Pain medication purchases before and after total hip and knee arthroplasty: a register study of 329,743 arthroplasties
Ville TURPPO 1, Reijo SUND 1,2, Jukka HUOPIO 3, Heikki KRÖGER 1,3, and Joonas SIROLA 1,3
1 Kuopio Musculoskeletal Research Unit (KMRU), Institute of Clinical Medicine, University of Eastern Finland (UEF), Kuopio; 2 Unit of Health Economics and Equity in Health Care, Department of Public Health and Welfare, Finnish Institute for Health and Welfare (THL), Helsinki; 3 Department of Orthopaedics, Traumatology and Hand Surgery, Kuopio University Hospital, Kuopio, Finland
Background and purpose — Total hip (THA) and knee (TKA) arthroplasty are effective pain treatment in osteoarthritis; however, there are patients with long-term pain and in need of analgesics. We studied purchases of paracetamol, non-steroidal anti-inflammatory drugs (NSAIDs), opioids, and neuropathic pain medication before and after THA or TKA.
Patients and methods — We searched all THA (n = 149,158) and TKA (n = 180,585) cases in Finland between the years 1998 and 2018 and the drug purchases made by patients during 1997–2018 using linked Finnish register data. Drug purchases were studied in 3-month periods.
Results — The purchases of all analgesics increased from 3 years before operation to 3 months before operation. Around the time of THA or TKA, the purchases of all analgesics spiked to 7–56%, depending on drug. The purchases of all analgesics decreased rapidly during the first 6 months postoperatively. Purchases of paracetamol, NSAIDs, and opioids at 6 months postoperatively (6–23%) were lower than they were at 3 months preoperatively. At 3 years postoperatively, only paracetamol purchases were lower (15–18%) postoperatively than they were 3 years before arthroplasty. NSAID, opioid, and neuropathic pain medication purchases remained higher (4–14%).
Interpretation — THA and TKA stop and reduce the preoperative increases in purchases of paracetamol, NSAIDs, and opioids. The purchases of pain medications by THA and TKA patients 1 year after operation are close to those in the general population.
Citation: Acta Orthopaedica 2022; 93: 534–541. DOI http://dx.doi.org/10.2340/17453674.2022.2929.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-02-28. Accepted: 2022-05-04. Published: 2022-06-08.
Correspondence: ville.turppo@gmail.com
TV, SR, HJ, KH, SJ: writing the manuscript. TV, SR, SJ: data analysis and interpretation of the results. SR, HJ, KH, SJ: supervision of the study and proofreading.
Acta thanks Jan A N Verhaar and Carl-Olav Stiller for help with peer review of this study.
According to Finnish Current Care treatment guidelines paracetamol is the primary analgesic for osteoarthritis (OA). The next step is to use non-steroidal anti-inflammatory drugs (NSAIDs). Opioids should be used only when pain cannot be controlled otherwise (1). Some patients may develop pain sensitization, and medication for neuropathic pain can then be used (e.g., antidepressants and anticonvulsants) (1-3).
When pain and disability of hip and knee OA cannot be controlled adequately by nonoperative means, the next treatment is usually total hip (THA) or knee arthroplasty (TKA). These surgical interventions have good long-term results for physical capability and well-being (4). However, prior studies have shown THA and TKA patients reporting unfavorable longterm pain outcomes from 2% to even over 20% (5,6).
Postoperative pain management includes the same medicines as before operation. Prior studies on perioperative pain management have mainly focused on opioid use, showing that preoperative opioid use is the strongest risk factor for long-term opioid use after THA or TKA (7,8). A few papers report pain medication consumption before and after THA or TKA and show an increase in analgesic use a few months before operation and then a decrease after operation, but a noticeable number of patients continue using analgesics long term (9-11). 1 study reports increased analgesic use after TKA (12).
As patients undergo THAs and TKAs to treat pain and disability caused by osteoarthritis, pain medication purchases and consumption can be considered an indirect outcome measure for arthroplasties. We hypothesize that pain medication purchases are reduced after THA and TKA and we studied the purchases of different types of analgesics (paracetamol/acetaminophen, NSAIDs, opioids, medication for neuropathic pain) in the years before and after THA and TKA.
