Surgery rates for lumbar spinal stenosis in Denmark between 2002 and 2018: a registry-based study of 43,454 patients
Rikke K JENSEN 1,2, Berit SCHIØTTZ-CHRISTENSEN 3,4, Christian Volmar SKOVSGAARD 5, Mathias THORVALDSEN 6, Rune Mygind MIERITZ 6, Andreas K ANDRESEN 7, Henrik Wulff CHRISTENSEN 2, and Jan HARTVIGSEN 1,2
1 Department of Sports Science and Clinical Biomechanics, University of Southern Denmark, Odense; 2 Chiropractic Knowledge Hub, Odense; 3 Spine Centre of Southern Denmark, University Hospital Lillebaelt, Middelfart; 4 Department of Regional Health Research, University of Southern Denmark, Odense; 5 DaCHE—Danish Centre for Health Economics, Department of Public Health, University of Southern Denmark, Odense; 6 Department of Neurosurgery, University Hospital Odense, Odense; 7 Spine Surgery and Research, Spine Centre of Southern Denmark, University Hospital Lillebaelt, Middelfart, Denmark
Background and purpose — Over the last decades, many countries have shown increased surgery rates for lumbar spinal stenosis (LSS), but little information is available from Denmark. We describe the development in diagnosis and surgery of LSS in Denmark between 2002 and 2018.
Patients and methods — We collected diagnostic ICD10-codes and surgical procedure codes from private and public hospitals in Denmark from the Danish National Patient Register. Patients diagnosed with LSS and those with surgical procedure codes for decompression surgery with or without fusion were identified. Annual surgery rates were stratified by age, sex, and type of surgery.
Results — During these 17 years, 132,138 patients diagnosed with LSS and 43,454 surgical procedures for LSS were identified. The number of surgical procedures increased by 144%, from 23 to 56 per 100,000 inhabitants. The proportion of patients diagnosed with LSS who received surgery was about 33%, which was almost stable over time. Decompression without fusion increased by 128% from 18 to 40 per 100,000 inhabitants and decompression with fusion increased by 199%, from 5 to 15 per 100,000.
Interpretation — Both the prevalence of LSS diagnoses and LSS surgery rates more than doubled in Denmark between 2002 and 2018. However, the proportion of patients diagnosed with LSS who received surgery remained stable. Decompression surgery with fusion increased at a higher rate than decompression without fusion, although recent evidence suggests no advantage of decompression plus fusion over decompression alone.
Citation: Acta Orthopaedica 2022; 93: 488–494. DOI http://dx.doi.org/10.2340/17453674.2022.2744.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-01-25. Accepted: 2022-04-07. Published: 2022-05-24.
Correspondence: rikkekruger@kiroviden.sdu.dk
RKJ, BSC, MT, RMM, AKA, and JH conceptualized the study. CVS conducted the analysis and RKJ drafted the paper. All authors participated in the interpretation of data for the work, critically revised the manuscript for important intellectual content, and contributed to discussion of the manuscript.
The authors would like to thank the Danish National Patient Register for providing access to the data used in this paper.
Acta thanks Roel F M R Kersten and Peter Fritzell for help with peer review of this study.
Degenerative lumbar spinal stenosis (LSS) is a common condition, although the prevalence varies substantially according to diagnostic criteria and target population (1). A systematic review found a pooled prevalence estimate of 11% (95% CI 4–18) in the general population and 29% (95% CI 22–36) in a secondary care population with low back and/or leg pain (1). The prevalence of LSS increases with age due to the degenerative nature of the disease. As the prevalence of diseases such as diabetes, overweight, and hypertension also increases with age, the overall risk of a complicated course of disease for people with LSS due to multimorbidity increases (2-4). With a growing elderly population, a higher burden of LSS must be expected both for the individual patients suffering from pain and disability and for the society facing higher healthcare expenditure.
If patients do not benefit from the non-surgical treatment options or present with severe progressive neurological deficits, decompression surgery is often suggested (5,6). Decompression surgery is the most commonly performed procedure in spine surgery in people over 65 years of age (7) and over the last decades there has been an increase in rates of surgery for LSS.
