Return to work following anterior cruciate ligament reconstruction
Anssi ARIMAA 1, Jani KNIFSUND 1, Heli KESKINEN 1, Mika KIVIMÄKI 2–4, Ville AALTO 2, Tuula OKSANEN 5, Keijo MÄKELÄ 1, Jussi VAHTERA 6,7,a, and Petteri LANKINEN 1,8,a
1 Department of Orthopedics and Traumatology Turku, Turku University Hospital and University of Turku, Turku, Finland; 2 Finnish Institute of Occupational Health, Helsinki, Finland; 3 Clinicum, Faculty of Medicine, University of Helsinki, Helsinki, Finland; 4 Department of Epidemiology and Public Health, University College London, London, UK; 5 Institute of Public Health and Clinical Nutrition, University of Eastern Finland, Kuopio, Finland; 6 Department of Public Health, University of Turku, Turku, Finland; 7 Centre for Population Health Research, University of Turku and Turku University Hospital; Turku, Finland; 8 Satasairaala Central Hospital, Pori, Finland.
a Joint senior authors.
Background and purpose — Amongst people of working age, the return to work (RTW) after anterior cruciate ligament (ACL) reconstruction is an important marker of success of surgery. We determined when patients are able to return to work after ACL reconstruction and identified factors that are associated with the timing of RTW.
Patients and methods — We used logistic regression analyses to examine patient-related factors that may be associated with the length of RTW (above vs. below the median 59 days) after arthroscopic ACLR in a large cohort of patients working in the public sector in Finland (n = 803; n = 334 male, n = 469 female; mean age 41 years [SD 8.6]).
Results — The mean length of RTW was 65 days (SD 41). Higher odds ratios (OR) were observed for age groups 40–49 and ≥ 50 years compared with ≤ 30 years old (OR 2.0, 95% confidence interval 1.3–3.1 and 2.0, 1.2–3.4, respectively); for lower level non-manual and manual work compared with higher level non-manual work (3.0, 2.0–4.3 and 4.9, 3.4–7.0, respectively); and for those who had been on sick leave > 30 days in the preceding year (2.0, 1.4–2.9). Sex, comorbid conditions, preceding antidepressant treatment and concomitant procedures were not associated with the length of RTW.
Interpretation — Factors associated with prolonged sick leave beyond the median time of 59 days are higher age, lower occupational status, and preoperative sick leaves.
Citation: Acta Orthopaedica 2022; 93: 554–559. DOI http://dx.doi.org/10.2340/17453674.2022.3139.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-01-11. Accepted: 2022-05-17. Published: 2022-06-14.
Correspondence: Anssi.arimaa@tyks.fi
All authors contributed to the study design, interpretation of the results, and writing and editing of the manuscript. AA, VA, and PL contributed to the data collection. All authors revised and approved the manuscript.
Acta thanks Jon Olav Drogset and Alejandro Ignacio Marcano for help with peer review of this study.
Anterior cruciate ligament (ACL) injury is one of the most common knee injuries affecting especially young and active working age patients (1). Of all knee ligament surgeries, 80% are ACL reconstructions (ACLR) (2). The overall incidence of ACL injuries in the general population has been reported to be 69 per 100,000 people (3). Based on Swedish, Danish and Norwegian ACL registries, the annual incidence of primary ACLR is 32–38 per 100,000 inhabitants (4). In US registry analysis, the incidence of ACLR increased from 33 per 100,000 in 1994 to 44 in 2006 (5,6). That may in part reflect an increase in the overall number of ACL injuries.
The goal of the ACLR surgery is to allow patients to return to their daily activities and sports. Previous studies have mainly focused on return to sports, even in specific athletic groups (7,8). These studies provide valuable information on recovery in these certain sports groups, but do not accurately reflect the return to work in the general population. Timing of surgery after injury seems to have an association with sickness absence, as acute-phase ACLR may lead to shorter sick leave and potentially faster RTW compared with delayed ACLR (9). We are aware of only 3 previous studies analyzing factors that may contribute to the rate and timing of return to work (RTW) after ACLR. They found that heavy knee-demanding work, a prolonged period in which walking was aided by crutches, and work-related accidents were associated with slower RTW after ACLR (7,10,11). However, they were only single-center studies and limited with low numbers of patients and they evaluated only a limited number of mainly clinical factors related to RTW.
