Progressive proximal loosening of initially well-fixed bilateral Corail stems: a case report and review of the literature
Michael G JOHNSTON 1, Kade E EPPICH 1, Celeste GRAY 2, Matthew A PORTER 1, and David F SCOTT 1,2
1 Washington State University, Elson S. Floyd College of Medicine, Spokane, WA; 2 Spokane Joint Replacement Center/Orthopaedic Specialty Clinic of Spokane, Spokane, WA, USA
Citation: Acta Orthopaedica 2022; 93: 542–546. DOI http://dx.doi.org/10.2340/17453674.2022.3037.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-02-14. Accepted: 2022-05-17. Published: 2022-06-14.
Correspondence: Michael.g.johnston@wsu.edu
MJ undertook chart review, data collection, patient interview, literature review, and manuscript writing. KE assisted with chart review, data collection, patient interview and manuscript writing. DS was the surgeon managing the case and performing surgical interventions, and had a supervisory role in manuscript writing. CG undertook administration of the data and chart review, manuscript editing, and literature review. MP undertook manuscript editing and literature review.
Acta thanks Ove Nord Furnes and Keijo T Mäkelä for help with peer review of this study.
The Corail hip stem (Depuy Synthes, Raynham, MA, USA), is a tapered Ti-6AI-4V, ASTM Grade 5, alpha-beta titanium alloy femoral stem that was introduced in 1986 (1). It is straight with a quadrangular proximal cross-section, which is flared in the coronal and sagittal planes to promote proximal fixation. The distal stem is tapered, and the entirety of the stem is fully hydroxyapatite (HA) coated with a thickness of 150 μm, with a macrotexture of horizontal and vertical grooves (1). Since its inception, no changes have been made to the stem’s macrotexture or HA thickness due to its relative success. This device has received widespread worldwide use and has shown high long-term survival in primary total hip arthroplasty (THA) (1-3).
Case presentation
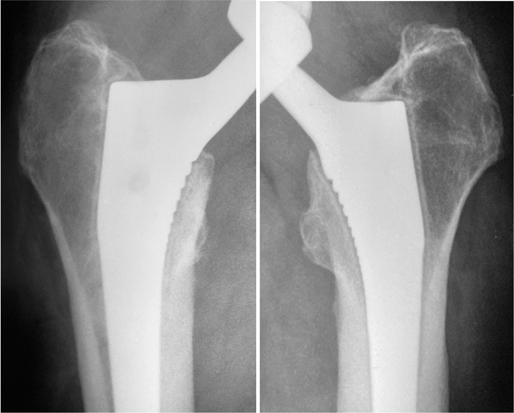
This report presents the case of a 52-year-old male with Dorr A femoral morphology diagnosed with bilateral avascular necrosis and osteoarthritis (Figure 1). His diagnosis of osteonecrosis was idiopathic in etiology with no history of alcoholism or steroid use implicated in this finding. Symptom onset was gradual following an injury in August 2008 when he had an occupational fall from a 4-meter ladder. Attempts at core decompression failed to save his hip and his continued symptoms severely impacted his activities of daily life. Non-operative management was attempted; however, this proved unsuccessful and he underwent a left THA in May 2009, followed by a right THA in January 2010. At the time of surgery his height was 1.75 m, weight was 88.5 kg, and his BMI was 29. Size 12 high-offset (48 mm) collarless Corail femoral stems were used in both right and left procedures. Reliable measurement of his preoperative offset is difficult with available radiographs, though the patient had no coxa vara or coxa valga. A ceramic head with a highly cross-linked polyethylene liner (CoP) was utilized as the bearing couple on the left hip, and on his right hip a Pinnacle acetabular shell with a 36-mm inner diameter metal liner and a 36-mm metal femoral head (metal on metal, MoM) was utilized.
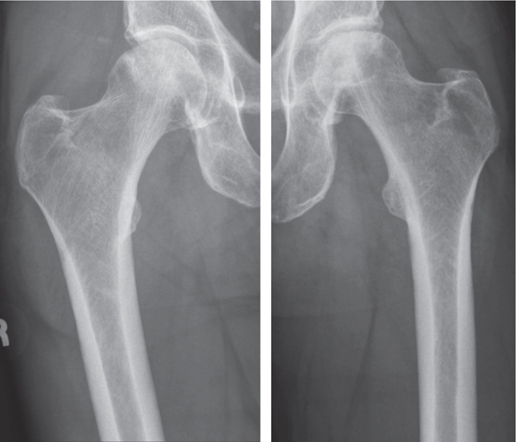
Figure 1. Preoperative Dorr A femoral morphology.
