Feasibility, safety, and patient-reported outcomes 90 days after same-day total knee arthroplasty: a matched cohort study
Anne Mette SCHMIDT 1,2, Mette GARVAL 1, Kirill GROMOV 3, Carsten HOLM 1, Jens R LARSEN 1,4, Charlotte RUNGE 1,4, Morten VASE 1, Lone R MIKKELSEN 1,4, Louise MORTENSEN 1,5,6, and Søren T SKOU 7,8
1 Elective Surgery Centre, Silkeborg Regional Hospital; 2 University Research Clinic for Innovative Patient Pathways, Diagnostic Centre, Silkeborg Regional Hospital; 3 Department of Orthopedic Surgery, Copenhagen University Hospital, Hvidovre; 4 Department of Clinical Medicine, Aarhus University, Aarhus; 5 Department of Physiotherapy and Occupational Therapy, Aarhus University Hospital, Aarhus; 6 Orthopaedic Research Unit, Aarhus University Hospital, Aarhus; 7 Research Unit for Musculoskeletal Function and Physiotherapy, Department of Sports Science and Clinical Biomechanics, University of Southern Denmark; 8 The Research Unit PROgrez, Department of Physiotherapy and Occupational Therapy, Næstved-Ringsted-Slagelse Hospital, Denmark
Background and purpose — Despite increased attention to and acceptance of fast-track procedures, there is a lack of studies concerning discharge on the day of surgery (DOS) following total knee arthroplasty (SD-TKA). We evaluated the feasibility of SD-TKA, and compared safety and patientreported outcomes (PROs) between patients undergoing SD-TKA and patients undergoing standard TKA.
Patients and methods — A SD-TKA group (n = 101) was matched 1:1 to a standard TKA group (n = 101) on age, sex, and ASA score. Feasibility (being discharged on DOS), safety (unplanned contacts and complications evaluated by telephone calls (2 weeks), outpatient visits (2 weeks), and readmission (90 days)) were assessed. Further, Oxford Knee Score (OKS) and Visual Analogue Scale (VAS) (pain at rest and activity) were reported (90 days).
Results — 89 of 101 SD-TKA patients were discharged on DOS. The number of telephone calls (≤ 83) and outpatient visits (12) were similar in the 2 groups. The number of readmissions was ≤ 3 in both groups, and only 1 of the readmissions was related to TKA surgery. No differences were found at 90-day follow-up in terms of OKS (34 in both groups) or VAS (rest: SD-TKA = 7 and standard TKA = 8; activity: SD-TKA = 17 and standard TKA = 15).
Interpretation — SD-TKA is feasible in a selected group of patients, and safety and PROs are comparable to patients undergoing standard TKA.
Citation: Acta Orthopaedica 2022; 93: 509–518. DOI http://dx.doi.org/10.2340/17453674.2022.2807.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-01-19. Accepted: 2022-04-26. Published: 2022-06-16.
Correspondence: anne.mette.schmidt@rm.dk
MG designed the SIKS database and collected the data. AMS, MG, and STS analyzed the data and drafted the manuscript. All authors provided input on the design of the study, interpreted the results, and revised and approved the manuscript.
Helle Kjær Hvidtfeldt, RN, is thanked for organizing patient flow, Trine Astrup Bech Vestergaard, physiotherapist, is thanked for providing practical support, and statistician Asger Roer Pedersen is thanked for helpful advice.
Acta thanks Urban Berg and Tina Strømdal Wik for help with peer review of this study.
As a result of general quality improvements in the clinical pathway of arthroplasty surgery, fast-track procedures have emerged, resulting in reduced mean length of stay (LOS) in hospital (1-5). In Denmark, mean LOS is 1.5 days for patients undergoing primary total knee arthroplasty (TKA) surgery (6). Recently, discharge on the same day as TKA surgery (SD-TKA) has increasingly gained attention and acceptance (5,7).
Several systematic reviews including studies on different arthroplasty procedures have revealed that discharge on the day of surgery appears feasible, safe, and effective in selected patients (1-4,8). The reviews on TKA include both comparative (non-randomized) and non-comparative studies; the definition of discharge on the day of surgery (DOS) varies, and clinical pathway protocols differ (1-4,8). Most studies were conducted in the United States, and only a few in Europe (9-13). Given the low number of patients undergoing SD-TKA in previous European studies, further studies on SD-TKA are warranted, particularly in Scandinavian populations. Furthermore, although the importance of patientreported outcomes (PROs) is acknowledged when assessing knee function (5), only a few studies have reported PROs following SD-TKA (3,13).
This study evaluates the feasibility of SD-TKA, and compares safety and also PROs at 90-day follow-up between patients undergoing SD-TKA and patients undergoing standard TKA.
Patients and methods
This single-center cohort study, reported according to the STROBE Statement, compared a group of patients who underwent SD-TKA with a group of patients who underwent standard TKA. SD-TKA patients were scheduled to be discharged to their home on DOS, whereas standard TKA patients stayed at least 1 night in the hospital.
