Manipulation under anesthesia after total knee arthroplasty: a retrospective study of 145 patients
Julius SALA 1,2, Antti JAROMA 1,2, Reijo SUND 1, Jukka HUOPIO 1,2, Heikki KRÖGER 1,2, and Joonas SIROLA 1,2
1 Kuopio Musculoskeletal Research Unit (KMRU), University of Eastern Finland, Kuopio; 2 Department of Orthopaedics, Traumatology and Hand Surgery, Kuopio University Hospital, Kuopio, Finland
Background and purpose — Manipulation under anesthesia (MUA) is considered to be effective in treating stiffness after total knee arthroplasty (TKA). However, not all patients achieve a satisfactory range of motion (ROM) after MUA. This retrospective study determined the outcome of MUA and identified the factors affecting it.
Patients and methods — The final sample consisted of 150 MUAs performed on 145 patients. The parameters of interest were ROM and Knee Society Score (KSS) or Oxford Knee Score (OKS). The associations of preoperative, perioperative, and postoperative risk factors with gain in flexion and flexion at post-MUA follow-up (an average of 2 months after MUA) were analyzed using multivariable regression model.
Results — The mean of 26° (95% CI 23–29) gain in flexion and the mean of 3° (CI 2–4) gain in extension were noticed at post-MUA follow-up when compared with the ROM preceding MUA. The mean post-MUA-FU flexion was 99° (CI 97–102) and the mean post-MUA-FU extension deficit was 4° (CI 2–5). KSS (121 vs. 129) and OKS (29 vs. 28) were similar before and after MUA. The early timing of MUA was associated with better gain in flexion –0.04 (CI –0.08 to –0.01), while we found no association between the timing of MUA and flexion after MUA –0.004 (CI –0.03 to 0.03). High BMI was associated with better gain in flexion 0.8 (CI 0.2–1.5).
Interpretation — We found that ROM improved substantially after MUA. The gain in flexion decreased as the time between TKA and MUA increased.
Citation: Acta Orthopaedica 2022; 93: 583–587. DOI http://dx.doi.org/10.2340/17453674.2022.3167.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2021-12-07. Accepted: 2022-05-04. Published: 2022-06-21.
Correspondence: juliussa@uef.fi
All authors contributed to the planning of the study. JS (Sala) wrote the article. JS (Sirola), AJ, JH, HK, and RS conducted the study. RS, JS (Sirola), and AJ assisted in statistical analysis.
Acta thanks Annette W-Dahl for help with peer review of this study.
Manipulation under anesthesia (MUA) is considered to be effective in treating stiffness after total knee arthroplasty (TKA), with an average of 22° to 39° gain in flexion (1-11) and an average of 2° to 5° gain in extension (2,3,8,10). MUA is a procedure in which a patient’s knee is manipulated under anesthesia with the purpose of breaking arthrofibrosis (12). Despite the generally good outcome of MUA, not all patients have a satisfactory range of motion (ROM) after MUA (4,5,9,11,13). Numerous factors are suggested to predict worse outcome of MUA. Diabetes mellitus (8), prior knee procedures (9), and pre-TKA ROM (2,4) are preoperative factors found to have been associated with lower flexion after MUA. Additionally, using a posterior stabilizing (PS) prosthesis instead of a cruciate retaining (CR) was found to be associated with better flexion after MUA (8).
The timing of MUA is the most widely recognized postoperative factor affecting the outcome of MUA. MUA performed early was found to be associated with better gain in flexion and better flexion after MUA (7,8). In particular, MUA later than 3 months after TKA gave inferior results. However, the role of many risk factors in affecting the results of MUA remains unclear. MUA is considered a safe procedure, but rare complications such as femoral or tibial fractures, patellar tendon ruptures, incision ruptures, and hemarthrosis are reported (6,12).
This retrospective study determines the improvement of ROM (flexion and extension) and Knee Society Score (KSS) (15) or Oxford Knee Score (OKS) (16) after MUA and, further, the influence of preoperative, perioperative, and postoperative factors on gain in flexion and total flexion at follow-up in patients who underwent MUA as a treatment for stiffness after primary TKA.
Patients and methods
Patients
The study included patients who underwent MUA after TKA as a treatment for stiffness at Kuopio University Hospital from 2009 to 2019. Only MUAs that were done after primary TKAs were included. The study did not have any lower or upper time limit between TKA and MUA and a maximum gap of 2 years was applied to guarantee comparable extraction of events from the data. Between January 1, 2009 and December 31, 2019, 6,281 primary TKAs were identified. As a result of stiffness, 168 MUAs were performed on 163 patients. 5 patients underwent bilateral manipulation. The prevalence of MUA was thus 2.7%. After the exclusion of 18 patients who did not attend follow-up visits after MUA, the final sample consisted of 150 MUAs performed on 145 patients.