The patient was initially seen for consultation in our referral center for complaints of bilateral hip pain that had a gradual onset over the prior 1–2 years. Radiolucent lines had also started to become apparent at that time. Serum metal ion values were elevated with serum chromium in range at 1.8 μg/L (ref < 5.0) and serum cobalt out of range at 1.6 μg/L (ref < 1.0). These results in conjunction with the patient’s symptoms were believed to be consistent with a metal hypersensitivity reaction and subsequent revision surgery was performed in November 2014. A pseudotumor with dark brown synovial staining was seen, without any substantial bone or soft tissue destruction, consistent with the preoperative diagnosis of metal hypersensitivity. The acetabular shell and femoral stem were retained, as they were properly positioned and did not appear to be grossly loose. The MoM insert was exchanged for a polyethylene insert and a titanium-sleeved ceramic femoral head was implanted. His postoperative course was uncomplicated.
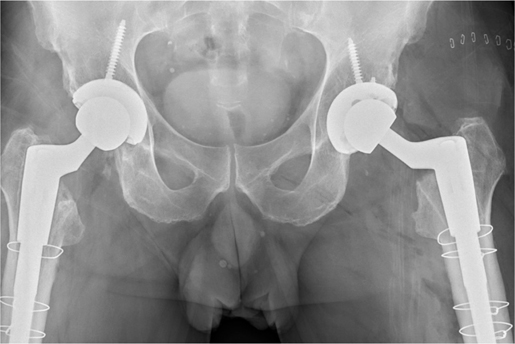
In September 2018, the patient returned for follow-up with a complaint of progressive bilateral hip and thigh pain. Radiographic evaluation revealed bilateral Corail stems that appeared well-fixed distally yet had progressive proximal radiolucencies. As seen in Figure 2, in 2010 there are subtle radiolucent lines (RLL) visible around the proximal stems in Gruen zones 1 and 7 bilaterally. By 2018, these RLLs have become more apparent, measuring on the right roughly 1.5 mm and 1 mm in Gruen zones 1 and 7 respectively, and on the left approximately 2.5 mm in Gruen zone 1 and 2 mm in Gruen zone 7 (Figure 3).
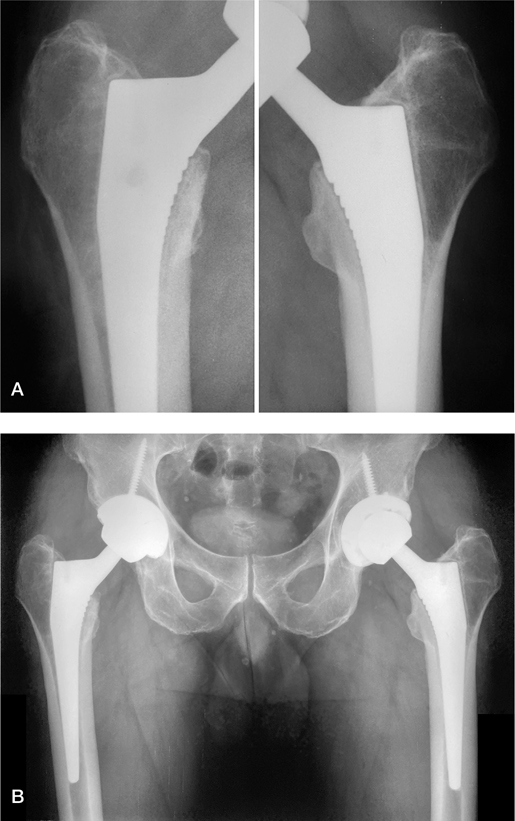
Figure 2. 2010 after bilateral THA (A) and 2014 (B).
A full workup including screening labs and nuclear medicine studies ruled out infection but revealed increased activity in the proximal femurs bilaterally in the delayed phase of a three-phase bone scan. The right hip was revised in December 2019. The preoperative diagnosis was aseptic loosening of the femoral stem. A posterolateral approach was used and upon initial examination no signs of chronic infection or inflammation were seen. After dislocation of the hip, forcible stress applied to the trunnion revealed visible motion between the proximal stem and the host bone, confirming the preoperative diagnosis. However, the senior surgeon (DS) was initially perplexed to discover that the femoral component could not be removed despite substantial and extended efforts; it remained well fixed distally. An extended trochanteric osteotomy (ETO) was required for stem removal. Once the femur was bivalved, direct visual examination revealed that the distal aspect of the stem was well fixed with robust bone attachment in the distal 2–3 cm of the stem.
