Large hospital variation in the risk of dislocation after primary total hip arthroplasty for primary osteoarthritis: 31,105 patients in 59 hospitals from the Danish Hip Arthroplasty Register
Lars L HERMANSEN 1-3, Bjarke VIBERG 1,4, and Soeren OVERGAARD 5,6
1 The Orthopedic Research Unit, Department of Orthopedic Surgery and Traumatology, Odense University Hospital, Odense; 2 Department of Orthopedics, Hospital of South West Jutland, Esbjerg; 3 Department of Clinical Research, University of Southern Denmark, Odense; 4 Department of Orthopedic Surgery and Traumatology, Lillebaelt Hospital, University Hospital of Southern Denmark, Kolding; 5 Department of Orthopedic Surgery and Traumatology, Bispebjerg Hospital; 6 Department of Clinical Research, University of Copenhagen, Denmark
Background and purpose — The risk of dislocation after primary total hip arthroplasty (THA) is affected by several factors, which increases the possibility of substantial differences among hospitals. We compared cumulative incidences of dislocation between regions and hospitals after primary THA surgery in osteoarthritis (OA) patients.
Patients and methods — From the Danish Hip Arthroplasty Register, we included 31,105 THAs performed from 2010 to 2014 with 2 years’ follow-up. Dislocations treated by closed reduction were identified in the Danish National Patient Register combined with patient file review. The results are presented as 2-year cumulative incidence on national, regional, and hospital level as proportions with 95% confidence intervals (CI) and as adjusted odds ratios (OR) analyzed by multiple logistic regression.
Results — 1,861 dislocations in 1,079 THAs were identified from 59 orthopedic departments. The 2-year cumulative incidence ranged from 2.2% to 4.3% between the 5 regions in Denmark. Hospital variation was 0–12%. For hospitals with a 5-year volume of more than 100 procedures, the incidence was 0.9–7.4%. Using the highest volume hospital as the reference, ORs for dislocation for the remaining hospitals were between 0.3 (CI 0.1–0.6) and 2.7 (1.9–4.0) after adjusting for age, sex, head size, and fixation method. Low-volume hospitals showed a higher dislocation risk than high-volume units with an adjusted OR of 1.2 (1.1–1.4).
Interpretation — We found substantial variation in the incidence of dislocation between hospitals within Denmark, which can be explained by a combination of patient-, component-, and surgery-related factors. There is a need for continuous monitoring of THA dislocation on regional and hospital levels to reduce overall and local dislocation risk for future patients.
Citation: Acta Orthopaedica 2022; 93: 503–508. DOI http://dx.doi.org/10.2340/17453674.2022.2754.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2021-01-18. Accepted: 2022-04-27. Published: 2022-05-31.
Correspondence: lars.lykke.hermansen@rsyd.dk
LH, BV and SO were responsible for the conception of this study; LH was responsible for data analysis; LH drafted the manuscript; BV and SO revised the manuscript critically for important intellectual content. All authors approved the final version to be published.
Acta thanks Bart G Pijls and Liza N van Steenbergen for help with peer review of this study.
Dislocation after primary total hip arthroplasty (THA) is a serious complication and is reported to vary from 0.2% to 10% (1-4). This notable variation is the result of the multifactorial causality of dislocation, including both patient-, component-, and surgery-related factors (5-7). In addition, surgeons’ skills and routine may impose a greater impact on the outcome than the use of particular approaches or implants, impliying an increased risk of regional differences among hospitals within a single country (3,4,8,9).
Continuous monitoring of local hip dislocation rates is challenging with the current standard registry settings. During the last 50 years, several national hip arthroplasty registries have been established to monitor the use of different prosthesis designs and their complications through revision rates (10-13). However, as most hip dislocations are treated by closed reduction only, they are not captured in these registries. Additionally, patients with dislocations are treated by a variety of orthopedic subspecialties with varying experience, resulting in inconsistent coding practice and making it challenging to identify the procedure in national patient registries (14).
A recently published, nationwide study revealed that 3.5% of Danish patients with osteoarthritis experienced at least 1 hip dislocation within 2 years after THA surgery, but the study did not focus on regional or hospital variations (7). To ensure high treatment quality, it is important to monitor complications to learn from the institutions with the best outcomes. Before efforts are made regarding a national monitoring initiative, we compared cumulative incidences of dislocation between hospitals and regions within Denmark after primary THA surgery in patients with osteoarthritis and assessed the association with number of procedures per hospital. This will be important for identifying hospitals with high dislocation rates with the focus on quality development in the future.
