How long does an elbow replacement last? A systematic review and meta-analysis of case-series and national registry reports with more than 10 years of follow-up
Jonathan P EVANS 1,2, Jonathan T EVANS 3, Hasan R MOHAMMAD 4,5, Adrian SAYERS 3, Ashley W BLOM 3,6, Michael R WHITEHOUSE 3,6, and Jonathan L REES 4,5
1 Health & Policy Research Group, University of Exeter, Exeter; 2 National Institute for Health Research Applied Research Collaboration South West Peninsula, University of Exeter, Exeter; 3 Musculoskeletal Research Unit, Translational Health Sciences, Bristol Medical School, 1st Floor Learning & Research Building, Southmead Hospital, Bristol; 4 Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences, University of Oxford, Botnar Research Centre, Oxford; 5 National Institute for Health Research Oxford Biomedical Research Centre, Oxford; 6 National Institute for Health Research Bristol Biomedical Research Centre, University Hospitals Bristol NHS Foundation Trust and University of Bristol, Bristol, UK
Background and purpose — This study aims to determine, for the first time, generalizable data on the longevity and long-term function of elbow replacements.
Methods — In this systematic review and meta-analysis, we searched MEDLINE and Embase for articles reporting 10-year or greater survival of total elbow replacements (TERs) and distal humeral hemiarthroplasty. Implant survival and patient reported outcome measures (PROMs) data were extracted. National joint replacement registries were also analyzed. We weighted each series and calculated a pooled survival estimate at 10, 15, and 20 years. For PROMs we pooled the standardized mean difference (SMD) at 10 years.
Findings — Despite its widespread use, we identified only 9 series reporting all-cause survival of 628 linked TERs and 610 unlinked TERs and no series for distal humeral hemiarthroplasty. The studied population was treated for rheumatoid arthritis in over 90% of cases. The estimated 10-year survival for linked TERs was 92% (95% CI 90–95) and unlinked TERs 84% (CI 81–88). 2 independent registries contributed 32 linked TERs and 530 unlinked TERs. The pooled registry 10-year survival for unlinked TERs was 86% (CI 83–89). Pooled 10-year PROMs from 164 TERs (33 linked and 131 unlinked), revealed a substantial improvement from baseline scores (SMD 2.7 [CI 1.6–3.8]).
Interpretation — Over 80% of all elbow replacements and over 90% of linked elbow replacements can last more than 10 years with sustained patient-reported benefits. This information is long overdue and will be particularly useful to patients as well as healthcare providers.
Citation: Acta Orthopaedica 2022; 93: 495–502. DOI http://dx.doi.org/10.2340/17453674.2022.2753.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-02-01. Accepted: 2022-03-22. Published: 2022-05-31.
Correspondence: j.p.evans2@exeter.ac.uk
JPE and JTE were responsible for study concept, design, screening, data extraction, data analysis, and writing of this manuscript. HM completed the primary screening of abstracts and review of the manuscript. JR, AB, MRW, and AS were responsible for study concept, design, and writing of the manuscript.
This report is independent research supported by the National Institute for Health Research Applied Research Collaboration South West Peninsula, National Institute for Health Research Biomedical Research Centre at the University Hospitals Bristol National Health Service (NHS) Foundation Trust and the University of Bristol, and National Institute for Health Research Oxford Biomedical Research Centre. The views expressed in this publication are those of the authors and not necessarily those of the National Institute for Health Research or the Department of Health and Social Care.
Acta thanks Ilse Degreef and Johan Scheer for help with peer review of this study.
The indications for elbow replacement have expanded over the last 20 years. Initially employed almost exclusively for inflammatory arthritis, surgeons are now increasingly utilizing this technology to treat osteoarthritis and unreconstructable fractures (1).
Elbow replacement is a procedure performed relatively infrequently in comparison with hip and knee arthroplasty. This pattern of low-volume practice means that data from single institutions and randomized trials is scarce, and even individual countries registries shed limited light on the long-term outcome of elbow replacement. A global synthesis of outcome data from multiple sources offers the only currently practical solution to provide better evidence on efficacy and longevity of elbow replacement. Such information is long overdue and is needed by patients and clinicians to aid joint decision-making. It will also assist commissioners and healthcare providers in understanding the utility and likely revision burden associated with this procedure.
