally effective in the treatment of glenohumeral osteoarthritis for patients with concentric wear of the glenoid (1,2). However, within the last decades, total shoulder arthroplasty has shown superior outcomes compared with hemiarthroplasty (3,4) and is now regarded as the gold standard in the treatment of severe osteoarthritis in patients with intact rotator cuff function (4).
Although most patients have good outcomes after anatomical total shoulder arthroplasty, certain risk factors for a worse outcome have been identified. Young patients have inferior patient-reported outcomes and are less satisfied with their results compared with the elderly population (5-7). Glenohumeral osteoarthritis after shoulder dislocation is common (8-10), and previous publications have indicated that prior surgery for instability may lead to suboptimal functional outcome or an increased risk of complications (11-13). Whether young age and previous surgery for instability are independent risk factors for a worse outcome or if the inferior outcome of patients with previous surgery for instability is related to a higher proportion of young patients is not known.
We assessed risk factors for a worse patient-reported outcome after anatomical shoulder arthroplasty for osteoarthritis. Our hypothesis was that previous surgery for instability would be a risk factor for a worse patient-reported outcome independent of age, sex, and arthroplasty type.
Patients and methods
Data source
We obtained data from the Danish Shoulder Arthroplasty Registry (14), which is a nationwide registry financed by the Danish government. It is independent of the industry and of any other commercial interests. The registry was established in 2004. Since 2006, reporting to the registry has been mandatory for all Danish hospitals performing shoulder arthroplasty. The surgeon reports data related to the patient and the operation using an electronic platform system. Surgeons are encouraged to reply to all questions and the proportion of missing data is less than 1% for previous surgery, age, sex, indication for arthroplasty, and arthroplasty type. In 2004 and 2005, the completeness of reporting to the registry was low and is therefore now regarded as a trial period. Since 2006, the completeness has been 95% (15).
Population
We included all primary shoulder arthroplasties for primary or secondary osteoarthritis that were reported to the Danish Shoulder Arthroplasty Registry between 2006 and 2018. We excluded patients with a proximal humeral fracture, avascular necrosis, rheumatoid arthritis, or rotator cuff arthropathy, patients who were treated with a reverse shoulder arthroplasty, patients where the arthroplasty type was not reported or reported as “other arthroplasty type,” and patients who did not have a Danish civil registration number. 3,743 arthroplasties were included (Figure).
There were 1,509 men and 2,234 women. 516 patients were aged 55 years or younger and 3,227 patients were older than 55 years. 3,456 arthroplasties were recorded as primary osteoarthritis and 287 as secondary osteoarthritis. Previous non-arthroplasty surgery was reported for 568 patients of whom 116 had previous surgery for instability and 430 had subacromial decompression with or without acromioclavicular joint resection or synovectomy. For 22 patients the type of previous surgery was missing. These patients were excluded from the linear regression model.
Patient-reported outcome
The Western Ontario Osteoarthritis of the Shoulder (WOOS) index was used as outcome. The questionnaire was sent to all patients 12 months (10–14) after surgery by the DSR. For economic and logistical reasons there was no preoperative assessment, and the questionnaire was sent to the patients only once without reminders. The WOOS Index is a disease specific questionnaire that measures the quality of life of patients with glenohumeral osteoarthritis (16). A VAS score that ranges from 0 to 100 is used for each question. There are 19 questions, giving a total score ranging from 0 to 1,900, with 1,900 being the worst. For simplicity of presentation, it is recommended to convert the raw scores to a percentage of the maximum score, with 100 being the best (16). The questionnaire has been translated into a Danish version according to international guidelines (17).
Information concerning the clinically relevant difference of WOOS is limited. The patient-acceptable symptom state (PASS) is not known. In a small population of patients treated with anatomical total shoulder arthroplasty for osteoarthritis, the minimal clinically important difference (MCID) varied from 10% to 14% of a maximum score depending on the methodological approach (18). We used the MCID of 12% of a maximum score from the anchor-based method to define the clinically relevant difference.
In the case of revision or death within 1 year of the operation, the WOOS questionnaire was not sent to the patient. In the case of revision later than 1 year after the operation, the WOOS score was recorded as usual and included in the analysis. 57 (2%) patients died and 60 patients (2%) underwent revision surgery within the first year. Of the remaining 3,626 patients, 2,497 (69%) returned a complete questionnaire, 196 (5%) returned an incomplete questionnaire, and 933 (26%) did not respond. Only patients with a complete questionnaire were included in the general linear model.
