Distal radioulnar joint kinematics before surgery and 12 months following open foveal reinsertion of the triangular fibrocartilage complex: comparison with the contralateral non-injured joint
Janni K THILLEMANN 1,2,3, Sepp DE RAEDT 3,4, Emil T PETERSEN 1,2,3, Katriina B PUHAKKA 5,6, Torben B HANSEN 1,2 and Maiken STILLING 2,3,7
1 Department of Orthopaedics, University Clinic for Hand, Hip and Knee Surgery, Gødstrup Hospital, Herning; 2 Department of Clinical Medicine, Aarhus University; 3 AutoRSA Research Group, Orthopaedic Research Unit, Aarhus University Hospital; 4 NRT X-RAY A/S, Hasselager; 5 Department of Radiology, Aarhus University Hospital; 6 Department of Radiology, Regional Hospital Horsens; 7 Department of Orthopaedic Surgery, Aarhus University, Denmark
Background and purpose — Foveal triangular fibrocartilage complex (TFCC) lesion may cause distal radioulnar joint (DRUJ) instability. Dynamic radiostereometry (dRSA) has been validated for objective measurement of DRUJ kinematics. We evaluated DRUJ kinematics by dRSA before surgery and 12 months following open foveal reinsertion of the TFCC in comparison with contralateral non-injured DRUJs.
Patients and methods — In a prospective cohort study, 21 patients (11 men) of mean age 34 years (22–50) with arthroscopically confirmed foveal TFCC lesion were evaluated preoperatively, and at 6 and 12 months after open foveal TFCC reinsertion with QDASH, PRWE, pain on NRS, and bilateral dRSA imaging during a patient active press test motion cycle, including a force-loaded downstroke and a release phase.
Results — Preoperatively, the force-loaded part (> 2.3 kg; 95% CI 1.6–3.0) of the press test motion cycle (from 15% to 75%) revealed a more volar position of the ulnar head in the sigmoid notch (DRUJ position ratio) and increased distance in DRUJs with foveal TFCC lesion compared with the patients’ contralateral non-injured DRUJ (p < 0.05). 6 months postoperatively, the DRUJ position was generally normalized and remained normalized at 12 months. However, the DRUJ distance remained higher on the injured side. 12 months postoperatively, patients reported less pain during activities, with improved QDASH and PRWE scores (p < 0.007).
Interpretation — DRUJ kinematics during the press test showed increased DRUJ translation to a more volar position of the ulnar head after foveal TFCC lesion compared with the contralateral non-injured DRUJs. Open foveal TFCC reinsertion had a stabilizing effect on DRUJ kinematics towards normalization, and improved patient-reported outcomes 6 and 12 months after surgery.
Citation: Acta Orthopaedica 2022; 93: 574–582. DOI http://dx.doi.org/10.2340/17453674.2022.3141.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-01-05. Accepted: 2022-05-21. Published: 2022-06-21.
Correspondence: teamjanni@gmail.com
JKT, SDR, TBH, and MS designed the study. JKT and MS participated in data acquisition. JKT, KBP, ETP, SDR, and MS analyzed and interpreted data. SDR and MS developed the AutoRSA software used in the work. JKT drafted the manuscript. SDR, KBP, ETP, TBH, and MS critically revised the manuscript. All authors read and approved the final manuscript.
The authors would like to thank radiographer Lars Lindgren from the Department of Radiology, Aarhus University Hospital, and Michael Frosted Mathiasen, from the Department of Radiology, Gødstrup Hospital, Herning, for their valuable help with the radiostereometric recordings.
Acta thanks Stephan Maximilian Röhrl and Maria Wilcke for help with peer review of this study.
The triangular fibrocartilaginous complex (TFCC) is the main stabilizer of the distal radioulnar joint (DRUJ) and lesions may lead to DRUJ instability and ulnar wrist pain during activities. Wrist arthroscopy with a positive Hook test, or DRUJ arthroscopy with direct visualization of a foveal TFCC lesion, have been the diagnostic gold standard for many years (1) as clinical examination of DRUJ stability (Ballottement test) is observer dependent and lacks validity across observers (2). Imaging modalities such as CT have poor agreement with clinical examination (3) and MRI has limited sensitivity and specificity for visualizing TFCC lesions (4). We recently validated a non-invasive highly precise dynamic radiostereometry (dRSA) imaging method for objective measurement of DRUJ kinematics and instability in vivo (5). Foveal TFCC lesions can be treated surgically by open or arthroscopic reinsertion, with similar postoperative results evaluated clinically at follow-up by a radioulnar stress test (i.e., the Ballottement test) (6,7).
We used dRSA to evaluate DRUJ kinematics before surgery and 1-year following open foveal reinsertion of the TFCC in comparison with the contralateral non-injured DRUJs. The hypotheses were that increased DRUJ translation in joints with foveal TFCC lesion and surgical treatment with open foveal reinsertion would normalize DRUJ kinematics. We also report clinical outcomes, and patient-reported outcomes (PROMS).
Patients and methods
Between February 2017 and April 2020, 21 eligible patients were recruited prospectively to the study at Regional Hospital West and Aarhus University Hospital.
The inclusion criteria were age > 18 years, ulnar-sided wrist pain related to a history of trauma, clinical impression of DRUJ instability with the Ballottement test (8), and arthroscopic confirmation of a foveal TFCC lesion as evaluated by the Hook test, which could be classified as repairable (Class 2 or 3) according to Atzei’s classification of TFCC injuries (9). In addition, it was mandatory for intra-subject comparison that the included patients had a contralateral asymptomatic side without any history of pain, wrist or forearm trauma, or previous surgery. The exclusion criteria were pre-existing rheumatoid conditions, wrist or DRUJ osteoarthritis, MRI verified ulnocarpal impaction with ulnar variance > 2 mm, arthroscopically verified intercarpal ligament injury, presence of osteosynthesis material (metal artefacts on bone models), malunion in the case of previous distal radius fracture, previous forearm or elbow fracture, and inability to communicate in Danish. At baseline, patient characteristics including age, sex, hand dominance, side of the injured wrist, and injury mechanism were collected.