Patients were included from the Silkeborg Knee Replacement Study (SIKS) database. The SIKS database is a prospective cohort including 1,026 consecutive patients who underwent TKA at the Elective Surgery Center, Silkeborg Regional Hospital, Denmark (a public tax-financed hospital with free access for patients) between February 2018 and March 2020. From November 2018, the SIKS database also included SD-TKA patients; the first 18 patients were defined as pilot patients and treated in accordance with the clinical pathway protocol (Table 1, see Supplementary data). To imitate discharge to the home, pilot patients spent 1 night at the patient hotel accompanied by their own adult support person and without nightly nurse supervision. In the clinical setting, patients were scheduled to SD-TKA based on the following eligibility criteria: (i) primary unilateral TKA, (ii) accepting SD-TKA, (iii) ≥ 18 years, (iv) ASA score 1+2 , (v) availability of an adult support person at home during the first 24 hours after discharge, (vi) living within 1-hour drive from the hospital, and (vii) not categorized as a pain care patient (pain care patients fulfill the following criteria: (a) intake of > 80 mg opioids/24 hours, (b) current or previous abuse of opioids or alcohol, (c) opioid intolerance, (d) previous gastric banding or sleeve operation, (e) current use of medicinal cannabis, (f) complex history of pain, and/or (g) current methadone treatment). All patients who were offered SD-TKA were consecutively included in the study from the SIKS database. For the purpose of the study and to ensure that the standard TKA group was as comparable as possible to the SD-TKA group we used the following selection criteria for the standard TKA group: (i) primary unilateral TKA, (ii) ≥ 18 years, (iii) ASA score 1+2, (iv) cohabiting (a proxy for criteria v) in the SD-TKA group), and (v) not categorized as a pain care patient.
Patients from the standard TKA group either underwent surgery before SD-TKA was initiated or in the same period as SD-TKA was offered. No procedural changes in the clinical pathway protocol occurred during the inclusion period. This justified the inclusion of standard TKA patients from the period prior to when SD-TKA was offered. SD-TKA patients were matched 1:1 on sex and age (nearest-neighbor in the interval between ± 5 years) with standard TKA patients. Of note are 2 issues. First, 4 of the pilot patients were discharged on the DOS. 1 of these 4 pilot patients was excluded due to being categorized as a pain care patient; thus, 3 pilot patients were included in the analyses as they were considered to have the same safety risk as the rest of the SD-TKA group. Second, 8 patients had been included as SD-TKA patients although they had an ASA score = 3, which was a predefined exclusion criterion in the clinical setting. As we intended the study to reflect clinical practice, it was decided to match these 8 patients with 8 patients with ASA score = 3 from the standard TKA group and include them in the analyses.
The clinical pathway was delivered by a multidisciplinary team consisting of anesthesiologists, orthopedic surgeons, nurses, and physiotherapists. The main differences in the clinical pathway of the 2 patient groups were: (i) that patients from the SD-TKA group were transferred to the day care unit whereas patients from the standard TKA group were transferred to a specialized orthopedic ward, and (ii) physiotherapy was initiated on DOS for the SD-TKA group, and the day after surgery for the standard TKA group (Table 1, see Supplementary data).
Participant and surgical characteristics were collected at baseline. Variables related to feasibility were LOS, and reason(s) for not being discharged on DOS. These variables were retrieved from the electronic medical record, and were collected retrospectively. In terms of safety, data on unplanned contacts and complications (i.e., the reason(s) for the unplanned contact) were collected and categorized into (i) telephone calls, (ii) outpatient visits, and (iii) readmission (admission to hospital for more than 12 hours). Data on telephone calls and outpatient visits was collected retrospectively from the electronic medical record within 2 weeks from discharge. Data on readmission was obtained retrospectively from the Danish National Patient Registry (DNPR) within the first 90 days after surgery. PROs on function and pain were measured by the Oxford Knee Score (OKS), a 12-item questionnaire summarized to a total score between 0 and 48 (the higher the score, the better function and pain) (14). PROs were also collected on mean pain intensity (rest and activity) during the last 24 hours by visual analogue scale (VAS) ranging from “no pain” (0) to “worst pain” (100) (15). PROs were collected prospectively at baseline and 90 days after discharge. In addition, data on activity level measured by the University of California at Los Angeles (UCLA) activity level scale (16), and data on health-related quality of life (HRQoL) measured by the EuroQol 5-domain 5-level (EQ-5D-5L) and EuroQol VAS (EQ VAS) (17) were collected at baseline.
Statistics
Participant and surgical characteristics plus PROs were presented with mean (SD) if normally distributed and median (IQR) if non-normally distributed. Categorical variables were reported as numbers and proportions.