Statistics
The results did not follow the assumption of normal distribution in all subgroups, but this has few practical consequences in large datasets without outliers (19). Thus, the results of subgroups were reported using mean value and standard deviation (SD). A general linear model was used to identify patients with a worse outcome. Age group (55 years or younger or older than 55 years), sex, arthroplasty type (hemiarthroplasty and total shoulder arthroplasty), and previous non-arthroplasty surgery of the same shoulder (no previous surgery, previous surgery for instability, previous surgery with subacromial decompression with or without acromioclavicular joint resection or synovectomy) were included in the multivariate model. Estimates were given with 95% confidence intervals (CI). Men, total shoulder arthroplasty, age above 55 years, and no previous surgery were used as references. 435 patients with bilateral procedures were included with both arthroplasties as independent cases. The analysis was performed using SPSS version 25.0 (IBM Corp, Armonk, NY, USA).
Ethics, funding, data sharing, and potential conflicts of interest
Approval by the local ethics committee was not required for this registry study. The study was approved by the Danish Data Protection Agency (registration number: P-2020-316). No intervention was made, and all patients were treated according to clinical practice at the time of surgery. Informed consent was not required. Data may be made available to other researchers upon request to the Danish Shoulder Arthroplasty registry given that approval from the registry can be provided. No funding was received. There were no conflicts of interest to be declared related to this study.
Results
The mean WOOS score was 78 (SD 23) for patients with no previous surgery, 55 (SD 28) for patients with previous surgery for instability, and 66 (SD 28) for patients with previous subacromial decompression with or without acromioclavicular joint resection or synovectomy. The mean WOOS score was 83 (SD 23) for total shoulder arthroplasty and 70 (SD 26) for hemiarthroplasty. For patients with previous surgery for instability the mean WOOS was 54 (SD 24) for hemiarthroplasty and 57 (SD 35) for total shoulder arthroplasty (Table 1). Patients with previous surgery for instability were more often 55 years or younger, more often men, and were more often treated with a hemiarthroplasty compared with patients with no previous surgery (Table 2). The results of the multivariate regression model showed that patients with previous surgery for instability had a worse outcome compared with patients without previous surgery which can be regarded as clinically relevant. Patients with previous subacromial decompression with or without acromioclavicular joint resection or synovectomy also had a statistically significant worse outcome compared with patients without previous surgery, but the difference was not regarded as clinically relevant. Hemiarthroplasty had a significantly worse outcome compared with total shoulder arthroplasty, and young patients had a significantly worse outcome compared with older patients. The differences were similar to the clinically relevant difference of 12 (Table 3).
| Subgroups | Instability | Others a | None |
| Age | |||
| ≤ 55 | 70 (60) | 134 (31) | 307 (10) |
| > 55 | 46 (40) | 296 (69) | 2,868 (90) |
| Sex | |||
| Women | 41 (35) | 232 (54) | 1,951 (61) |
| Men | 75 (65) | 198 (46) | 1,224 (39) |
| Arthroplasty type | |||
| Hemi- | 82 (71) | 239 (56) | 1,582 (50) |
| Total | 34 (29) | 191 (44) | 1,593 (50) |
| a Including subacromial decompression with or without acromioclavicular joint resection or synovectomy. | |||
| Factor | Δ (CI) |
| Age (ref. > 55) | |
| ≤ 55 a | –16 (–13 to –19) |
| ≤ 55 b | –11 (–8 to –14) |
| Sex (ref. > men) | |
| Women a | –1 (–3 to 1) |
| Women b | –4 (–2 to –6) |
| Arthroplasty type (ref. > total) | |
| Hemi- a | –13 (–11 to –15) |
| Hemi- b | –12 (–10 to –14) |
| Previous surgery for (ref. > none) | |
| Instability a | –24 (–17 to –30) |
| Instability b | –16 (–10 to –22) |
| Others a, c | –12 (–9 to –15) |
| Others b, c | –9 (–7 to –12) |
| WOOS score, see Table 1. a 1 factor linear regression b Multivariate model c Others, see Table 1. |
|
Discussion
We found worse outcomes for patients with previous surgery for instability independent of age, sex, and arthroplasty type. The reason cannot be deduced from our study and there is no adequate explanation in the literature. Several factors could, in theory, have an adverse effect on the outcome for these patients. A long history of instability and previous surgery may lead to eccentric glenoid wear and subsequently a technically demanding operation with risk of persisting instability, subluxation of the humeral component, or loosening of the glenoid component. Changes in anatomy with a retracted and stiff anterior capsule may lead to poor range of motion if not adequately released during the arthroplasty procedure. A retracted and stiff anterior capsule may also force the humeral component posteriorly with risk of instability or subluxation, wear or loosening of the glenoid component, or rotator cuff failure. Stiffness and scarring may make glenoid exposure technically demanding resulting in suboptimal positioning of the glenoid component. Although intact, the rotator cuff tendons may be either loose, rigid, or both. In this case, an anatomical shoulder arthroplasty can fail because of inadequate rotator cuff function. Finally, for these, often multi-operated patients, low-grade infections may lead to persistent pain if the infection is not recognized and addressed during the arthroplasty procedure.