Study parameters
The parameters of interest were knee ROM (flexion and extension) and KSS or OKS. ROM was measured at 6 time points: preoperatively at the preoperative appointment (pre-TKA), perioperatively after implanting (peri-TKA), postoperatively on the day of discharge (post-TKA), preceding MUA (pre-MUA), on the day of discharge after MUA (post-MUA), and at the follow-up approximately 2 months after MUA (post-MUA-FU). KSS or OKS was gathered from 3 time points: pre-TKA, pre-MUA, and post-MUA-FU. The clinical rating system that was used in our clinic was changed during the study time: from 2009 to 2017, KSS was used; and from 2018 to 2019, OKS was used. KSS and OKS are patient-reported outcome measures (PROM) with higher points referring to better knee function. The scale of KSS is 0–200 and OKS is 0–48.
In this study, the preoperative factors of interest were age, sex, BMI, ASA score, diabetes mellitus (DM), smoking status, prior knee procedures, indication for TKA, and pre-TKA flexion. Perioperative factors of interest were the type of prosthesis, use of patellar component, and possible femoral component overstuffing. Postoperative factors of interest were the length of stay (LOS) and the timing of MUA. Femoral component overstuffing was measured using a postoperative lateral view knee radiograph. Overstuffing is the distance between the most proximal part of the component and the femoral cortex. Patients were divided into 3 groups by the timing of MUA: early (< 8 weeks), postponed (8–12 weeks), and late (> 12 weeks).
Postoperative protocol
At our institution, the postoperative protocol for TKA patients was as follows. Patients were advised to contact a physiotherapist in the case of severe early postoperative mobilization problems. For these patients, MUA prior to the first scheduled postoperative control might have been performed. If no early rehabilitation problems were detected, patients who underwent TKA had a postoperative follow-up at 3 months. If knee ROM was considered clinically sufficient by the orthopedic surgeon and the patient was satisfied, no more follow-ups were scheduled. In the case of limited ROM, physiotherapy was prescribed. If ROM was not increased despite enhanced physiotherapy, MUA was considered. MUA might have been an option after the first postoperative follow-up if the knee was considered to be excessively stiff for physiotherapy only. We did not use any specific flexion cut-off for MUA, but the decision to perform MUA was based on a patient-specific case-by-case analysis. The day after MUA, patients were discharged and ROM was measured. A continuous passive motion (CPM) device was used at home to support ROM for 1 week after MUA. Patients were invited for follow-up about 2 months after MUA. If ROM was satisfactory, no more follow-ups were scheduled. If ROM was still limited, patients were monitored and physiotherapy was intensified. In the case of recurrent stiffness, a second MUA was considered. In this study, only primary MUAs were included.
Statistics
To determine which factors might have an association with the outcome of MUA, we created 2 multivariable regression models in which we included all the pre-, peri-, and postoperative factors that were included in this study. The terminal variables were the post-MUA-FU flexion and gain in flexion. The gain in flexion was the difference in flexion between the post-MUA-FU flexion and the pre-MUA flexion. Mean, SD, range, and 95% confidence intervals (CI) of mean are presented as appropriate in patient characteristics. The results of multivariable regression analysis were presented with regression coefficients (Beta) and 95% confidence intervals. Demographic and clinical data were gathered from medical records, the local knee register, and anesthesiology databases. All statistical analyses were done using IBM SPSS version 27 (IBM Corp, Armonk, NY, USA).
Ethics, funding, potential conflict of interest, and data sharing
The study was approved by the ethics committee in December 2019 (approval no. 5203120). This study did not receive any form of grants or funding. The authors declare no conflict of interest. Due to privacy regulation, the original data cannot be shared. Anonymized summary tables can be shared on reasonable request.