Fusion is often considered if cooccurring degenerative spondylolisthesis is present on imaging, although recent evidence suggests no advantage of decompression plus fusion over decompression alone (8).
The development in LSS surgery rates in Denmark has not previously been presented. Therefore, we aimed to describe the development in diagnoses of LSS in Danish hospitals and surgery rates for LSS in Denmark between 2002 and 2018.
Patients and methods
This is a retrospective observational study based on data from the Danish National Patient Register (DNPR) (9,10). This study was reported according to the STROBE checklist.
Setting and data source
Data on diagnoses and surgical procedures was harvested from the DNPR. The DNPR serves as the basis for ongoing hospital statistics and is administered by the Danish Health Authority (9,10). Danish hospital departments register data from both inpatient and outpatient activities in the DNPR, which was established in 1977 (10). The DNPR contains information on LSS diagnoses and all surgical procedures from publicly funded hospitals and private hospitals from 2002 onward. Registrations in DNPR are digital and performed by the hospital on discharge. Since 2000 the DNPR has formed the basis for payment to public hospitals, and registration is assumed to be complete since then (10). Danish hospitals are primarily publicly funded and reporting to the DNPR also became compulsory for private hospitals in 2003. Private hospitals also receive payment from the DNPR system as they offer services paid for by taxes or as part of an agreement with the region. However, services can also be paid for privately either by insurance companies or private persons, and this registration is known to be incomplete (10). The National Board of Health has estimated that 5% of all operations are missing in the DNPR (10). The research potential of the DNPR has previously been validated (11). The DNPR includes data on diagnostic codes based on ICD-10 or ICD-11 and surgical procedure codes, which build on the Danish version of the Nordic Medico-Statistical Committee (NOMESCO) Nordic Classification of Surgical Procedures (NCSP) system.
Study population
The study population consisted of patients above 18 years registered by a public or private hospital in the DNPR between January 1, 2002, and December 31, 2018. To estimate the prevalence of LSS in secondary care, data was collected on patients classified with a primary diagnostic code of (i) spinal stenosis (DM48.0) or (ii) spondylolisthesis (DM43.1) as the primary diagnostic code in combination with spinal stenosis (DM48.0) as the secondary diagnostic code. Patients were defined as incident in a certain year if they were registered with the relevant codes and were not part of the population in the previous year. Although DM48.0 is primarily used for LSS, it is possible that patients with cervical or thoracic stenosis could be assigned the same code because of differences in coding practices between departments. As there is no specific diagnostic code to differentiate spinal regions (cervical, thoracic, and lumbar), we attempted to “clean” the group by excluding patients with a surgical procedure code of cervical disc herniation (ABC01, ABC10, ABC20, ABC21), cervical decompression (ABC30, ABC50, ABC60), thoracic disc herniation (ABC04, ABC13, ABC23), or thoracic decompression (ABC33, ABC53, ABC63) 270 days after or 90 days before diagnosis. We still refer to this study population as “LSS” for practical reasons.
To estimate LSS surgery rates, we collected data on surgical procedure codes for decompression (ABC36, ABC56, ABC66) and supplementary fusion surgery codes (NAG43, NAG44, NAG46, NAG63, NAG64, NAG66, NAG73, NAG74, NAG76). Procedure codes had to be in combination with a primary or secondary diagnostic code of spinal stenosis (DM48.0). Exclusion criteria were diagnoses indicating scoliosis, deformation, inflammation or infection, fracture, tumors, cancer, or spinal disease from a secondary disease (e.g., tuberculosis). Only the 1st code was included if a patient had more than 1 surgical procedure code within a year. However, the number of surgical episodes per person per year was collected to gain an overview of the total number of surgical episodes. Data on interlaminar stabilization (ABC28) using an interspinous distraction device was collected separately.
Variables
Data on diagnostic codes, surgical procedure codes, date, age, and sex were collected.
Statistics
The annual prevalence and incidence of a diagnosis of LSS in secondary care as well as the annual incidence of LSS surgery were calculated both as totals and stratified by type of surgery, sex, and 10-year age categories. Also, data was stratified as 1 or more surgical procedures within a year. Changes in surgery rates were reported as percentages with 95% confidence intervals (CI).