We also found a statistically significant worse outcome for patients with previous subacromial decompression with or without acromioclavicular joint resection or synovectomy compared with patients without previous surgery, but the difference in WOOS of -9 cannot be regarded as clinically relevant. The relatively small difference confirms the results of a recent publication where 43 patients who had a shoulder arthroplasty with a history of previous arthroscopic debridement and 86 patients without previous surgery were included in a matched-pair analysis. The authors concluded that previous arthroscopic debridement was not associated with an inferior outcome for either total shoulder arthroplasty or hemiarthroplasty with ream-and-run of the glenoid (20).
Whether the worse outcome for patients with previous surgery for instability is related to the surgical procedure, the instability pathology, or both cannot be deduced from our study. It has previously been reported that patients with secondary osteoarthritis have a worse outcome compared with patients with primary osteoarthritis (21). However, that study did not report separate results for patients with osteoarthritis secondary to instability.
The type of osteoarthritis (i.e., primary or secondary) was reported during the entire study period, but the reason for secondary osteoarthritis (i.e., fracture, instability, and others) has been reported to the registry only since January 2016. In the future it would be interesting to compare the outcome for patients with previous surgery for instability, patients with osteoarthritis second to instability but without previous surgery, and patients with primary osteoarthritis.
Our data did not include information on the indication for or type of previous surgery for instability. Thus, we were unable to distinguish between anterior, posterior, or multidirectional instability as the indication, between open or arthroscopic labral repair, and between different types of bone block transfer procedures such as Bristow, Latarjet, or Eden–Hybinette.
We found that hemiarthroplasty was associated with a statistically significantly worse outcome than total shoulder arthroplasty, which also could be regarded as clinically relevant. This confirms the results of previous studies and supports the recommendation from national guidelines suggesting using a total shoulder arthroplasty in patients with osteoarthritis and intact rotator cuff function. However, for patients with previous surgery for instability we found similar poor outcomes of hemiarthroplasty and total shoulder arthroplasty.
There is little information available to guide decision-making regarding patients with severe osteoarthritis after previous surgery for instability. Existing information is based on either case series or small comparative studies. Sperling et al. reported disappointing outcomes of 10 hemiarthroplasties and 21 total shoulder arthroplasties, a high rate of revisions, and no difference in satisfaction or functional result between the 2 arthroplasty types (11). In a more recent paper, the authors included 5 hemiarthroplasties and 14 total shoulder arthroplasties for osteoarthritis in patients with a previous Bristow or Latarjet procedure. They found that 3 out of 5 patients with a hemiarthroplasty and 7 out of 14 patients with a total shoulder arthroplasty were unsatisfied with the result (12). Bigliani et al. reported the outcome of 5 hemiarthroplasties and 12 total shoulder arthroplasties in patients with previous surgery for instability and found that 4 of the 17 patients were unsatisfied (22). The results of shoulder arthroplasty for osteoarthritis in patients with previous surgery for instability have been summarized in a recent systematic review. In their metaanalysis the authors found a Constant Murley score of 68 and a complication rate of 37% for all types of anatomical shoulder arthroplasty (13). The nature of this non-intervention and non-randomized study does not allow conclusions as to the optimal treatment of patients with previous surgery for instability. However, based on our data we emphasize that patients with previous surgery should be informed of the higher risk of a worse outcome after shoulder arthroplasty. Although the evidence is sparse, use of bone-block, an augmented glenoid component, or a reverse shoulder arthroplasty could be considered in the case of sever posterior glenoid wear.