LOS for each group and the reason(s) for not being discharged on DOS for the SD-TKA group were presented descriptively. Due to the inclusion of the 3 pilot patients a sensitivity analysis was performed in terms of feasibility. A descriptive comparison was made between groups in terms of unplanned contacts and complications. Student’s t-test was used to compare continuous parametric variables (OKS), and the Wilcoxon rank sum test was used to present non-normally distributed variables (VAS). We calculated 95% confidence intervals (CI) for within- and between-group differences on OKS and VAS. STATA 16 (V.16 Stata, College Station, TX, USA) was used for data analysis.
Ethics, registration, data sharing, funding, and potential conflicts of interest
The SIKS database was approved by the Danish Data Protection Agency (1-16-02-935-17), and pre-registered at ClinicalTrials.gov (NCT03411083). Participants gave written informed consent. Central Denmark Region and the hospital management consented to transfer data from the electronic medical record to the SIKS database (1-45-70-70-20) after expiration of informed consent. The Danish Health Data Board provided data from the DNPR (00005469). Data on feasibility, telephone calls, outpatient visits, and PROs from the SIKS database is available from the authors upon reasonable request and with the needed permissions. Data on readmission from the Danish National Patient Registry was provided by the Danish Health Data Board. Restrictions apply to the availability, as the data was used under license for the current study, and so is not publicly available.
The study was funded by grants from Fogs Fond; it played no role in the completion of the study or the manuscript. STS is funded by a grant from Region Zealand (Exercise First) and 2 grants from the European Union’s Horizon 2020 research and innovation program (MOBILIZE (No 801790) and ESCAPE (No 945377). All authors declared they had no conflicts of interest.
Results
Following the study inclusion and exclusion criteria and the matching procedure, each group consisted of 101 patients (Figure and Table 2).
| Factor | SD-TKA (n = 101) | Standard TKA (n = 101) |
| Sex (woman) a | 48 | 48 |
| Age a, mean (SD) | 66 (7) | 66 (7) |
| range | 43–80 | 47–80 |
| ASA classification a | ||
| 1–2 | 93 | 8 |
| 3 | 93 | 8 |
| Educational level (years) b | ||
| Low (s 12) | 28 | 36 |
| Middle (> 12 and < 15) | 22 | 18 |
| High (a 15) | 48 | 45 |
| Employment situation b | ||
| Self-supporting/student | 28) | 28 |
| Social benefits | 9 | 6 |
| Age-related pension | 62 | 65 |
| Smoking status b | ||
| Never smoked/stopped smoking | 85 | 86 |
| Current smoker | 16 | 4 |
| Alcohol intake (units a week) b | ||
| ≤ 7/14 (women/men) | 96 | 83 |
| > 7/14 (women/men) | 5 | 7 |
| BMI, mean (SD) | 29 (5) | 29 (4) |
| Previous standard TKA in opposite knee | b 14 | 21 |
| Anesthesia | ||
| General | 5 | 4 |
| Spinal | 96 | 97 |
| Use of opioids b | ||
| Yes (seldom to several times a week) | 5 | 7 |
| Yes (once a day or more) | 9 | 9 |
| Patient-reported outcomes b | ||
| Function and pain (OKS c) | 24 (7) | 24 (6) |
| Pain intensity, rest (VAS d) | 29 (39) | 41 (40) |
| Pain intensity, activity (VAS d) | 63 (32) | 71 (31) |
| Activity level (UCLA e) | 6 (2) | 6 (2) |
| HRQoL (EQ-5D-5L f) | 0.66 (0.13) | 0.66 (0.11) |
| HRQoL (EQ VAS g) | 66 (20) | 65 (21) |
| a Matching variable b Due to missing values n does not correspond to 101 in the following variables: Educational level (SD-TKA n = 98; Standard TKA n = 99), Employment situation (SD-TKA n = 99; Standard TKA n = 99), Smoking status (SD-TKA n = 101; Standard TKA n = 90), Alcohol intake (SD-TKA n = 101; Standard TKA n = 90), Previous standard TKA in opposite knee (SD-TKA n = 97; Standard TKA n = 97), Use of opioids (SD-TKA n = 72; Standard TKA n = 73), Function and pain (OKS) (SD-TKA n = 98; Standard TKA n = 99), Pain intensity rest (VAS) (SD-TKA n = 87; Standard TKA n = 99), Pain intensity activity (VAS) (SD-TKA n = 90; Standard TKA n = 100), Activity level (UCLA activity-level scale) (SD-TKA n = 94; Standard TKA n = 98), HRQoL (EQ-5D-5L) (SD-TKA n = 99; Standard TKA n = 100), and HRQoL (EQ VAS) (SD-TKA n = 98; Standard TKA n = 96). c OKS – Oxford Knee Score (0–48), mean (SD). d VAS – Visual analogue scale (0 to 100), median (IQR). e UCLA – University of California at Los Angeles activity-level scale (0–10), mean (SD) f Health-related quality of life (EQ-5D-5L – EuroQol 5-domain 5-level) (–0.624 to 1), mean (SD). g Health-related quality of life (EQ VAS – Visual analogue scale) (0–100), mean (SD) |