Ideally, clinicians and surgeons should be able to provide patients with contemporary outcome data for the specific implant used. While manufacturers do facilitate the collection of implant-level data in order to gain relevant benchmark accreditation (2), detailed and reliable data is not yet available for elbow replacements. Until such granular brand-level information is available, clinicians and patients need, at minimum, accurate information on the different classes of available implants. Hip and knee replacement have shown that although there is variation between brands, classes of implants behave in broadly similar fashion (3,4).
In this study we aimed to answer the simple, patient-focused question: “How long does an elbow replacement last?” We pooled the estimates of implant survival, categorized by implant class, 10 years after surgery as a pragmatic compromise between the volume of data available and what patients would consider “long-term.” As the decision to revise a poorly performing elbow replacement is multifactorial, with both patient and surgeon factors influencing the choice, we also pooled PROMs estimated to answer the question: “Will my elbow be better 10 years after surgery?”
Methods
Search strategy and selection criteria
We conducted a systematic review and meta-analysis of elbow replacements’ survival and patient-focused outcomes from case-series and national joint registries following a pre-registered protocol (PROSPERO CRD 42020192903). Reporting complies with PRISMA guidelines (5).
The search strategy used MeSH and keyword terms relating to elbow replacements and survival (Table 1, see Supplementary data). Databases searched were MEDLINE and Embase, accessed through OVID Silver Platter (Wolters Kluwer, Alphen aan den Rijn, The Netherlands). Database searches were conducted from their commencement to June 8, 2021. The search strategy used elbow- and implant-specific modifications to previously published strategies exploring the survival of hip, knee, and shoulder replacements (6-8). We searched full-text articles forwards and backwards.
| Factor | Individual case series articles | Registry data | ||
| TER | TER | TER | TER | |
| linked | unlinked | linked | unlinked | |
| Study-level characteristics | ||||
| Location | USA (x3) | Japan | Australia | Norway |
| UK | UK | |||
| France | ||||
| Switzerland | ||||
| Finland | ||||
| Number of unique implant series included | 6 | 3 | 1 | 4 |
| Year of publication | 1998–2020 | 2010–2014 | 2018-2020 | 2018 |
| Participant-level characteristics | ||||
| Mean age | 64 a | 57 a | 71 b | 63 |
| Female sex (%) | 77 a | 92 a | 74 b | 83 |
| Reumatoid arthritis (%) | 89 | 96 | 100 | NA |
| Arthroplasties at start | 628 | 610 | 32 | 530 |
| Lost to follow-up | 15 (2.4%) | 0 | ||
| a Weighted on number of arthroplasties in the series. | ||||
| b Estimates from whole-group data.NA = Not available | ||||
Studies were included if they encompassed patients who had undergone an elbow replacement (distal humeral hemiarthroplasty or total elbow replacement). Radial head replacements were included only when in conjunction with total elbow replacement. The indication for surgery had to be predominantly inflammatory arthritis, osteoarthritis, or trauma (acute or chronic manifestations). For inclusion, the case-series had to report the survival of a specific brand of implant with a mean or median follow-up of greater than 10 years. With published registry reports, implant-level data of at least 10 years’ follow-up was included. It is widely accepted that survival of hip arthroplasties varies by the brand of implant (3). Although this has not specifically been assessed in elbow replacements, we utilized the technique of treating each brand as its own series (7). This method allows us to treat each series as an individual study and weight the meta-analysis of survival results according to the standard error of each series. Aggregate data from multiple implant brands would not allow this granularity and thus hide the potential variability in performance between implant brands. A cut-off of minimum mean or median follow-up of 10 years was chosen as “long-term” survival and allowed inclusion of sufficient studies to make analyses robust, and represents a time period that is relatable to patients and clinicians.
Studies were excluded if they reported the outcome of revision surgery, which is more complex and carries different survivorship, and if they performed isolated radial head replacement. Conference abstracts were excluded due to the limited data available from these reports. Systematic reviews were assessed for their citations but their pooled data was not included, to avoid duplication of individual patient data.
We assessed the reports from all available national joint registers that collect and publish the individual implant-specific survivorship for elbow replacements with at least 10 years of follow-up. Reports were identified through a systematic search of the published literature or accessed through their websites.
Article screening and data extraction
Screening was undertaken in a stepwise manner using the web application Rayyan (9). JTE and HM screened journal article titles and abstracts with arbitration of conflict undertaken by JPE. Full-text review and data extraction were undertaken by JPE and JTE. Data extracted were: publication date, baseline population demographics, number of patients (n), surgical indication proportion (% OA and/or % inflammatory arthritis and/or % trauma), follow-up duration (if > 10 years), implant name and construct type (hemiarthroplasty, TEA [linked or unlinked]), loss to follow-up, survival estimates (including 95% confidence intervals), and all available PROM (e.g. Visual Analogue Scales (VAS), Disabilities of the Arm, Shoulder and Hand (DASH), Oxford Elbow Score (OES) etc.) data (outcome measures used baseline mean score [SD], follow-up mean score [SD]). Data was not extracted from figures (e.g., Kaplan–Meier plots) to avoid potential transcription inaccuracy.