Patients and methods
Study design
This is a population-based cohort study with prospectively collected data from the Danish Hip Arthroplasty Register (DHR). We have reported according to RECORD guidelines.
Participants
We included patients with the diagnosis “primary/idiopathic hip osteoarthritis (OA)” that was reported to the DHR to have a primary THA at either a public or private hospital in Denmark in the 5-year period from January 1, 2010 to December 31, 2014 (10,15). We followed each patient for 2 years, except in the event of hip revision, death, or migration, in which case follow-up was terminated.
Patients with diagnoses other than primary OA were excluded, as were patients younger than 40 years due to the rare presence of primary OA to achieve a more homogeneous population. In the case of bilateral THA, the second THA was excluded to avoid dependency issues among observations (16).
Variables and data sources
We extracted data from 3 separate sources. Due to the unique 10-digit social security numbers for all Danish citizens, crossmatching between registers was possible (17).
First, the patient cohort and surgical characteristics regarding the primary procedure as well as any potential hip revisions were extracted from the DHR. Registration of THAs in this national hip arthroplasty register is compulsory, and it has a completeness of 98% for primary operations and 93–95% for revisions (10,15). Only dislocations that led to revision surgery are registered herein but not closed reductions.
Therefore, to capture every patient with a dislocation we combined data from the Danish National Patient Register (DNPR) and the local patient files stored electronically at each treating hospital. The DNPR is an administrative database that contains information on every hospital contact in Denmark (both public and private hospitals), including admission and discharge time and date, diagnosis, and operation codes, with a completeness of 99.7% (18). The DNPR dataset included both orthopedic and non-orthopedic hospital admissions, as well as emergency room contacts. We excluded contacts regarding the contralateral hip, scheduled outpatient contacts, planned revision surgery, and contacts with private hospitals as there is no tradition of admission of patients with acute conditions in these locations in Denmark. The definition of public/private and independent hospitals are based on the Danish 7-digit hospital-department classification system (SHAK) managed by the Danish Health Data Authority.
To verify the correctness of the dislocation diagnosis in the remaining hospital contacts, we divided these contacts into 2 groups. “Genuine dislocation” contacts were defined as having both the correct diagnostic ICD-10 code for THA dislocation (DT84.0A) and procedure NSCP code for prosthesis reduction (KNFH20), and the rest as “possible dislocations.” We manually reviewed all patient files containing the possible dislocations, as well as the “genuine dislocation” contacts with either inconsistency of laterality in the dataset or more than 1 operation per admission (7). In the case of insufficient information in the patient files, radiology databases were used to confirm dislocations.
Statistics
The cumulative incidence of dislocation during the observation period is presented as proportions with 95% confidence intervals (CI). We evaluated statistically significant differences for hospitals with more than 100 THA procedures during the 5-year inclusion period using a multiple logistic regression analysis adjusting for age, sex, head size, and fixation method. The hospital (no. 33) with the highest volume was chosen as reference hospital, as it represented the national incidence. A corresponding analysis was performed to compare the outcome of high-volume (defined as > 1,000 procedures during the 5-year inclusion period) versus low-volume hospitals (< 1,000 procedures). We performed the statistical analysis with STATA software version 17.0 (StataCorp, College Station, TX, USA).
Ethics, data-sharing, funding, and potential conflicts of interest
The Danish Patient Safety Authority (3-3013-2128/1), the Danish Data Protection Agency (2008-58-0035) and head of local departments approved the storage and review of patient medical records. The names of the 5 main regions in Denmark as well as the included hospitals are anonymized throughout the paper.
Several donations were kindly provided, and they all made this study feasible. They are listed randomly: Clara Hansens Memorial Fund and Appropriation Merchant Sven Hansen & Wife Ina Hansens Foundation, the Danish Rheumatism Association, the A.P. Møller Foundation for the Advancement of Medical Science, the Orthopaedic Fund of West Jutland, Doctor of Bramming, Grethe Marie Justesens Fund, the University of Southern Denmark, and Region of Southern Denmark. There are no conflicts of interest.
