Rate of conversion to secondary arthroplasty after femoral neck fractures in 796 younger patients treated with internal fixation: a Swedish national register-based study
Sebastian STRØM RÖNNQUIST 1,2, Johan LAGERGREN 3,4, Bjarke VIBERG 2,5, Michael MÖLLER 6–8, and Cecilia ROGMARK 1,8,9
1 Department of Orthopaedics, Lund University, Skåne University Hospital, Malmö, Sweden; 2 Department of Orthopaedic Surgery and Traumatology, Odense University Hospital, Odense, Denmark; 3 Department of Clinical Sciences, Faculty of Medicine, Lund University, Malmö, Sweden; 4 Western Hospital Group, Alingsås, Sweden; 5 Department of Orthopaedic Surgery and Traumatology, Lillebaelt Hospital, University Hospital of Southern Denmark, Denmark; 6 Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; 7 Department of Orthopaedics, Sahlgrenska University Hospital Gothenburg/Mölndal, Sweden; 8 Swedish Fracture Register, Gothenburg, Sweden; 9 Swedish Arthroplasty Register, Gothenburg, Sweden
Background and purpose — In younger patients with a femoral neck fracture (FNF), internal fixation is the recommended treatment regardless of displacement. Healing complications are often treated with arthroplasty. We determined the rate of conversion to arthroplasty up to 5 years after fixation of either undisplaced FNFs (uFNFs) or displaced FNFs (dFNFs).
Patients and methods — The study was based on prospectively collected data from the Swedish Fracture Register (SFR) and the Swedish Arthroplasty Register (SAR). FNFs in patients aged < 60 treated with parallel pins/screws or sliding hip screws (SHS) registered in SFR 2012–2018 were cross-referenced with conversions to arthroplasty registered in SAR until 2019. The cumulative conversion and mortality rates were determined by Kaplan–Meier analyses and patient- and surgery-dependent risk factors for conversion by Cox regression analyses.
Results — We included 407 uFNFs and 389 dFNFs (median age 52, 59% men). The 1-year conversion rate was 3% (95% CI 1–5) for uFNFs and 9% (CI 6–12) for dFNFs. Corresponding results at 5 years were 8% (CI 5–11) and 25% (CI 20–30). Besides a displaced fracture, age 50–59 was associated with an increased rate of conversion in uFNFs. This older group also had a higher mortality rate, compared with patients aged < 50. There was no sex difference for mortality.
Interpretation — Adults aged under 60 with uFNFs and dFNFs face an 8–25% risk, respectively, of conversion to arthroplasty within 5 years after internal fixation. This is new and pertinent information for surgeons as well as patients.
Citation: Acta Orthopaedica 2022; 93: 547–553. DOI http://dx.doi.org/10.2340/17453674.2022.3038.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-02-07. Accepted: 2022-05-16. Published: 2022-06-14.
Correspondence: sebastian.strom_ronnquist@med.lu.se
All authors were involved in the study design and approved the final manuscript. SSR initiated the study, curated data, performed statistical analysis, wrote, and reviewed the manuscript. JL critically reviewed the manuscript. BV contributed expert knowledge, wrote, and reviewed the manuscript. MM contributed expert knowledge and critically reviewed the manuscript. CR initiated the study, supervised SSR, wrote, and reviewed the manuscript.
The authors wish to thank Emma Nauclér at Registercentrum for help with statistical visualization. They also thank all who contribute to the SFR and SAR by registration of fractures and treatments.
Acta thanks Wierd P Zijlstra and an anonymous reviewer for help with peer review of this study.