Statistics
For the assessment of the published case-series our primary exposure was the elbow replacement implant and our primary outcome was all-cause revision, of any part of this construct, as guided by our patient group (10). Statistical analysis was performed with Stata 16 (Stata Statistical Software: Release 16; StataCorp LLC, College Station, TX, USA). Survival estimates, assuming that survivorship approximated revision risk, were pooled by meta-analysis. Each series was weighted according to its standard error (calculated from published confidence intervals). The effect size (standardized mean difference [SMD]) of the primary PROMs reported in each study was pooled with meta-analysis with weighting according to sample size and analyzed using a random effects model as a more conservative estimate of treatment effect. Effect size was considered small if it was less than ≥ 0.2, moderate if ≥ 0.5 and large if ≥ 0.8 (11).
Quality assessment
Study quality was assessed using the non-summative 4-point system (consecutive cases, multi-center, under 20% loss to follow-up, and use of multivariable analysis) developed by Wylde et al. (12).
Funding and potential conflicts of interest
This study was supported by the NIHR Applied Research Collaboration South West Peninsula, NIHR Biomedical Research Centre at the University Hospitals Bristol NHS Foundation Trust and University of Bristol, and NIHR Oxford Biomedical Research Centre. JPE was supported by an NIHR Clinical Lectureship.
The authors declare no competing interests.
Findings
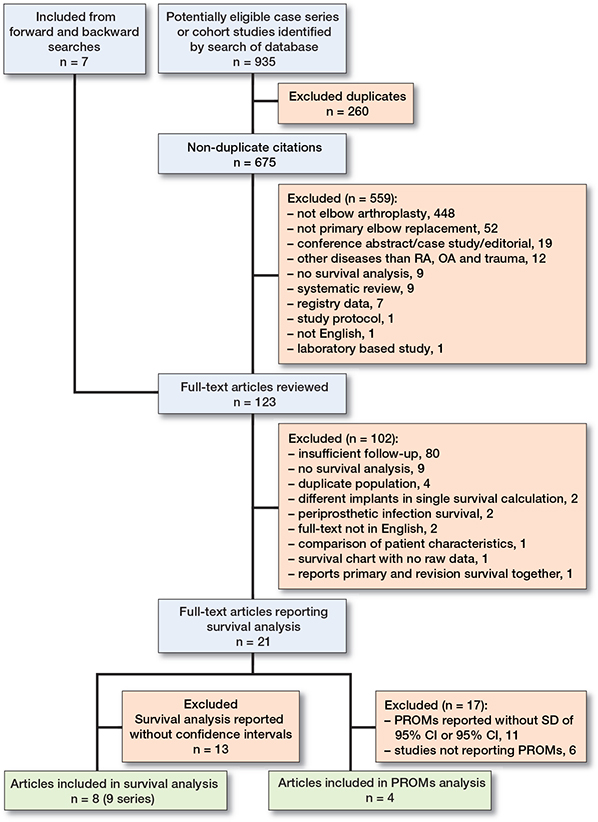
The search of published case-series yielded 935 articles, of which 260 duplicates were removed, leaving 675 articles for screening (Figure 1). Following abstract review, 124 full-text articles were reviewed; dual-reviewer screening isolated 21 full-text articles of case-series reporting greater than 10 years’ mean/median follow-up and reporting survival analysis. Of these, 8 articles, containing 9 implant series, were included in the survival meta-analysis. Of the 21 full-text articles reviewed, 11 reported PROMs, of which only 4 reported in the detail required for the PROMs meta-analysis (Table 2). Of the included articles, 5 (including 6 series) reported survival in linked TER, and 3 (including 3 series) reported survival in unlinked TER. There were no articles reporting > 10-year survival in distal humeral hemiarthroplasty. The proportion of articles with inflammatory arthritis as the primary indication for surgery was 92%.
Quality assessment revealed that 5 (56%) of the 9 series were consecutive, 3 (22%) were multicenter, all had > 80% follow-up (mean loss to follow-up 1.5% ranging from 0% to 7.5%). 2 undertook multivariable analysis. The proportions do reflect that the quality of the published case-series is low.