Therefore, we examined how various patient-related factors including sociodemographics (age, sex, occupational status) and various health indicators (comorbidities, anti-depressant medication, preoperative sickness absence), and surgery-related factors (concomitant procedures, subsequent knee surgery) are associated with the timing of RTW after ACLR in a large nationwide cohort of public sector employees.
Patients and methods
The study population is derived from the Finnish Public Sector (FPS) study (12-14). This register cohort comprises all employees who had worked a minimum of 6 months in the participating organizations between 1991 and 2010 (n = 151,901). It covers a wide range of occupations—from highlevel non-manual workers to low-level manual workers. Participants were linked by their unique identification number to national registries of hospital discharge information (recorded by the National Institute for Health and Welfare) and information on absence from work due to sickness (recorded by the Social Insurance Institution of Finland) until December 31, 2011.
Type of surgery and patient characteristics
Of the FPS cohort participants, 1,062 underwent an anterior cruciate ligament reconstruction between 1999 and 2011 (Figure 1). Complete data concerning surgery-related information, occupational status, and sick leaves was available for 803 patients (n = 334 male; n = 469 female; mean age 41 years, SD 8.6) (Figure 1). The type of surgery was defined as NGE35 according to the NOMESCO Classification of Surgical Procedures Version 1.14 by the Nordic Medico-Statistical Committee. Concomitant surgical procedures were defined as follows: meniscus resection, NGD05/NGD00; meniscus fixation, NGD25/NGD20; collateral ligament repair, NGE20/NGE25; and other defined procedures, NGF30, NGF35, NGF40, NGE10, NGF15, NGF20/NGF25, NFK30, NGK30, NGE60, NGL30, NGL66, NGU20. Subsequent knee surgery within 90 days from primary surgery was defined as NGW10/NGS99 and or ICD-10 code T81.4.
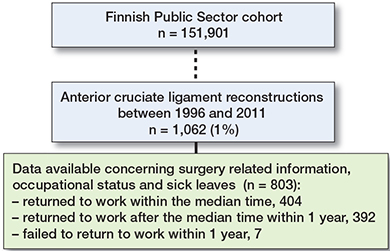
Figure 1. Flowchart of the selection of the analytical sample.
Among the FPS cohort (n = 151,901) participants, 1,062 patients underwent an anterior cruciate ligament reconstruction between 1999 and 2011 (Figure 1). Of these, 803 participants with data available concerning surgery-related information, occupational status, and sick leaves were included in the study
Return to work
Return to work (RTW) was determined as the number of days between the date of discharge and the date of the end of sick leave (Figure 1). Finnish residents aged 16 to 67 years are entitled to receive daily allowances due to medically certified sickness absence from the Social Insurance Institution of Finland. After a qualifying period of the first 10 days of illness, compensation is paid for a maximum of 1 year for medically certified periods of sickness absence, which are registered with the start and end dates. Overlapping and consecutive periods of sick leaves were merged. The linkage data was available until December 31, 2011. Based on median split, a binary variable for the length of RTW was determined as longer or shorter than median duration.
Studied factors associated with return to work
The participants’ age, sex, and occupational status at the time of the surgery were obtained from the employers’ registers. Based on the International Standard Classification of Occupations (ISCO), we grouped the occupations into higher level non-manual work (ISCO classes 1–2, including, e.g,. managers, teachers, and physicians), lower level non-manual work (ISCO classes 3–4, e.g., registered nurses, technicians), and manual work (ISCO classes 5–9, e.g., practical nurses, cleaners, maintenance workers) (15,16).
Prevalent diabetes, coronary heart disease, asthma, chronic obstructive pulmonary disease, and rheumatoid arthritis were derived from the Drug Reimbursement Register, which contains information on all persons entitled to special reimbursement for treatment of chronic health conditions from the Social Insurance Institution of Finland. Information on purchases of prescribed antidepressants (ATC code N06A; yes or no) and periods of sickness absences longer than 30 days (yes or no) within the 1-year period preceding the operation were also obtained from the registers of the Social Insurance Institution of Finland (15).