In younger individuals with femoral neck fractures (FNF), internal fixation (IF) is the recommended treatment alternative (1). Nevertheless, the risk of healing complications has to be acknowledged; osteonecrosis of the femoral head and non-union are the most common but the actual rate of conversion to arthroplasty is insufficiently described in younger patients. A population-based study on 796 individuals aged under 50 years found a conversion rate of 14%, but did not distinguish fracture displacement (2). A smaller case series (n = 122) presented a conversion rate of 22% for displaced FNFs (dFNF) (3). Besides the obvious need to give correct information on prognosis to younger patients, detailed knowledge on conversion rate is mandatory to underpin a sound treatment strategy. The debate focuses on where to draw the line between internal fixation and hip replacement as primary treatment of a dFNF. Different age limits are proposed, even as low as 45 years has been suggested (4). Traditions and surgical preferences vary internationally; the Scandinavian countries have had a higher age limit for primary arthroplasty as treatment for FNFs but have gradually shifted from 70 to approximately 60 years (5,6). Also, for undisplaced FNFs (uFNF), primary arthroplasty has recently been put forward as an alternative, at least in elderly patients (7,8). We designed a national register-based study to determine the rate of conversion to arthroplasty from IF due to uFNFs and dFNFs in patients under the age of 60. Furthermore, we descriptively analyzed mortality and the relationship between conversion rate and sex, age, trauma mechanism, and surgeon’s experience.
Patients and methods
Study design
This longitudinal cohort study is based on 2 Swedish national registries with prospectively collected data: the Swedish Fracture Register (SFR) and the Swedish Arthroplasty Register (SAR). We followed the STROBE guidelines for reporting the study.
Setting
The SFR started in 2011 and during the study period (2012–2018) the coverage for hip fractures increased from 18% to 86% due to an increased number of hospitals reporting to the register (9,10). By 2021 all orthopedic departments in Sweden participated, i.e., coverage of 100%, in the register, which comprised 645,000 fractures at the end of 2021. The completeness of the register has been validated and in 2018 the completeness for femoral fractures was 55% (11,12). FNFs are classified in the SFR according to the 2007 AO/OTA classification as undisplaced subcapital (31-B1), transcervical/basicervical (31-B2), and displaced subcapital (31-B3) (13). The accuracy of the fracture classification in the SFR has been validated, and was found to be substantial (14). The injury, fracture classification, and treatment are registered by a physician through individual log-in on the SFR webpage.
SAR is the national quality register for hip and knee replacement surgery in Sweden. SAR has a coverage of 100% for all departments performing hip replacement surgery, both public and private. For the years of the current study, the completeness was approximately 98% for total hip arthroplasty (THA), 96% for hemiarthroplasties (HA), and 92% regarding revisions of both THA and HA (15). By regular co-processing with the population register (the Swedish Tax Agency) any date of death is noted in both register databases.
Participants
Data for all patients aged 18 to 59 years registered with a hip fracture (defined by the ICD codes S72.00, S72.10 and S72.20) in SFR from 2012 to 2018 was extracted and cross-referenced with available data from SAR for each individual from the date of the index fracture until December 31, 2019. The unique individual personal number of each Swedish citizen ensures a reliable match between registers and subsequent surgeries and/or death. Only the 1st registered hip fracture was included in the study; contralateral and subsequent ipsilateral fractures and duplicate registrations were excluded. The uFNFs (AO/OTA 31-B1, Garden 1–2) and dFNFs (AO/OTA 31-B3, Garden 3–4) were further examined for eligibility; other fracture types were excluded (13). We identified all available FNFs in the SFR, but the data search did not include any concurrent fractures. As they are specified in the reporting procedure, and identified by their ICD-10 diagnose codes (M84.4, M84.8, M84.3), pathological, spontaneous, and stress fractures were excluded from the analysis together with peri-implant fractures. Based on the primary treatment, fractures treated with IF (parallel pins/screws or sliding hip screw devices [SHS]) were identified, and we excluded patients treated with primary arthroplasty, intramedullary nail, other types of plate fixation, or non-surgically from further analysis on conversion rate (Figure 1).
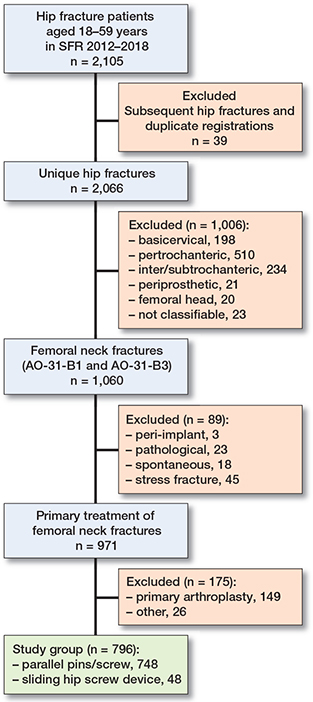
Figure 1. Flowchart of inclusion.