Patients and methods
Data sources
The data is provided by the Finnish Institute for Health and Welfare and their PERFECT (PERFormance, Effectiveness, and Cost of Treatment episodes) project, which started in 2004. This was established to monitor specialized medical care treatment episodes, and it includes data on diseases and procedures with high costs and number of patients (e.g., arthroplasty). Data has been collected by combining data from multiple registers. In this study, we focus on data from the Care Register for Health Care (CRHC), the Finnish Arthroplasty Register (FAR), and the Social Insurance Institution of Finland (SII). The CRHC records all special healthcare hospital admissions. It holds records of arthroplasty operations since 1987. The FAR is maintained by the Finnish Institute for Health and Welfare, and it includes data on THAs and TKAs since 1980. SII’s registers provide information on all dispensed prescriptions and reimbursements for medicine expenses since 1994, yet in PERFECT the prescription data starts from the year 1997 (13).
Included patients and analgesics
Using the CRHC and FAR data, we searched for all primary THAs and TKAs in Finland during 1998–2018. Eventually, 149,158 THAs and 180,585 TKAs were found (Table 1). Next, all purchases of prescription medication of interest during 1997–2018 for arthroplasty patients up to 15 years before and after arthroplasty were searched (Figure 1 and 2, see Supplementary data). For additional sensitivity analysis (Figure 3 and Table 2, see Supplementary data) we searched for other arthroplasties (revision or arthroplasty of other joint) for the patients in the original population. If other arthroplasties were found, the follow-up for drug purchases was ended directly before those. Eventually there were 104,045 THA and 117,203 TKA patients (at the time of arthroplasty) included in the analysis. The Anatomical Therapeutic Chemical (ATC) codes were used to identify prescriptions of interest, and the following analgesics were included: paracetamol/acetaminophen (N02BE00), oral NSAIDs (M01A***, N02B*** excluding N02BE00), oral and transdermal opioids (N02A***, N07B***), antidepressants (venlafaxine/N06AX16, duloxetine/N06AX21, amitriptyline/N06AA09, and nortriptyline/N06AA10), and anticonvulsants (pregabalin/N03AX16, gabapentin/N03AX12). We divided the drugs into 4 groups—paracetamol, NSAIDs, opioids, and neuropathic pain medication—following the treatment guidelines for osteoarthritis (1,2).
The available register data did not reveal non-prescription drugs, whether the pills were consumed after purchase, or the indication for use. In Finland, there are smaller packages of paracetamol, and some NSAIDs (ibuprofen, ketoprofen, and acetylsalicylic acid) that are prescription-free and sold “over the counter,” and these are not captured by the register. However, a prescription is needed to get the reimbursed price for the drugs, and a maximum of three months’ supply of pills can be purchased in advance. All this results in a practice whereby purchases of prescribed drugs can be followed easily, and for continuous users there will be purchases of drugs at least once every 3 months.
For the purposes of this particular study, the individual data was processed into aggregate form that included a matrix of the number of patients who had drug purchases in certain 3-month window before or after arthroplasties and the total number of patients with follow-up in that window. Time-windows covered periods up to about 15 years before and after the arthroplasty operation, but for the purposes of this study we focused only on the ±3 years since THA/TKA. The data was stratified by drug group, sex, year group of THA/TKA, and by age (< 70 years, ≥ 70 years). Such data allowed us to calculate the proportion of patients purchasing drugs for each 3-month period.
Statistics
The Statistical Package for the Social Sciences (SPSS), version 27 (IBM Corp, Armonk, NY, USA) was used for statistical analysis. A chi-square test was used to compare whether the proportions of patients purchasing certain pain medication at different follow-up points are statistically significantly different. We calculated 95% confidence intervals (CI) for proportions of purchases for all pain medications during the follow-up. For this calculation, results from all follow-up points (3-month intervals) from 3 years before until 3 years after THA or TKA were included. Also, 95% CIs were calculated for proportion of purchases of different pain medications at certain time points.
Ethics, funding, potential conflicts of interest, and data sharing
The Finnish Institute for Health and Welfare has granted permission for the PERFECT project data (THL/538/6.02.00/2019). This work was supported by the Päivikki and Sakari Sohlberg Foundation and the North-Savo Regional Fund of the Finnish Cultural Foundation. The authors have no conflicting interests to report. Due to privacy regulations the original data cannot be shared. Anonymized summary tables can be shared on reasonable request.