Results
Characteristics (Table 1)
The mean age in this sample was 62 years (SD 8.6, range 42–83). 70% of the patients were female. The mean BMI was 29 (SD 5, range 19–46). The ASA score was 1 in 35 cases, 2 in 90 cases, and 3 in 25 cases. The prevalence of DM was 20%, and of current smoking was 9%. At least 1 prior knee procedure was performed on 62 knees. The most common prior knee procedures were arthroscopy for 45 knees, high tibial osteotomy (HTO) for 8 knees, and anterior cruciate ligament (ACL) reconstruction for 7 knees. Several other prior knee procedures were identified, but frequencies of those were less than 5. Indications for TKA were primary osteoarthritis in 130 cases, post-traumatic osteoarthritis in 15 cases, rheumatoid arthritis in 4 cases, and idiopathic aseptic necrosis in 1 case. Usually, a cruciate-retaining (CR) prosthesis was used (133 knees). In 15 cases, a posterior stabilized (PS) prosthesis was used. In 2 cases, a stabilizing (TC III-type) prosthesis was used. 11 knees had a patellar component. The mean femoral component overstuffing was 1.0 mm (SD 1.1, range 0.0–5.0). The mean LOS after TKA was 3.8 days (SD 1.3, range 1–12). 1 patient’s incision ruptured during MUA. No other complications were noticed. The mean time between TKA and MUA was 13 weeks (CI 11–15). The time between TKA and MUA was < 8 weeks in 48 cases, 8–12 weeks in 41 cases, and > 12 weeks in 61 cases. The mean time between MUA and post-MUA-FU was 9 weeks (CI 7–10).
Range of motion (Table 2)
The mean gain in flexion of 26° (CI 23–29) was noticed when comparing the mean post-MUA-FU flexion of 99° (CI 96–102) with the mean pre-MUA flexion of 73° (CI 70–76). Correspondingly, the mean gain in extension was 3° (CI 2–4). The mean post-MUA-FU extension deficit was 4° (CI 2–5). Gain in flexion was > 20° in 85 cases, 5–20° in 50 cases, and ≤ 0° in 15 cases. The mean post-MUA-FU flexion remained significantly lower than the mean pre-TKA flexion of 113° (111–115). The mean post-MUA flexion of 104° (CI 102–106) was significantly higher than the mean post-MUA-FU flexion. In 24 cases (16%), the pre-MUA extension deficit was more than 10° (mean 19°, CI 18–21). These patients’ mean gain in extension was 11° (CI 8–13), and the mean post-MUA-FU extension deficit was 9° (CI 6–11).
KSS, OKS (Table 2)
We found that KSS and OKS were similar before and after MUA. The mean post-MUA-FU OKS was 28 (CI 23–33) and the mean pre-MUA OKS was 29 (CI 26–32). However, the mean post-MUA-FU KSS of 129 (CI 118–139) was higher than the mean pre-MUA KSS of 121 (CI 109–133) but the difference was not statistically significant. The mean post-MUA-FU OKS was higher than the mean pre-TKA OKS of 25 (CI 22–28) but not significantly. Nevertheless, the mean post-MUA-FU KSS was significantly higher than the mean pre-TKA KSS of 96 (CI 91–102). Consequently, there was a statistically significant variation in post-MUA-FU KSS and OKS, with a range of 38–199 (KSS) and 15–40 (OKS).
Associated factors (Table 3)
We found that BMI and timing of MUA had an association with gain in flexion. High BMI had a significant association with better gain in flexion (0.8, CI 0.2–1.5, for beta in multivariable regression), but did not have an association with post-MUA-FU flexion (0.4, CI –0.2 to 1.1, for beta in multivariable regression). The timing of MUA had a significant negative association with gain in flexion (–0.04, CI –0.08 to –0.01, for beta in multivariable regression). This is shown in the Figure. Nevertheless, the timing of MUA did not have an association with post-MUA-FU flexion (–0.004, CI –0.03 to 0.03, for beta in multivariable regression). We noticed a significant difference in the mean gain in flexion between the early, postponed, and late groups. The mean gain in flexion was 37° (CI 30–43) in the early group, 28° (CI 22–33) in the postponed group, and 17° (CI 13–21) in the late group. Nevertheless, we did not find a significant difference in the mean post-MUA-FU flexion between the groups. The mean post-MUA-FU flexion was 102° (CI 96–108) in the early group, 100° (CI 95–104) in the postponed group, and 97° (CI 93–101) in the late group. Excluding BMI and timing, none of the pre-, peri-, and postoperative factors had an association with post-MUA-FU flexion or gain in flexion.