Study variables
We analyzed basic demographic and epidemiological variables (i.e., sex, age, and trauma mechanism) and data on the primary fracture treatment from SFR (i.e., type of IF used and surgeon’s experience defined as performed by either a resident or a specialist), together with the rate of conversion to hip arthroplasty registered in SAR and mortality. Trauma mechanism was defined according to the definition used in SFR: low-energy trauma is same-level falls and high-energy trauma is caused by truly high level of energy, such as traffic accidents or falls from a height. Length of follow-up was defined as time from injury date to date of death or end of study period on December 31, 2019.
Study outcomes
The main aim was to determine rates of conversion to arthroplasty after IF of uFNFs and dFNFs at 1, 2, and 5 years. Furthermore, analyses were performed on mortality and associations between conversion to arthroplasty and sex, age, trauma mechanism, and surgeon’s experience in the study group.
Statistics
Observations were grouped according to fracture classification (i.e., uFNF or dFNF), sex, and age < 50 or 50–59. Data on continuous variables were assessed for normality and presented as mean or median, depending on normal distribution. We analyzed associations between categorical variables using a chi-square test. Kaplan–Meier analysis was used to determine the rate of conversion to secondary arthroplasty as cumulative reoperation rate (CRR) with 95% confidence interval (CI) at 1, 2, and 5 years after the injury and to estimate mortality rates. We used a Cox proportional hazards regression model to determine hazard ratios (HR) between risk factors for secondary arthroplasty, where female sex, age 50–59, high-energy trauma mechanism, and resident surgeon previously have been described to have increased risk of reoperation and were assumed to be associated with a higher HR (4,16-18). Participants with missing data for a variable were excluded from analysis of that specific variable. Analysis of data was performed in IBM SPSS version 26 (IBM Corp, Armonk, NY, USA) and R version 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria).
Ethics, data sharing, funding, and potential conflicts of interests
The study was conducted in accordance with the Helsinki Declaration and was approved by the Swedish national ethical review board (Etikprövningsnämnden: Dnr 2019-05024). Data was pseudonymized before extraction from the registries and subsequent analysis. The data supporting the findings of this study is available upon reasonable request to the corresponding author. The study was supported by grants from the Research and Development Council of Region Skåne and a grant from the Swedish Research Council funding for clinical research in medicine. The authors declare no conflicts of interest related to the study.
Results
2105 hip fractures were identified in the SFR. After exclusion, 407 uFNFs and 389 dFNFs treated with internal fixation with parallel pins/screws or SHS were analyzed (Figure 1).
Patients were aged 20 to 59 years at the time of the fracture, 59% of the fractures occurred in men, and 77% were due to low-energy trauma. Fractures due to high-energy trauma were more prevalent in dFNFs compared with uFNFs. The distribution of parallel pins/screws and SHS was similar in uFNFs and dFNFs. Specialists performed 2/3 of all operations due to FNFs (Table 1).
108 of the 796 participants underwent a conversion to arthroplasty, 28 after IF of uFNFs, and 80 after dFNFs. There were 2 conversions to HA, all others to THA. In an implant survival analysis, the conversion rates after 1, 2, and 5 years for dFNFs were 9% (95% CI 6–12), 17% (CI 13–21), and 25% (CI 20–30), which were higher than for uFNFs, which demonstrated 3% (CI 1–5), 5% (CI 3–8), and 8% (CI 5–11) (Table 2, see Supplementary data).
Age 50–59 was associated with an increased rate of conversion to arthroplasty for uFNFs but not for dFNFs (Figure 2). When analyzing risk factors for conversion, age 50–59 had an HR of 5.2 (CI 1.4–20) compared with age < 50 years in the uFNF groups. No other risk factors could be identified (Table 3).