Statistics
We used logistic regression analyses to study the associations between explanatory factors and RTW (longer vs. shorter than median time). We examined the associations separately for each factor adjusted for age and sex. The results were presented as odds ratios (OR) and their 95% confidence intervals (CI). Kaplan–Meier graphs were created by Proc Lifetest to describe RTW over time for all participants (Figure 2A), and by the occurrence of preoperative sickness absence (Figure 3A), by occupational status (Figure 3B), and by age group (Figure 3C).
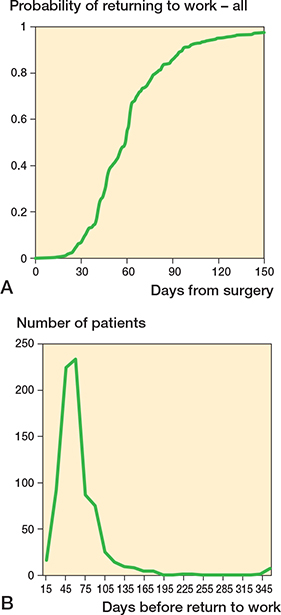
Figure 2. Kaplan-Meier survival graphs showing (A) probability of returning to work overall after ACLR and (B) RTW time (days) overall after ACLR.
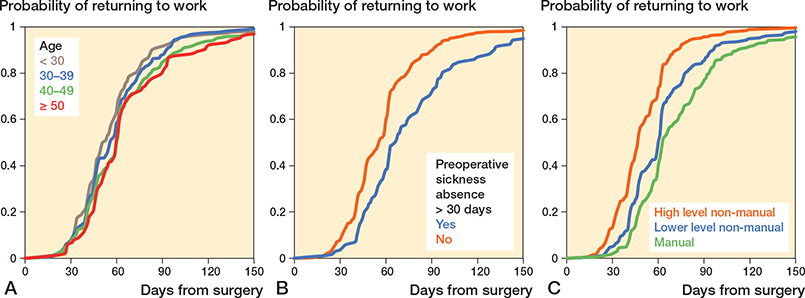
Figure 3. Kaplan-Meier survival graphs showing probability of returning to work (A) in different age groups, (B) according to preoperative sick leave absence, and (C) according to occupational status.
All analyses were performed using the SAS statistical software, version 9.4 (SAS Institute, Inc, Cary, NC, USA).
Ethics, funding, data sharing, and potential conflicts of interest
The ethics committee of the Hospital District of Helsinki and Uusimaa approved the study (ethical approval: 22.3.2011, Dnor 60/13/03/00/2011). No funding was received. This manuscript is based on third-party data. Access to dat is regulated by Finish law and Findat. Disclosure of data to third parties without explicit permission from Findata is prohibited. Access to data may be requested from www.findata.fi. No conflicts of interest were declared by the authors.
Results
The majority (58%) of patients were women and 37% worked in manual jobs. The mean age at the time of surgery was 40 years (SD 8.6). Only 7.6% of patients had a comorbid chronic medical condition (Table). The mean time to RTW was 65 days (SD 41, median 59). After the surgery, 99% (n = 796) of patients returned to work within the 1-year follow-up time.