To account for changes in the composition of the background population over time the denominator was defined according to the numerator, but for the Danish population. For instance, when the numerator included only males, the denominator included all males in the Danish population in the given year, and when the numerator included a given age group, the denominator included all Danes in the given age group in that year. “Danes” were defined as people living in Denmark on January 1 of each year, and rates were reported per 100,000 inhabitants. This information is publicly available through Statistics Denmark (12).
Surgery was divided into 2 categories: decompression without fusion and decompression with fusion. A third type of surgery, “interlaminar stabilization”, did not fit either of the categories and was therefore reported separately.
Characteristics of patients and distribution of surgical procedure codes are presented as total and percentage of all Danes. Proportions of age groups for all Danes were calculated as the weighted averages of yearly age group proportions and the yearly proportion of surgeries was used as weights. For example, for 2002, the age groups proportions received a weight of 0.028, corresponding to the share of all surgeries that were performed in 2002. Proportions of men and women for all Danes were calculated in the same way.
Ethics, registration, data sharing, funding, and potential conflicts of interest
The use of registry data for research does not require approval from the ethics committees in Denmark (13). The Danish National Patient Register is administered by the Danish Health Authorities and patient consent is not required for statistical use of data.
The use of personal data follows the General Data Privacy Regulations and Danish data protection legislation. Data access was granted from the Research Service, part of the Danish Health Data Authority. The Danish Data Protection Agency was notified of the project (file number 2015-57-0008; register 10.353).
The data that supports the findings of this study can be applied for from the Danish National Patient Register, but restrictions apply to the availability of this data, which was used under license for the current study, and so it is not publicly available. No funding was received to perform this study. The authors have no conflicts of interest to declare.
Results
The total number of LSS diagnoses in secondary care between 2002 and 2018 was 132,138 (Figure 1). The mean age was 67 (SD 12) (10th percentile: 51 years, 90th percentile: 80 years), and 55% were women.
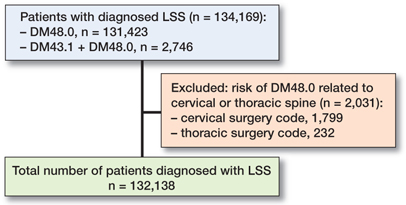
Figure 1. Flowchart of data collection for LSS according to diagnostic ICD10-code DM48.0.
The number of surgical procedure codes for decompression between 2002 and 2018 was 43,454 (Figure 2, Table). Patients had a mean age of 67 (SD 11) (10th percentile: 52 years, 90th percentile: 80 years), and 55% were women. Of the 43,454 operated patients, 69% had decompression surgery only, and 31% received decompression with fusion. 5% (n = 2,152) had 2 or more decompression surgical procedures within a year.
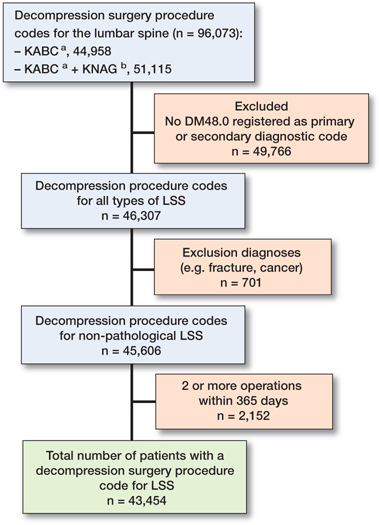
Figure 2. Flowchart of data collection for surgical procedure coding of LSS. a ABC36, ABC56, ABC66; b NAG43, NAG44, NAG46, NAG63, NAG64, NAG66, NAG73, NAG74, NAG76.
Patients receiving decompression surgery were underrepresented in the age category 18–50 and generally overrepresented in age categories above 50 years. Also, women were slightly overrepresented compared with men, which can be explained by a large overrepresentation of women receiving decompression with fusion (Table).
The number diagnosed with LSS increased from 3,847 in 2002 to 10,156 in 2018. The increase happened between 2002 and 2015 and then stabilized and even decreased a little in 2018.
The increasing LSS diagnoses over time exceeded the population growth in the Danish population for the corresponding age groups and increased by 164% from 2002 to 2018 (6.3% yearly). The increase in surgery rates and LSS diagnoses was similar until about 2010–2012, after which noticeable variation over time was observed (Figure 3).
