Orthopedic surgical procedures in 3,305 children and young adults with cerebral palsy: a register-based cohort study
Anna TELLÉUS 1, Nikolaos KIAPEKOS 1,2, Johan VON HEIDEKEN 1,2, Philippe WAGNER 3, Eva BROSTRÖM 1,2, Gunnar HÄGGLUND 4, and Per ÅSTRAND 1,2
1 Department of Women’s and Children’s Health, Karolinska Institutet, Karolinska University Hospital, Stockholm; 2 Department of Pediatric Orthopedics, Astrid Lindgren’s Children Hospital, Karolinska University Hospital, Stockholm; 3 Centre for Clinical Research Västerås, Uppsala University—Region Västmanland, Västerås; 4 Department of Clinical Sciences, Lund, Orthopedics, Lund University, Sweden
Background and purpose — Few reports have described the panorama of orthopedic surgeries that children with cerebral palsy (CP) undergo. We analyzed the risk of a first surgery, and describe the frequency of orthopedic surgeries in terms of age, sex, anatomical location, and Gross Motor Function Classification System (GMFCS) level in children and young adults with CP.
Patients and methods — This was a register-based cohort study of 3,305 individuals followed until 2–25 years of age. We used data from 2 national Swedish registers: the CPUP CP surveillance program and the Swedish National Patient Register. Kaplan–Meier survival curves were calculated to describe the risk of undergoing a first orthopedic surgery, related to age.
Results — We included data for 3,311 orthopedic operations in 1,717 surgical sessions. The percentage of children operated on before age 15 years increased from 22% (95% CI 19–26) for GMFCS level I to 70% (CI 64–75) for level V. Ankle and foot surgery was predominant as first surgery for GMFCS I–II, and hip and femur surgery for GMFCS IV–V. Spinal surgery occurred almost exclusively for GMFCS IV–V. Descriptive data showed repeated surgical sessions to be frequent for higher GMFCS levels.
Interpretation — The risk of having a first orthopedic surgical treatment increased with increasing GMFCS level and was initiated at younger age in children with higher GMFCS level.
Citation: Acta Orthopaedica 2022; 93: 472–477. DOI http://dx.doi.org/10.2340/17453674.2022.2583.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-01-15. Accepted: 2022-04-04. Published: 2022-05-23.
Correspondence: anna.telleus@ki.se
All authors designed the study. AT collected the data and wrote the first draft, which was then actively improved and revised by all authors. Study design: AT, NK, JvH, EB, GH, PÅ. Data collection: AT, JvH, GH, PÅ. Data analysis: PW, AT, NK, PÅ.
Acta thanks Deborah M Eastwood and Freeman Miller for help with peer review of this study.
Cerebral palsy (CP) is the most common neurological disorder causing motor impairment in children and affects about 2–3 per 1,000 children in Sweden (1-3). CP covers a broad range of clinical presentations, and the severity of gross motor function is usually classified according to the Gross Motor Function Classification System (GMFCS) (4,5), a 5-point scale in which level V indicates the greatest disability. The muscular and skeletal deformities secondary to the brain injury in CP can be treated with various forms of orthopedic surgery (6,7). Few reports have described the panorama of orthopedic surgical procedures that children with CP undergo, and they do not provide information for all GMFCS levels and sex distribution (8-11).
In Sweden, the national register for children and adults with CP, Cerebral Pares Uppföljnings Program (CPUP) (https://www.cpup.se), and the National Patient Register (NPR) (https://www.socialstyrelsen.se/en/statistics-and-data/registers/register-information/the-national-patient-register/) provide opportunities for studying the surgical procedures performed in the total population of children and young adults with CP.
We used data from the CPUP and NPR to analyze the risk of a first orthopedic surgical procedure with respect to age, sex, and anatomical distribution, and stratified by GMFCS level. Our hypothesis was that young people with CP with a higher GMFCS level are more likely to be treated with orthopedic surgery than are those with a lower GMFCS level. Another purpose was to describe the scope of orthopedic treatments received by the study cohort during childhood and adolescence.