Results
Population
We extracted 36,693 registered THA procedures due to primary OA in 32,904 patients from the DHR between January 1, 2010 and December 31, 2014. The final study cohort consisted of 31,105 THAs after exclusions (Figure 1 and Table 1). These patients accounted for 16,108 healthcare contacts in the DNPR during the subsequent 2 postoperative years. The majority were discarded, leaving 1,143 genuine dislocations and 4,726 possible dislocations at 37 hospitals. The majority of patients completed the intended follow-up period, while 3.6% underwent hip revision for any reason and 2.7% died during the 2 years.
| Complete study population (n = 31,105) | THAs with dislocation(s) (n = 1,079) | THAs without dislocation (n = 30,026) | |
| Age group, years | |||
| < 65 | 8,928 | 216 (20) | 8,712 (29) |
| 65-75 | 12,668 | 443 (41) | 12,225 (41) |
| > 75 | 9,509 | 420 (39) | 9,089 (30) |
| Female sex | 17,400 | 650 (60) | 16,750 (56) |
| Head size, mm | |||
| ≤ 28 | 1,468 | 52 (4.8) | 1,416 (4.7) |
| 32 | 8,563 | 352 (33) | 8,211 (27) |
| 36 | 18,746 | 615 (57) | 18,131 (60) |
| ≥ 40 | 1,603 | 56 (5.2) | 1,547 (5.2) |
| Dual-mobility cup | 725 | 4 (0.4) | 721 (2.4) |
| Fixation method | |||
| Cemented | 3,930 | 133 (12) | 3,797 (13) |
| Uncemented | 22,592 | 782 (73) | 21,810 (73) |
| Hybrid | 4,583 | 164 (15) | 4,419 (15) |
| Surgical approach | |||
| Posterior | 29,879 | 1,067 (99) | 28,812 (96) |
| Lateral | 1,226 | 12 (1.1) | 1,214 (4.0) |
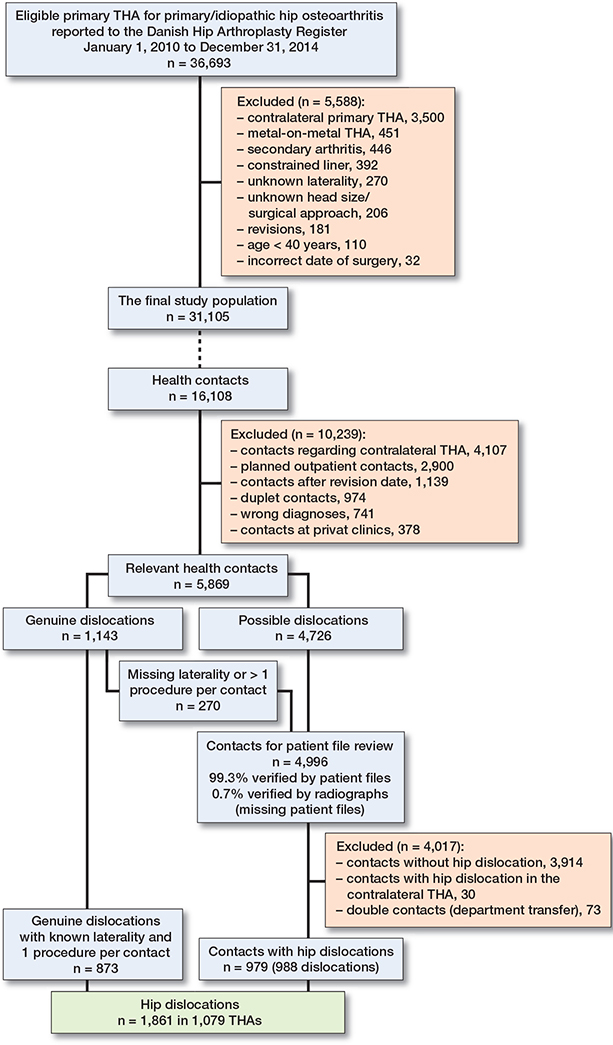
Figure 1. Flowchart overview of the process starting with identification of the final study population based on DHR data (part A). Subsequently, the process continues with finding relevant hospital contacts in the DNPR for these patients and, combined with patient file review, the “true” incidence of dislocations is identified (part B). The dotted line indicates that 16,108 hospital contacts were found in the DNPR for the 31,105 included THAs.