The patient recovered without complications, and was ultimately satisfied with the results, with the right thigh pain sub-siding. However, he started to experience similar symptoms of thigh pain on the left side. The patient subsequently elected to have the left hip revised in March 2021. Proximal loosening of the stem with distal fixation was again present. Given our experience with the right hip revision surgery, an ETO was promptly performed. It was estimated that between 50% and 75% of the proximal stem had no bone ingrowth, but as seen on the right side there was solid osseointegration of the distal end of the stem, resisting attempts at removal without an ETO. Due to the performance of the ETOs, long-stem revision femoral components were utilized on both sides (Depuy Reclaim 16 mm 190 mm angled) (Figure 4). The patient is recovering well without complications and is a highly active individual with full-time employment as a building maintenance supervisor. Though his radiographs do not provide a reliable measurement of postoperative offset, he has no postoperative indication of problems, indicating his offset has likely been anatomically restored. He is now largely pain-free, but he had to be subjected to extensive bilateral revision hip surgery, thus exposed to the possibility of major complications, to correct this clinical problem.
Discussion
The Corail stem has been widely used since 1986 and has excellent overall survivorship (1-3). However, some individuals may not be well-suited for its fully coated tapered stem design.
In a review of 41,265 Corail stems in the Australian Joint Replacement Registry, Hoskins et al. (4) found that the revision rate for aseptic loosening was 4 times higher in small stem sizes (sizes 8 and 9) than larger stem sizes, and this difference in revision rate was 6 times greater in male patients, and 14 times greater when the anterior approach was utilized. Another large registry study (5) corroborates these findings, reporting increased hazard rates for revision with smaller stem sizes, but also for subjects with hard bearings, including MoM as well as ceramic-on-ceramic (CoC). Radiographic findings were not available for either of these observational studies, and the exact reason(s) for these substantial differences in revision rates are unexplained. Stems below size 12 should be avoided in young, active men, especially in those patients with Dorr A bone morphology, which was a key factor in the stem selection size of this patient, which was size 12 bilaterally.
Relevant to the finding of an association between increased failure rate and MOM bearings, Gascoyne et al. (6) reported that proximal aseptic loosening occurred in 37% of Corail stems coupled with a MoM bearing, with a 7.25 times greater risk of loosening. They observed a relationship between the severity of taper corrosion and aseptic loosening and hypothesized that corrosion byproduct-activated macrophage-induced osteolysis and/or metal-induced lymphocytes releasing cytokines cause osteoclastic resorption, resulting in dissolution of the proximal HA coating, and thus progressive radiolucencies and ultimate loosening of the stem.
Our patient originally had a MoM bearing on the right but had the same issue of proximal loosening on left side, which was a CoP bearing. Thus, in this case, it does not appear that the presence of the MoM bearing on the right is exclusively responsible for the lack of proximal ingrowth. However, this MoM issue may be relevant in this case as the left THA was performed three years before the right THA, yet the right side became symptomatic before the left.
Buttaro et al. (7) reviewed 855 Corail cases and found 18 cases of metaphyseal debonding, with the same preoperative and intraoperative findings as with our case. The predominant finding was the development of radiolucent lines in the proximal Gruen zones 1, 7, 8, and 14. These patients were all initially asymptomatic and then developed progressive thigh pain and limp, with appearance of the abnormal radiographic findings. They were asymptomatic for a mean of 36 months. The surgical findings upon revision revealed that the proximal part of the stem was not osseointegrated, but the distal stem was well-fixed, allowing a “windshield wiper” movement, which could be confirmed at surgery. Paradoxically, despite being macroscopically loose proximally, these cases also required an osteotomy to remove the stem, as was required in our case.
Another report (8) describes a group of patients with the Corail stem with unexplained pain and without obvious radiographic signs of loosening, who underwent an experimental PET/CT protocol, revealing a marked difference in metabolic activity compared with a control group of pain-free Corail subjects. These subjects were found to have mechanically loose stems at revision.