Participants and methods
Registers and data extracted
The CPUP was initiated in southern Sweden in 1994 as a regional follow-up program for children with CP. In 2001, it was expanded to include all children with CP in Sweden and, since 2011, to include also adults. More than 95% of children with CP in Sweden are followed up in the CPUP (2). The data reported to CPUP includes information on GMFCS level and surgical procedures. From the CPUP, we extracted data on GMFCS level and date of the individual’s last CPUP program visit to a physiotherapist for 3,305 individuals born between 1990 and 2014.
The NPR is maintained by the Swedish National Board of Health and Welfare, and collects information on all inpatient and outpatient contacts from all hospitals in Sweden (12). Inpatient data including sex, date of birth, and date and procedure code for orthopedic surgery for all people with a CP diagnosis (G80) according to the ICD-10 (13) was collected from the NPR for patients seen between January 1, 1997 and December 31, 2015.
Study cohort
The comparison of data between the CPUP and NPR was based on the 10-digit national registration number, which is unique for every Swedish individual. This comparison showed 72 patients in the NPR database (2.0% of the material) with an ICD-10 code for CP (G80) who were not registered in the CPUP. The responsible orthopedic surgeons or neuropediatricians were contacted regarding these 72 patients. The code G80 had been incorrectly assigned for 30, the CP diagnosis could not be verified for 26, and the patients either declined to participate in the CPUP or were lost to the study for the remaining 16. All 72 of these patients were excluded from this study. The study cohort thus comprised 3,305 young people born between 1990 and 2014 whose data could be retrieved from the CPUP and NPR. The age distribution (range 2–25 years) of the cohort at the end of the data collection period in 2015 is shown in Figure 1.

Figure 1. Number of children grouped according to age at the end of data collection period and Gross Motor Function Classification System (GMFCS) level (n = 3,226).
Orthopedic surgical procedure codes and surgical sessions
The procedure codes extracted from the NPR are based on the Swedish version of the NOMESCO Classification of Surgical Procedures (NCSP 96) and have 5 positions comprising 3 letters followed by 2 digits. The 1st letter specifies the organ system, and the 2nd letter specifies 1 of the following anatomical regions: spine, shoulder/upper arm, elbow/lower arm, wrist/hand, pelvis, hip/femur, knee/lower leg, and ankle/foot. The 3rd letter and the 2 digits specify the type of surgery. For example, “NHL69” stands for “tenodesis or tendon lengthening/shortening at the ankle/foot.” Bilateral procedures were counted as 2 separate procedures and were reported by either 2 identical N-codes or by 1 N-code together with the code “ZXA10,” signifying a bilateral procedure. Unless the data contained clear documentation of bilateral surgery, we assumed that it was unilateral. Procedure codes were collected for the period January 1, 1997 to December 31, 2015. Before 1997, a different coding system was used, which made comparisons with the present material difficult. Therefore, in the oldest 6% of the cohort (those born in 1990–1994, i.e., aged 21–25 years at the end of the study, see Figure 1), the procedure codes for orthopedic surgeries of these patients at 3–6 years of age were not included.
Specific performance dates were lacking for 151 surgical procedure codes (4.6%). These undated procedure codes were assumed to represent (part of) a separate surgical session (SS) and were included, unless there was an identical procedure code with a specified performance date given. In the latter case, the undated procedure code was considered redundant and was excluded from further analysis.
The risk of a first surgical procedure was analyzed, and the frequency of procedures was described with reference to age, sex, and anatomical distribution, and stratified according to GMFCS level. In 79 patients (2.4%), no GMFCS level had been reported to the CPUP, and these were defined as “unclassified” (Tables 1–3).
| GMFCS level | Total study population | Number of children operated on (%) | Number of SSs (% of total) | SSs/100 patients | Mean number SSs/operated patient (range) |
| I | 1,457 | 203 (14) | 302 (18) | 21 | 1.5 (1–6) |
| II | 527 | 115 (22) | 210 (12) | 40 | 1.8 (1–6) |
| III | 287 | 67 (23) | 119 (7) | 41 | 1.8 (1–7) |
| IV | 445 | 155 (35) | 331 (19) | 74 | 2.1 (1–9) |
| V | 510 | 271 (53) | 716 (42) | 141 | 2.6 (1–11) |
| Unclassified | 79 | 19 (24) | 39 (2) | 49 | 2.1 (1–6) |
| Total | 3,305 | 830 (25) | 1,717 | 52 | 2.0 (1–11) |
| The table is designed to facilitate comparison with Valentine et al. (11). | |||||
| GMFCS: Gross Motor Function Classification System; | |||||
| SS: surgical session. | |||||
Statistics
Descriptive statistics such as count, proportion, and mean (range) were used together with the number of surgeries per child for different GMFCS levels, the total number at different anatomical locations, and the most common type and location in order to characterize the sample.