Case-series
6 unique case-series, published between 1998 and 2020, reported the survival of 628 linked total elbow replacements (linked TERs) at 9 time points with follow-up ranging from 10 to 20 years (Tables 3 and 4, see Supplementary data) (13-17). 6 series reported survival at exactly 10 years (616 linked TERs), 2 at 15 years (487 linked TERs), and 1 at 20 years (435 linked TERs). Pooled survival from those studies reporting at exactly 10 years was 92% (CI 90–95), at 15 years 88% (CI 83–92), and at 20 years 68% (CI 57–79) (Figure 2).
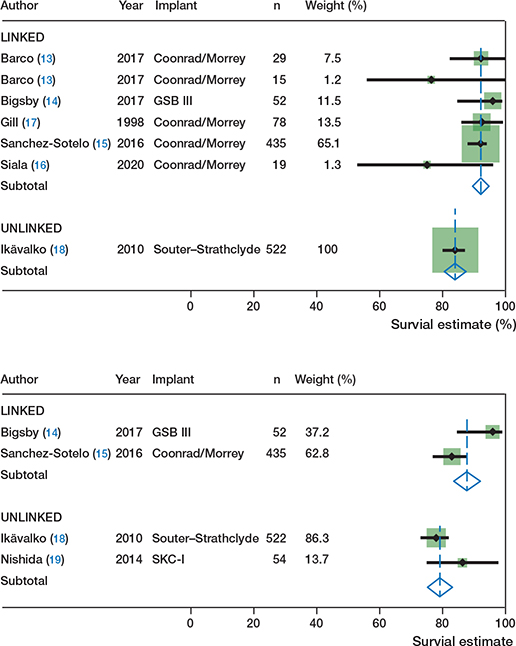
Figure 2. Forest plot estimates for survival of elbow replacements from case series at 10 years (upper panel) and 15 years (lower panel).
3 unique case-series, published between 2010 and 2014, reported the survival of 610 unlinked total elbow replacements (unlinked TERs) at 7 time points with follow-up ranging from 10 to 20 years (18-20). 1 series reported survival at exactly 10 years (522 unlinked TERs), 2 at 15 years (576 unlinked TERs), and 1 at 20 years (54 unlinked TERs). Pooled survival from those studies reporting at exactly 10 years was 84% (CI 81, 88), at 15 years 79% (CI 75–83), and at 20 years 86% (CI 75–98). When studies reported survival estimates at between 10 and 15 years, these results were rounded down to 10 years as a sensitivity analysis. This resulted in a pooled survival of 3 series (610 unlinked TERs) of 84% (CI 81–87) (Figure 3).
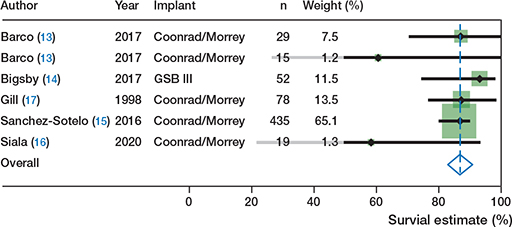
Figure 3. Forest plot of estimates of survival for reported survival of elbow replacements from case series with rounding to 10 years.
Registry data
Implant-level data at 10 years was available from 1 registry report, the Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) 2019 annual report supplemental material (21). Implant-level data at > 10 years from the Norwegian registry was available from a published article (22). In combination, these reports provided 10-year survival of 1 series of linked TER (32 arthroplasties) and 4 series of unlinked TER (530 arthroplasties). The single implant series reporting linked TER at 10 years was 79% (CI 51–92) and was not able to be pooled with other implant series, and for unlinked TER pooled survival was 86% (CI 83–89). At 15 and 20 years, results only for unlinked TER were available and were 74% (CI 68–80) and 76% (CI 68–84) respectively (Figure 4).
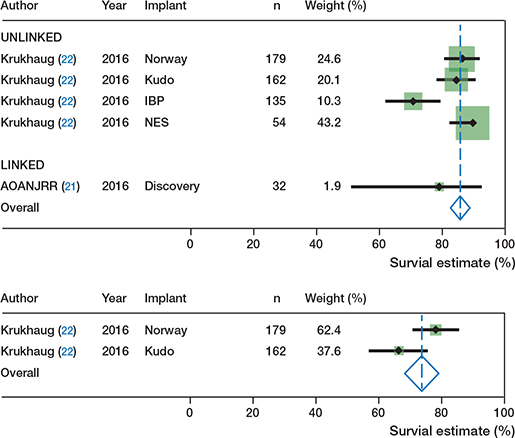
Figure 4. Forest plot of estimates for reported survival of elbow replacements from registry reports at 10 years (upper panel) and 15 years (lower panel).