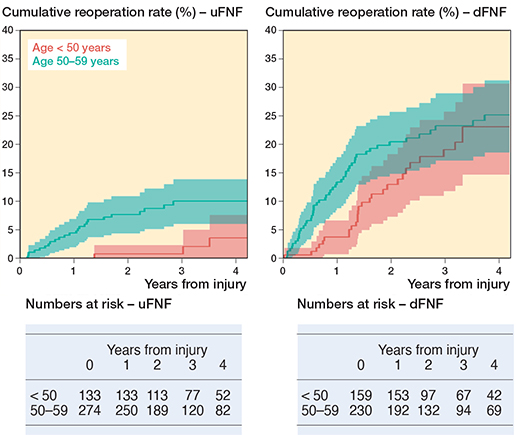
Figure 2. Cumulative reoperation rate with 95% confidence intervals presented by age classification and fracture type. uFNF: undisplaced femoral neck fracture. dFNF: displaced femoral neck fracture.
The exclusion of 149 patients treated with primary arthroplasty theoretically reduced the number of FNFs at risk of conversion to arthroplasty (Figure 1). Median age (IQR) for patients treated with primary arthroplasty was 56 (54–58). 9% were aged < 50, 56% were women, and 89% low-energy trauma (n = 14, 84 and 133 respectively).
The mortality rates were similar between uFNFs and dFNFs and between men and women (Figures 3 and 4). At 1 year, 20 individuals had died and at 5 years, 62. The 1- and 5-year cumulative mortality rate of individuals aged 50–59 at the time of the fracture was 4% (CI 2–6) and 16% (CI 11–20) compared with 0% and 5% (CI 2–7) for those aged < 50 (Table 4, see Supplementary data).
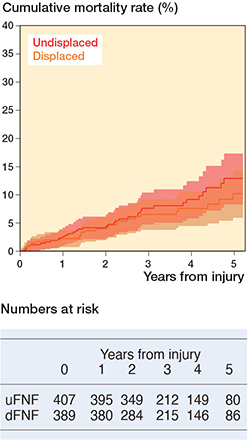
Figure 3. Cumulative mortality rate with 95% confidence intervals presented by fracture type.
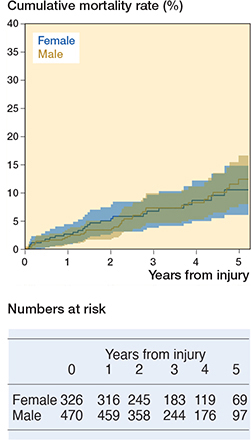
Figure 4. Cumulative mortality rate with 95% confidence intervals presented by sex.
Discussion
A considerable proportion of young and middle-aged individuals with an FNF can expect a conversion to hip arthroplasty within 5 years post-fracture, 1 in 4 for displaced fractures and 1 in 12 for undisplaced fractures.
Our rates of conversion to arthroplasty were comparable to previous reports on younger patients (2,3). Stockton et al. (2) considered their conversion rate to be high and called for improvement in the treatment of FNFs in younger patients. Our results for uFNFs are in close proximity, but we regard the conversion rate to be acceptable and believe it confirms IF as the gold standard for uFNFs in this age group. For patients with dFNFs on the other hand, outcome after IF is poorer. In our 50–59-year group, there is an immediate and steady increase in the rate of conversion during the entire follow-up, showing a readiness of the surgeons to perform secondary surgery. Surgeons may feel at ease, as other patients in the same age span with symptomatic osteoarthritis are routinely given a hip replacement nowadays, as we know better the good long-term prognosis for the arthroplasty. Remarkably, the youngest group with dFNF also ended up with a 23% conversion rate at 5 years, albeit their rate was modest during the earliest years, maybe reflecting a more guarded attitude towards arthroplasty in this age group. On the other hand, when 3 of 4 with dFNFs still had their native hip at 5 years, the result in terms of conversion to arthroplasty can be said to be acceptable or even good. Future endeavors should focus on improving the clinical pathway for this group of young patients, for whom this fracture is still unsolved (19).
In elderly patients, the degree of displacement of the FNF, including both posterior and anterior tilt, and fracture comminution, have been found to predict failure of IF (20-22). Our results confirm that displacement according to Garden is a risk factor for failure leading to conversion arthroplasty in younger patients also. Nevertheless, our conversion rate is much lower than in geriatric patients treated with internal fixation of their dFNFs, where major secondary surgery can be expected in approximately 40% (23,24).