||
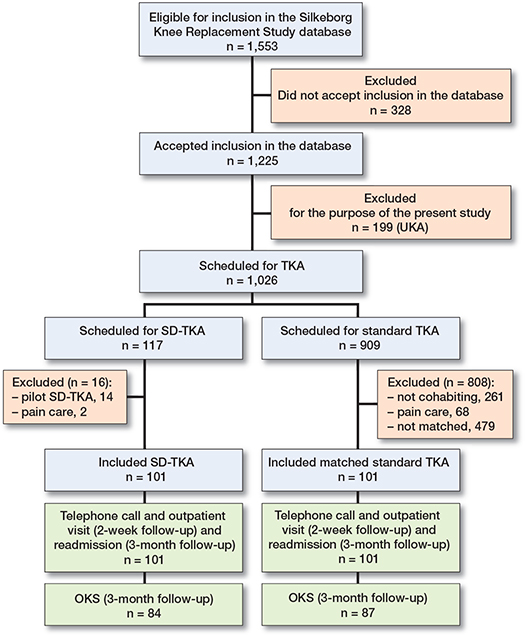
Participant flow. UKA: unicompartmental knee arthroplasty; TKA: total knee arthroplasty; SD-TKA: discharge on the same day as TKA surgery; Pain care: patients fulfilling the following criteria: (a) intake of > 80 mg opioids/24 hours, (b) current or previous abuse of opioids or alcohol, (c) opioid intolerance, (d) previous gastric banding or sleeve operation, (e) current use of medicinal cannabis, (f) complex history of pain, and/or (g) current methadone treatment; OKS: Oxford Knee Score.
In terms of feasibility, 89 of the 101 patients (88%) offered the SD-TKA procedure were discharged on DOS (Table 3).
| Discharge | SD-TKA (n = 101) | Standard TKA (n = 101) |
| Day of surgery | 89 | 0 |
| Day 1 after surgery | 11 a | 89 |
| Day 2 after surgery | 1 b | 10 |
| Day 3 or 4 after surgery | 0 | 2 |
| A sensitivity analysis of the SD-TKA group results without inclusion of the 3 pilot patients revealed no differences compared with the primary analysis (Day of surgery (86/98), Day 1 (11/98), Day 2 (1/98), and Day 3 or 4 (0/98). a Reasons for prolonged admission: patient-related (1), wound seepage/bleeding (4), dizziness and nausea (3), other (3). b Reason for prolonged admission: wound seepage/bleeding (1). |
||
By using data from the electronic medical record and the DNPR, we were able to obtain complete data on follow-up on unplanned contacts and complications (Figure). The number of telephone calls was similar in the 2 groups (Table 4). The main reasons for telephone calls were wound seepage/bleeding (SD-TKA), and pain management (standard TKA) (Table 5, see Supplementary data). The number of outpatient visits was identical in the 2 groups (Table 4). The main reasons for the outpatient visits were wound seepage/bleeding (SD-TKA) or related to swelling/compression stocking use (standard TKA) (Table 5, see Supplementary data). 3 patients were readmitted (admission to hospital for more than 12 hours) within the first 90 days after discharge. 2 of those patients were from the standard TKA group; 1 of them was readmitted once (tachycardia), and 1 was readmitted twice (cystitis and inpatient rehabilitation due to overweight). The 3rd patient was from the SD-TKA group and was readmitted for manipulation of the knee under anesthesia. The readmissions occurred between postoperative days 29 and 90, and are considered independent of TKA procedure (Table 4 and Table 5, see Supplementary data) .
| SD-TKA (n = 101) | Standard TKA (n = 101) | |
| Factor | ||
| Telephone calls a | ||
| Total number of patients | 47 | 50 |
| 1 telephone call | 25 | 30 |
| 2 telephone calls | 10 | 13 |
| 3 telephone calls | 10 | 5 |
| 4–6 telephone calls | 2 | 2 |
| Total number of telephone calls | 83 | 81 |
| Outpatient visits a | ||
| Total number of patients | 10 | 9 |
| 1 outpatient visit | 9 | 7 |
| 2 outpatient visits | 0 | 1 |
| 3 outpatient visits | 1 | 1 |
| Total number of outpatient visits | 12 | 12 |
| Readmission b | ||
| Total number of patients | 1 | 2 |
| 1 readmission | 1 | 1 |
| 2 readmissions | 0 | 1 |
| Total number of readmissions | 1 | 3 |
| a from discharge until the follow–up visit 2 weeks postoperatively. b admission to hospital for more than 12 hours within the first 90 days after surgery. |
||
The 90-day follow-up rate for PROs was 87%. Patients in the 2 groups were similar with respect to mean OKS at baseline, 90-day follow-up, and when estimating the mean within- and between-group differences. A difference in median VAS (rest and activity) between the 2 groups was identified at baseline, but there was no statistically significant difference between the 2 groups either at baseline or at 90-day follow-up (Table 6).