Patient-reported outcome measures
Of the 8 articles reporting survival analysis with confidence intervals, only 1 reported PROMs in enough detail to be included in the meta-analysis (19). Of the remainder of articles reporting survival without CIs, a further 3 reported pre- and postoperative PROMs with standard deviation or confidence intervals (23-25). All studies used the Mayo Elbow Performance Score (MEPS). 164 TERs (33 linked TERs and 131 unlinked TERs), with an average follow-up of 12 years, were included in the analysis. Demographic data was concordant with the survival outcome series with the indication for surgery as rheumatoid arthritis in 88%, mean age of 57 years (range 55–59) and 88% female. Average mean preoperative scores were 40 (SD 16) and postoperative scores 80 (SD 17). Mean difference between preoperative and postoperative scores was 40 point on the 0–100 scale. Pooled PROMs data showed a large effect of improved outcome from baseline with a SMD of 2.7 (CI 1.6–3.8) in this predominantly rheumatoid arthritis group (Figure 5). No registry reports provide implantlevel PROMs at 10 years or greater follow-up.
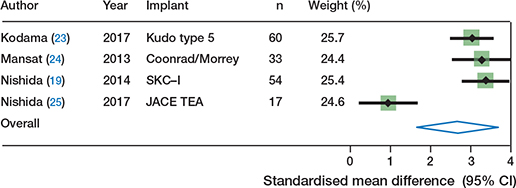
Figure 5. Forest plot of estimates of standardized mean difference (SMD) in patient reported outcome measures (PROMs) score following elbow replacement at > 10 years.
Discussion
This study has identified that over 84% of total elbow replacements can last for at least 10 years and that patients receiving this treatment have a sustained improvement in their patientreported outcome measures. Interpretation of the results from both case-series and registry data for implant type suggest improved survival for linked compared with unlinked TERs, with greater than 90% surviving to 10 years. The generalizability of this finding is limited, as rheumatoid arthritis was the treated pathology in over 90% of the included studies.
This study has employed a methodology previously used in the exploration of hip, knee, and shoulder replacements (6-8). This has provided a simple and easily interpretable result. It is notable that the volume of evidence is more limited for both shoulder and elbow replacements in comparison with hip and knee replacements. Although the number of implants within case-series reports was marginally higher for elbow replacements than shoulders, there is sparse registry-level data available for elbows. Encouragingly, the available evidence from registries and case-series estimates the same results for unlinked TERs, suggesting that these case-series were not prone to publication bias, which is a common criticism.
We have calculated a survival estimate for each individual implant. This estimate is then pooled to give a construct/class estimate (linked or unlinked TER), weighted according to the standard error. The rationale for this process, and the exclusion of multi-implant series, relates to the implant itself being fundamental to the survival outcome, which may be hidden in a series including multiple implants. This type of analysis is unique to our study, and values each series as an individual cohort, thereby providing an overall estimate based on the frequency of use of the implant. The construct/class chosen for this study was linked and unlinked prostheses; although further granular classification of implant is possible, we wished to provide a patient-focused and generalizable result. With the maturity of registry data and improved case-series reporting, more granular exploration of data may be possible in the future. This method is dependent, however, on both case-series and registries reporting implant-level data, without which patterns of implant failure cannot be accounted for. This restriction on inclusion resulted in significant attrition of potential data and we would strongly encourage implant-level reporting in future long-term survival series.
At 10 years, synthesis of case-series estimates suggests a difference in long-term survival between linked TER (92%) and unlinked TER (84%) in a cohort treated almost exclusively for rheumatoid arthritis. The survival advantage of linked TER is maintained at 15 years; at 20 years very limited evidence from a single series suggests a significant decline in survival. At 10 years the predominant linked TER was the Coonrad/Morrey (ZimmerBiomet, Warsaw, IN, USA) and unlinked TER was the Souter-Strathclyde (Stryker Howmedica Osteonics, Limerick, Ireland). As we have asserted, survival and implant choice are interrelated and therefore the reported implants need to be placed within the context of contemporary practice. The Coonrad/Morrey remains a frequently utilized implant, with the NJR reporting its use in 52% of all primary elbow replacements (26). However, the Souter-Strathclyde has been discontinued owing to poor survival, therefore the estimates within this review may not be representative of contemporary unlinked designs. Within the registry reports, the most frequently reported implants were the Norway, iBP, and Kudo; no Souter-Strathclyde prostheses were within this registry dataset. It is of note that the resultant survival for unlinked designs was similar between case-series (84%) and registry (86%) data, suggesting that the survival is not explicitly related to a single brand of implant.