Results
Time frame of follow-up
The complete register data included up to 15 years of pre- and postoperative follow-up data on dispensed prescriptions. Each THA and TKA had its own follow-up time, depending on when it was conducted during 1998–2018. Thus, the number of arthroplasties available at different follow-up points varied, as seen in Figure 1 (see Supplementary data). At the beginning and at the end of the follow-up, the number of arthroplasties was lower due to a lack of follow-up data (i.e., drug purchases before 1997 or after 2018), and we decided to focus on the follow-up of 3 years before and after arthroplasty.
Analgesics
Analgesics purchases before arthroplasty increase in all groups when getting closer to THA or TKA (Figure 4 and Table 3). The proportions of purchases for all analgesics and groups peaks around the time of arthroplasty. THA and TKA seemed to stop this rapid increase in analgesics purchases. The greatest decrease in purchases occurred during the 1st postoperative months, so that that the purchases of paracetamol, NSAIDs, and opioids decreased below the level they were 3–6 months before the arthroplasties. After that, the analgesics purchases stayed approximately on the same level until the end of follow-up. Eventually, 4–18% of arthroplasty patients were purchasing analgesics, depending on the group and analgesic, at the end of follow-up. Only paracetamol purchases decreased when postoperative proportions of purchases were compared with the proportions years before arthroplasty.
| Paracetamol | NSAIDs | Opioids | Neuropathic pain medication | |
| THA patients | ||||
| 3 years preoperative | 21 | 6 | 3 | 3 |
| 2 years preoperative | 25 | 8 | 4 | 3 |
| 1 year preoperative | 33 | 12 | 7 | 4 |
| Arthroplasty | 46 | 29 | 17 | 7 |
| 1 year postoperative | 17 | 10 | 5 | 4 |
| 2 years postoperative | 16 | 11 | 5 | 4 |
| 3 years postoperative | 15 | 11 | 5 | 4 |
| 95% confidence intervals a | ||||
| Lower limit | 15 | 9 | 4 | 2.9 |
| Upper limit | 17 | 11 | 6 | 3.4 |
| TKA patients | ||||
| 3 years preoperative | 25 | 7 | 3 | 3 |
| 2 years preoperative | 27 | 9 | 4 | 4 |
| 1 year preoperative | 31 | 12 | 6 | 4 |
| Arthroplasty | 56 | 33 | 25 | 9 |
| 1 year postoperative | 21 | 12 | 6 | 4 |
| 2 years postoperative | 19 | 13 | 6 | 5 |
| 3 years postoperative | 18 | 14 | 7 | 5 |
| 95% confidence intervals a | ||||
| Lower limit | 17 | 11 | 5 | 3.7 |
| Upper limit | 19 | 14 | 7 | 4.3 |
| The Finnish general | ||||
| population in 2018 | 15 | 26 | 8 | 4 b |
| aCalculated using all follow-up points (3-month intervals). | ||||
| bAmitriptyline was not included in the calculations, as prescription data could not be acquired. | ||||
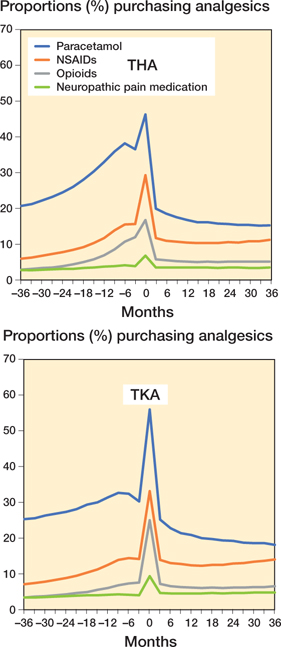
Figure 4. Proportions of patients purchasing analgesics from 3 years before to 3 years after THA/TKA.
Paracetamol was the most purchased pain medication among both THA and TKA patients (Figure 4 and Table 3). After arthroplasty, paracetamol purchases were clearly reduced, and at 3 years postoperatively, the proportion of patients purchasing paracetamol (THA 15%, CI 15.1–15.5; TKA 18%, CI 17.9–18.3) was lower than 1 year before the operation in both joints (p < 0.001) (Table 4). TKA patients purchased a little more paracetamol postoperatively than THA patients.