We performed 3 secondary analyses. First, in the SD-TKA group, patients not discharged on DOS (n = 12) did not differ from those discharged on DOS (n = 89). Second, when comparing those discharged on DOS (n = 89) and their matched standard TKA patients (n = 89), unplanned contacts and PROs were similar to those from the primary analysis (including n = 101 in both groups). Third, a comparison of non-responders and responders to the 90-day PROs showed statistically significant differences in sex, ASA score, and VAS; no statistically significant differences in patient age and OKS were found (Tables 7 and 8, see Supplementary data).
Discussion
This cohort study showed that the SD-TKA procedure was feasible, as 88% of the scheduled SD-TKA patients were discharged on DOS. Further, we found similar numbers of unplanned contacts and complications as well as similar PROs at 90-day follow-up when comparing the SD-TKA group with the standard TKA group, indicating that the SD-TKA procedure is safe in a selected group of patients.
A single study and a review including 6 studies found sameday (SD) discharge rates in TKA populations between 88% and 100% (3,18). With a feasibility rate of 88%, our study confirms previous findings from outside Scandinavia. These high SD discharge rates were not reported in previous Danish studies, showing SD discharge rates between 31% and 34% in unselected TKA patients eligible for outpatient surgery (9,11). Not complying with standard discharge criteria in relation to functioning was the main reason for patients not being discharged on DOS (11). In our study, the main reason for not being discharged on DOS was wound seepage/bleeding.
A readmission rate of 3% was found in a review on SD-TKA populations (3). Another review reported no difference in readmission rates between TKA groups (± discharged on DOS) (8). This is supported by 2 studies with 30-day follow-up (19,20). These results were confirmed in studies with 90-day (21,22) and 12-month follow-up (23). A recent Danish study found readmission (90-day follow-up), discharging department visits (3-week follow-up), and telephone calls to other departments and general practitioner (3-week follow-up) to be similar between TKA groups (± discharged on DOS) (12). In contrast to our study, the study found telephone calls to the discharging department to be statistically significant higher in patients discharged on DOS (12).
Overall, our study confirmed previous findings and did not identify differences in unplanned contacts between an SD-TKA group and a standard TKA group.
A review based on 2 comparative studies with 2-year follow-up (4) and 2 studies with 30-day follow-up (10,19) concluded that complication rates were similar in patients discharged on DOS and those not discharged on DOS. Apart from this, the general picture showed a higher rate of post discharge blood transfusion in the group discharged on DOS in the latter study (19). In contrast, a study (30-day follow-up) found that patients discharged on day 1 and 2 postoperatively had fewer minor and major complications compared with patients discharged on DOS (20). This was not demonstrated in a study (90-day follow-up) estimating that the rate of minor complications was lower for patients discharged on DOS compared with patients not discharged on DOS; the rate of major complications was similar between groups (22). The latter was confirmed by a study with a 1-year follow-up (23). Our study is the first Scandinavian study to assess complications solely in a TKA population. Our study supports the hypothesis that patients discharged on DOS do not experience more severe complications than patients discharged later.
There is a lack of studies reporting PROs when comparing patients undergoing knee arthroplasty discharged on DOS and patients not discharged on DOS (3). Only 1 Danish study has been identified assessing the OKS in these populations. In that study, the OKS was similar at 3- and 12-month followup between SD-TKA patients and patients scheduled for discharge on DOS, but who were actually not discharged on DOS (13). Our study confirms the findings from the aforementioned study (13), with no difference between SD-TKA and standard TKA at baseline, 90-day follow-up, or in improvement of function. We also compared the 2 groups in terms of VAS during rest and activity within the first 7 days after surgery. No statistically significant difference was found except for a higher score on day 2 in the group discharged on DOS (13). We did not measure VAS during the first week, but we found a difference (though not statistically significant) between the 2 groups in median VAS scores (rest and activity) before surgery. These differences might be coincidental or relate to actual differences between the SD-TKA group and the standard TKA group. The between-group differences in median VAS scores (rest and activity) had disappeared at 90-day follow-up; thus, the standard TKA group seemed to experience more pronounced improvements.
Our study is the first European study to include more than 100 SD-TKA patients matched with standard TKA patients. Moreover, it adds valuable knowledge to the existing evidence base regarding SD-TKA by including PROs. The study has several strengths. First, using the same eligibility criteria and matching we succeeded in making the 2 groups comparable on essential variables enabling a reasonable comparative analysis. Second, by using data from the electronic medical records and the DNPR in terms of feasibility, unplanned contacts and complications we reduced the risk of information and selection bias and ensured complete follow-up. Third, the response rate on PROs at 90-day follow-up was satisfying (87%) and although non-responders differed slightly from responders, risk of selection bias is considered low. Finally, by studying the direct effect of a non-controlled daily practice, we strengthened the external validity.