| Factor | n (%) | RTW days (SD) | RTW > median | RTW ≤ median | Odds ratio (CI) |
| All | 803 | 65 (41) | 399 | 404 | |
| Sex | |||||
| Male | 334 (42) | 64 (43) | 163 | 171 | 1.0 (0.8–1.4) |
| Female | 469 (58) | 65 (40) | 236 | 233 | 1 |
| Age, years | |||||
| ≤ 29 | 106 (13) | 62 (47) | 41 | 65 | 1 |
| 30–39 | 295 (37) | 60 (26) | 136 | 159 | 1.4 (0.9–2.2) |
| 40–49 | 300 (37) | 67 (43) | 166 | 134 | 2.0 (1.3–3.1) |
| ≥ 50 | 102 (13) | 74 (58) | 16 | 102 | 2.0 (1.1–3.4) |
| Comorbidities | |||||
| No | 742 (92) | 65 (39) | 372 | 370 | 1 |
| Yes | 61 (7.6) | 66 (61) | 27 | 34 | 0.8 (0.4–1.3) |
| Antidepressant medication purchase within 1 year | |||||
| No | 752 (94) | 64 (39) | 367 | 385 | 1 |
| Yes | 51 (6.4) | 77 (67) | 32 | 19 | 1.7 (0.9–3.0) |
| Occupational status (missing = 2) | |||||
| High level, non-manual | 273 (34) | 50 (21) | 83 | 190 | 1 |
| Low level, non-manual | 235 (29) | 65 (35) | 127 | 108 | 3.0 (2.0–4.3) |
| Manual | 293 (37) | 78 (53) | 189 | 104 | 4.9 (3.4–7.0) |
| Preoperative sickness absence a | |||||
| No | 633 (79) | 60 (33) | 291 | 342 | 1 |
| Yes | 170 (21) | 82 (59) | 108 | 62 | 2.0 (1.4–2.9) |
| Surgery | |||||
| No concomitant procedures | 655 (82) | 64 (38) | 322 | 333 | 1 |
| Concomitant procedure | 148 (18) | 68 (51) | 77 | 71 | 1.1 (0.8–1.6) |
| Meniscus resection | 104 | 69 (50) | 59 | 45 | 1.3 (0.9–2.0) |
| Meniscus fixation | 27 | 60 (24) | 12 | 15 | 0.8 (0.4–1.8) |
| Collateral repair | 4 | 49 (20) | 1 | 3 | 0.3 (0.0–3.4) |
| Other | 22 | 82 (70) | 12 | 10 | 1.2 (0.5–2.8) |
| Subsequent knee surgery within 90 days b | |||||
| No | 789 (98) | 64 (41) | 385 | 404 | – |
| Yes | 14 (1.7) | 100 (48) | 0 | 14 | – |
| a > 30 days of sickness absence within the 1-year period preceding the operation. | |||||
| b Either knee. | |||||
Factors associated with return to work
In logistic regression analyses adjusted for age and sex, patients aged 40–49 had a 2.0 times higher odds ratio (OR) (CI 1.3–3.1) of longer RTW time (over 59 days) compared with patients aged < 30 years. For the patients aged ≥ 50 years, the corresponding OR was 2.0 (1.1–3.4). Compared with patients in manual work, those in lower-level non-manual and higher-level non-manual work had 3.0-fold OR (2.0–4.3) and 4.9-fold OR (3.4–7.0), respectively, for shorter RTW (Figure 3). Patients without preoperative sickness absence were associated with 2.0 times higher OR (1.4–2.9) to return to work before the median time as compared with those with such absence (Table).
In contrast, concomitant injuries, sex, chronic medical comorbidities (asthma, diabetes mellitus, rheumatoid arthritis, and coronary artery disease), and preceding antidepressant usage were not associated with RTW (Table).
Discussion
The most important finding in this study is that age over 40 years, manual work, and preoperative sickness absence are associated with prolonged RTW. Such association was not found with concomitant injuries, chronic medical comorbidities (asthma, diabetes mellitus, rheumatoid arthritis, and coronary artery disease), or preceding antidepressant usage. After operation, practically all (99%) of the patients returned to work within one year, in an average of 8–9 weeks (mean 65, median time 59 days).
We found only 3 previous studies analyzing factors that may contribute to the length of time before RTW after ACLR. In those studies, the number of patients was quite small compared with ours (7,10,11). In the Groot et al. (7) (n = 89) and Jenny and Clement (11) (n = 72) study population, 92–96% of the patients fully returned to work with a median time interval of 10–11 weeks (69–78 days), which is slightly longer than in our study (median 59 days; mean 65, SD 41) (Figure 3). In the study by Tiftikci et al. (10) (n = 33) the average time for RTW among miners was reported as 15 ± 4 weeks, which is longer than for manual workers in our study (mean 11 weeks). In line with these studies, we found that patients in higher-level non-manual jobs, where physically knee-demanding work is rare, returned to work earlier than those in manual jobs, where physically knee-demanding work is common. On the other hand, Jenny and Clement did not find any difference for RTW between sedentary and strenuous work. Our results were also in line with Groot regarding concomitant surgical procedures, which were not associated with the rate or timing of RTW.