Cumulative incidence of dislocation
The nationwide cumulative incidence of dislocation location was 3.5% (CI 3.3–3.7) (7). The incidence varied from 2.2% to 4.3% between the 5 public regions and private hospitals (Table 2). We identified 59 independent orthopedic hospitals (both public and private) that performed between 1 and 2,558 THAs with 2-year dislocation incidences ranging from 0% to 12% (Figure 2). Revisions due to dislocation occurred in 0-3.8% of the patients, with proportions as high as 42% of a single unit’s total number of patients with dislocation (Figure 2). If excluding the smallest units (5-year volume < 100 procedures) and thereby minimizing the degree of coincidences, the 2-year dislocation incidence range narrowed to 0.9–7.4%. The regression analysis revealed 6 hospitals with statistically significant fewer dislocations and 11 hospitals with more dislocations than the reference (data not shown). After adjusting for age, sex, head size, and fixation method the numbers were 4 and 10 hospitals, respectively, with ORs between 0.3 (0.1–0.6) and 2.7 (1.9–4.0) (Figure 3). The analysis of high- versus low-volume hospitals showed a statistically significant higher dislocation risk at low-volume units with an adjusted OR of 1.2 (1.1–1,4). Dislocation incidence versus hospital volume also shows that in hospitals with more than 1,000 procedures during the 5-year period using the posterior approach, there was a lower risk the higher the volume (Figure 4).
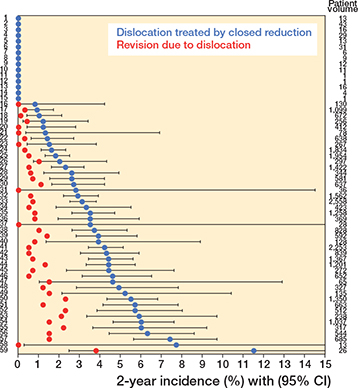
Figure 2. Between-hospital variation of the 2-year dislocation incidence (95% CI) with increasing values (blue dots). The proportion of patients having a revision due to dislocation is shown without CI (red dots).
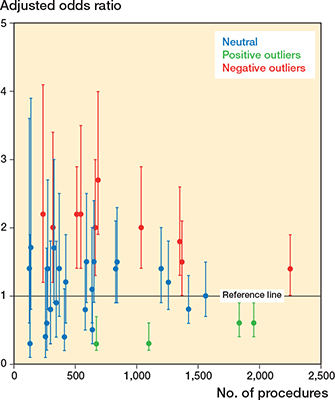
Figure 3. Hospital variation adjusted for age, sex, head size, and fixation method with hospital 33 as reference. Only departments with more than 100 procedures during the 5-year period were included in this analysis.
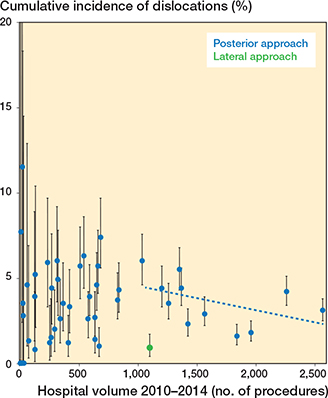
Figure 4. Impact of hospital volume on dislocation incidence with 95% CIs. Blue dots = units using posterior approach. Green dot = 1 unit using the lateral approach.
Discussion
The cumulative incidences of dislocation after primary THA between hospitals revealed large differences, with 2-year outcomes varying from 0% to 12%. Using the highest volume hospital as a reference measure close to the overall national result, we found that 14 hospitals deviated statistically significantly during our inclusion period. The validity of our findings is strengthened by the large study population, our country’s high-quality registries, and in particular the nationwide review of patient files securing the inclusion of every hip dislocation.
In hospitals with a 5-year volume between 1 and 1,000 procedures, we found the cumulative incidence range from 0% to 12% with no correlation to the hospital volume. First, this indicates that the relative rareness of dislocation naturally leads to large deviations due to coincidences, and second that many other factors impact the risk. In higher volume hospitals (> 1,000 procedures, posterior approach), the risk stabilized in a more predictable range from 1.6% to 6.0% and showed a lower risk at higher volume hospitals, suggestive the influence of surgical experience (Figure 4). The benefit of high-volume surgeons on dislocation risk has been confirmed in previous studies (3,9). Although we found a higher risk of dislocation after surgery in low-volume hospitals, we cannot present data on surgeon level due to lack of this information in the register. Therefore, our finding remains an association as many other factors may be of influence. High-volume centers may have many surgeons affiliated, but attract healthier patients, whereas low-volume, academic centers may have few surgeons performing the more complicated primary cases. The level of early revisions due to dislocation might add to the evaluation of surgical quality, as the patients with dislocation and obvious component malposition are presumed to be revised more readily than the opposite case. We observed a large variation in revision rates among hospitals, which has to be interpreted with caution as we do not possess information on patient level, and many factors interact when deciding to revise.