Kaplan–Meier survival curves with 95% confidence intervals (CI), with the first orthopedic surgery of a specific type, and of any type, as endpoints, were calculated to show the proportion of patients who underwent orthopedic surgical procedures at a given age. For this analysis, children were followed from birth until their last CPUP program visit to the physical therapist, a first surgery or to the end of the study, i.e., December 31, 2015. The curves were analyzed sepa-rately with regard to sex, anatomical location, and GMFCS level. The logrank test was used to test differences between groups. A p-value less than 0.05 was considered statistically significant. STATA (version 14; StataCorp, College Station, TX, USA) were used for statistical analyses.
Ethics, funding, and potential conflicts of interest
Ethical approval was obtained from the Regional Ethical Review Board in Lund (DNR 2015/159). Verbal consent to use the data for research was provided by all families participating in the CPUP. This work was supported by the following research funds: Stiftelsen Promobilia, Norrbacka-Eugeniastiftelsen, Sunnerdahls Handikappfond, Linnéa och Josef Carlssons stiftelse, and Stiftelsen för bistånd åt rörelsehindrade i Skåne. The authors declare no conflicts of interest.
Results
Demographics
3,311 orthopedic surgical procedures were performed in 830 (25%) of the 3,305 included patients (Table 1). More than 1 surgical procedure was often performed during the same SS. The mean number of SSs per 100 children increased-with increasing GMFCS level and numbers of SSs per operated child increased from 1.5 (1–6) for GMFCS level I to 2.6 (1–11) for GMFCS level V (Table 2).
Age at surgery (Figure 2)
The proportion of children operated on for the first time started to increase at 3–4 years of age and appeared to level out after 15 years. No significant sex difference was found (p = 0.3). The proportion of children operated on by age 15 years increased from 22% (CI 19–26) for GMFCS I to 70% (CI 64–75) for GMFCS V. Surgical treatment started at a younger age in the children with a higher GMFCS level (p < 0.001).
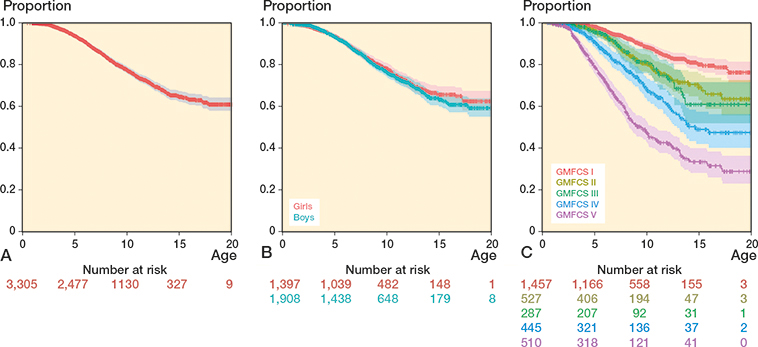
Figure 2. Kaplan–Meier survivorship curves with 95% confidence intervals with first orthopedic surgery as the endpoint for (A) the entire material, (B) according to sex and (C) according to Gross Motor Function Classification System (GMFCS) level.
GMFCS level and anatomical location of surgery
The anatomical locations of the 3,311 orthopedic surgical procedures according to GMFCS level are shown in Table 3, and locations of the most common operations in different age groups according to GMFCS level in Table 4. Overall, the most frequent procedure was “myo- or tenotomy at the hip/thigh” (NFL39), which was reported 453 times (14%), followed by “tenodesis or tendon lengthening/shortening at the ankle/foot” (NHL69), (348 times [11%]), and “angulating, rotational or displacing osteotomy of the femur” (NFK59), (342 times [11%]).