Sample size
In a cadaver study, DRUJ translation measured with RSA was 1.36 mm (SD 1.42) with intact TFCC and 2.30 mm (SD 1.07) after lesion of the peripheral TFCC insertions at the styloid and in the fovea (10). Based on 2-sample comparison of paired means, power of 0.90, and alpha of 0.05, a sample size of 12 patients was estimated. Inclusion of 20 patients in the study period was selected to compensate for incomplete data collection, technical issues with imaging, and loss to follow-up.
Clinical examination and patient-reported outcome measures
At baseline, 6-month, and 12-month follow-up, data from clinical examinations and PROMs was recorded by the surgeon (JKT). We used DRUJ translation examined by the Ballottement test to grade DRUJ instability as slight (< 5mm), mild (5–10 mm) or severe (> 10 mm) (11). Grip strength was measured by the DHD-1 digital Hand Dynamometer (SAEHAN Corporation, Gyeongsangnam, South Korea) and active range of motion (AROM) was measured with a goniometer. PROMs included Quick Disabilities of the Arm, Shoulder and Hand (QDASH) (range 0–100, 0 represents no disability) and Patient-Rated Wrist Evaluation (PRWE) (range 0–100, 0 represents no disability and pain). Pain was rated on a numeric rating scale (NRS) at rest and during defined activities (range 0–10, 0 indicates no pain).
CT and MRI imaging
All 21 patients were investigated preoperatively with conventional wrist radiographs of the injured wrist. Bilateral CT scans of the forearm were used to generate individualized 3D bone-volume models and surface models of the radius and ulna by segmentation (Kitware, New York, USA) (5). The 3D bone models were used for simulation of 2D digital reconstructed radiographs (DRR) and analysis of dRSA recordings. This enables in vivo estimation of joint kinematics using anatomical landmarks and axes (Figure 1) (5). Preoperative MRI of the patient’s symptomatic wrist was performed for evaluation of (i) foveal TFCC tear (positive), (ii) no tear detected but abnormal “signal” with peripheral edema (uncertain), and (iii) other competing injuries by an experienced consultant radiologist (KBP). MR sequences and scanner details are available (Table 1, see Supplementary data).
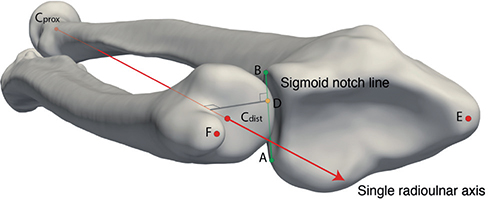
Figure 1. Bony landmarks, bone axis, and kinematic outcome measures on CT-based bone models. The sigmoid notch (SN) line connects the midpoint of the volar (landmark A) and dorsal (landmark B) radius sigmoid notch rims. The axis of rotation in the forearm was defined as the radioulnar joint axis (RUJ axis) extending thorough the radial head center (Cprox) to the ulnar head center (Cdist) (33). The forearm rotation was defined as the angle between a plane formed from the radial head center (Cprox), the ulnar head center (Cdist) to the ulnar styloid (F), and the plane formed from the Cprox, the radial styloid E, and the midpoint of the sigmoid notch line. The position of the ulnar head center in the sigmoid notch (DRUJ position = yellow ball) was estimated by orthogonal projection of the RUJ axis on the sigmoid notch line and measured in mm from the volar sigmoid notch rim. Considering the individual differences of bone sizes and sigmoid notch length, the DRUJ position ratio was calculated (DRUJ position ratio = DRUJ position/SN length). Translation in the DRUJ was calculated as the change of DRUJ position in mm. Change of ulnar variance was calculated as movement of Cdist along the RUJ axis with respect to the SN line midpoint and, finally, DRUJ distance was estimated as the orthogonal projected distance (grey line) from the RUJ axis to the SN line (AB).
Press test setup and dynamic RSA
A custom-made weight platform recorded the applied force (kg) during a standardized press test performed by the patients, as related dRSA images were recorded digitally at an image rate of 10 Hz (Adora RSA system, NRT X-Ray, Hasselager, Denmark) (Figure 2) (5). We conducted preoperative bilateral press test double examinations to test the dRSA repeatability. At 6-month and 12-month follow-up, dRSA imaging of the press test was repeated on the injured side. An averaged calibration image from all dRSA images was compiled by custom-made software and model-based RSA software was used for calibration (MBRSA 4.11, RSAcore, Leiden, Netherlands). The DRR was manually initialized to approximately fit the initial image of the dRSA recording prior to automated radiostereometric analysis (AutoRSA software, Orthopaedic Research Unit, Aarhus, Denmark) (12). The AutoRSA software was used to estimate the 3D bone position and orientation in the calibration box coordinate system, which was later transformed into individual anatomical coordinate systems of the radius and ulna defined from anatomical landmarks on the individual 3D bone-surface models (5).

Figure 2. Dynamic radiostereometric setup during press test application. The patients were positioned with shoulder adduction, elbow flexion, and the approximately 90° pronated forearm resting in the horizontal plane with the hand flat on a custom-made weight platform logging the force (kg) gradually applied by the patients to their maximum, and released gradually, to no force, to induce dorso-volar directed translation of the ulnar head. A custom-made Raspberry Pi was used to timestamp dynamic radiostereometric image recordings (dRSA) (10 Hz), and further to record and relate the dRSA images and the force applied on the weight platform. The press test was performed during by 2 ceiling mounted X-ray tubes with 20°–20° tube position on the vertical plane, projecting on 2 digital image detectors (Canon CXDI-50RF) slotted beneath a uniplanar carbon box (Carbon box 24, Medis Specials, Leiden, The Netherlands). The source to image distance (SID) was 150 cm and the source to skin distance (SSD) was 100 cm. The exposures were 60kV, 630 mA, and 2.0 ms exposure time for acquiring a resolution of 2208 x 2688 pixels resolution (0.16 x 0.16 mm/pixel). Images were exported as multi-frame DICOM files.