NSAIDs were the second most purchased drug by all patient groups. Even though arthroplasty seemed to reduce NSAID purchases when the first postoperative months were compared with the final preoperative year, the proportions of patients purchasing NSAIDs at 3 years after THA (11%, CI 11.1–11.5) and TKA (14%, CI 13.9–14.3) were higher than the results from more than 1 year before arthroplasty (Figure 4, Tables 3 and 4).
Around the time of arthroplasty, the proportions of patients purchasing opioids were THA 17% (CI 16.6–17.0) and TKA 25% (CI 24.8–25.2) (Figure 4 and Table 3). The lowest level of purchases (5–6%) was reached approximately 12 months after arthroplasty, which was lower than during the final months preoperatively. After the 1st postoperative year, the purchases remained on the same level.
Neuropathic pain medication (antidepressants and anticonvulsants) had a low number of patients purchasing drugs through follow-up, mainly less than 5% (Figure 4 and Table 3). The purchases of these analgesics also peaked around the time of THA and TKA, as for the other analgesics. However, the proportion of purchases seemed not to be affected by arthroplasty. Purchases of these drugs increased steadily but by only 0.7–1.4% during the 6 years of follow-up. Eventually, 3.5% (CI 3.4–3.7) of THA and 4.8% (CI 4.7–4.9) of TKA patients were purchasing neuropathic pain medication.
Only one THA or TKA during follow-up
A sensitivity analysis was performed to determine the effect of arthroplasties of other joints or revisions on the primary results. Thus, in this analysis, only the 1st ever THA or TKA arthroplasties of the patients were included, and the follow-up was terminated if the THA or TKA patient had other THA or TKA arthroplasties or revisions. These THA and TKA cases also had a steady increase in purchases of all analgesics from 3 years until the final months before arthroplasty (Figure 3 and Table 2, see Supplementary data). The drug purchases then peaked around the time of arthroplasty. The greatest decrease in purchases of analgesics occurred during the 1st postoperative months, and then the proportion of patients purchasing drugs stabilized. At the end of follow-up, the proportion of patients purchasing analgesics was 3–17%, depending on the joint and drug. Paracetamol was the only drug with a lower proportion of purchases 3 years postoperatively compared with 3 years before the operation, among both THA and TKA patients.
Effect of age during arthroplasty on the results
The effect of age on purchases of pain medications was studied by dividing the patients into groups by the age at the time of arthroplasty (Table 5, see Supplementary data). Under 70-year-old patients purchased slightly more paracetamol (14–15% more at the time of arthroplasty) and a few less NSAIDs (3–6% less at the time of arthroplasty) throughout the follow-up compared with over 70-year-old THA and TKA patients. In opioids and neuropathic pain medication the younger patients purchased more drugs at the time of arthroplasty. Yet, during other follow-ups there were minimal or no differences between age groups.
Effect of time frame of the arthroplasty on results
Supplementary data 1 shows larger changes in the number of arthroplasties postoperatively than preoperatively. This is mainly due to short follow-up times of some arthroplasty events. Some arthroplasties were done close to the end of follow-up (2018) and they do not have long postoperative follow-ups. We studied whether the original results were affected by this phenomenon. We excluded arthroplasties from the last 6 years of follow-up (2012–2018). In this analysis the number of arthroplasties in the postoperative follow-up remained more stable, with 198,591 total (THA + TKA) events at the time of arthroplasty and 189,520 events at three years postoperatively. The patterns of medication purchases were similar to the original results and the proportion were within a few percentage points (maximum of 4 percentage points difference). NSAIDs were purchased a little less often than in the original results. During arthroplasty this was 11 and during the follow-up 2–6 percentage points less by both THA and TKA patients.
Discussion
Both THA and TKA seemed to reduce the purchases of paracetamol, NSAIDs, and opioids when the perioperative purchases were studied. However, extending the follow-up time revealed that only the purchases of paracetamol were reduced after arthroplasty when compared with the results more than 1 year before arthroplasty. The greatest reduction in drug purchases occurred during the first 6 months after THA or TKA. Reduction in purchases continues until 12 months, after which the proportion of patients purchasing analgesics stabilizes. Approximately 4–18% of arthroplasty patients were purchasing different analgesics at 3 years postoperatively. Beswick et al., in their review of 14 articles, describe 2–23% of THA and 10–34% of TKA patients reporting unfavorable pain outcome during long-term follow-up (5).