For patients with GMFCS level I or II, surgeries at the ankle/foot level were most common in all age groups. At age 15 years, 16% of the children in GMFCS I and 32% in GMFCS II had had ankle/foot surgery. Spinal surgery was rarely performed in patients with GMFCS level I or II (Figure 3). Descriptive data also showed that upper extremity surgery was more frequent in GMFCS level I and II compared with other GMFCS levels but represented approximately 11% of all operations (Table 3).
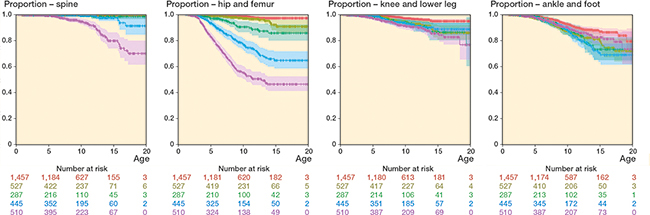
Figure 3. Kaplan–Meier curves with 95% confidence intervals with first orthopedic surgery as the endpoint for different Gross Motor Function Classification System levels in the following regions: spine, hip and femur, knee and lower leg, and ankle and foot. For color codes see Figure 2C.
In patients with GMFCS level III, hip/femur surgery was most frequent in the younger age groups, whereas ankle/foot surgery became more common in the older age groups. By age 15 years, 15% had had hip/femur surgery and 31% ankle/foot surgery.
In patients with GMFCS level IV or V, surgeries at the hip/femur were most common in children up to age 12 years. Hip surgery occurred at younger ages and became gradually more frequent in those with GMFCS level IV or V. About 25% of the children with GMFCS level V had hip surgery before age 5 years, and approximately 50% had had 1 or more hip/femur surgeries by age 12 years (Figure 3). After age 12 years, skeletal surgery in the ankle/foot became more frequent in patients with GMFCS level IV and spinal surgery became far more common in those with GMFCS level V (Figure 3). The percentages of patients undergoing surgery of the lower leg/knee and foot/ankle (Figure 3) were more similar in all GMFCS levels with regard to age, as compared with the situation in the spine and hip/femur.
Discussion
Our main finding was that the proportion of children undergoing orthopedic surgery before the age of 15 increased from 22% in GMFCS level I to 70% in level V, but did not differ between boys and girls. In GMFCS levels I–II, ankle–foot surgery was the most common first surgery while hip and spine surgery was most common in GMFCS levels IV–V.
A population-based study of botulinum toxin treatment and lower limb surgery in 771 children born in 2000–2009 (aged 8–17 years) in Western Australia also reported a higher number of operations with higher GMFCS levels (11). The Kaplan–Meier survival curves in our study, even if they also included surgery on the upper extremity, spine, and pelvis, show that the proportions of children having had surgery for the different GMFCS levels appear largely to agree. Though comparisons are complicated by differing distributions of age at end of follow-up between the cohorts, our descriptive data on mean number of surgeries per child were also within 20% of those reported by Valentine et al. for all GMFCS levels, and were highest in patients with GMFCS level V (11). A Danish population-based questionnaire study also reported higher orthopedic surgery rates in patients with higher GMFCS levels (8), although GMFCS levels III to V were not analyzed separately in that study.
By contrast, 2 retrospective studies based on reviews of medical records found that the mean number of surgeries did not increase statistically significantly with higher GMFCS level after level I (9,10). However, the study by Yu et al. (9) did not include children with GMFCS level V or those with hemiplegia who had isolated Achilles tendon-lengthening surgery. In both these studies, the 3 most frequent procedures were hip adductor tenotomy, hamstring lengthening, and lower leg soft tissue surgery. In our study, descriptive data showed that the most frequent procedures were also soft tissue surgeries at the hip/femur and foot/ankle levels, although the register data allowed no differentiation between some procedures such as the lengthening of the tibialis posterior or the Achilles tendon. None of the above studies provided information on sex differences; however, in our analysis the proportion of girls and boys undergoing orthopedic surgery was similar with regard to age.