Arthroscopic evaluation and TFCC surgery
Stability of the foveal TFCC insertion was assessed arthroscopically by the Hook test through a 6-R portal. Open foveal TFCC reinsertion was performed with exposure of the DRUJ through a dorsal skin incision via the 5th extensor compartment. Through an L-shaped capsular opening proximal to the dorsal radioulnar ligament, DRUJ synovitis was removed in the ulnar fovea and a 2–0 suture anchor inserted (Mitek Mini Quickanchor, DePuy Syntes, Raynham, MA, USA). The distal side of the TFCC was approached through a 1 cm transverse incision in the wrist capsule. The TFCC was reinserted to the ulnar fovea with a mattress suture (5 knots) while compressing the DRUJ positioned in neutral forearm rotation. The dorsal capsule was closed with 3–0 absorbable braided sutures before closure of the skin. An above-elbow back-slap cast was applied.
Rehabilitation program and follow-up
The above elbow cast was worn for 6 weeks. Thereafter, a removable wrist splint was used for another 4 weeks during a protocolled staged 3-month rehabilitation program supervised by an occupational therapist. The aim was normalization of the upper extremity AROM and strength. 8 weeks postoperatively the treatment involved also proprioceptive and neuromuscular wrist exercises. 10 weeks postoperatively, increasing loads were allowed and neuromuscular wrist strengthening increased, and splinting was recommended only during risk activities. 6 months after surgery, unlimited use was allowed if tolerated.
Kinematic outcomes and data management
We used bony landmarks to define the individual radioulnar joint (RUJ) axis of forearm rotation and to estimate the kinematic outcomes. The kinematic outcomes were DRUJ translation (primary outcome), DRUJ position ratio, DRUJ distance, and change in ulnar variance (pistoning) (Figure 1) (5).
The press test examination with the highest applied force during a motion cycle was chosen for data analysis. Customized software was used to handle individual differences in timing of force application. Each motion cycle was split in a downstroke and a release phase at the point of maximum force, defined as the 50% mark of the motion cycle. Linear interpolation was used to construct new data points (percentage of the motion cycle with 5% increment) from the known RSA image numbers and to estimate new time-normalized force data and related kinematic outcome data (5).
Statistics
We assessed normality of the data distribution by probability plots. Data following a normal distribution was reported with 95% confidence intervals (CI) and data with non-normal distribution was reported as median values with (IQR).
In order to evaluate hypotheses of no difference of grip strength and AROM variables in the non-injured compared with the foveal TFCC injured DRUJ, at the preoperative stage, we used paired 2-tailed Student’s t-test for statistical comparison of paired normally distributed data, and the Wilcoxon signed-rank test was used in the case of paired data with a non-normal data distribution. Hypotheses regarding repeated measures on the injured side including grip strength, AROM, QDASH, and PRWE were tested using ANOVA repeated measurement analyses. For evaluation of hypotheses regarding variables in contingency tables (Ballottement test), the chi-square test was used.
Time-normalized DRUJ kinematic data during the press test motion cycle was reported as DRUJ translation, DRUJ position ratio, DRUJ distance, and pistoning. The hypothesis of no difference was analyzed using univariate repeated measurement analysis (mixed model), with percentage of the motion cycle, injury status (non-injured/injured at baseline/6 months/12 months), and side (non-injured/injured) as fixed effects, and patient and side as random effects. We used pairwise group comparisons for each percentage of the motion cycle to describe differences. Unequal standard deviations and correlations of the non-injured/injured side were considered in the analyses. Normal distribution of the mixed-model residuals was tested by Q–Q plots.
Repeatability of dRSA press test double examinations was estimated and reported as absolute mean differences (SD) and prediction intervals (1.96 x SD). The dRSA double examinations were used to determine the intraclass correlation coefficients (ICC) based on an assumption of a single rater (interrater agreement), absolute greement, and 2-way mixed-effects model (ICC 2,1). We used Stata 16 (StataCorp, College Station, TX, USA) for statistical analysis. The statistical significance was set at p < 0.05.
Ethics, registration, funding, and potential conflict of interests
The study was conducted in accordance with the Helsinki guidelines and patients gave their informed consent to participate. Study approval was given by the Central Denmark Region Committees on Health Research Ethics (j.no.1–10–72–146–16, August 2016). This research has received grants from the Health Research Fund of Central Denmark Region, Aarhus University, the Danish Rheumatism Association, and Innovation Fund Denmark (Grant 69-2013-1). Funding sources had no influence on data interpretation and presentation. The authors have no conflicts of interest.
Results
Demographics of the patient cohort are presented in Table 2. At 12-month follow-up 2 patients had left the study, 1 due to new trauma and fracture of the scaphoid, and another who withdrew from the study.
Clinical examination (Table 3)
On the TFCC-injured side, the preoperative AROM was decreased by 8° (CI 4–12) of flexion and 7° (CI 2–11) of extension (p < 0.004), and the grip strength was a mean 5.7 kg (CI 1.8–9.6) less, in comparison with the contralateral non-injured side (p = 0.006).