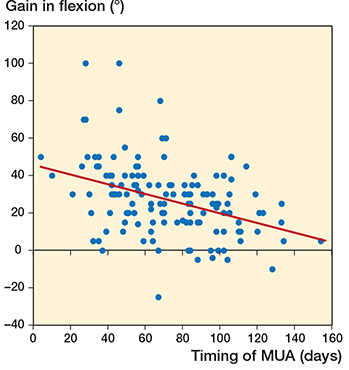
Association between the timing of MUA and the gain in flexion. Multivariable regression analysis showed that there was a statistically significant negative association between the timing of MUA and the gain in flexion –0.04 (CI –0.08 to –0.01). MUA = manipulation under anesthesia
Discussion
We found that ROM improved substantially, with an average of 26° gain in flexion, which is comparable with the results reported previously (1-11). An average of 3° gain in extension occurred. However, in patients with moderate or severe extension deficit (> 10°), a substantial gain in extension with an average of 11° was noticed. These findings support the current knowledge that MUA is an effective procedure for lack of flexion and also for lack of extension (3,10). We noticed a pronounced variation in the gain in flexion, with a range of –25° to 100°. A negative gain in flexion means that a patient’s knee stiffens between MUA and follow-up. Consequently, some patients deteriorated compared with the status before MUA, but most patients improved their ROM. These findings confirm previous knowledge that the benefit of MUA is individual, and the expected outcome varies (4,5,9,11,13).
Although ROM increased after MUA, KSS and OKS did not. KSS consists of 2 parts: knee score (including pain, ROM, alignment, and stability) and function (including assessment of walking on the flat, walking on stairs, and need for walking aids) (15). OKS measures the knee’s function and pain in daily routines such as walking on the flat and stairs, doing housework, and getting in or out of a car (16). Patients did benefit from MUA by gaining ROM, but pain and restrictions in daily living were not reduced. This might be explained by the relatively short follow-up time. MUA is a procedure that demands time to recover.
Another purpose of this study was to discover whether there were pre-, peri-, or postoperative factors associated with lower flexion after MUA or lower gain in flexion. Among preoperative factors, we found that high BMI was associated with better gain in flexion. Previous studies did not consider high BMI as a risk factor for worse outcome of MUA (7,9,11). We found that patients with higher BMI benefited more from MUA. The role of diabetes in predicting the outcome of MUA is contradictory (7,8,11). In our study, diabetes did not have an association with gain in flexion or post-MUA-FU flexion. The impact of flexion before TKA on the outcome of MUA is unclear. Both association (2,4) and no association (1,11) between flexion before TKA and flexion after MUA or gain in flexion are reported. We did not find association between pre-TKA flexion and gain in flexion or post-MUA-FU flexion. The association between prior knee procedures and the outcome of MUA is unclear. Ipach et al. (9) found an association between at least 2 prior knee procedure and worse outcome of MUA, but the result was not confirmed by Cates and Schmidt (3). We did not find associations between 1 or more prior knee procedures and gain in flexion or post-MUA-FU flexion. Previous studies did not find association between smoking and outcome of MUA, confirming our findings (3).
We did not find associations between perioperative factors and post-MUA-FU flexion or gain in flexion. The type of prosthesis is suggested to affect the outcome of MUA. Better flexion after MUA is reported when using a PS instead of a CR prosthesis (8). We did not find an association between the type of prosthesis and the gain in flexion or the post-MUA-FU flexion. Femoral component overstuffing or use of the patellar component did not have an association with gain in flexion or post-MUA-FU flexion.
In our study, the timing of MUA was the most significant postoperative factor influencing the outcome of MUA: the earlier MUA was performed, the better the gain in flexion. These results support the previous findings (7,8). However, we did not find an association between the timing of MUA and post-MUA-FU flexion. Consequently, patients with severe stiffness end up with MUA earlier than patients whose knees are less stiff. When performing MUA late, especially more than 12 weeks after TKA, the expected gain in flexion was less than when performing MUA before 12 weeks. Nevertheless, even the late MUAs (12 weeks postoperatively) gave a satisfactory gain in flexion, which could be important for an individual patient. 59% of MUAs were performed within 12 weeks from TKA and therefore performed before or at the time of postoperative control visit of 3 months. Accordingly, most of the MUA patients had mobilization problems and contacted the hospital before the control visit. We did not find an association between the length of stay and gain in flexion or post-MUA-FU flexion.
MUA may not be the best solution for all patients with stiff TKA. Thorsteinsson et al. (17) found that MUA patients had an approximately double 10-year cumulative revision rate compared with general TKA patients. Our study had a different purpose than that of Thorsteinsson et al. and did not include the analysis of revision rates.
The strength of our study is the number of subjects. To our knowledge, this is one of the largest studies analyzing the outcome of MUA and factors affecting it. Additionally, the roles of several potential risk factors on the outcome of MUA were investigated. The knee ROM, most commonly flexion, is generally the main interest in publications on MUA. In addition to flexion, we included extension, KSS, and OKS. Our study has some limitations. The first is the retrospective study design. Additionally, many risk factors were not divided evenly in this cohort. There were fewer knees with a patellar component, PS prosthesis, history of smoking, and post-traumatic or rheumatoid osteoarthritis. These frequencies could be too small to show a possible influence on the outcome of MUA. Additionally, we used 2 different patient-reported outcome measures during the study time. In particular, the proportion of valid OKS reports was low. Knee ROM was measured by surgeons and physiotherapists. There can be a variation in the accuracy of measurement of ROM between different persons.