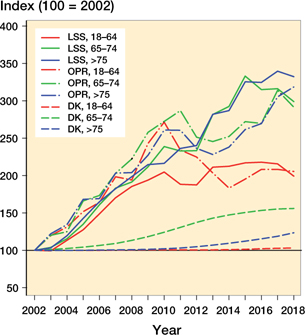
Figure 3. Development in diagnoses of LSS (solid lines), LSS surgery (dashed dotted lines), and demographic in Denmark (dashed lines) by 3 age groups.
The number of surgical procedure codes for decompression with or without fusion per 100,000 inhabitants increased by 144% from 23 (CI 22–24) to 56 (CI 54–57) per 100,000 between 2002 and 2018 (5.7% yearly). Decompression without fusion increased by 128% from 18 (CI 17–19) to 40 (CI 39–42) per 100,000 (5.3% yearly) and decompression with fusion increased by 199% from 5.1 (CI 4.5–5.7) to 15 (CI 14–16) per 100,000 (7.1% yearly) (Figure 4). Between 2002 and 2018, there were 418 procedure codes registered for an interspinous distraction device. The use of this procedure peaked from 2006 to 2010 and then dropped to less than 20 per year.
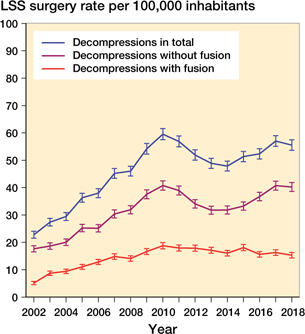
Figure 4. Procedure codes for decompression with and without fusion and in total from 2002 to 2018. Rates were calculated per 100,000 inhabitants in Denmark as of January 1 each year.
Throughout the period, 23% of all patients diagnosed with LSS received decompression surgery without fusion, and 10% underwent decompression with fusion. These proportions remained relatively stable over time except for a small decline between 2011 and 2014. The decline was mainly related to a decline in decompression without fusion (Figure 5).
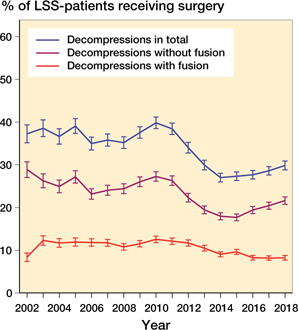
Figure 5. Percentage of patients with LSS per year receiving decompression surgery with or without fusion. Percentages were calculated based on the prevalent LSS population each year.
We did not find a difference in “decompression without fusion” when surgery rates were stratified by sex. However, statistically significantly more women than men received “decompression with fusion” (Figure 6). The difference between women and men increased with age, and the difference became statistically significant for the groups with patients aged 61–70 and 71–80 but not for the group with patients > 80 years.
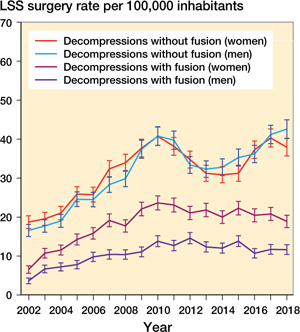
Figure 6. Procedure codes for decompression with and without fusion from 2002 to 2018 stratified by sex. Rates were calculated respectively per 100,000 men and per 100,000 women in Denmark as of January 1 each year.
Surgery rates were very low in the youngest age group (18–50) and increased with increasing age except for the oldest age group (> 80 years) (Figure 7).
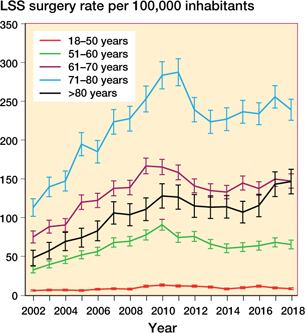
Figure 7. Procedure codes for decompression with and without fusion from 2002 to 2018 stratified by age. Rates were calculated per 100,000 in each age group in Denmark as of January 1 each year to account for changes in the age composition of the population. For instance, the rates in 2010 were calculated per 100,000 in each age group in Denmark in 2010.