| Factor | Non-injured (n = 21) | TFCC lesion | p-value a | p-value b | ||
| Preoperative (n = 21) | 6 months (n = 19) | 12 months (n = 19) | ||||
| Women/men, n | 10/11 | 10/11 | 8/11 | 8/11 | ||
| Grip strength total (kg) 45 (39–51) | 39 (32–47) | 36 (30–42) | 39 (32–47) | 0.006 | 0.04 c | |
| Women | 33 (29–38) | 25 (20–30) | 23 (17–29) | 25 (17–33) | 0.002 | 0.3 |
| Men | 56 (52–60) | 52 (46–58) | 48 (44–51) | 52 (46–59) | 0.3 | 0.05 c |
| Wrist AROM (°) | ||||||
| Flexion | 78 (73–82) | 70 (65–76) | 67 (62–72) | 68 (62–73) | 0.001 | 0.6 |
| Extension | 74 (70–78) | 67 (61–73) | 68 (64–72) | 66 (61–71) | 0.004 | 0.6 |
| Radial deviation | 22 (19–25) | 20 (17–24) | 18 (16–20) | 19 (17–22) | 0.01 | 0.1 |
| Ulnar deviation | 37 (34–40) | 33 (29–37) | 28 (25–30) | 32 (28–37) | 0.01 | 0.02 d |
| Forearm rotation (°) | ||||||
| Supination | 84 (81–87) | 78 (75–82) | 76 (72–80) | 74 (70–78) | 0.001 | 0.2 |
| Pronation | 81 (77–85) | 79 (74–83) | 77 (73–81) | 79 (75–83) | 0.04 | 0.5 |
| Ballottement test, n e | 21/0/0 | 0/15/6 | 13/6/0 | 13/6/0 | 0.00 | < 0.01 |
| DRUJ: distal radioulnar joint, AROM: active range of motion, TFCC: triangular fibrocartilage complex. | ||||||
| a Preoperative comparison between the healthy arm and the foveal TFCC injury arm. | ||||||
| b Comparison of the foveal TFCC injury arm over time, from preoperative, to 6-month and 12-month. | ||||||
| c Statistically significant difference between 6-month and 12-month follow-up. | ||||||
| d Statistically significant difference between preoperative and 6-month follow-up. | ||||||
| e Clinical evaluation of DRUJ stability: Slight (< 5 mm)/mild (5–10 mm)/severe instability (> 10 mm). | ||||||
12 months after surgery, grip strength had improved towards the preoperative level but did not reach the level of the contralateral non-injured side. Clinical grading of DRUJ stability evaluated by the Ballottement test improved after surgical treatment.
Patient-reported outcomes (Table 4, Figure 3)
At 12-month follow-up, a statistically significant and clinically relevant reduction in patient-reported outcomes was found. The QDASH score improved 14 points (CI 7–21) (13). The total PRWE improved 21 points (CI 13–28) (14). During activities a clinically relevant pain reduction of 2 NRS points was present after surgical treatment (15,16).
| Factor | Preoperative (n = 21) | 6 months (n = 19) | 12 months (n = 19) | p-value a |
| QDASH preop | 39 (31–47) | 29 (22–36) | 25 (16–34) | < 0.001 b |
| Pain PRWE | 29 (25–33) | 17 (14–20) | 18 (13–23) | < 0.001 b |
| Function PRWE | 20 (15–24) | 12 (8–15) | 10 (6–14) | < 0.001 b |
| Total PRWE | 49 (41–57) | 29 (23–35) | 28 (19–37) | < 0.001 b |
| TFCC: triangular fibrocartilage complex, QDASH: Quick Disabilities of the Arm, Shoulder and Hand, PRWE: patient-rated wrist evaluation. | ||||
| a Comparison of the foveal TFCC injury arm over time, from preoperative, to 6-month and 12-month follow-up. | ||||
| b Statistically significant difference between preoperative and 6-month follow-up in the foveal TFCC-injured wrist. | ||||
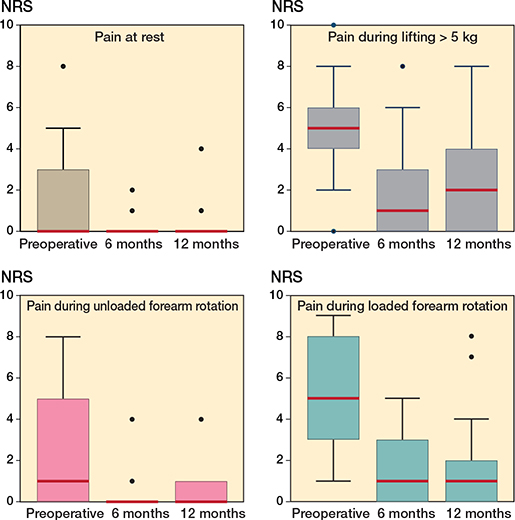
Figure 3. Patient-reported pain on numeric rating scale in patients with foveal TFCC injury. Boxplots of the patient reported pain at rest, during lifting more than 5 kg, with loaded and unloaded forearm rotation, from the preoperatively throughout the 6-month and 12-month follow-up. Boxplots display median pain, with interquartile ranges (IQR), whiskers (1.5 x IQR), and outliers.
MRI
The sensitivity of diagnosing a foveal TFCC lesion by MRI was 33% and increased to 71% when peripheral edema detected around the foveal TFCC insertion was included and regarded as a sign of foveal TFCC lesion.
Dynamic DRUJ Kinematics (Table 5, Figure 4 and 5, and Video, see link in Supplementary data)
The precision of DRUJ kinematics at maximum force was comparable for the TFCC-injured side and the contralateral non-injured side (p > 0.3) and within prediction intervals of < 0.62 mm. The ICC rater consistency was excellent (r > 0.90) (Table 6, see Supplementary data). Throughout the entire press test motion cycle, similar force (up to 0.9 kg mean difference) was applied by the TFCC-injured side and the contralateral non-injured side at all follow-up times (p > 0.7). Pain triggered during the press test did not reach a clinically relevant level compared with the pain-free contralateral side.