Return to sports after ACLR has been studied in recent years. Return to sports is not directly proportional to the return to work in the general population, but it may reflect the time needed for recovery and rehabilitation after ACLR. Return to sports (RTS) after ACLR is reported to be associated with the patient’s age and sex, injury and surgery-related findings, physical activity level and knee function-related factors, and psychological factors such as motivation and confidence (6,7,17,18). Previous studies show that, on average, 83% of elite athletes RTS after ACLR after a mean time of 6–13 months (19,20). Athletes returning to pivoting sports within the first year after ACLR have up to 15 times higher risk of ACL re-rupture compared with non-injured athletes (21). This and times in between these may in part explain the longer rehabilitation period before RTS compared with RTW. There is a difference in RTS rate and RTS time between specific sports. Football and soccer players had the lowest RTS rate and longest RTS time whereas ice hockey players had the highest RTS rate and shortest RTS time. Basket-ball players had RTS rates and times in between these numbers (20,22). Also, performance levels after ACLR seem to vary. Only 40–65% of competitive athletes return to their previous level of performance (19,23,24). On the other hand, the performance of elite athletes who returned to sport following ACLR was comparable with the performance of matched cohorts of elite athletes who had not undergone ACLR (20). This highlights the overall need to better identify those individuals who benefit from ACLR.
Return to work after total knee arthroplasty (TKA) has been more thoroughly studied. The average time to RTW varies from 7.7 to 12 weeks after TKA. RTW after TKA has been found to be associated with general health status, age, sex, comorbidities, psychosocial and motivational factors, work-related factors such as knee demand, the possibility of making adjustments to work, and the length of sick leaves before the surgery (13,14,25-27). Despite TKA patients being typically substantially older than ACLR patients, those results are in line with our results among patients with ACLR. Younger age, higher education, working one month preoperatively, and non-manual work are associated with better work outcomes after TKA, as we found also after ACLR (27).
Strengths and weaknesses
The generalizability of these findings may reflect the differences in national welfare, pension, and workers’ compensation schemes (28). The studied cohort was limited to public sector employees in a Scandinavian welfare state. Based on the available data, we could not determine whether patients had had previous surgery to the same lower limb. Time between injury and surgery was not provided, which may be associated with the time to RTW after ACLR (9). We did not have data on the motivation to return to work, a potentially important factor. However, antidepressant treatment, a proxy of negative emotional state and indicator of poor mental health, was not associated with return to work in our study. The number of reoperations was low and did not allow statistical analysis of their impact on RTW. A further limitation is that that we were not able to assess factors associated with post-surgery activity levels, satisfaction with the outcome, or functional outcome scores. Patients’ pre-surgery expectations and the patient–healthcare provider interaction were not available (29). Further, we did not have data on workplace adjustments before or after the surgery, graft choice or surgery method, injury mechanism, time between injury and surgery, or perioperative complications. Also, RTW may also be associated with patients’ interactions with healthcare professionals as well as patients’ pre-surgery expectations (29). Moreover, we had no information on health-related behaviors potentially associated with RTW.
Finally, it is possible that some patients did not receive any sick leave. In accordance with the national regulations, self-certification for a sick leave certificate is possible only in cases of short spells (1–3 days), but for longer spells examination by a physician and a medical certificate covering the entire period of sickness absence is required from all employees working in the Finnish public sector irrespective of their job. Employees are paid a full salary during their sick leave. Employers receive compensation from the Finnish Social Insurance Institution for loss of salary due to sick leave that lasts more than 10 days. To receive the full compensation to which they are entitled, employers are obliged to keep strict records of all sick leaves. Thus, in cases where return-to-work would be possible within a few days postoperatively, it could affect the findings. As such cases are rare, a major bias is unlikely.