The orthopedic surgical panorama we describe should be interpreted with the main goals of CPUP in mind, i.e., to prevent hip dislocation and to prevent severe contractures. With the CPUP program the rate of hip dislocations is below 1% in all children with CP in Sweden (14). In this study 38% of all surgeries involved hip and pelvic procedures in children with GMFCS level IV or V, and surgical treatment started at age 2–3 years, when the risk of hip migration increases in the most affected children (15,16). This probably reflects the proportion of children exposed to surgery needed to maintain the low rate of hip dislocations in Sweden. Regarding prevention of contractures, the availability and use of alternative treatment modalities such as, e.g., physiotherapy, orthoses, serial casting, and Botulinum toxin A injections is likely to influence the rate of orthopedic surgeries (17). Therefore, comparisons or extrapolation to other cohorts is complex.
Spinal surgery was performed almost exclusively in children with GMFCS level IV or V. Although a recent population-based study provided data for the incidence of scoliosis in children with CP (18), to our knowledge no previous studies have reported on the timing of surgery. In contrast to the situation in the hip and spine, the percentages of young people who had surgery in the lower leg and foot/ankle regions were more similar across the different GMFCS levels with regard to age.
In the later teens the proportion of those undergoing a first orthopedic surgical procedure did not increase. It seems likely that when longitudinal growth stops, one of the driving forces for development of soft tissue contractures disappears. Another contributing factor is that impairment, for example regarding the hip, has been addressed at a younger age.
Sweden is a country with state-funded medicine and surgery, and other treatment modalities are accessible and equitable for children with CP. We can only speculate, but most children and young adults in our study cohort probably received the surgery the patient, the family, and the treating doctor thought necessary.
Strengths and limitations
One main limitation of our study concerns possible misclassification and missing data on surgical procedures. However, it was not within the scope of this study to compare register data with data from medical records. Moreover, the quality of the NPR has been systematically reviewed and the accuracy of the coding is reported to be high and the underreporting is low (12). Another limitation concerns missing data for GMFCS level (2.4%) and date of surgery (4.6%), and the potential for missing data on bilateral surgeries. An incompatible classification of surgical procedure codes was used before 1997, and procedure codes for the first 3–6 years of age are lacking in the oldest 6% of the study cohort (the age group born 1990–1994, see Figure 1). We estimate that in this 6% of the cohort, at most 10–15% of all surgical procedure codes were missing. These individuals were included in the study because information regarding orthopedic surgery in younger adults with CP is scarce in the literature.
Our Kaplan–Meier survival curves do not reflect the total frequency of orthopedic surgeries in the study cohort, as they illustrate only variation in risk of a first surgery with age, and repeated orthopedic surgeries performed on the same person are not accounted for. Consequently, we also chose to present a crude summary of the total number of surgeries performed in the cohort and on average in each child. Thus, Tables 2–4 characterize the surgical load the children were exposed to, but do not account for end-of-study censoring, differences in in mortality rates between GMFCS levels, and variation in the risk of surgery with age. Figure 1 clearly illustrates that a proportion of children may not have reached an age where surgery is deemed suitable. This has likely resulted in underestimation of the expected number of surgeries of different types, in total and for each child.
Many factors make comparisons of our results with other populations of young people with CP complex. For example, indications for and classifications of orthopedic surgical procedures may vary locally, regionally, nationally, and over time.
Strengths of our study are the size of the population included and the concordance of data from 2 national registers for the population-based study cohort. It seems reasonable to assume that this cohort closely represents the population of children and young adults with CP in Sweden, and orthopedic surgery during the study period. Moreover, the Kaplan–Meier analyses and the large number of orthopedic surgical procedures allowed us to analyze the data with respect to age, sex, anatomical distribution, and GMFCS level. Stratifying the material by GMFCS level provides information for patients and families on the timing and likelihood of different orthopedic surgical procedures that may become recommended during childhood and adolescence. This information may also be of value for professionals and administrators responsible for planning of resources for orthopedic surgery.
In conclusion, the proportion of young people receiving orthopedic surgery increased with increasing difficulties in ambulation. In children and adolescents capable of walking without limitations (GMFCS I), about 1/5 had had surgery before age 15 years, typically a lower leg or foot operation such as heel cord lengthening. In children who needed support for walking (GMFCS level II or III), the same type of surgery was performed in up to 1/3 of the children. In children who use a wheelchair for ambulation (GMFCS level IV or V), hip and spine surgery was performed more frequently. About 25% of the children in GMFCS level V had hip surgery before age 5 years, and about half had it before age 12 years.