| Factor | Non-injured (n = 21) | TFCC lesion | p-value a | p-value b | ||
| Preoperative (n = 21) | 6 months (n = 19) | 12 months (n = 19) | ||||
| Sigmoid notch size (mm) | 13.4 (12.9–14.0) | 13.7 (13.0–14.4) | – | – | 0.6 | |
| At 0% of the motion cycle | ||||||
| Forearm pronation (°) | 61 (56–67) | 59 (54–65) | 60 (55–65) | 59 (54–64) | 0.6 | 0.5 |
| DRUJ position ratio | 0.72 (0.68–0.76) | 0.68 (0.61–0.75) | 0.69 (0.62–0.75) | 0.70 (0.63–0.77) | 0.3 | 0.5 |
| DRUJ distance (mm) | 9.9 (9.4–10.4) | 10.6 (10.0–11.1) | 10.6 (10.0–11.1) | 10.7 (10.1–11.2) | 0.07 | 0.2 |
| At 50% of the motion cycle | ||||||
| Forearm pronation (°) | 52 (47–58) | 50 (44–57) | 54 (49–59) | 53 (48–59) | 0.6 | 0.2 |
| Maximum force in kg | 6.7 (5.6–7.7) | 6.9 (5.7–8.1) | 7.4 (6.2–8.6) | 7.5 (6.0–9.1) | 0.7 | 0.7 |
| DRUJ position ratio | 0.39 (0.34–0.44) | 0.29 (0.21–0.37) | 0.32 (0.24–0.39) | 0.31 (0.22–0.40) | 0.01 | 0.5 |
| DRUJ distance (mm) | 9.1 (8.5–9.7) | 10.6 (9.9–11.4) | 10.5 (9.9–11.2) | 10.5 (9.7–11.2) | 0.002 | 0.2 |
| From 0% to 50% of the motion cycle | ||||||
| DRUJ translation (mm) | 4.4 (3.9–5.0) | 5.3 (4.4–6.1) | 5.1 (4.3–5.8) | 5.3 (4.5–6.1) | 0.09 | 0.7 |
| Increase in ulnar variance (mm) | 1.14 (0.95–1.32) | 0.96 (0.75–1.07) | 0.94 (0.74–1.13) | 1.03 (0.85–1.2) | 0.1 | 0.3 |
| Pain on NRS during RSA press test, | ||||||
| median (IQR) | 0 (0–0) | 1 (0–4) | 0 (0–1) | 0 (0– 0) | ||
| DRUJ: Distal radioulnar joint, TFCC: triangular fibrocartilage complex, IQR: interquartile range, FU: follow-up. | ||||||
| a Preoperative comparison of non-injured DRUJs and DRUJs with foveal TFCC lesion. | ||||||
| b Comparison of DRUJs with foveal TFCC lesion over time. | ||||||
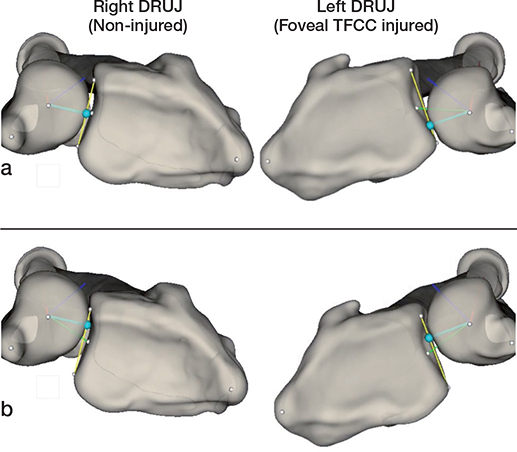
Figure 4. Example of DRUJ kinematics during the press test. The applied force resulted in volar ulnar head translation and DRUJ gapping on the (left) DRUJ with foveal TFCC injury compared with the (right) non-injured DRUJ: (a) maximal force after downstroke on the weight platform and (b) after release.
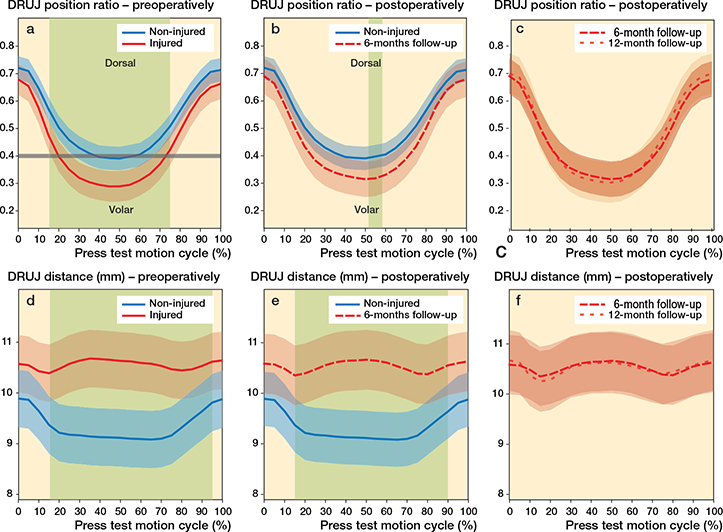
Figure 5. Dynamic kinematic outcomes including mean distal radioulnar joint position ratio (DRUJ position ratio) and mean distal radioulnar joint distance (DRUJ distance) during the press test. Preoperative (solid line) and postoperative (dashed lines) comparison of the mean DRUJ position ratio (a–c) and DRUJ distance (mm) (d–f) of patient DRUJs with foveal TFCC lesion (red) and the contralateral non-injured DRUJ (blue). Graphs display means with 95% confidence intervals. Mixed model statistics was used to define intervals of the press test motion cycle with significant differences (displayed as light green areas). The DRUJ position ratio resembles the position of the ulnar head center in the sigmoid notch (0 indicates the most volar position and 1 indicates the most dorsal position). The DRUJ distance increased (d) as the DRUJ position ratio was below the 0.4 level (grey line) (a).