The indication for surgery in the included case-series was predominantly rheumatoid arthritis (92%). Although this is likely to have represented practice over 10 years ago, the emergence of biological drug therapies has significantly diminished the surgical burden of rheumatoid arthritis (27). In their review of indications for TER, Samdanis et al. reported that although rheumatoid arthritis remained the most common indication for TER, the proportionate use of this procedure dropped from 77% in 1982 to 50% in 2010 (28). In their review of registry reports, Macken et al. report inflammatory arthritis as the primary indication in 44% of TEA, followed by acute trauma (28%) and osteoarthritis (17%) (1). Differential survival based on indication at medium-term follow-up has been found in the Danish National Patient Register where, at 8.7 years follow-up, fracture sequelae were associated with the highest revision risk (29). Within the Australian Joint Registry, TER for primary osteoarthritis is reported as conferring the poorest survival at 7 years, with acute fracture/dislocation the best survival (21). Further registry and case-study reports assessing survival in cohorts representative of contemporary practice are required to assess for differences between indications that may change the generalizability of this review’s survival estimate.
Of the 21 studies that reported survival at > 10 years, 13 did not include CIs and could not be added to the meta-analysis. Were these studies included, an additional 594 arthroplasties would have been included. Excluded studies also reported the combined survival of multiple implants, and individual component failure (ulna or humeral) but not whole-construct or combined radiographic failure and revision (30).
Only 4 studies reported pre- and postoperative PROMs. All the included studies used the Mayo Elbow Performance Score (MEPS), which is a clinician- and patient-completed outcome measure. The MEPS was developed in 1992 for the assessment of elbow replacement outcomes, has adequate metric properties, and is the most commonly used PROM for elbow replacement (31-33). Over 10 years from initial surgery, a large improvement (SMD 2.7) was observed. This composite clinician- and patient-reported improvement in pain and function is of a similar order of magnitude to that previously reported in shoulder arthroplasty (7). The mean difference between pre and postoperative scores was 40, exceeding the estimated 11-point change required to be clinically meaningful to patients (34). Although multiple registries now collect validated PROMs for elbow arthroplasty, none have reported results to 10 years’ follow-up.
The limitations of this work are worth noting. Results from individual case series, as opposed to national registries, may be altered by differing revision thresholds between surgeons. The reliance on single-center and design-center case-series data may alter the representativeness of the findings, particularly when extrapolated to low-volume surgeons and centers. Our analysis of the data in this study highlights the results that are possible, but as the majority of data is not nationally mandated data, it cannot be assumed that these results would be achieved uniformly. As not all implant failures result in revision, we reported patient-reported outcomes to better define the overall value of elbow replacement, although the depth and granularity of this data was poor. We suggest that a high compliance of reporting of patient-reported outcome measures that have strong evidence of psychometric validity is highly desirable. Our pooled registry results are drawn predominantly from the Norwegian register, which has a predominance of implants not currently used. As the available follow-up in other registries increases, a wealth of data will soon become available, and we would encourage implantlevel reporting by brand and product line. We also assumed that survival estimates are equivalent to risks for generating pooled estimates, and although the assumption that no censoring occurs (patients dying with an elbow in situ) is violated, it provides a useful method of aggregation in the absence of individual patient data. The aggregated estimates of survival are, however, the largest possible sample and this is the largest report of this type and length of follow-up.
The strengths of this study include an inclusive and comprehensive design and realistic interpretation of survivorship that accounts for all revisions and not a limited or biased subset, as well as a patient outcome focus. From a patient perspective, all revision surgery carries risk and therefore all-cause revision should be considered.
Conclusion
Although elbow replacement is performed far less frequently than hip, knee, or shoulder replacement, its use is increasing and information for patients and clinicians on the longevity of implants and impact on quality of life is vital. We pooled estimates from case-series and registry data and found that over 80% of elbow replacements last more than 10 years in rheumatoid arthritis. For linked elbow replacements this was over 90%. Patients experienced a sustained improvement in pain and function for the 10 years following surgery.
- Macken A A, Prkic A, Kodde I F, Lans J, Chen N C, Eygendaal D. Global trends in indications for total elbow arthroplasty: a systematic review of national registries. EFORT Open Rev 2020; 5: 215-20.
