Median 10-year whole blood metal ion levels and clinical outcome of ReCap-M2a-Magnum metal-on-metal total hip arthroplasty
Sakari PIETILÄINEN 1–3, Axel LINNOVAARA 3, Mikko S VENÄLÄINEN 4,5, Heikki MÄNTYMÄKI 6, Inari LAAKSONEN 1,2, Petteri LANKINEN 1,2,7, and Keijo T MÄKELÄ 1,2
1 Department of Orthopaedics and Traumatology, Turku University Hospital; 2 University of Turku; 3 Department of Orthopaedics and Traumatology, Vaasa Central Hospital; 4 Turku Bioscience Centre, University of Turku and Åbo Akademi University; 5 Turku University Hospital, Division of Medical Imaging, Department of Medical Physics, Turku; 6 Department of Orthopaedics, Tampere University Hospital, Tampere; 7 Satasairaala Central Hospital, Satakunta Hospital District, Pori, Finland
Background and purpose — We have previously reported that the whole blood (WB) chromium (Cr) and cobalt (Co) ion levels decrease in the short term after ReCap-M2a-Magnum large-diameter head (LDH) metal-on-metal (MoM) total hip arthroplasty (THA). This study reports long-term metal ion levels and clinical outcomes after ReCap-Magnum THA.
Patients and methods — ReCap-M2a-Magnum LDH THA was used in 1,450 patients in our hospital district from 2005 to 2012. Median follow-up time was 10 years. 991 patients had 2 or more metal ion measurements. The median measurement interval was 4 years. Individual metal ion change was assessed using logarithmic metal ion values in a random coefficient model. Kaplan–Meier survival estimates were calculated for revision surgery for any reason for revision, and separately for metal-related adverse events (metal ions above safe upper limit [SUL], revision due to ARMD, or pseudotumor).
Results — Geometric mean of Cr decreased from 1.8 ppb (geometric standard deviation [GSD] 1.8) to 1.0 ppb (GSD 2.8, p < 0.001). The Co levels decreased from 1.7 ppb (GSD 2.4) to 1.4 ppb (GSD 2.8, p < 0.001). The hip-specific survival was 85% for revision due to any reason at 14 years and the hip-specific survival for any metal-related adverse event was 69% at 14 years.
Interpretation — WB Cr and Co levels continued to decrease in the long-term follow-up of ReCap-M2a-Magnum THA patients. The amount of metal-related adverse events was rather high, but revision surgery was seldom required. We suggest that after 10 years from the implantation a 5-year measurement interval may be sufficient for asymptomatic ReCap-M2a-Magnum patients.
Citation: Acta Orthopaedica 2022; 93: 444–450. DOI http://dx.doi.org/10.2340/17453674.2022.2510.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-01-25. Accepted: 2022-04-04. Published: 2022-04-19.
Correspondence: Correspondence: sakari.pietilainen@gmail.com
KTM, MV, and SP designed the study protocol and methods. KTM organized the systematic screening. MV analyzed the data and performed the statistics. All authors contributed to the writing and revision of the manuscript.
The authors would like to thank Mari Järvinen, registered nurse, for managing the MoM Hip Arthroplasty follow-up in Turku University Hospital.
Acta thanks Jean Alain Epinette and Alexander Oxblom for help with peer review of this study.
In well-functioning metal-on-metal (MoM) total hip arthroplasty (THA), patients’ whole blood (WB) chromium (Cr) and cobalt (Co) metal ion levels peak in the first years after the implantation and usually decrease thereafter (1). Data concerning long-term metal ion changes in MoM THA patients is scarce (2). Most MoM THAs have been performed over a decade ago, and many patients are doing relatively well without the need for revision surgery (3). The follow-up of these patients is important to recognise the failing implants, and also to identify and prevent systemic cobalt toxicity. Additionally, the long-term follow-up guidelines need to be updated to optimize the usage of limited healthcare resources (1,4,5).