The preoperative DRUJ translation during the downstroke phase was a mean 5.3 mm (CI 4.4–6.1) in DRUJs with TFCC lesion and mean 4.4 mm (CI 3.9–5.0) in the contralateral non-injured DRUJ (p = 0.09). The preoperative DRUJ position ratio in DRUJs with TFCC injury was smaller (more volar position) compared with the contralateral non-injured DRUJ (p < 0.05) in the most force-loaded phase (mean force > 2.3 kg; CI 1.6–3.0) of downstroke and release (15% to 75% of the motion cycle). At maximum force, the ulnar head translated more volarly, in the DRUJs with foveal TFCC injury, compared with the contralateral non-injured DRUJs, as the DRUJ translation was increased by 0.82 mm (CI 0.03–1.61) and the DRUJ position ratio changed 10 percentage points (CI 2–18).
At 6-month follow-up, no statistically significant difference in DRUJ position ratio throughout the press test motion cycle was present when comparing the TFCC-injured DRUJs and the contralateral non-injured DRUJs (p > 0.06), except at 55% of the motion cycle when the release phase was initiated. The kinematic pattern after TFCC reinsertion normalized towards the kinematic pattern of the contralateral non-injured DRUJs and was unchanged 12 months after surgery (p > 0.4).
The DRUJ distance decreased as the press test motion cycle was initiated (0% to 15% of the press test motion cycle), regardless of the presence of a TFCC injury. Thereafter, the DRUJ distance reduced further in the contralateral non-injured DRUJs as the mean DRUJ position of the ulnar head was centered in the sigmoid notch, but the DRUJ position ratio remained above a level of 0.4 until the force was released. Conversely, the DRUJ distance in wrists with foveal TFCC lesion was higher until 75% of the press test motion cycle, where the ulnar head was below the DRUJ position ratio level of 0.4.
At maximum force, the preoperative difference in DRUJ distance between the TFCC-injured side and the contralateral non-injured DRUJ was 1.5 mm (CI 0.6–2.4) (p = 0.002). Surgical treatment did not change the pattern of the DRUJ distance at 6-month or 12-month follow-up (p > 0.2).
Discussion
The most important kinematic difference between DRUJs with foveal TFCC injury compared with the contralateral non-injured side was an increased DRUJ volar translation of 0.82 mm (CI 0.03–1.61) resulting in a 10 percentage points (CI 2–18) more volar DRUJ position ratio during maximum pressure. As the individual variation in distal radius size and sigmoid notch length is an important factor for comparison of DRUJ translation, we previously recommended evaluation of DRUJ instability using the DRUJ position ratio (5). Despite dRSA being a highly precise method and the fact that the press test has excellent repeatability in both non-injured and foveal TFCC-injured DRUJ (Table 6, see Supplementary data), the difference in DRUJ position ratio between foveal TFCC-injured DRUJs and the contralateral non-injured DRUJ had broad variation (CI ranging from 2 to 18 percentage points). This is likely due to inter-individual differences of DRUJ stability in normal joints. Therefore, paired comparisons between the normal side and the injured side may be important to evaluate a clinically relevant difference in DRUJ instability. This was also recommended by Hess et al., who utilized sonography for measurement of DRUJ translation during a press test. Hess et al. suggested a 1 mm difference in DRUJ translation between the injured DRUJ and the contralateral side, to indicate instability (17). Thus, a clinically relevant difference may be closer to the CI upper limit of the difference in DRUJ translation and DRUJ position ratio reported in this study. Dynamic RSA evaluates only the bony translation, while other methods typically include soft tissue motion and show larger translation values. Therefore, direct comparison between DRUJ translation measured with dRSA in the present study and DRUJ translation measured with less precise methods in other experimental (18-20) and clinical studies (17,21) is not feasible. However, examination of a larger patient cohort may decrease the variation and show more clearly a DRUJ translation threshold between foveal injured DRUJs and DRUJs with a normal TFCC.
The articular incongruency of the DRUJ, with the small ulnar head and greater sigmoid notch, makes it inherently unstable. Previous clinical findings of dorsal prominence of the ulnar head on lateral radiographs (22) and axial CT scans (23) have been taken as indicators of an unstable DRUJ. However, in unloaded pronation, the DRUJ position ratio evaluated by dRSA did not indicate dorsal ulnar head prominence in DRUJs with foveal TFCC injury compared with the contralateral non-injured DRUJs. This supports the notion that DRUJ instability can present both as a dorsal and volar instability, depending on whether the volar or dorsal limb of the foveal TFCC component was torn. Further stratification of instability patterns needs clarification in future kinematic studies.
The DRUJ stabilizers allow for complex joint motions including forearm rotation, longitudinal pistoning, and anteroposterior translation, but gapping is not expected in the stable DRUJ as the TFCC provides a compressive force perpendicular to the articular surface. In unstable DRUJs, gross joint gapping can be detected on plain posteroanterior radiographs or by clenched fist radiographs (24). However, sub-millimeter differences between non-injured and injured arms with foveal TFCC lesion may not be visible. We reported increased DRUJ distance during the press test in DRUJs with foveal TFCC lesion. Moreover, this may reflect gliding of the ulnar head onto the volar rim of the radius sigmoid notch, as the DRUJ position ratio decreases below the 0.4 level, rather than increased distance between the articulating surfaces of the DRUJ. To evaluate DRUJ distance, future studies using proximity mapping may be useful for mapping the contact point during movement and for estimating the DRUJ distance of the closest articulating surfaces. However, DRUJ distance may be a good measure of altered kinematics following surgical treatment. Yet, the long-term consequences of non-normal DRUJ kinematics are not known but may potentially lead to arthritis.
In general, studies on the surgical effect of foveal TFCC reinsertion are evaluated by clinical examination of stability (25). Frequently, the Ballottement test is used for this clinical DRUJ stability assessment but suffers from subjectivity and has poor (2) to moderate inter-observer agreement (26). Further, a positive Ballottement test is correlated to DRUJ instability, but the sensitivity of diagnosing foveal TFCC injuries in comparison with arthroscopic findings was only moderate (sensitivity 59%) (27). Thus, clinical examination of surgical outcomes of DRUJ stability is a biased and uncertain outcome measure.