Should we lower the age limit for primary arthroplasty? The rationale for treating younger patients with internal fixation, even if their fracture is displaced, is the theoretical benefits of preserving the femoral head and a fear of multiple revisions of an arthroplasty during a long remaining life span. But if we consider long-term results from RCTs on patients aged over 60, those initially treated with IF never reached superior functional results compared with those treated with arthroplasty (22,25). When considering risk of revision of the primary arthroplasty, one should bear in mind that conversion arthroplasties are associated with inferior outcome compared with primary arthroplasties for FNFs (26,27). Ideally, those with an inherently higher risk of fixation failure should be identified preoperatively and selected for primary arthroplasty. Otherwise, a focus on realistic expectations and readiness for swift conversion arthroplasty when needed would also be acceptable in the future, given that most young patients’ fractures actually do heal.
Notably, there was no difference between men and women regarding mortality, although elderly males with hip fractures have a higher risk of dying (28), and younger women have been reported to have more comorbidities (29). The 5-year mortality of 16% for those 50–59 years old is noteworthy, and the 1-year mortality of 4% was 10-fold higher compared with the mean mortality rate for the same ages in the general Swedish population during the years of the study (30,31). They may in this aspect resemble the elderly, which could speak in favor of a primary arthroplasty rather than internal fixation in those of advanced biological age and an expected shorter survival. This is supported by an analysis of cost-effectiveness where the lowest age proposed for THA as primary treatment of FNFs was 45 years in patients with multiple comorbidities whereas it was 54 for healthy patients (4).
Limitations
That some individuals in the older age span with dFNF were initially selected for primary arthroplasty may affect the conversion rates reported in our study. Assuming that these patients were identified as at particularly high risk of fixation failure, our estimates of the conversion rates are potentially underestimated by this selection bias.
The number of parallel implants varies internationally. In line with Scandinavian tradition, 2 pins or screws are used almost exclusively in this cohort. There is little support in the literature that adding extra screws will reduce the risk of redislocation or non-union (16). That only 6% received an SHS hindered us from testing the suggestion made by the FAITH study (32), i.e., that SHS could have some benefits in those with displaced fractures.
We lack data on whether an open reduction has been performed, but the Swedish tradition is to rely on closed reduction only. Also, the literature has so far not been able to show any clear benefits of open reduction (33,34).
Indices depicting comorbidities and biological age/frailty would have been desirable variables to analyze, but unfortunately the registers do not include these potentially important risk factors for conversion to arthroplasty. Those selected for primary arthroplasty in our material may represent such a subgroup of frailer individuals.
Strengths
Our study is the largest to date analyzing conversion rate after IF due to uFNFs and dFNFs. We believe our result to have good external validity as it reflects everyday practice in non-selected patients and surgeons. We consider conversion to arthroplasty as a marker of a major hip complication. Naturally, other outcomes are valuable and patient-reported outcome is always preferrable. Any kind of reoperation could be relevant to report, but in Sweden valgus osteotomy, core decompression, or vascular grafts are very seldom utilized. Implant removal is a common reoperation, but the severity of the underlying situation is difficult to grade. It can span from routine procedures with no or little discomfort experienced by the patients to major complications such as deep infection or fracture collapse. We also chose our outcome due to the SAR’s high completeness and national coverage, leading to a reliable result.
Conclusion
After IF in patients aged < 60, the rate of conversion to arthroplasty for dFNFs was significantly higher than for uFNFs during the entire follow-up. At 5 years, 25% and 8%, respectively, had undergone a conversion to hip arthroplasty.
In dFNFs, the conversion rates were similar in all ages. For uFNFs the conversion rates in patients aged 50–59 were significantly higher than for younger patients. No other risk factors for conversion to arthroplasty could be identified in our material. Mortality rates were markedly higher for patients aged 50–59 but did not differ between men and women or between uFNFs and dFNFs.
In perspective, both surgeons and patients should be aware of the risk of conversion to arthroplasty at the time of initial treatment. A clinical implication would be a long-term follow-up scheme and readiness for swift conversion when needed.
- Bhandari M, Swiontkowski M. Management of acute hip fracture. N Engl J Med 2017; 377(21): 2053-62.
- Stockton D J, O’Hara L M, O’Hara N N, Lefaivre K A, O’Brien P J, Slobogean G P. High rate of reoperation and conversion to total hip arthroplasty after internal fixation of young femoral neck fractures: a population-based study of 796 patients. Acta Orthop 2019; 90(1): 21-5.