Prescription analgesics purchases in the Finnish population
The proportions of patients purchasing drugs were close to that of drug purchases in the general population. In 2018, paracetamol was purchased by 15% (prescription purchases only), NSAIDs by 26%, and opioids by 8% of the population in Finland (SII’s registers) (14).
Analgesics purchases compared with prior literature
Paracetamol was the most purchased drug in all groups, which is in line with care guidelines, with paracetamol being the primary drug recommended for osteoarthritis (1,3). Around the time of arthroplasty, the proportion of patients purchasing paracetamol was 46–56%. Prior studies have reported paracetamol use ranging from 24% to 88% at a point close to THA or TKA (9,10,12). At 12 months postoperatively, paracetamol was purchased by 17–21% of THA and TKA patients, which is close to the 24% reported by Jørgensen et al. (10). Paracetamol was the only drug with lower proportions of purchases postoperatively than 1–3 years before arthroplasty. At the end of follow-up, THA and TKA patients’ paracetamol purchases were on the same level as in the general population. Prescription purchases of paracetamol were made by 15% of Finland’s population (14).
NSAIDs were purchased second most among both THA and TKA patients. In a prior Finnish study by Rajamäki et al. (9) the results are different. In their study, NSAIDs were the most used single group of analgesics. They report higher numbers of use at 3 months postoperatively (> 50% THA and > 60% TKA). However, at 2 years postoperatively, the level of NSAID use was comparable to the proportion of NSAID purchases in our study. Bolland et al. (15) report 21% of THA and TKA patients being NSAID users 1 year preoperatively, which is a little more than the NSAID purchases in our study from the same time period. They also conclude that the decrease in NSAID use occurs during the 1st year postoperatively. Our results support this conclusion, with the decrease in purchases happening during the 1st postoperative year. In 2018 in Finland, NSAIDs were purchased by 26% of the general population, which is a little more than among arthroplasty patients at the end of follow-up (14).
In prior studies, the number of opioid users is close to the levels of opioid purchases in our study, with increasing use preoperatively and some residual users after the 1st postoperative year (9,10,12,16,17).
In our study, THA patients purchased more opioids than TKA patients before arthroplasty, if the peak of purchases perioperatively is excluded. After arthroplasty, TKA patients had a higher proportion of opioid purchases. Rajamäki et al. also report THA patients using more mild opioids preoperatively, whereas TKA patients used more opioids postoperatively. Also, the postoperative proportions of mild opioid users (5–8%) were similar to our study (9). Opioid purchases were made by 8% of the general population in Finland in 2018, which is a few percentage points higher than in our study at 3 years after arthroplasty.
Neither NSAID nor opioid purchases were reduced when postoperative results were compared with the results from 1 to 3 years before arthroplasty. However, the postoperative levels of NSAID and opioid purchases were on similar levels to those among the general population. This could indicate that the patients had other diseases causing drug purchases. However, they may also have developed an addiction or a habit of treating pain with opioids. The side effects of NSAIDs need special attention when treating older people with possible comorbidities (18). More importantly, opioids have side effects and dependency potential that need consideration in all patient groups and that clinicians need to consider thoroughly, whether prescribing opioids or referring the patient for surgery (19).
Medication for neuropathic pain had the fewest purchases and the purchases remained constant during follow-up, except around the time of arthroplasty. These drugs are also used for other conditions, such as depression, epilepsy, and fibromyalgia, which are likely to explain the “base” level of consumption. The proportions of purchases were close to the levels of neuropathic pain medication use reported by Jørgensen et al. (10) for THA and TKA patients, at 6.5% preoperatively and 8.6% postoperatively. Medication for neuropathic pain is only conditionally recommended by osteoarthritis current care guidelines, and thus the low level of purchases was a predictable outcome (1,2). However, prior literature estimates that at least 23% of THA and TKA patients have neuropathic pain (20). Osteoarthritis patients also develop pain sensitization in the affected joints and even peripheral sites (21).