To explain the observed between-hospital variation, it is important to consider all factors that may influence the risk of dislocation, whether these are related to the patient, the implants, the surgeon, or the organization. Obviously, surgeons possess limited options in terms of modifying most patient-related factors that may affect the dislocation risk. If the indication for surgery is maintained, this leaves the surgeon with the possibility of differentiating between surgical approaches and technique, as well as implant type and fixation method. Regarding head size, the last 10 to 15 years have demonstrated the use of larger sizes. From 2000 to 2003, 90% of patients received a 28 mm head, whereas 85% received a 32 or 36 mm head from 2012 to 2017 (15). This change was facilitated by fewer dislocations with larger heads (7,19,20). In Denmark, approximately 96% of primary THAs are performed through a posterior approach and only 4% by a lateral approach (a single institution), with the latter being superior in terms of dislocation (7,15). Regarding implants, in terms of brand/manufacturer, the availability is determined on a regional level and therefore varies between the 5 regions with only few local options for the surgeon. We observed considerable variation between the regions, with Regions A and E performing inferiorly compared with Regions B, C and D (public regions), whereas the private sector demonstrated the best outcome with 2.2% dislocations. The lower dislocation incidence among private hospitals versus the public regional hospitals may be explained partly by patient selection, as they do not treat patients with high comorbidity (21). Additionally, the public hospitals are also responsible for training future hip surgeons, which entails a learning curve that may influence the dislocation risk.
The study has several limitations. An important limitation is the missing knowledge regarding patient comorbidities, in particular information on neuromuscular disorders like Parkinson’s disease and specific conditions such as alcoholism and psychosis that cause cognitive dysfunction, which may increase the dislocation risk (22,23). Widely used comorbidity measurements like the Charlson Comorbidity Index and the ASA score do not include these conditions. Higher ASA score has been associated with increased dislocation risk in several studies, but this score was not registered nationally during our inclusion period (7,24). The availability of detailed patient characteristics would have enabled us to calculate case-mixadjusted dislocation incidences and to identify “true” hospital differences rather than possible chance variation (25). We sought to eliminate the influence of other patient-related factors by adjusting for age and sex, including only patients diagnosed with primary OA and excluding patients with acute fractures or previous hip surgery.
In conclusion, we have demonstrated large differences in the dislocation risk between the hospitals performing primary THAs. The number of procedures explains some of the variation, but difference in case mix, surgical technique and positioning of the components, attention from the surgical team, and administrative factors may also play a role.
In perspective, we believe there is a need for national and local monitoring of this complication to identify hospitals with inferior outcome. Currently, arthroplasty registers are excellent for identifying components and articulations associated with increased revision rates, and the inclusion of dislocations treated by closed reduction would be the next obvious step, which we plan to implement.
- Mäkelä K T, Matilainen M, Pulkkinen P, Fenstad A M, Havelin L I, Engesaeter L, et al. Countrywise results of total hip replacement: an analysis of 438,733 hips based on the Nordic Arthroplasty Register Association database. Acta Orthop 2014; 85(2): 107-16.
- Gromov K, Troelsen A, Otte K S, Orsnes T, Ladelund S, Husted H. Removal of restrictions following primary THA with posterolateral approach does not increase the risk of early dislocation. Acta Orthop 2015; 86(4): 463-8.
- Malkani A L, Ong K L, Lau E, Kurtz S M, Justice B J, Manley M T. Early- and late-term dislocation risk after primary hip arthroplasty in the Medicare population. J Arthroplasty 2010; 25(6 Suppl.): 21-5.
- Kwon M S, Kuskowski M, Mulhall K J, Macaulay W, Brown T E, Saleh K J. Does surgical approach affect total hip arthroplasty dislocation rates? Clin Orthop Relat Res 2006; 447: 34-8.
- Brooks P J. Dislocation following total hip replacement: causes and cures. Bone Joint J 2013; 95-b(11 Suppl. A): 67-9.