Some limitations warrant consideration. Despite our attempt to identify 2 comparable groups, the main limitation of our study is the non-randomized design. A randomized design is the best way to balance confounding variables, thus improving the validity of the results considerably. Clinical practice within SD-TKA surgery outpaced research as it was introduced faster than we had the opportunity to design and conduct a randomized trial. Still, we found it reasonable to assess SD-TKA surgery using our data, including safety, which is one of the main concerns within SD surgery. We chose a matched design as an alternative to making patients in 2 groups more similar and thus a useful and previously applied way of controlling for confounding in studies in this field (9,19-22). A second limitation is the inclusion criteria for SD-TKA patients, which reflect clinical practice but result in status as a selected group of patients. Thus, the patients accepting SD-TKA might have been advantaged in a biopsychosocial perspective, e.g., in relation to motivation, and this should be remembered when generalizing the results. By including 3 pilot patients and 8 patients with ASA = 3 in the analyzes, we modified the study inclusion criteria in comparison with the predefined clinical inclusion criteria. This was done to reflect clinical practice. Further, in terms of generalizability, providing the total number of patients fulfilling the criteria for SD-TKA surgery could have illustrated the number of patients offered and choosing this option, as well as characteristics of these patients. Unfortunately, this was not registered in the SIKS database. As a third limitation, one could argue that longer follow-up (12 months) could be an advantage but, as part of our aim was to assess feasibility and safety, we consider a 90-day follow-up to be sufficient based on a previous Danish study documenting readmission as occurring within the first 58 days after surgery (9). A final limitation is the relatively small sample size limiting the statistical power to determine differences between groups in terms of rare events such as readmission and related complications. Due to the COVID-19 pandemic during 2020–2022, there has been an urgent needed to reduce pressure on hospital wards (24). Consequently, the inclusion criteria for SD-TKA were extended in the clinical setting, and the rate of SD-TKA procedures performed was increased from approximately 15% (March 2019–February 2020) to approximately 35% (March 2020–February 2021). Thus, in the clinical setting the majority of patients are now offered SD-TKA.
In conclusion our data suggests that the SD-TKA procedure is feasible in a selected group of patients. Further, our data suggests similar rates of unplanned contacts and complications, and similar PROs at 90-day follow-up when comparing a SD-TKA group and a standard TKA group.
- Jaibaji M, Volpin A, Haddad FS, Konan S. Is outpatient arthroplasty safe? A systematic review. J Arthroplasty 2020; 35(7): 1941-9. doi: 10.1016/j.arth.2020.02.022.
- Hoffmann J D, Kusnezov N A, Dunn J C, Zarkadis N J, Goodman G P, Berger R A. The shift to same-day outpatient joint arthroplasty: a systematic review. J Arthroplasty 2018; 33(4): 1265-74. doi: 10.1016/j.arth.2017.11.027.
- Lovett-Carter D, Sayeed Z, Abaab L, Pallekonda V, Mihalko W, Saleh K J. Impact of outpatient total joint replacement on postoperative outcomes. Orthop Clin North Am 2018; 49(1): 35-44. doi: 10.1016/j.ocl.2017.08.006.
- Pollock M, Somerville L, Firth A, Lanting B. Outpatient total hip arthroplasty, total knee arthroplasty, and unicompartmental knee arthroplasty: a systematic review of the literature. JBJS Rev 2016; 4(12). doi: 10.2106/jbjs.Rvw.16.00002.
- Price A J, Alvand A, Troelsen A, Katz J N, Hooper G, Gray A, et al. Knee replacement. Lancet 2018; 392(10158): 1672-82. doi: 10.1016/s0140-6736(18)32344-4.
- Danish Knee Arthroplastry Register. Yearly report 2020; December 2020.
- Vehmeijer S B W, Husted H, Kehlet H. Outpatient total hip and knee arthroplasty. Acta Orthop 2018; 89(2): 141-4. doi: 10.1080/17453674.2017.1410958.
- Xu J, Cao J Y, Chaggar G S, Negus J J. Comparison of outpatient versus inpatient total hip and knee arthroplasty: a systematic review and meta-analysis of complications. J Orthop 2020; 17: 38-43. doi: 10.1016/j.jor.2019.08.022.
- Gromov K, Jørgensen C C, Petersen P B, Kjaersgaard-Andersen P, Revald P, Troelsen A, et al. Complications and readmissions following outpatient total hip and knee arthroplasty: a prospective 2-center study with matched controls. Acta Orthop 2019; 90(3): 281-5. doi: 10.1080/17453674.2019.1577049.