Strengths and limitations
We analyzed the proportions of THA and TKA patients purchasing different drugs. The design and data were limited, so that we were able to see the prescription drug purchases only and were unable to consider doses or actual individual-level drug use. Also, over-the-counter pain medication purchases were not captured. In every class of drugs, there were patients purchasing drugs at the end of follow-up. During aging, several other medical conditions require pain medication. Some patients with the longest follow-up were 6 years older at the end of study. The patients may have had degenerative diseases in other joints and in the spine, too, that required prescribed pain medication. However, the postoperative purchases were the same or close to those made by the general population. Also, as we compared patients based on age at the time of arthroplasty, only small differences between under- and over-70-year-old patients could be seen. Even more, the younger patients seemed to purchase more paracetamol, opioids, and neuropathic pain medication at the time of arthroplasty. In the sensitivity analysis, we excluded other arthroplasties and revisions, and the results were very similar to the primary results during the entire follow-up. We used aggregated-level data, which does not support individual-level analyses. In future studies, it will be interesting to study specific subgroups of arthroplasty patients (i.e., other medical conditions and fixation method of the implant) and their pain medication purchases. The strengths of this study are large nationwide registers and long follow-up times. The registers contain all THA and TKA cases and drug purchases made by the patients, enabling follow-up times up to 15 years before and after arthroplasty.
Conclusion
THA and TKA stop and reduce the preoperative increases in purchases of paracetamol, NSAIDs, and opioids. The purchases of pain medications by THA and TKA patients one year after operation are close to those in the general population
- Working group set up by the Finnish Medical Society Duodecim and the Finnish Orthopaedic Assocation. Knee and hip osteoarthritis; 2018. Available from: www.kaypahoito.fi (Accessed July 1, 2021).
- Hochberg M C, Altman R D, April K T, Benkhalti M, Guyatt G, McGowan J, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken) 2012; 64(4): 465-74.
- Hunter D J, Bierma-Zeinstra S. Osteoarthritis. Lancet 2019; 393(10182): 1745-59.
- Turppo V, Sund R, Huopio J, Kröger H, Sirola J. Physical capability after total joint arthroplasty: long-term population-based follow-up study of 6,462 women. Acta Orthop 2021; 92(5): 551-6.
- Beswick A D, Wylde V, Gooberman-Hill R, Blom A, Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open 2012; 2(1): e000435-000435.
- Mercurio M, Gasparini G, Carbone E A, Galasso O, Segura-Garcia C. Personality traits predict residual pain after total hip and knee arthroplasty. Int Orthop 2020; 44(7): 1263-70.
- Sheth D S, Ho N, Pio J R, Zill P, Tovar S, Namba R S. Prolonged opioid use after primary total knee and total hip arthroplasty: prospective evaluation of risk factors and psychological profile for depression, pain catastrophizing, and aberrant drug-related behavior. J Arthroplasty 2020; 35(12): 3535-44.
- Franklin P D, Karbassi J A, Li W, Yang W, Ayers D C. Reduction in narcotic use after primary total knee arthroplasty and association with patient pain relief and satisfaction. J Arthroplasty 2010; 25(6 Suppl.): 12-16.
- Rajamäki T J Jr, Puolakka P A, Hietaharju A, Moilanen T, Jämsen E. Use of prescription analgesic drugs before and after hip or knee replacement in patients with osteoarthritis. BMC Musculoskelet Disord 2019; 20(1): 427-4.
- Jørgensen C C, Petersen M, Kehlet H, Aasvang E K. Analgesic consumption trajectories in 8975 patients 1 year after fast-track total hip or knee arthroplasty. Eur J Pain 2018; Apr 20.
- Blågestad T, Nordhus I H, Grønli J, Engesæter L B, Ruths S, Ranhoff A H, et al. Prescription trajectories and effect of total hip arthroplasty on the use of analgesics, hypnotics, antidepressants, and anxiolytics: results from a population of total hip arthroplasty patients. Pain 2016; 157(3): 643-51.
- Fuzier R, Serres I, Bourrel R, Palmaro A, Montastruc J L, Lapeyre-Mestre M. Analgesic drug consumption increases after knee arthroplasty: a pharmacoepidemiological study investigating postoperative pain. Pain 2014; 155(7): 1339-45.
- Peltola M, Juntunen M, Häkkinen U, Rosenqvist G, Seppälä T T, Sund R. A methodological approach for register-based evaluation of cost and outcomes in health care. Ann Med 2011; 43(Suppl. 1): 4.