- Duckworth A D, Bennet S J, Aderinto J, Keating J F. Fixation of intracapsular fractures of the femoral neck in young patients: risk factors for failure. J Bone Jt Surg Br 2011 Jun; 93:811-6.
- Swart E, Roulette P, Leas D, Bozic K J, Karunakar M. ORIF or arthroplasty for displaced femoral neck fractures in patients younger than 65 years old: an economic decision analysis. J Bone Joint Surg Am 2017; 99(1): 65-75.
- Al-Ani A N, Neander G, Samuelsson B, Blomfeldt R, Ekstrom W, Hedstrom M. Risk factors for osteoporosis are common in young and middle-aged patients with femoral neck fractures regardless of trauma mechanism. Acta Orthop 2013; 84: 54-9.
- Bartels S, Gjertsen J E, Frihagen F, Rogmark C, Utvåg S E. High failure rate after internal fixation and beneficial outcome after arthroplasty in treatment of displaced femoral neck fractures in patients between 55 and 70 years. Acta Orthop 2018; 89(1): 53-8.
- Wolf O, Sjöholm P, Hailer N P, Möller M, Mukka S. Study protocol: HipSTHeR—a register-based randomised controlled trial—hip screws or (total) hip replacement for undisplaced femoral neck fractures in older patients. BMC Geriatr 2020; 20(1): 19.
- Viberg B, Kold S, Brink O, Larsen M S, Hare K B, Palm H. Is arthroplaSty bEtter than interNal fixation for undiSplaced femoral nEck fracture? A national pragmatic RCT: the SENSE trial. BMJ Open 2020; 10(10): e038442.
- Lagergren J, Möller M, Rogmark C. Displaced femoral neck fractures in patients 60–69 years old: treatment and patient reported outcomes in a register cohort. Injury 2020; 51(11): 2652-7.
- SFR Årsrapport 2018 [Internet]. [cited 2022 Mar 22]. Available from: https://registercentrum.blob.core.windows.net/sfr/r/sfr_2018_web-SJxx-Qsru4H.pdf
- Bergdahl C, Nilsson F, Wennergren D, Ekholm C, Möller M. Completeness in the Swedish Fracture Register and the Swedish National Patient Register: an assessment of humeral fracture registrations. Clin Epidemiol 2021; 13: 325-33.
- Täckningsgradsanalys · Svenska Frakturregistret [Internet]. [cited 2022 Jan 28]. Available from: https://sfr.registercentrum.se/om-registret/taeckningsgradsanalys/p/HJedFyVyE
- Marsh J L, Slongo T F, Agel J, Broderick J S, Creevey W, DeCoster T A, et al. Fracture and Dislocation Classification Compendium—2007: Orthopaedic Trauma Association Classification, Database and Outcomes Committee. J Orthop Trauma 2007; 21(10): S1.
- Knutsson S B, Wennergren D, Bojan A, Ekelund J, Möller M. Femoral fracture classification in the Swedish Fracture Register: a validity study. BMC Musculoskelet Disord 2019; 20(1): 197.
- W-Dahl A, Kärrholm J, Rogmark C, Nauclér E, Nåtman J, Bülow E, et al. Årsrapport 2021 Svenska Ledprotesregistret [Internet]. Svenska Ledprotesregistret; 2021 [cited 2022 Jan 28] p 25475202 byte. Available from: http://refdocs.registercentrum.se/10.18158/SyZ333H5F
- Nyholm A M, Palm H, Sandholdt H, Troelsen A, Gromov K, Danish Fracture Database Collaborators. Osteosynthesis with parallel implants in the treatment of femoral neck fractures: minimal effect of implant position on risk of reoperation. J Bone Joint Surg Am 2018; 100(19): 1682-90.
- Kanthasamy S, To K, Webb J I, Elbashir M, Parker M J. Timing of surgery for internal fixation of intracapsular hip fractures and complications at 1 year: a 32 year clinical study of 2,366 patients at a single center. Injury 2022; 53(2): 584-9.
- Authen A L, Dybvik E, Furnes O, Gjertsen J E. Surgeon’s experience level and risk of reoperation after hip fracture surgery: an observational study on 30,945 patients in the Norwegian Hip Fracture Register 2011–2015. Acta Orthop 2018; 89(5): 496.