To our knowledge, our study is the only publication that presents dynamic kinematic patterns of the DRUJ before and after TFCC stabilizing surgery compared with the normal values on the contralateral non-injured DRUJ. We found a statistically significant difference in DRUJ position ratio and DRUJ distance during the loaded phase of the press test motion cycle. Open foveal reinsertion improved the PROMs at 12-month follow-up and had a normalizing effect on the DRUJ position ratio kinematics, but the level of the non-injured contralateral arms was not reached. It is unknown how well the reinserted TFCC footprint heals to the bony ulnar fovea. To our knowledge no studies with arthroscopic confirmation of TFCC healing exist.
Arthroscopic foveal TFCC reinsertion is used increasingly, and numerous techniques have been proposed to achieve an anatomical footprint at the TFCC reinsertion site (11,28-31). However, the objective stabilizing effect on DRUJ kinematics after open and arthroscopic foveal TFCC reinsertion has not yet been compared. Rather, similar clinically evaluated stability and frequency of surgical failure (DRUJ re-instability) has been shown repeatedly (6,7,32). The only randomized study to compare osseous foveal TFCC repair techniques by open versus arthroscopic techniques presented similar improvement in clinical outcomes and recurrence of DRUJ instability (evaluated by the Ballottement test). However, substantial differences were found in PROM improvements including pain and DASH score, favoring arthroscopic treatment (7).
Strengths and limitations
We validated dRSA as a precise non-invasive dynamic imaging method that has the advantage of excluding examination bias from the clinician. Further, dRSA captures the kinematic endpoints if recorded by a sufficiently high image frequency (Hz). However, the patient may be unable to present his/her maximum instability due to reflective muscle contraction upon loading.
The DRUJ distance was evaluated as the projected perpendicular distance from the ulnar fovea and RUJ axis to the sigmoid notch line. Thus, the gapping between joint surfaces of the DRUJ is not portrayed by this study. Further, the press test may not be the most ideal examination to display kinematics in unstable DRUJs. Dynamic RSA can also be utilized to examine, e.g., forced forearm rotation, but new tests require new validation.
In conclusion, dRSA for assessment of DRUJ kinematics during the press test showed increased DRUJ translation after foveal TFCC lesion compared with the contralateral non-injured DRUJs, and a DRUJ stabilization towards normal values 6 months and 12 months after open foveal TFCC reinsertion. The clinical relevance thereof is supported by reduced pain during activity and improvement of QDASH and PRWE scores at 12-month follow-up. Dynamic RSA may help to identify the most effective treatments.
- Ruch D S, Yang C C, Smith B P. Results of acute arthroscopically repaired triangular fibrocartilage complex injuries associated with intraarticular distal radius fractures. Arthroscopy 2003; 19: 511-16.
- Jupiter J B. Commentary: the effect of ulnar styloid fractures on patientrated outcomes after volar locking plating of distal radius fractures. J Hand Surg Am 2009; 34: 1603-4.
- Kim J P, Park M J. Assessment of distal radioulnar joint instability after distal radius fracture: comparison of computed tomography and clinical examination results. J Hand Surg Am 2008; 33: 1486-92.
- Boer B C, Vestering M, van Raak S M, van Kooten E O, Huis In ’t Veld R, Vochteloo A J H. MR arthrography is slightly more accurate than conventional MRI in detecting TFCC lesions of the wrist. Eur J Orthop Surg Traumatol 2018; 28: 1549-53.
- Thillemann J K, De Raedt S, Petersen E T, Puhakka K B, Hansen T B, Stilling M. Normal values of distal radioulnar joint kinematics during a dynamic press test. J Wrist Surg 2021. doi: 10.1055/s-0041-1740486.
- Andersson J K, Ahlen M, Andernord D. Open versus arthroscopic repair of the triangular fibrocartilage complex: a systematic review. J Exp Orthop 2018; 5: 6.
- Luchetti R, Atzei A, Cozzolino R, Fairplay T, Badur N. Comparison between open and arthroscopic-assisted foveal triangular fibrocartilage complex repair for post-traumatic distal radio-ulnar joint instability. J Hand Surg Eur 2014; 39: 845-55.
- Kleinman W B. Stability of the distal radioulna joint: biomechanics, pathophysiology, physical diagnosis, and restoration of function what we have learned in 25 years. J Hand Surg Am 2007; 32: 1086-1106.
- Atzei A, Luchetti R. Foveal TFCC tear classification and treatment. Hand Clin 2011; 27: 263-72.
- Thillemann J K, De Raedt S, Jorgensen P B, Romer L, Hansen T B, Stilling M. Distal radioulnar joint stability measured with radiostereometry during the piano key test. J Hand Surg Eur 2020; 45: 923-30.
- Atzei A, Rizzo A, Luchetti R, Fairplay T. Arthroscopic foveal repair of triangular fibrocartilage complex peripheral lesion with distal radioulnar joint instability. Tech Hand Up Extrem Surg 2008; 12: 226-35.
- Christensen R, Petersen E T, Jurgens-Lahnstein J, Rytter S, Lindgren L, De Raedt S, et al. Assessment of knee kinematics with dynamic radiostereometry: validation of an automated model-based method of analysis using bone models. J Orthop Res 2021; 39: 597-608.
- Sorensen A A, Howard D, Tan W H, Ketchersid J, Calfee R P. Minimal clinically important differences of 3 patient-rated outcomes instruments. J Hand Surg Am 2013; 38: 641-9.
- Kim J K, Park E S. Comparative responsiveness and minimal clinically important differences for idiopathic ulnar impaction syndrome. Clin Orthop Relat Res 2013; 471: 1406-11.
- Farrar J T, Young J P
Jr , LaMoreaux L, Werth J L, Poole M R. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001; 94: 149-58. - Salaffi F, Stancati A, Silvestri C A, Ciapetti A, Grassi W. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur J Pain 2004; 8: 283-91.