However, compared with previous literature, our study also had notable strengths. The large patient sample was drawn from a well-characterized occupational cohort and represented a wide range of occupations with comprehensive data on health before the surgery. All data was linked to reliable national health registers including detailed information on the operation and the start and end dates of all periods of sickness absence, enabling accurate estimation of the length of time before return to work. All factors associated with RTW, such as occupational status, sickness absences before the operation, and comorbid medical conditions, were measured objectively from the registers. Although we had no information on knee-demanding duties, the three different occupational status groups provided us with a proxy for the overall physical demands of the occupations. Further population-based research is needed to confirm these findings in other national and occupational settings. Further research may reveal whether the associations found in this study are robust for various subgroups of patients with ACL injuries and different types of ACL graft choices.
In conclusion, length of sick leave after ACLR varies individually. In this nationwide occupational cohort of 803 patients who underwent ACLR, return to work occurred after a mean time of 65 days after surgery. In general, non-manual workers returned to work with a mean 65 days of sickness absence and manual workers at a mean 78 days and patients over 50 years old at a mean 74 days after ACLR. This study provides evidence on factors that are associated with RTW and helps occupational healthcare services to estimate the length of sick leave after ACLR. Patients in manual labor, older than 40 years, and patients on sick leave over 30 days prior to surgery had higher odds of a slower RTW time after ACLR compared with other groups.
- Musahl V, Karlsson J. Anterior cruciate ligament tear. N Engl J Med 2019; 380(24): 2341-2348. doi: 10.1056/NEJMcp1805931.
- Gianotti S M, Marshall S W, Hume P A, Bunt L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: a national population-based study. J Sci Med Sport 2009; 12(6): 622-7. doi: 10.1016/j.jsams.2008.07.005.
- Sanders T L, Maradit Kremers H, Bryan A J, Larson D R, Dahm D L, Levy B A, et al. Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med 2016; 44(6): 1502-7. doi: 10.1177/0363546516629944
- Granan L P, Forssblad M, Lind M, Engebretsen L. The Scandinavian ACL registries 2004–2007: baseline epidemiology. Acta Orthop 2009; 80(5): 563-7. doi: 10.3109/17453670903350107.
- Mall N A, Chalmers P N, Moric M, Tanaka M J, Cole B J, Bach B R Jr, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med 2014; 42(10): 2363-70. doi: 10.1177/0363546514542796.
- Lyman S, Koulouvaris P, Sherman S, Do H, Mandl L A, Marx R G. Epidemiology of anterior cruciate ligament reconstruction: trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am 2009; 91(10): 2321-8. doi: 10.2106/JBJS.H.00539.
- Groot J A, Jonkers F J, Kievit A J, Kuijer P P, Hoozemans M J. Beneficial and limiting factors for return to work following anterior cruciate ligament reconstruction: a retrospective cohort study. Arch Orthop Trauma Surg 2017; 137(2): 155-66. doi: 10.1007/s00402-016-2594-6
- Webster K E, Hewett T E. What is the evidence for and validity of return-to-sport testing after anterior cruciate ligament reconstruction surgery? A systematic review and meta-analysis. Sports Med 2019; 49(6): 917-29. doi: 10.1007/s40279-019-01093-x
- von Essen C, McCallum S, Barenius B, Eriksson K. Acute reconstruction results in less sick-leave days and as such fewer indirect costs to the individual and society compared to delayed reconstruction for ACL injuries. Knee Surg Sports Traumatol Arthrosc 2020; 28(7): 2044-2052. doi: 10.1007/s00167-019-05397-3.
- Tiftikci U, Serbest S, Kilinc C Y, Karabicak G Ö, Vergili Ö. Return to work in miners following anterior cruciate ligament reconstruction. Pan Afr Med J 2015; 22:173. doi: 10.11604/pamj.2015.22.173.7979
- Jenny J Y, Clement X. Patient-based decision for resuming activity after ACL reconstruction: a single-centre experience. Eur J Orthop Surg Traumatol 2016; 26(8): 929-935. doi: 10.1007/s00590-016-1861-0.
- Airaksinen J, Jokela M, Virtanen M, Oksanen T, Pentti J, Vahtera J, et al. Development and validation of a risk prediction model for work disability: multicohort study. Sci Rep 2017; 7(1): 13578. doi: 10.1038/s41598-017-13892-1.