- Cassard X, Garnault V, Corin B, Claverie D, Murgier J. Outpatient total knee arthroplasty: readmission and complication rates on day 30 in 61 patients. Orthop Traumatol Surg Res 2018; 104(7): 967-70. doi: 10.1016/j.otsr.2018.07.014.
- Gromov K, Kjærsgaard-Andersen P, Revald P, Kehlet H, Husted H. Feasibility of outpatient total hip and knee arthroplasty in unselected patients. Acta Orthop 2017; 88(5): 516-21. doi: 10.1080/17453674.2017.1314158.
- Husted C E, Husted H, Nielsen C S, Mikkelsen M, Troelsen A, Gromov K. No increase in postoperative contacts with the healthcare system following outpatient total hip and knee arthroplasty. Acta Orthop 2021; 92(5): 557-61. doi: 10.1080/17453674.2021.1922966.
- Husted C E, Husted H, Ingelsrud L H, Nielsen C S, Troelsen A, Gromov K. Are functional outcomes and early pain affected by discharge on the day of surgery following total hip and knee arthroplasty? Acta Orthop 2021; 92(1): 62-6. doi: 10.1080/17453674.2020.1836322.
- Murray D W, Fitzpatrick R, Rogers K, Pandit H, Beard D J, Carr A J, et al. The use of the Oxford hip and knee scores. J Bone Joint Surg Br 2007; 89(8): 1010-4. doi: 10.1302/0301-620x.89b8.19424.
- Hawker G A, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken) 2011; 63(Suppl. 11): S240-52. doi: 10.1002/acr.20543.
- Zahiri C A, Schmalzried T P, Szuszczewicz E S, Amstutz H C. Assessing activity in joint replacement patients. J Arthroplasty. 1998; 13(8): 890-5. doi: 10.1016/s0883-5403(98)90195-4.
- The EuroQol Group. About EQ-5D-5L 2021. Available from: https://euroqol.org/eq-5d-instruments/eq-5d-5l-about/.
- Gogineni H C, Gray C F, Prieto H A, Deen J T, Boezaart A P, Parvataneni H K. Transition to outpatient total hip and knee arthroplasty: experience at an academic tertiary care center. Arthroplast Today 2019; 5(1): 100-5. doi: 10.1016/j.artd.2018.10.008.
- Bovonratwet P, Ondeck N T, Nelson S J, Cui J J, Webb M L, Grauer J N. Comparison of outpatient vs inpatient total knee arthroplasty: an ACS-NSQIP analysis. J Arthroplasty 2017; 32(6): 1773-8. doi: 10.1016/j.arth.2017.01.043.
- Nowak L L, Schemitsch E H. Same-day and delayed hospital discharge are associated with worse outcomes following total knee arthroplasty. Bone Joint J 2019; 101-b(7_Supple_C): 70-6. doi: 10.1302/0301620x.101b7.Bjj-2018-1402.R1.
- Darrith B, Frisch N B, Tetreault M W, Fice M P, Culvern C N, Della Valle C J. Inpatient versus outpatient arthroplasty: a single-surgeon, matched cohort analysis of 90-day complications. J Arthroplasty 2019; 34(2): 221-7. doi: 10.1016/j.arth.2018.10.015.
- Kimball C C, Nichols C I, Vose J G. Outpatient versus rapid recovery inpatient knee arthroplasty: comparison of matched cohorts. Orthopedics 2020; 43(1): 36-41. doi: 10.3928/01477447-20191122-01.
- Huang A, Ryu J J, Dervin G. Cost savings of outpatient versus standard inpatient total knee arthroplasty. Can J Surg 2017; 60(1): 57-62. doi: 10.1503/cjs.002516.
- Wainwright T W. Enhanced recovery after surgery (ERAS) for hip and knee replacement-why and how it should be implemented following the COVID-19 pandemic. Medicina (Kaunas) 2021; 57(1): 81. doi: 10.3390/medicina57010081.