Young patients had worse outcomes independent of sex, arthroplasty type, and previous non-arthroplasty surgery. Thus, the relatively poor outcome of shoulder arthroplasty in young patients found in previous publications (5-7,23) cannot be explained by the use of a specific arthroplasty type or a higher proportion of patients with a poor outcome because of previous non-arthroplasty surgery. It has been suggested that young patients have high functional demands (24) and higher expectations of improved ability to interact with others and to participate in sports and exercise compared with older patients (25). If the demands and expectations are not met, some patients may be disappointed by the outcome. This may be reflected in their WOOS score. As for patients with previous surgery for instability, we emphasize that young patients should also be informed about their individual risk of a disappointing outcome. We used an age limit of 55 years to define a young patient. This categorization was applied due to an expected change in the patient’s activity level. We acknowledge that other surgeons and authors may have chosen differently and that the use of another age limit could lead to other conclusions.
There are important methodological considerations for our study. The indication (e.g., threshold) for surgery and the choice for a specific arthroplasty type was not known. There was no preoperative assessment of WOOS. Thus, differences in the preoperative impairment between patients with and without previous non-arthroplasty surgery and between arthroplasty types might have influenced the WOOS at 1 year. A previous publication from the Danish Shoulder Arthroplasty Registry analyzed the consequences of missing WOOS scores. By sending one postal reminder the authors were able to increase the response rate from 65% to 80%. WOOS was similar between responders to the first and the reminder questionnaire. Furthermore, demographic data were similar between responders and non-responders. The authors concluded that non-responders did not appear to bias the overall results after shoulder replacement (26). Nevertheless, it is important to consider that not all patients in our study returned a complete questionnaire, and any systematic differences between responders and non-responders may have influenced the results.
Conclusion
Anatomical shoulder arthroplasty for osteoarthritis led to good patient-reported outcomes, especially in patients who were older than 55 years. Previous surgery for instability was associated with worse patient-reported outcomes independent of age, sex, and arthroplasty type. Patient with previous surgery for instability should be informed about their individual risk of a worse outcome. Accurate patient selection, thorough preoperative planning, and attention to technical details are important and may improve the outcome of shoulder arthroplasty in patients who have had previous surgery for instability.
- Neer C S. Replacement arthroplasty for glenohumeral osteoarthritis. J Bone Joint Surg Am 1974; 56: 1-13.
- Levy O, Copeland S A. Cementless surface replacement arthroplasty (Copeland CSRA) for osteoarthritis of the shoulder. J Shoulder Elbow Surg 2004; 13: 266-71.
- Singh J A, Sperling J, Buchbinder R, McMaken K. Surgery for shoulder osteoarthritis: a Cochrane systematic review. J Rheumatol 2011; 38: 598-605.
- Izquierdo R, Voloshin I, Edwards S, Freehill M Q, Stanwood W, Wiater J M, et al. Treatment of glenohumeral osteoarthritis. J Am Acad Orthop Surg 2010; 18: 375-82.
- Patel R B, Muh S, Okoroha K R, Wright T W, Flurin P H, Roche C, Zuckerman J D. Results of total shoulder arthroplasty in patients aged 55 years or younger versus those older than 55 years: an analysis of 1135 patients with over 2 years of follow-up. J Shoulder Elbow Surgery 2019; 28: 861-8.
- Roberson T A, Bentley J C, Griscom J T, Kissenberth M J, Tolan S J, Hawkins R J, et al. Outcomes of total shoulder arthroplasty in patients younger than 65 years: a systematic review. J Shoulder Elbow Surgery 2017; 26: 1298-1306.
- Rasmussen J V, Polk A, Sorensen A K, Olsen B S, Brorson S. Outcome, revision rate and indication for revision following resurfacing hemiarthroplasty for osteoarthritis of the shoulder: 837 operations reported to the Danish Shoulder Arthroplasty Registry. Bone Joint J 2014; 96-B (4): 519-25.
- Samilson R L, Prieto V. Displocation arthropathy of the shoulder. J Bone Joint Surg Am 1983; 65(4): 456-60.
- Hovelius L, Augustini B G, Fredin H, Johansson O, Norlin R, Thorling J. Primary anterior dislocation of the shoulder in young patients: a ten-year prospective study. J Bone Joint Surg Am 1996; 78(11): 1677-84.