In conclusion, we found that the majority of patients benefit from MUA by gaining ROM. The gain in flexion decreased as the time between TKA and MUA increased. In this study, no associations between risk factors and lower flexion after MUA were found.
- Yeoh D, Nicolaou N, Goddard R, Willmott H, Miles K, East D, et al. Manipulation under anaesthesia post total knee replacement: long term follow up. Knee 2012; 19(4): 329-31. doi: 10.1016/j.knee.2011.05.009.
- Rubinstein R A Jr, DeHaan A. The incidence and results of manipulation after primary total knee arthroplasty. Knee 2010; 17(1): 29-32. doi: 10.1016/j.knee.2009.07.001.
- Cates H E, Schmidt J M. Closed manipulation after total knee arthroplasty: outcome and affecting variables. Orthopedics 2009; 32(6): 398. doi: 10.3928/01477447-20090511-10.
- Keating E M, Ritter M A, Harty L D, Haas G, Meding J B, Faris P M, et al. Manipulation after total knee arthroplasty. J Bone Joint Surg Am 2007; 89(2): 282-6. doi: 10.2106/JBJS.E.00205.
- Ipach I, Schäfer R, Lahrmann J, Kluba T. Stiffness after knee arthrotomy: evaluation of prevalence and results after manipulation under anaesthesia. Orthop Traumatol Surg Res 2011; 97(3): 292-6. doi: 10.1016/j.otsr.2011.01.006.
- Issa K, Kapadia B H, Kester M, Khanuja H S, Delanois R E, Mont M A. Clinical, objective, and functional outcomes of manipulation under anesthesia to treat knee stiffness following total knee arthroplasty. J Arthroplasty 2014; 29(3): 548-52. doi: 10.1016/j.arth.2013.07.046.
- Vanlommel L, Luyckx T, Vercruysse G, Bellemans J, Vandenneucker H. Predictors of outcome after manipulation under anaesthesia in patients with a stiff total knee arthroplasty. Knee Surg Sports Traumatol Arthroscopy 2017; 25(11): 3637-43. doi: 10.1007/s00167-016-4413-6.
- Bawa H S, Wera G D, Kraay M J, Marcus R E, Goldberg V M. Predictors of range of motion in patients undergoing manipulation after TKA. Clin Orthop Relat Res 2013; 471(1): 258-63. doi: 10.1007/s11999-012-2591-1.
- Ipach I, Mittag F, Lahrmann J, Kunze B, Kluba T. Arthrofibrosis after TKA: influence factors on the absolute flexion and gain in flexion after manipulation under anaesthesia. BMC Musculoskelet Disord 2011; 12: 184. doi: 10.1186/1471-2474-12-184.
- Randsborg P H, Tajet J, Negård H, Røtterud J H. Manipulation under anesthesia for stiffness of the knee joint after total knee replacement. Arthroplast Today 2020; 6(3): 470-4. doi: 10.1016/j.artd.2020.05.019.
- Choi H R, Siliski J, Malchau H, Freiberg A, Rubash H, Kwon Y M. How often is functional range of motion obtained by manipulation for stiff total knee arthroplasty? Int Orthop 2014; 38(8): 1641-5. doi: 10.1007/s00264-014-2421-z
- Fox J L, Poss R. The role of manipulation following total knee replacement. J Bone Joint Surg 1981; 63(3): 357-62.
- Yercan H S, Sugun T S, Bussiere C, Ait Si Selmi T, Davies A, Neyret P. Stiffness after total knee arthroplasty: prevalence, management and outcomes. Knee 2006; 13(2): 111-17. doi: S0968-0160(05)00156-0.
- Issa K, Rifai A, Boylan M R, Pourtaheri S, McInerney V K, Mont M A. Do various factors affect the frequency of manipulation under anesthesia after primary total knee arthroplasty? Clin Orthop Relat Res 2015; 473(1): 143-7. doi: 10.1007/s11999-014-3772-x.
- Insall J N, Dorr L D, Scott R D, Scott W N. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 1989; (248): 13-14.
- Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br 1998; 80(1): 63-9. doi: 10.1302/0301-620x.80b1.7859.
- Thorsteinsson H, Hedström M, Robertsson O, Lundin N, W-Dahl A. Manipulation under anesthesia after primary knee arthroplasty in Sweden: incidence, patient characteristics and risk of revision. Acta Orthop 2019; 90(5): 484-8.