Discussion
Both the prevalence of LSS diagnoses and LSS surgery rates more than doubled in Denmark between 2002 and 2018, whereas the proportion of patients diagnosed with LSS who received surgery (33%) remained basically unchanged, except from a small decline from 2011 to 2014. However, decompression surgery with fusion increased at a higher rate than decompression without fusion.
The 144% increase in decompression surgery rates in Denmark (5.7% yearly) is lower than in a comparable study from Norway showing a 238% increase in decompression surgery from 1999 to 2013 (9.1% yearly) (14). Compared with the Scandinavian studies, an Australian study (15) investigating surgery rates for LSS from 2003 to 2013 reported an increase of only 31% (2.7% yearly). At the end of the data collection period (2013), the Norwegian study (14) reported a decompression surgery rate with or without fusion of 39 per 100,000, and the Australian study (15) had a surgery rate of 27 per 100,000. The surgery rate for decompression with or without fusion in Denmark in 2013 was 49 per 100,000 and thus comparable to Norway, although about 25% higher. Populations and healthcare systems are considered comparable between Norway and Denmark, but the Norwegian study did not include private hospitals, accounting for about 10% of LSS surgeries, which could explain some of the difference.
Decompression with fusion increased by 199% (7.1% yearly) in Denmark, 78% (4.2% yearly) in Norway (14), and 174% (11% yearly) in Australia (15). There is no clear explanation for this variation. Fusion is traditionally considered in lumbar spondylolisthesis, which has previously been associated with increasing age in both sexes and shown to have a higher prevalence in women (16). Our results showed that surgery rates increased with age and that more women than men received decompression with fusion, which could explain some of the increase but not the variation between countries. A study from 2019 (17) compared LSS decompression surgery rates from 2011 to 2013 using data from 3 comparable Scandinavian national spine registries and found that decompression with fusion was used in 11% of the cases in Norway, 21% in Sweden, and 28% in Denmark. When the subgroup of patients with concomitant spondylolistheses was considered, the numbers were 47% in Norway, 56% in Sweden, and 88% in Denmark. In patients without spondylolisthesis the numbers were 4%, 9%, and 15%, respectively. However, that study did not find that concomitant fusion was associated with better outcomes, which is in line with previous findings (8,18,19). The 3 Scandinavian countries have comparable healthcare systems, social systems, educational systems, culture, and ethnicity. Therefore, the variation in use of concomitant fusion is more likely to reflect differences in surgical traditions and different interpretation of indications. The increasing rate of additional fusion in Denmark is notable considering that there is no apparent gain in effectiveness or reoperation rate while there is a risk of increased healthcare expenses as a consequence of prolonged hospital stay (8,17).
There are indications of provider inducement within the field of spine surgery. In a study from the United States (20) patients receiving surgery for LSS were more likely to have fusion surgery when operated on in a fee-for-service system compared with a system with salaried employees, even though LSS is not a generally accepted indication for fusion. Also, this difference was not found when the condition treated was spondylolisthesis, in which fusion is generally accepted as indicated surgical procedure. However, all surgeons at Danish public hospitals are salaried employees, and provider inducement is therefore unlikely to have influenced surgery rates or type of surgery in the present study.
The increase in the number of LSS diagnoses follows almost the same pattern as the surgery rates, but between 2011 and 2014 the number of diagnoses increased substantially more than the surgery rates. Hence, the increase in surgery rates is more likely linked to improved or increased awareness of LSS. The increased use of MRI over the previous 2 decades (21) is likely to have affected the diagnostic rates of LSS, as LSS is a common finding on MRI. A correlation between the use of advanced diagnostic imaging and an increase in healthcare utilization, including spine surgery has been shown (22,23), and it is possible that such an association also exists in Denmark. However, the general increase in LSS surgery rates shown across many studies (14,15,24,25) is most likely influenced by multiple factors such as aging populations, improved surgery techniques, better treatment capacity, and patient expectations.
Increasing surgery rates lead to increased healthcare costs for society as a direct consequence of the surgical procedure and hospital admission. Compared with decompression alone, decompression plus fusion has been shown to more than double the direct hospital costs (15). However, as surgery could have an impact on pain intensity and physical function (6), it is possible that social expenditure could be saved in relation to additional treatments, use of pain medication, and less need for home care as well as increased working capacity for those still on the labor market. Future research should include comprehensive socioeconomic analyses to explore the economic burden for society and the implication for patients.