- Hess F, Farshad M, Sutter R, Nagy L, Schweizer A. A novel technique for detecting instability of the distal radioulnar joint in complete triangular fibrocartilage complex lesions. J Wrist Surg 2012; 1: 153-8.
- Omokawa S, Iida A, Kawamura K, Nakanishi Y, Shimizu T, Kira T, et al. A biomechanical perspective on distal radioulnar joint instability. J Wrist Surg 2017; 6: 88-96.
- Onishi T, Omokawa S, Iida A, Nakanishi Y, Kira T, Moritomo H, et al. Biomechanical study of distal radioulnar joint ballottement test. J Orthop Res 2017; 35: 1123-7.
- Iida A, Omokawa S, Moritomo H, Omori S, Kataoka T, Aoki M, et al. Effect of wrist position on distal radioulnar joint stability: a biomechanical study. J Orthop Res 2014; 32: 1247-51.
- Pickering G T, Nagata H, Giddins G E B. In-vivo three-dimensional measurement of distal radioulnar joint translation in normal and clinically unstable populations. J Hand Surg Eur 2016; 41: 521-6.
- Nakamura R, Horii E, Imaeda T, Tsunoda K, Nakao E. Distal radioulnar joint subluxation and dislocation diagnosed by standard roentgenography. Skeletal Radiol 1995; 24: 91-4.
- Lo I K, MacDermid J C, Bennett J D, Bogoch E, King G J. The radioulnar ratio: a new method of quantifying distal radioulnar joint subluxation. J Hand Surg Am 2001; 26: 236-43.
- Iida A, Omokawa S, Akahane M, Kawamura K, Takayama K, Tanaka Y. Distal radioulnar joint stress radiography for detecting radioulnar ligament injury. J Hand Surg Am 2012; 37: 968-74.
- Robba V, Fowler A, Karantana A, Grindlay D, Lindau T. Open versus arthroscopic repair of 1B ulnar-sided triangular fibrocartilage complex tears: a systematic review. Hand (N Y) 2020; 15: 456-64.
- Lindau T, Runnquist K, Aspenberg P. Patients with laxity of the distal radioulnar joint after distal radial fractures have impaired function, but no loss of strength. Acta Orthop Scand 2002; 73: 151-6.
- Lindau T, Adlercreutz C, Aspenberg P. Peripheral tears of the triangular fibrocartilage complex cause distal radioulnar joint instability after distal radial fractures. J Hand Surg Am 2000; 25: 464-8.
- Iwasaki N, Minami A. Arthroscopically assisted reattachment of avulsed triangular fibrocartilage complex to the fovea of the ulnar head. J Hand Surg Am 2009; 34: 1323-6.
- Nakamura T, Sato K, Okazaki M, Toyama Y, Ikegami H. Repair of foveal detachment of the triangular fibrocartilage complex: open and arthroscopic transosseous techniques. Hand Clin 2011; 27: 281-90.
- Shinohara T, Tatebe M, Okui N, Yamamoto M, Kurimoto S, Hirata H. Arthroscopically assisted repair of triangular fibrocartilage complex foveal tears. J Hand Surg Am 2013; 38: 271-7.
- Kermarrec G, Cohen G, Upex P, Fontes D. Arthroscopic foveal reattachment of the triangular fibro cartilaginous complex. J Wrist Surg 2020; 9: 256-62.
- Anderson M L, Larson A N, Moran S L, Cooney W P, Amrami K K, Berger R A. Clinical comparison of arthroscopic versus open repair of triangular fibrocartilage complex tears. J Hand Surg Am 2008; 33: 675-82.
- Hagert C G. The distal radioulnar joint in relation to the whole forearm. Clin Orthop Relat Res 1992; (275): 56-64.
Supplementary data
VIDEO
Video can be viewed through this link: LINK TO VIDEO FILE
| Factor | Systematic bias (mean difference) | p-value a | Prediction | ||
| Precision (SD) | Interval (SD x 1.96) | ICC b | |||
| Maximum force (kg) | |||||
| Non-injured | 0.74 (0.43–1.06) | 0.8 | 0.69 | 1.35 | 0.89 (0.75–0.95) |
| Foveal TFCC injury | 0.80 (0.48–1.12) | 0.70 | 1.38 | 0.93 (0.80–0.97) | |
| DRUJ translation (mm) | |||||
| Non-injured | 0.32 (0.25–0.38) | 0.9 | 0.14 | 0.28 | 0.96 (0.91–0.98) |
| Foveal TFCC injury | 0.30 (0.16–0.44) | 0.31 | 0.62 | 0.97 (0.94–0.99) | |
| DRUJ position ratio | |||||
| Non-injured DRUJ | 0.02 (0.01–0.03) | 0.8 | 0.014 | 0.03 | 0.97 (0.93–0.99) |
| Foveal TFCC injury | 0.02 (0.01–0.04) | 0.030 | 0.06 | 0.98 (0.94–0.99) | |
| Ulnar variance (mm) | |||||
| Non-injured DRUJ | 0.09 (0.06–0.13) | 0.3 | 0.07 | 0.14 | 0.95 (0.88–0.98) |
| Foveal TFCC injury | 0.12 (0.08–0.16) | 0.09 | 0.18 | 0.91 (0.79–0.96) | |
| DRUJ distance (mm) | |||||
| Non-injured DRUJ | 0.30 (0.18–0.43) | 0.3 | 0.28 | 0.55 | 0.84 (0.52–0.94) |
| Foveal TFCC injury | 0.23 (0.15–0.31) | 0.18 | 0.35 | 0.97 (0.93–0.99) | |
| DRUJ: distal radioulnar joint, TFCC: triangular fibrocartilage complex. | |||||
| a Paired t-test | |||||
| b Intraclass coefficient: ICC (2,1) rater consistency between 1st and 2nd examination was calculated as 2-way mixed effects, absolute agreement displayed with 95% confidence intervals. | |||||