- Lädermann A, Lubbeke A, Stern R, Cunningham G, Bellotti V, Gazielly D F. Risk factors for dislocation arthropathy after Latarjet procedure: a long-term study. Int Orthop 2013; 37(6): 1093-8.
- Sperling J W, Antuna S A, Sanchez-Sotelo J, Schleck C, Cofield R H. Shoulder arthroplasty for arthritis after instability surgery. J Bone Joint surg Am 2002; 84(10): 1775-81.
- Willemot L B, Elhassan B T, Sperling J W, Cofield R H, Sànchez-Sotelo J. Arthroplasty for glenohumeral arthritis in shoulders with a previous Bristow or Laterjet Procedure. J Shoulder Elbow Surg 2018; 27: 1607-13.
- Cerciello S, Corona K, Morris B J, Paladini P, Porcellini G, Merolla G. Shoulder arthroplasty to address the sequelae of anterior instability arthropathy and stabilizing procedures: systematic review and metaanalysis. Arch Orthop Trauma Surg 2020; 140 (12): 1891-1900.
- Rasmussen J V, Jakobsen J, Brorson S, Olsen B S. The Danish Shoulder Arthroplasty Registry: clinical outcome and short-term survival of 2,137 primary shoulder replacements. Acta Orthop 2012; 83: 171-3.
- Rasmussen J V, El-Galaly A, Thillemann T M, Jensen S L. High completeness and accurate reporting of key variables make data from the Danish Shoulder Arthroplasty Registry a valuable source of information. Clin Epidemiol 2021: 13; 141-8.
- Lo I K, Griffin S, Kirkley A. The development of a disease-specific quality of life measurement tool for osteoarthritis of the shoulder: the Western Ontario Osteoarthritis of the Shoulder (WOOS) index. Osteoarthritis Cartilage 2001; 9: 771-8.
- Rasmussen J V, Jakobsen J, Olsen B, Brorson S. Translation and validation of the Western Ontario Osteoarthritis of the Shoulder (WOOS) Index: the Danish version. Patient Relat Outcomes Meas 2013: 18; 49-54.
- Nyring M R K, Olsen B S, Amundsen A, Rasmussen J V. The minimal clinically important difference for the Western Ontario Osteoarthritis of the Shoulder Index (WOOS) and the Oxford Shoulder Score (OSS). Patient Relat Outcome Meas 2021; 12: 299-306.
- Lumley T, Diehr P, Emerson S, Chen L. The importance of the normality assumption in large public health datasets. Annu Rev Public Health 2002; 23: 151-69.
- Schiffman C J, Whitson A J, Chawla S S, Matsen F A 3rd, Hsu J E. Arthroscopic management of glenohumeral arthritis in the young patient does not negatively impact the outcome of subsequent anatomic shoulder arthroplasty. Int Orthop 2021; 45(8): 2071-9.
- Ödquist M, Hallberg K, Rahme H, Salomonsson B, Rosso A. Lower age increases the risk of revision for stemmed and resurfacing shoulder hemi arthroplasty. Acta Orthop 2018; 89(1): 3-9.
- Bigliani L U, Weinstein D M, Glascow M T, Pollock R G, Flatow E L. Glenohumeral arthroplasty for arthritis after instability surgery. J Shoulder Elbow Surg 1995; 4(2): 87-94.
- Sperling J W, Cofield R H, Rowland C M. Neer hemiarthroplasty and Neer total shoulder arthroplasty in patients fifty years old or less: long-term results. J Bone Joint Surg Am 1998 (80): 464-73.
- Saltzman B M, Leroux T S, Verma N N, Romeo A A. Glenohumeral osteoarthritis in young patients. J Am Acad Orthop Surg 26: e361-e370.
- Henn F R 3rd, Ghomrawi H, Rutlede J R, Mazumdar M, Mancuso C A, Marx R G. Preoperative patient expectations of total shoulder arthroplasty. J Bone Joint Surg Am 2011: 93(22): 2110-15.
- Polk A, Rasmussen J V, Brorson S, Olsen B S. Reliability of patient-reported functional outcome in a joint replacement registry: a comparison of primary responders and non-responders in the Danish Shoulder Arthroplasty Registry. Acta Orthop 2013; 84(1): 12-17.