The risk of misclassification of diagnoses in registry data is the main limitation of this study (11,26). Although the diagnostic code for spinal stenosis (ICD-10 DM48.0) (27) is mainly used for LSS in clinical practice, it is not specific for the lumbar region, and even though we excluded surgical procedure codes for cervical and thoracic regions, our study population might contain some patients with cervical or thoracic spinal stenosis. Therefore, the “true” estimate of LSS diagnoses is likely lower. Also, as there is no gold standard for diagnosing LSS, the use of DM48.0 could be subject to variation. However, these uncertainties are unlikely to vary over time, and therefore the results can still provide an estimate of the development over time, keeping in mind that the absolute prevalence estimate should be interpreted with caution.
We used both a diagnostic code and a surgical procedure code to select the population who received surgery, and we excluded decompression surgery for other reasons (e.g., trauma, cancer, and infection), which decreases the risk of misclassification (26). Approximately 5,300 patients who received decompression surgery were coded with both DM48.0 (spinal stenosis) and DM51 “Other intervertebral disc disorders” or sub-classifications of DM51. It is therefore possible that some had symptoms more strongly linked to radiculopathy caused by, for example, disc herniation than to their LSS. However, multiple degenerative findings of lumbar motion segments are common with increasing age (28), and as disc pathology is part of the degenerative process involved in symptomatic LSS (29) a distinct diagnostic differentiation is not possible. A post hoc sensitivity analysis excluding patients with subclassifications of DM51 as the primary diagnosis (n = 1,612) did not alter the overall results except for a minimal change in surgery rates per 100,000.
The obvious strength of this study is the population size, which includes at least 95% of LSS surgeries in Denmark (10), the completeness of the DNPR which has previously been validated including data from both public and private hospitals (11), and the time span of 17 years.
In conclusion, the prevalence of LSS diagnoses and LSS surgery rates more than doubled in Denmark between 2002 and 2018. However, the proportion of patients diagnosed with LSS who received surgery remained relatively constant except for a small decline between 2011 and 2014. Decompression surgery with fusion increased at a higher rate than decompression without fusion.
- Jensen R K, Jensen T S, Koes B, Hartvigsen J. Prevalence of lumbar spinal stenosis in general and clinical populations: a systematic review and meta-analysis. Eur Spine J 2020; 29: 2143-63.
- Bays A, Stieger A, Held U, Hofer L J, Rasmussen-Barr E, Brunner F, et al. The influence of comorbidities on the treatment outcome in symptomatic lumbar spinal stenosis: a systematic review and meta-analysis. N Am Spine Soc J 2021; 6: 100072.
- Ferrero E, Lonjon G, Bouyer B, Sabourin M, Ould-Slimane M, Guigui P. Influence of comorbidities on patients reported outcomes in degenerative lumbar spinal stenosis. Orthop Traumatol Surg Res 2018; 104: 1031-6.
- MacMahon S, Calverley P, Chaturvedi N, Chen Z, Corner L, Davies M, et al. Multimorbidity: a priority for global health research. London: Academy of Medical Sciences; 2018.
- Bagley C, MacAllister M, Dosselman L, Moreno J, Aoun S G, El Ahmadieh T Y. Current concepts and recent advances in understanding and managing lumbar spine stenosis. F1000Res 2019; 8.
- Rousing R, Jensen R K, Fruensgaard S, Strom J, Brogger H A, Degn J D M, et al. Danish national clinical guidelines for surgical and nonsurgical treatment of patients with lumbar spinal stenosis. Eur Spine J 2019; 28: 1386-96.
- Deyo R A, Mirza S K, Martin B I, Kreuter W, Goodman D C, Jarvik J G. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 2010; 303: 1259-65.
- Forsth P, Olafsson G, Carlsson T, Frost A, Borgstrom F, Fritzell P, et al. A randomized, controlled trial of fusion surgery for lumbar spinal stenosis. N Engl J Med 2016; 374: 1413-23.
- Danish National Patient Register. Danish Health Data Authority; 1977. Available from https://sundhedsdatastyrelsen.dk/da/english (Accessed September 16, 2021).