- Orthopaedic Data Evaluation Panel (ODEP). Available from: http://www.odep.org.uk/ (accessed March 11, 2020).
- Deere K C, Whitehouse M R, Porter M, Blom A W, Sayers A. Assessing the non-inferiority of prosthesis constructs used in hip replacement using data from the National Joint Registry of England, Wales, Northern Ireland and the Isle of Man: a benchmarking study. BMJ Open 2019; 9: e026685.
- Smith A J, Dieppe P, Vernon K, Porter M, Blom A W. Failure rates of stemmed metal-on-metal hip replacements: analysis of data from the National Joint Registry of England and Wales. Lancet 2012; 379: 1199-204.
- Moher D, Liberati A, Tetzlaff J, Altman D G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009; 151: 264-9.
- Evans J T, Evans J P, Walker R W, Blom A W, Whitehouse M R, Sayers A. How long does a hip replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet 2019; 393: 647-54.
- Evans J P, Evans J T, Craig R S, Blom A W, Whitehouse M R, Sayers A. How long does a shoulder replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 10 years of follow-up. Lancet Rheumatol 2020; 2: e539-48.
- Evans J T, Walker R W, Evans J P, Blom A W, Sayers A, Whitehouse M R. How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet 2019; 393: 655-63.
- Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan: a web and mobile app for systematic reviews. Syst Rev 2016; 5: 210.
- Gooberman-Hill R, Burston A, Clark E, Johnson E, Nolan S, Wells V, et al. Involving patients in research: considering good practice. Musculoskeletal Care 2013; 11: 187-90.
- Cohen J. Statistical power analysis for the behavioral sciences. London: Routledge; 2013. doi: 10.4324/9780203771587.
- Wylde V, Beswick A D, Dennis J, Gooberman-Hill R. Post-operative patient-related risk factors for chronic pain after total knee replacement: a systematic review. BMJ Open 2017; 7: e018105.
- Barco R, Streubel P N, Morrey B F, Sanchez-Sotelo J. Total elbow arthroplasty for distal humeral fractures: a ten-year-minimum follow-up study. J Bone Joint Surg Am 2017; 99: 1524-31.
- Bigsby E, Kemp M, Siddiqui N, Blewitt N. The long-term outcome of the Gschwend–Scheier–Bähler III elbow replacement. J Shoulder Elbow Surg 2016; 25: 362-8.
- Sanchez-Sotelo J, Baghdadi Y M K, Morrey B F. Primary linked semiconstrained total elbow arthroplasty for rheumatoid arthritis: a single-institution experience with 461 elbows over three decades. J Bone Joint Surg Am 2016; 98: 1741.
- Siala M, Laumonerie P, Hedjoudje A, Delclaux S, Bonnevialle N, Mansat P. Outcomes of semiconstrained total elbow arthroplasty performed for arthritis in patients under 55 years old. J Shoulder Elbow Surg 2019. doi: https://dx.doi.org/10.1016/j.jse.2019.08.006.
- Gill D R J, Morrey B F. The Coonrad-Morrey total elbow arthroplasty in patients who have rheumatoid arthritis: a ten to fifteen-year follow-up study. J Bone Joint Surg 1998; 80: 1327-35.
- Ikävalko M, Tiihonen R, Skyttä E T, Belt E A. Long-term survival of the Souter-Strathclyde total elbow replacement in patients with rheumatoid arthritis. J Bone Joint Surg Br 2010; 92: 656-60.
- Nishida K, Hashizume K, Nasu Y, Kishimoto M, Ozaki T, Inoue H. A 5–22-year follow-up study of stemmed alumina ceramic total elbow arthroplasties with cement fixation for patients with rheumatoid arthritis. J Orthop Sci 2014; 19: 55-63.
- Qureshi F, Draviaraj K P, Stanley D. The Kudo 5 total elbow replacement in the treatment of the rheumatoid elbow: results at a minimum of ten years. J Bone Joint Surg Br 2010; 92: 1416-21.
- AOANJRR. Australian Orthopaedic Association National Joint Replacement Registry. Demographics and outcome of elbow and wrist arthroplasty; 2020. Available from: https://aoanjrr.sahmri.com/annual-reports-2020/supplementary. (accessed July 19, 2021).
- Krukhaug Y, Hallan G, Dybvik E, Lie S A, Furnes O N. A survivorship study of 838 total elbow replacements: a report from the Norwegian Arthroplasty Register 1994–2016. J Shoulder Elbow Surg 2018; 27: 260-9.