Park et al. (9) found a relation between Dorr Type A femoral anatomy and the development of proximal radiolucent lines in total hip arthroplasty utilizing fully coated cementless tapered wedge stems similar in design to the Corail. This study found that at a 5-year follow-up, patients with Dorr type A femurs had a 7.8% incidence of radiolucent lines compared with 2.5% (p < 0.001). Other studies of fully HA-coated stems of a comparable design (10) as well as proximally coated stems (11,12) reveal similar findings. Additionally, Magill et al. (13) and Karayiannis et al. (14) both report a statistical relationship between under-sizing the Corail stem and the development of radiolucent lines in zone 7.
These reports point to the possibility of tight distal fixation in the champagne flute diaphysis of Dorr A bone, causing a dimensional mismatch between proximal and distal. The result is that the proximal stem is not mechanically stable because it is relatively undersized, and thus stable osseointegration does not occur. Distal fixation is achieved at the loss of proximal fixation. This is seen consistently across the multiple reports discussed, and is worse in the male subpopulation, presumably because there is a higher percentage of Dorr A anatomy, and it is found in greater frequency with the anterior surgical approach, presumably because femoral exposure is more difficult, making it harder to ensure the best stem size (largest possible) is implanted in every case.
These findings demonstrate the need to consider an alteration in surgical technique and/or prosthesis choice. One option recommended by the manufacturer is to ream the distal canal to allow larger stem sizes that will also fill the proximal anatomy, promoting stable osseointegration in the metaphysis. Additionally, use of a collar has been recommended and many long-term studies of the Corail have used the collared version of this stem (15). Alternatively, consideration of the avoidance of stem designs that do not allow a full fit and fill of the metaphysis, thus preventing “potting” in the diaphysis before the metaphysis is filled, may help avoid this complication. Another alternative would be the evaluation of design modifications to such stems, whereby, in the smaller size range, there are alternative sizes which increase the proximal body relative to the distal size.
Additionally, the full HA coating, thickness of HA coating, and relative smoothness of this stem has proven to be problematic in multiple areas of the current literature as shown by Jaffe et al. (16). Jaffe et al. performed a thorough analysis of HA-coated prostheses revealing benefits of expedited osseointegration provided by HA coating; however, the best results are seen with HA coatings in the 25–75 mm range, and increasing the coating thickness beyond this range can be counter-productive (16). Hailer et al. concluded that there was no clinically significant advantage to utilizing a full HA coating in uncemented stems (17). Perhaps eliminating the HA coating from the distal aspect of the stem should be considered. Another alternative would be utilizing a proximally porous-coated stem without HA coating, which has yielded superior results (17). There is strong evidence that the promotion of proximal fixation over distal fixation improves the long-term performance of hip implants by minimizing the deleterious effects of adaptive bone remodeling (18).
It is difficult to indicate a patient for major revision surgery, one that may require the use of an ETO and implantation of a long revision stem, when the femoral component is not loose through its whole surface, and thus does not demonstrate gross, macroscopic loosening with subsidence. In fact, the operating surgeon was surprised by the difficulty encountered in removing these stems despite a lack of proximal fixation. It has subsequently come to our attention that there are osteotomes designed specifically for this implant. Our patient was told by the implanting surgeon that there was no problem, prompting him to seek a second opinion. It is possible that this issue is underreported (11), and that a higher percentage of Corail stems, and those with similar designs, are in fact lacking metaphyseal fixation and demonstrating a “windshield washer” finding with distal fixation.
Conclusion
The Corail stem has demonstrated excellent long-term survival, yet it is found to fail in a small percentage of cases. There appears to be a common denominator to these failures, which is that distal fixation is achieved at the loss of proximal fixation. The stem is “potted” distally with osseointegration to the HA-coated surface, and metaphyseal fixation is absent. This is a progressive process, initially with the possibility of normal findings on plain radiographs, but serial examination reveals the development of RLLs. Revision surgery likely requires an ETO to remove the stem, and the patient is subjected to substantial risks. Proper preoperative planning and prosthesis selection optimized for the patient’s individual anatomy, adjustments to surgical technique, and consideration of design modifications could address this problem and improve outcomes, avoiding this potentially serious complication associated with the use of these devices.
Ethical approval and consent
Written informed consent was obtained from the patient for this report to include publication of case and associated images.
- Vidalain J P. Twenty-year results of the cementless Corail stem. Int Orthop 2011; 35(2): 189-94.