- Himmelmann K. Putting prevention into practice for the benefit of children and young people with cerebral palsy. Arch Dis Child 2018; 103: 1100.
- Westbom L, Hägglund G, Nordmark E. Cerebral palsy in a total population of 4–11 year olds in southern Sweden. Prevalence and distribution according to different CP classification systems. BMC Pediatrics 2007; 7: 41.
- Hollung S J, Hägglund G, Gaston M S, Seid A K, Lydersen S, Alriksson-Schmidt A I, et al. Point prevalence and motor function of children and adolescents with cerebral palsy in Scandinavia and Scotland: a CP-North study. Dev Med Child Neurol 2021; 10.1111/dmcn.14764.
- Rosenbaum P L, Palisano R J, Bartlett D J, Galuppi B E, Russell D J. Development of the Gross Motor Function Classification System for cerebral palsy. Dev Med Child Neurol 2008; 50: 249-53.
- Palisano R J, Rosenbaum P, Bartlett D, Livingston M H. Content validity of the expanded and revised Gross Motor Function Classification System. Dev Med Child Neurol 2008; 50: 744-50.
- Aversano M W, Sheikh Taha A M, Mundluru S, Otsuka N Y. What’s new in the orthopaedic treatment of cerebral palsy. J Pediatr Orthop 2017; 37: 210-16.
- Blumetti F C, Wu J C N, Barzi F, Axt M W, Waugh M C, Selber P. Orthopaedic surgery in dystonic cerebral palsy. J Pediatr Orthop 2019; 39: 209-16.
- Rackauskaite G, Uldall P W, Bech B H, Ostergaard J R. Management of cerebral palsy varies by healthcare region. Dan Med J 2015; 62: A5152.
- Yu S, Rethlefsen S A, Wren T A, Kay R M. Long-term ambulatory change after lower extremity orthopaedic surgery in children with cerebral palsy: a retrospective review. J Pediatr Orthop 2015; 35: 285-9.
- Rehbein I, Teske V, Pagano I, Cuneo A, Perez M E, von Heideken J. Analysis of orthopedic surgical procedures in children with cerebral palsy. World J Orthop 2020; 11: 222-31.
- Valentine J, Davidson S A, Bear N, Blair E, Ward R, Thornton A, et al. Botulinum toxin and surgical intervention in children and adolescents with cerebral palsy: who, when and why do we treat? Disabil Rehabil 2021; 43(7): 936-43.
- Ludvigsson J F, Andersson E, Ekbom A, Feychting M, Kim J L, Reuterwall C, et al. External review and validation of the Swedish national inpatient register. BMC Public Health 2011; 11: 450.
- Park H, Castano J, Avila P, Perez D, Berinsky H, Gambarte L, et al. An information retrieval approach to ICD-10 classification. Stud Health Technol Inform 2019; 264: 1564-5.
- Hägglund G, Alriksson-Schmidt A, Lauge-Pedersen H, Rodby-Bousquet E, Wagner P, Westbom L. Prevention of dislocation of the hip in children with cerebral palsy: 20-year results of a population-based prevention programme. Bone Joint J 2014; 96-B: 1546-52.
- Hägglund G, Lauge-Pedersen H, Wagner P. Characteristics of children with hip displacement in cerebral palsy. BMC Musculoskelet Disord 2007; 8: 101.
- Hägglund G, Andersson S, Duppe H, Lauge-Pedersen H, Nordmark E, Westbom L. Prevention of dislocation of the hip in children with cerebral palsy: the first ten years of a population-based prevention programme. J Bone Joint Surg Br 2005; 87: 95-101.
- Novak I, Morgan C, Fahey M, Finch-Edmondson M, Galea C, Hines A, et al. State of the evidence traffic lights 2019: systematic review of interventions for preventing and treating children with cerebral palsy. Curr Neurol Neurosci Rep 2020; 20: 3.
- Hägglund G, Pettersson K, Czuba T, Persson-Bunke M, Rodby-Bousquet E. Incidence of scoliosis in cerebral palsy. Acta Orthop 2018; 89: 443-7.