- Speed K. The unsolved fracture. Surg Gynecol Obst 1935; 60: 341-52.
- Palm H, Gosvig K, Krasheninnikoff M, Jacobsen S, Gebuhr P. A new measurement for posterior tilt predicts reoperation in undisplaced femoral neck fractures: 113 consecutive patients treated by internal fixation and followed for 1 year. Acta Orthop 2009; 80(3): 303-7.
- Sjöholm P, Otten V, Wolf O, Gordon M, Karsten G, Sköldenberg O, et al. Posterior and anterior tilt increases the risk of failure after internal fixation of Garden I and II femoral neck fracture. Acta Orthop 2019; 90(6): 537-41.
- Alho A, Benterud J G, Rønningen H, Høiseth A. Prediction of disturbed healing in femoral neck fracture: radiographic analysis of 149 cases. Acta Orthop Scand 1992; 63(6): 639-44.
- Chammout G K, Mukka S S, Carlsson T, Neander G F, Helge Stark A W, Skoldenberg O G. Total hip replacement versus open reduction and internal fixation of displaced femoral neck fractures: a randomized long-term follow-up study. J Bone Joint Surg Am 2012; 94(21): 1921-8.
- Leonardsson O, Sernbo I, Carlsson Å, Åkesson K, Rogmark C. Long-term follow-up of replacement compared with internal fixation for displaced femoral neck fractures. J Bone Joint Surg Br 2010; 92-B(3): 406-12.
- Støen R Ø, Lofthus C M, Nordsletten L, Madsen J E, Frihagen F. Randomized trial of hemiarthroplasty versus internal fixation for femoral neck fractures: no differences at 6 years. Clin Orthop 2014; 472(1): 360-7.
- Blomfeldt R, Törnkvist H, Ponzer S, Söderqvist A, Tidermark J. Displaced femoral neck fracture: comparison of primary total hip replacement with secondary replacement after failed internal fixation: a 2-year follow-up of 84 patients. Acta Orthop 2006; 77(4): 638-43.
- Frihagen F, Madsen J E, Aksnes E, Bakken H N, Maehlum T, Walløe A, et al. Comparison of re-operation rates following primary and secondary hemiarthroplasty of the hip. Injury 2007; 38(7): 815-9.
- Meyer A C, Ek S, Drefahl S, Ahlbom A, Hedström M, Modig K. Trends in hip fracture incidence, recurrence, and survival by education and comorbidity: A Swedish register-based study. Epidemiol Camb Mass 2021; 32(3): 425-33.
- Strøm Rönnquist S, Viberg B, Kristensen M T, Palm H, Jensen J E B, Madsen C F, et al. Frailty and osteoporosis in patients with hip fractures under the age of 60: a prospective cohort of 218 individuals. Osteoporos Int 2022; 33(5): 1037-55.
- Statistiska centralbyrån. Ettårig livslängdstabell för hela riket efter kön och ålder. År 1960 - 2020 [Internet]. Statistikdatabasen [cited 2022 Feb 3]. Available from: http://www.statistikdatabasen.scb.se/pxweb/sv/ssd/START__BE__BE0101__BE0101I/LivslangdEttariga/
- Bergh C, Möller M, Ekelund J, Brisby H. 30-day and 1-year mortality after skeletal fractures: a register study of 295,713 fractures at different locations. Acta Orthop 2021; 92(6): 739-45.
- Nauth A, Creek A T, Zellar A, Lawendy A R, Dowrick A, Gupta A, et al. Fracture fixation in the operative management of hip fractures (FAITH): an international, multicentre, randomised controlled trial. Lancet 2017; 389(10078): 1519-27.
- Rogmark C, Kristensen M T, Viberg B, Rönnquist S S, Overgaard S, Palm H. Hip fractures in the non-elderly: who, why and whither? Injury 2018; 49(8): 1445-50.
- Patterson J T, Ishii K, Tornetta P I, Leighton R K, Friess D M, Jones C B, et al. Open reduction is associated with greater hazard of early reoperation after internal fixation of displaced femoral neck fractures in adults 18–65 years. J Orthop Trauma 2020; 34(6): 294-301.
Supplementary data