- KELA—Lääkekorvausten saajat ja reseptitiedot. Available from: http://raportit.kela.fi/ibi_apps/WFServlet?IBIF_ex=NIT137AL (Accessed October 6, 2021).
- Bolland B J, Culliford D J, Maskell J, Latham J M, Dunlop D G, Arden N K. The effect of hip and knee arthroplasty on oral anti-inflammatory use and the relationship to body mass index: results from the UK general practice research database. Osteoarthritis Cartilage 2011; 19(1): 29-36.
- Wilson R, Pryymachenko Y, Audas R, Abbott J H. Long-term opioid medication use before and after joint replacement surgery in New Zealand. N Z Med J 2019; 132(1507): 33-47.
- Kim S C, Choudhry N, Franklin J M, Bykov K, Eikermann M, Lii J, et al. Patterns and predictors of persistent opioid use following hip or knee arthroplasty. Osteoarthritis Cartilage 2017; 25(9): 1399-1406.
- Wongrakpanich S, Wongrakpanich A, Melhado K, Rangaswami J. A comprehensive review of non-steroidal anti-inflammatory drug use in the elderly. Aging Dis 2018; 9(1): 143-50.
- Benyamin R, Trescot A M, Datta S, Buenaventura R, Adlaka R, Sehgal N, et al. Opioid complications and side effects. Pain Physician 2008; 11(2 Suppl.): 105.
- French H P, Smart K M, Doyle F. Prevalence of neuropathic pain in knee or hip osteoarthritis: a systematic review and meta-analysis. Semin Arthritis Rheum 2017; 47(1): 1-8.
- Suokas A K, Walsh D A, McWilliams D F, Condon L, Moreton B, Wylde V, et al. Quantitative sensory testing in painful osteoarthritis: a systematic review and meta-analysis. Osteoarthritis Cartilage 2012; 20(10): 1075-85.
Supplementary data
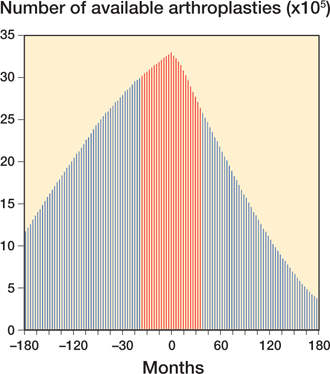
Figure 1. The number of available THAs and TKAs for entire follow-up time. The red columns (±36 months) represent the timeframe included in the study.
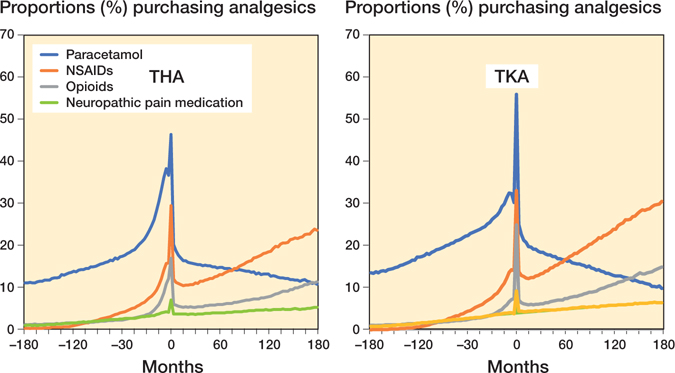
Figure 2. Proportions of patients purchasing analgesics for entire follow-up time available from the data.
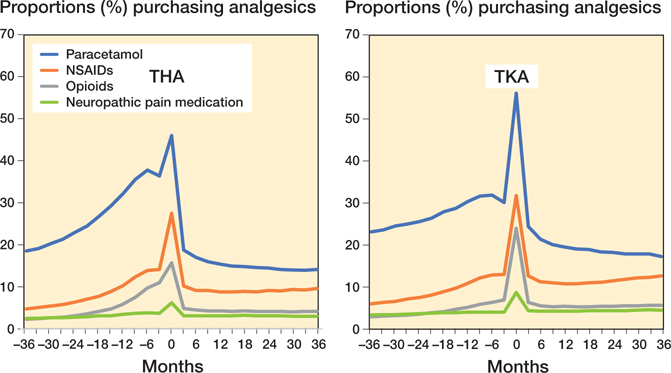
Figure 3. Proportions of patients purchasing analgesics for individuals with only 1 arthroplasty during follow-up.