- Kodama A, Mizuseki T, Adachi N. Kudo type-5 total elbow arthroplasty for patients with rheumatoid arthritis: a minimum ten-year follow-up study. Bone Joint J 2017; 99-B: 818-23.
- Mansat P, Bonnevialle N, Rongières M, Mansat M, Bonnevialle P, for Shoulder FS. Results with a minimum of 10 years follow-up of the Coonrad/Morrey total elbow arthroplasty. Orthop Traumatol Surg Res 2013; 99: S337-43.
- Nishida K, Hashizume K, Ozawa M, Takeshita A, Kaneda D, Nakahara R, et al. Results of total elbow arthroplasty with cementless implantation of an alumina ceramic elbow prosthesis for patients with rheumatoid arthritis. Acta Med Okayama 2017; 71: 41-7.
- Ben-Shlomo Y, Blom A, Boulton C, et al. The National Joint Registry 17th Annual Report 2020. London (www.njrcentre.org.uk); 2020.
- Burmester G R, Pope J E. Novel treatment strategies in rheumatoid arthritis. Lancet 2017; 389: 2338-48.
- Samdanis V, Manoharan G, Jordan R W, Watts A C, Jenkins P, Kulkarni R, et al. Indications and outcome in total elbow arthroplasty: a systematic review. Shoulder Elbow 2020; 12: 353-61.
- Plaschke H C, Thillemann T M, Brorson S, Olsen B S. Implant survival after total elbow arthroplasty: a retrospective study of 324 procedures performed from 1980 to 2008. J Shoulder Elbow Surg 2014; 23: 829-36.
- Sayers A, Evans J T, Whitehouse M R, Blom A W. Are competing risks models appropriate to describe implant failure? Acta Orthop 2018; 89: 256-8.
- Evans J P, Smith C D, Fine N F, Porter I, Gangannagaripalli J, Goodwin V A, et al. Clinical rating systems in elbow research: a systematic review exploring trends and distributions of use. J Shoulder Elbow Surg 2018; 27: e98-106.
- Morrey B F, Adams R A. Semiconstrained arthroplasty for the treatment of rheumatoid arthritis of the elbow. J Bone Joint Surg 1992; 74: 479-90.
- Dawson J, Doll H, Boller I, Fitzpatrick R, Little C, Rees J, et al. The development and validation of a patient-reported questionnaire to assess outcomes of elbow surgery. J Bone Joint Surg Br 2008; 90-B: 466-73.
- Celik D. Psychometric properties of the Mayo Elbow Performance Score. Rheumatol Int 2015; 35: 1015-20.
Supplementary data
| Author | Year | Implant | F-U years | Survival estimate (%) (CI) |
| Barco (13) a | 2017 | Coonrad/Morrey | 10 | 92 (82–100) |
| Barco (13) b | 2017 | Coonrad/Morrey | 10 | 76 (56–100) |
| Bigsby (14) | 2016 | GSBIII | 10 | 96 (85–99) |
| 15 | 96 (85–99) | |||
| Ikävalko (18) | 2010 | Souter Strathclyde | 10 | 84 (80–87) |
| 15 | 78 (73–82) | |||
| 19 | 72 (65–88) | |||
| Nishida (19) | 2014 | SKC-I | 12.3 | 86 (75–98) |
| 15 | 86 (75–98) | |||
| 20 | 86 (75–98) | |||
| Sanchez-Sotelo (15) | 2016 | Coonrad/Morrey | 10 | 92 (88–94) |
| 15 | 83 (77–88) | |||
| 20 | 68 (56– 78 | |||
| Siala (18) | 2020 | Coonrad/Morrey | 10 | 75 (53–96) |
| Gill (17) | 1998 | Coonrad/Morrey | 10 | 92 (86–99) |
| a not rheumatoid arthritis | ||||
| b rheumatoid arthritis | ||||
| Author | Year | Implant | F-U years | PROM | Mean score (SD) | |
| preoperative | pos toperative | |||||
| Kodama (23) | 2017 | Kudo type 5 | 12 | MEPS | 43 (14) | 80 (11) |
| Mansat (24) | 2013 | Coonrad/Morrey | 11 | MEPS | 31 (17) | 82 (14) |
| Nishida (19) | 2014 | SKC-I | 13 | MEPS | 40 (14) | 90 (15) |
| Nishida, (25) | 2017 | JACE TEA | 11 | MEPS | 45 (18) | 69 (28) |