- Lankinen P, Laasik R, Kivimäki M, Aalto V, Saltychev M, Vahtera J, et al. Are patient-related pre-operative factors influencing return to work after total knee arthroplasty. Knee 2019; 26(4): 853-60. doi: 10.1016/j.knee.2019.04.015
- Laasik R, Lankinen P, Kivimäki M, Aalto V, Saltychev M, Mäkelä K, et al. Return to work after primary total hip arthroplasty: a nationwide cohort study. Acta Orthop 2019; 90(3): 209-13. doi: 10.1080/17453674.2019.1591081
- Kivimäki M, Batty G D, Pentti J, Shipley M J, Sipilä P N, Nyberg S T, et al. Association between socioeconomic status and the development of mental and physical health conditions in adulthood: a multi-cohort study. Lancet Public Health 2020; 5(3): e140-e149. doi: 10.1016/S24682667(19)30248-8.
- Statistics Finland. The standard classification of occupations 2001. https://www2.stat.fi/en/luokitukset/ammatti/ammatti_1_20100101/ (last accessed March 2, 2022).
- Zätterström R, Fridén T, Lindstrand A, Moritz U. Rehabilitation following acute anterior cruciate ligament injuries: a 12-month follow-up of a randomized clinical trial. Scand J Med Sci Sports 2000; 10(3): 156-63. doi: 10.1034/j.1600-0838.2000.010003156.x.
- Everhart J S, Best T M, Flanigan D C. Psychological predictors of anterior cruciate ligament reconstruction outcomes: a systematic review. Knee Surg Sports Traumatol Arthrosc 2015; 23(3): 752-62. doi: 10.1007/s00167-013-2699-1.
- Waldén M, Hägglund M, Magnusson H, Ekstrand J. ACL injuries in men’s professional football: a 15-year prospective study on time trends and return-to-play rates reveals only 65% of players still play at the top level 3 years after ACL rupture. Br J Sports Med 2016; 50(12): 744-50. doi: 10.1136/bjsports-2015-095952.
- Lai C C H, Ardern C L, Feller J A, Webster K E. Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: a systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. Br J Sports Med 2018; 52(2): 128-38. doi: 10.1136/bjsports-2016-096836.
- Paterno M V. Incidence and predictors of second anterior cruciate ligament injury after primary reconstruction and return to sport. J Athl Train 2015; 50(10): 1097-9. doi: 10.4085/1062-6050-50.10.07.
- Mohtadi N G, Chan D S. Return to sport-specific performance after primary anterior cruciate ligament reconstruction: a systematic review. Am J Sports Med 2018; 46(13): 3307-16. doi: 10.1177/0363546517732541.
- Frobell R B, Roos E M, Roos H P, Ranstam J, Lohmander L S. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med 2010; 363(4): 331-42. doi: 10.1056/NEJMoa0907797.
- Ardern C L, Taylor N F, Feller J A, Webster K E. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med 2014; 48(21): 1543-52. doi: 10.1136/bjsports-2013-093398.
- Jorn L P, Johnsson R, Toksvig-Larsen S. Patient satisfaction, function and return to work after knee arthroplasty. Acta Orthop Scand 1999; 70(4): 343-7. doi: 10.3109/17453679908997822.
- Kuijer P P, de Beer M J, Houdijk J H, Frings-Dresen M H. Beneficial and limiting factors affecting return to work after total knee and hip arthroplasty: a systematic review. J Occup Rehabil 2009; 19(4): 375-81. doi: 10.1007/s10926-009-9192-1.
- Tilbury C, Schaasberg W, Plevier J W, Fiocco M, Nelissen R G, Vliet Vlieland T P. Return to work after total hip and knee arthroplasty: a systematic review. Rheumatology (Oxford) 2014; 53(3): 512-25. doi: 10.1093/rheumatology/ket389.
- Scott C E H, Turnbull G S, MacDonald D, Breusch S J. Activity levels and return to work following total knee arthroplasty in patients under 65 years of age. Bone Joint J 2017; 99-B(8): 1037-46. doi: 10.1302/0301620X.99B8.BJJ-2016-1364.R1.
- Bardgett M, Lally J, Malviya A, Deehan D. Return to work after knee replacement: a qualitative study of patient experiences. BMJ Open 2016; 6(2): e007912. doi: 10.1136/bmjopen-2015-007912.