Supplementary data
| SD-TKA (n = 101) | Standard TKA (n = 101) | ||
| Complications in relation to telephone calls a | |||
| Total number of patients | 47 | 50 | |
| Total number of telephone calls b | 83 | 81 | |
| Pain management | 17 | 38 | |
| Movement, activity and exercise | 7 | 5 | |
| PICO c | 4 | 2 | |
| Wound seepage/bleeding | 19 | 6 | |
| Side effects including nausea | 10 | 15 | |
| Additional questions about medication | 2 | 0 | |
| Swelling/compression stocking use | 18 | 25 | |
| Plaster/bandage | 12 | 9 | |
| Other | 6 | 12 | |
| Complications in relation to outpatient visits a | |||
| Total number of patients | 10 | 9 | |
| Total number of outpatient visits b | 12 | 12 | |
| Pain management | 0 | 3 | |
| Movement, activity and exercise | 0 | 0 | |
| PICO c | 6 | 2 | |
| Wound seepage/bleeding | 8 | 1 | |
| Side effects including nausea | 0 | 0 | |
| Additional questions about medication | 0 | 0 | |
| Swelling/compression stocking use | 1 | 6 | |
| Plaster/bandage | 4 | 1 | |
| Other | 2 | 3 | |
| Complications in relation to readmission d | |||
| Total numbers of patients | 1 | 2 | |
| Total number of readmissions | 1 | 3 | |
| Cystitis (29 days) | 0 | 1 | |
| Tachycardia (35 days) | 0 | 1 | |
| Inpatient rehabilitation due to overweight (71 days) | 1 | 0 | |
| Manipulation under anesthesia of the knee (90 days) | 1 | 0 | |
| a from discharge until the follow-up visit 2 weeks postoperatively. b 1 telephone call/outpatient visit can concern more than 1 complication. c PICO is a Single Use Negative Pressure Wound Therapy System. d admission to hospital for more than 12 hours within the first 90 days after surgery. |
|||
Secondary analyses
Secondary analysis 1: The 12 patients from the SD-TKA group not discharged on the day of surgery did not differ from the 89 patients from the SD-TKA group discharged on the day of surgery in relation to age (mean age 66 years) and gender (≈ 45% women).
Secondary analysis 2: When comparing the 89 patients from the SD-TKA group discharged on the day of surgery and the 89 matched patients from the standard group, the results on unplanned contacts (Table 7) and PROs (Table 8) were similar to the primary analysis.
Secondary analysis 3: 13 patients in each group did not complete the PROs at 90-day follow-up. A comparison of those non-responders to the 90-day PRO (n = 26) with responders (n = 176) showed that more women than men had completed the PROs, responders were more often classified as ASA 1+2, and those who had less pain (rest and activity) at baseline were more willing to complete the PROs. In terms of age and OKS at baseline, the 2 groups did not differ.
| Factor | SD-TKA | Standard TKA |
| Telephone calls a | ||
| Total number of patients | 42 | 43 |
| 1 telephone call | 21 | 26 |
| 2 telephone calls | 10 | 11 |
| 3 telephone calls | 9 | 4 |
| 4–6 telephone calls | 2 | 2 |
| Total number of telephone calls | 76 | 70 |
| Outpatient visits a | ||
| Total number of patients | 8 | 8 |
| 1 outpatient visit | 7 | 6 |
| 2 outpatient visits | 0 | 1 |
| 3 outpatient visits | 1 | 1 |
| Total number of outpatient visits | 10 | 11 |
| Readmission b | ||
| a from discharge until the follow-up visit 2 weeks postoperatively. b Data from the Danish National Patient Registry on readmission (admission to hospital for more than 12 hours) within the first 90 days after surgery is only available at group level. Thus, a sensitivity analysis on readmission for those actually discharged on the day of surgery (n = 89) cannot be performed. |
||
| Factor | SD-TKA | Standard TKA | Between-group mean difference (95%CI) | p-value | |
| Function and pain (OKS) (0–48) | |||||
| Baseline, mean (SD) | 24 (7) | 24 (6) | –0.5 (–2.4 to 1.4) | 0.6 | |
| 90–day, mean (SD) | 34 (7) | 34 (7) | –0.4 (–2.6 to 1.8) | 0.7 | |
| Within–group mean differences (95% CI) | 10 (7.9–11) | 10 (7.7–12) | –0.1 (–2.6 to 2.5) | 1.0 | |
| Pain intensity, rest (VAS) (0–100) | |||||
| Baseline, median (IQR) | 29 (39) | 44 (39) | 0.05 | ||
| 90–day, median (IQR) | 7 (14) | 8 (16) | 0.4 | ||
| Median of differences (IQR of differences) | –16 (41) | –28 (39) | 0.05 | ||
| Pain intensity, activity (VAS) (0–100) | |||||
| Baseline, median (IQR) | 65 (33) | 71 (33) | 0.1 | ||
| 90–day, median (IQR) | 17 (27) | 15 (23) | 0.5 | ||
| Median of differences (IQR of differences) | –37 (42) | -46 (42) | 0.1 | ||
| Due to missing values n does not correspond to 89 in the following variables: Function and pain (Oxford Knee Score): Baseline (SD-TKA n = 86; Standard TKA n = 88), 90-day (SD-TKA n = 75; Standard TKA n = 77), and Within-group mean differences (SD-TKA n = 73; Standard TKA n = 76). Pain intensity, rest (visual analogue scale): Baseline (SD-TKA n = 77; Standard TKA n = 87), 90-day (SD-TKA n = 77; Standard TKA n = 77), and Median of differences (SD-TKA n = 67; Standard TKA n = 76). Pain intensity, activity (visual analogue scale): Baseline (SD-TKA n = 80; Standard TKA n = 88), 90-day (SD-TKA n = 77; Standard TKA n = 75), and Median of differences (SD-TKA n = 70; Standard TKA n = 74). |
|||||