- Lynge E, Sandegaard J L, Rebolj M. The Danish National Patient Register. Scand J Public Health 2011; 39: 30-3.
- Schmidt M, Schmidt S A, Sandegaard J L, Ehrenstein V, Pedersen L, Sorensen H T. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 2015; 7: 449-90.
- Statistics Denmark. Available from www.dst.dk/en (Accessed September 16, 2021).
- Danish National Committee on Health Research Ethics. Act on research ethics review of health research projects. [Updated March 18, 2021.] Available from https://en.nvk.dk/ (Accessed September 15, 2021).
- Grovle L, Fjeld O R, Haugen A J, Helgeland J, Smastuen M C, Solberg T K, et al. The erates of LSS surgery in Norwegian Public Hospitals: a threefold increase from 1999 to 2013. Spine (Phila Pa 1976) 2019; 44: E372-E378.
- Machado G C, Maher C G, Ferreira P H, Harris I A, Deyo R A, McKay D, et al. Trends, complications, and costs for hospital admission and surgery for lumbar spinal stenosis. Spine (Phila Pa 1976) 2017; 42: 1737-43.
- Jacobsen S, Sonne-Holm S, Rovsing H, Monrad H, Gebuhr P. Degenerative lumbar spondylolisthesis: an epidemiological perspective: the Copenhagen Osteoarthritis Study. Spine (Phila Pa 1976) 2007; 32: 120-5.
- Lonne G, Fritzell P, Hagg O, Nordvall D, Gerdhem P, Lagerback T, et al. Lumbar spinal stenosis: comparison of surgical practice variation and clinical outcome in three national spine registries. Spine J 2019; 19: 41-9.
- Ghogawala Z, Dziura J, Butler W E, Dai F, Terrin N, Magge S N, et al. Laminectomy plus fusion versus laminectomy alone for lumbar spondylolisthesis. N Engl J Med 2016; 374: 1424-34.
- Forsth P, Michaelsson K, Sanden B. Does fusion improve the outcome after decompressive surgery for lumbar spinal stenosis?: a two-year follow-up study involving 5390 patients. Bone Joint J 2013; 95-B: 960-5.
- Schoenfeld A J, Makanji H, Jiang W, Koehlmoos T, Bono C M, Haider A H. is there variation in procedural utilization for lumbar spine disorders between a fee-for-service and salaried healthcare system? Clin Orthop Relat Res 2017; 475: 2838-44.
- Downie A, Hancock M, Jenkins H, Buchbinder R, Harris I, Underwood M, et al. How common is imaging for low back pain in primary and emergency care? Systematic review and meta-analysis of over 4 million imaging requests across 21 years. Br J Sports Med 2020; 54: 642-51.
- Jacobs J C, Jarvik J G, Chou R, Boothroyd D, Lo J, Nevedal A, et al. Observational study of the downstream consequences of inappropriate MRI of the lumbar spine. J Gen Intern Med 2020; 35: 3605-12.
- Lemmers G P G, van Lankveld W, Westert G P, van der Wees P J, Staal J B. Imaging versus no imaging for low back pain: a systematic review, measuring costs, healthcare utilization and absence from work. Eur Spine J 2019; 28: 937-50.
- Taylor V M, Deyo R A, Cherkin D C, Kreuter W. Low back pain hospitalization: recent United States trends and regional variations. Spine (Phila Pa 1976) 1994; 19: 1207-12.
- Jansson K A, Blomqvist P, Granath F, Nemeth G. Spinal stenosis surgery in Sweden 1987–1999. Eur Spine J 2003; 12: 535-41.
- Burns E M, Rigby E, Mamidanna R, Bottle A, Aylin P, Ziprin P, et al. Systematic review of discharge coding accuracy. J Public Health (Oxf) 2012; 34: 138-48.
- World Health Organization. International classification of diseases. Available from https://www.who.int/classifications/icd/en/ (Accessed September 16, 2021).
- Jensen R K, Kjaer P, Jensen T S, Albert H, Kent P. Degenerative pathways of lumbar motion segments: a comparison in two samples of patients with persistent low back pain. PLoS One 2016; 11: e0146998.
- Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ 2016; 352: h6234.