- Jacquot L, Bonnin M P, Machenaud A, Chouteau J, Saffarini M, Vidalain J P. Clinical and radiographic outcomes at 25-30 years of a hip stem fully coated with hydroxylapatite. J Arthroplasty 2018; 33(2): 482-90.
- Louboutin L, Viste A, Desmarchelier R, Fessy M H. Long-term survivorship of the Corail™ standard stem. Orthop Traumatol Surg Res 2017; 103(7): 987-92.
- Hoskins W T, Bingham R J, Lorimer M, de Steiger R N. The effect of size for a hydroxyapatite-coated cementless implant on component revision in total hip arthroplasty: an analysis of 41,265 stems. J Arthroplasty 2020; 35(4): 1074-8.
- Jameson S S, Baker P N, Mason J, Rymaszewska M, Gregg P J, Deehan D J, et al. Independent predictors of failure up to 7.5 years after 35 386 single-brand cementless total hip replacements: a retrospective cohort study using National Joint Registry data. Bone Joint J 2013; 95-b(6): 747-57.
- Gascoyne T, Flynn B, Turgeon T, Burnell C. Mid-term progressive loosening of hydroxyapatite-coated femoral stems paired with a metal-onmetal bearing. J Orthop Surg Res 2019; 14(1): 225.
- Buttaro M A, Oñativia J I, Slullitel P A, Andreoli M, Comba F, Zanotti G, et al. Metaphyseal debonding of the Corail collarless cementless stem: report of 18 cases and case-control study. Bone Joint 2017; 99-B(11): 1435-41.
- Ullmark G. Occult hip prosthetic loosening diagnosed by [18F] Fluoride-PET/CT. Arthroplast Today 2020; 6(3): 548-51.
- Park C W, Eun H J, Oh S H, Kim H J, Lim S J, Park Y S. Femoral stem survivorship in Dorr Type A femurs after total hip arthroplasty using a cementless tapered wedge stem: a matched comparative study with Type B femurs. J Arthroplasty 2019; 34(3): 527-33.
- D’Ambrosio A, Peduzzi L, Roche O, Bothorel H, Saffarini M, Bonnomet F. Influence of femoral morphology and canal fill ratio on early radiological and clinical outcomes of uncemented total hip arthroplasty using a fully coated stem. Bone Joint Res 2020; 9(4): 182-91.
- Cooper H J, Jacob A P, Rodriguez J A. Distal fixation of proximally coated tapered stems may predispose to a failure of osteointegration. J Arthroplasty 2011; 26(6 Suppl.): 78-83.
- Ishii S, Homma Y, Baba T, Ozaki Y, Matsumoto M, Kaneko K. Does the canal fill ratio and femoral morphology of Asian females influence early radiographic outcomes of total hip arthroplasty with an uncemented proximally coated, tapered-wedge stem? J Arthroplasty 2016; 31(7): 1524-8.
- Magill P, Hill J, O’Brien S, Stevenson M, Machenaud A, Beverland D. Observed effect of femoral component undersizing and a collarless design in the development of radiolucent lines in cementless total hip arthroplasty. Arthroplast Today 2020; 6(1): 99-103.
- Karayiannis P N, Cassidy R S, Isaac G, Hughes I, Hill J C, Machenaud A, et al. Risk factors for significant radiolucent line development in a fully coated hydroxyapatite stem. J Arthroplasty 2021; 36(11): 3709-15.
- Melbye S M, Haug S C D, Fenstad A M, Furnes O, Gjertsen J, Hallan G. How does implant survivorship vary with different Corail femoral stem variants? Results of 51,212 cases with up to 20 years of follow-up from the Norwegian Arthroplasty Register. Clin Orthop Relat Res 2021; 497: 2169-80.
- Jaffe W L, Scott D F. Current concepts review total hip arthroplasty with hydroxyapatite-coated prostheses. J Bone Joint Surg 1996; 78(12): 1918-34.
- Hailer N P, Lazarinis S, Makela K T, Eskelinen A, Fenstad A M, Hallan G, et al. Hydroxyapatite coating does not improve uncemented stem survival after total hip arthroplasty. Acta Orthop 2015; 86(1): 18-25.
- Sumner D R. Long-term implant fixation and stress-shielding in total hip replacement. J Biomechanics 2015; 48(5): 797-800.