- Crozier-Shaw G, Magill P. WHAT causes dislocation of a total hip arthroplasty: a simple mnemonic for the orthopaedic resident. Int Orthop 2015; 39(3): 605-6.
- Hermansen L L, Viberg B, Hansen L, Overgaard S. “True” cumulative incidence of and risk factors for hip dislocation within 2 years after primary total hip arthroplasty due to osteoarthritis: a nationwide population-based study from the Danish Hip Arthroplasty Register. J Bone Joint Surg Am 2021; 103(4): 295-302.
- Cossec C L, Colas S, Zureik M. Relative impact of hospital and surgeon procedure volumes on primary total hip arthroplasty revision: a nationwide cohort study in France. Arthroplast Today 2017; 3(3): 176-82.
- Katz J N, Losina E, Barrett J, Phillips C B, Mahomed N N, Lew R A, et al. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States Medicare population. J Bone Joint Surg Am 2001; 83(11): 1622-9.
- Gundtoft P H, Varnum C, Pedersen A B, Overgaard S. The Danish Hip Arthroplasty Register. Clin Epidemiol 2016; 8: 509-14.
- Malchau H, Herberts P, Eisler T, Garellick G, Söderman P. The Swedish Total Hip Replacement Register. J Bone Joint Surg Am 2002; 84-A(Suppl. 2): 2-20.
- Havelin L I. The Norwegian Joint Registry. Bull Hosp Jt Dis 1999; 58(3): 139-47.
- van Steenbergen L N, Denissen G A, Spooren A, van Rooden S M, van Oosterhout F J, Morrenhof J W, et al. More than 95% completeness of reported procedures in the population-based Dutch Arthroplasty Register. Acta Orthop 2015; 86(4): 498-505.
- Hermansen L L, Viberg B, Overgaard S. Development of a diagnostic algorithm identifying cases of dislocation after primary total hip arthroplasty-based on 31,762 patients from the Danish Hip Arthroplasty Register. Acta Orthop 2021; 92(2): 137-42.
- DHR. Danish Hip Arthroplasty Register—Annual Report. Available from: http://danskhoftealloplastikregisterdk/wp-content/uploads/2019/09/ DHR-årsrapport-2019_til-offentliggørelsepdf 2019.
- Ranstam J, Robertsson O. Statistical analysis of arthroplasty register data. Acta Orthop 2010; 81(1): 10-14.
- Pedersen C B. The Danish Civil Registration System. Scand J Public Health 2011; 39(7 Suppl.): 22-5.
- Schmidt M, Schmidt S A, Sandegaard J L, Ehrenstein V, Pedersen L, Sorensen H T. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 2015; 7: 449-90.
- Tsikandylakis G, Mohaddes M, Cnudde P, Eskelinen A, Kärrholm J, Rolfson O. Head size in primary total hip arthroplasty. EFORT Open Rev 2018; 3(5): 225-31.
- Howie D W, Holubowycz O T, Middleton R, Large Articulation Study G. Large femoral heads decrease the incidence of dislocation after total hip arthroplasty: a randomized controlled trial. J Bone Joint Surg Am 2012; 94(12): 1095-102.
- Tynkkynen L K, Vrangbaek K. Comparing public and private providers: a scoping review of hospital services in Europe. BMC Health Serv Res 2018; 18(1): 141.
- Espehaug B, Havelin L I, Engesaeter L B, Langeland N, Vollset S E. Patient-related risk factors for early revision of total hip replacements: a population register-based case-control study of 674 revised hips. Acta Orthop Scand 1997; 68(3): 207-15.
- Paterno S A, Lachiewicz P F, Kelley S S. The influence of patientrelated factors and the position of the acetabular component on the rate of dislocation after total hip replacement. J Bone Joint Surg Am 1997; 79(8): 1202-10.
- Khatod M, Barber T, Paxton E, Namba R, Fithian D. An analysis of the risk of hip dislocation with a contemporary total joint registry. Clin Orthop Relat Res 2006; 447: 19-23.
- van Schie P, van Steenbergen L N, van Bodegom-Vos L, Nelissen R, Marang-van de Mheen P J. Between-hospital variation in revision rates after total hip and knee arthroplasty in the Netherlands: directing quality-improvement initiatives. J Bone Joint Surg Am 2020; 102(4): 315-24.