ReCap-M2a-Magnum (ZimmerBiomet, Warsaw, IN, USA) large-diameter head (LDH) MoM THA was commonly used in Finland from 2005 to 2012 (6). In our previous reports regarding both unilateral and bilateral ReCap-M2a-Magnum LDH MOM THA patients in Turku University Hospital, 2.5% of the hips required a revision operation due to adverse reaction to metal debris (ARMD) and 12% had a definite ARMD, but revision was not performed during follow-up of 5 years. The WB Cr and Co ion levels decreased, and stayed mostly below the safe upper limit (SUL) if the initial values were low (7-9). SUL value describes the edge of acceptable metal ion levels, but there is no universally accepted SUL value for all MoM implants and normal metal ion levels do not exclude ARMD. Bosker et al. found a 4 times higher incidence of ARMD in ReCap-M2a-Magnum THA patients with metal ion levels above 5 ppb (10,11). High cobalt levels can cause pathological effects, such as cardiomyopathy, thyroid, hepatic, and hematology disorders, and neurological symptoms. High Cr levels can be both carcinogenetic and genotoxic (1). In the current study the ReCap-M2a-Magnum acetabular component and femoral head were paired with either uncemented Bi-Metric or Reach stems (ZimmerBiomet, Warsaw, IN, USA). Measurement interval, i.e., the time between the first and last metal ion measurement, was 2 years in our previous publications. We have previously stated that based on the Turku University Hospital data at the mean follow-up time of 5.2 years, 14.3 % of all ReCap-M2a-Magnum hips exhibited adverse reaction to metal debris (9).
This study analyzed metal ion levels of ReCap-M2a-Magnum LDH MoM THA patients’ change in the long term. We also assessed the clinical and imaging outcomes after ReCap-M2a-Magnum THA, and risk factors for revision surgery.
Patients and methods
We performed a retrospective cohort study to determine WB Cr and Co ion level changes in the long term. We have now analyzed WB Cr and Co ion level data in the Hospital District of Southwest Finland level with median follow-up of 10 years. We have also assessed the clinical outcome of ReCap-M2a-Magnum patients. All patients who had ReCap-M2a-Magnum LDH MOM THA from the Hospital District of Southwest Finland database from August 2005 to April 2012 were included. The patients were followed until revision surgery, death, or by the end of 2019. Patients with a unilateral Recap-M2a-Magnum THA and a different brand of MoM THA implant on the contralateral side were excluded from the analyses. A screening program for all MoM THA patients was started in 2012 at our institution.
We used previously established SUL values of 4.6 ppb for Cr and of 4.0 ppb for Co for unilateral implants, and 7.4 ppb for Cr and 5.0ppb for Co for bilateral implants (10). Patients with Co or Cr ions above 5 ppb or poor functional outcome in Oxford Hip Score (OHS) questionnaire were scheduled to MARS-MRI. The inclination angle of the cup was measured from straight anteroposterior pelvis radiographs, and the angle between ischial tuberosities and cup ring was measured. Further, the anteversion of the cup was assessed from lateral shoot-through radiographs measuring the angle between horizontal image plane and cup rim. Measurements were performed using the angle measurement tool of Carestream Vue PACS software (www.carestream.com/en/ca/). The details of this screening program have been explained in our previous publications (9,12,13). Data was obtained from the Hospital District of Southwest Finland data pool and electronic medical records. MARS-MRI images were performed in Turku University Hospital and were assessed by a radiologist consultant experienced in ARMD related pathologies. Pseudotumors were graded using the previously described classification system by Hart et al. (14).
Patients
1,450 patients (1,624 hips) were included in this study (Figure 1). 174 patients had bilateral ReCap-M2a-Magnum THA. 1,412 patients (1585 hips) had a Bimetric femoral stem while 38 patients (39 hips) had a Reach stem.
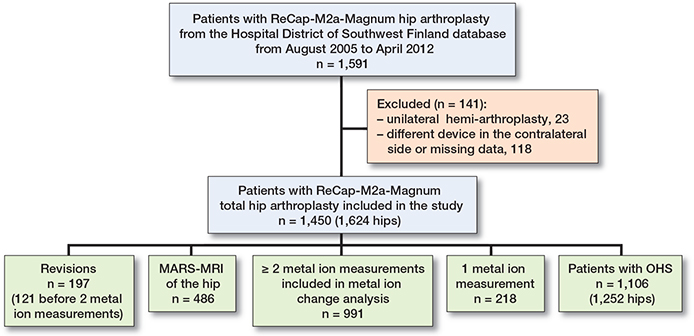
Figure 1. Flowchart demonstrating the inclusion criteria.
The median follow-up time for unilateral hips was 10 years (0.6–14) and 11 years (1–14) for bilateral hip implants. 313 patients died during follow-up. Median age of the patients was 65 years (interquartile range [IQR] 12), and 683 (47%) patients were male (Table 1)
We identified 991 patients with at least 2 WB metal ion measurements and evaluated the change between the first and the last measurement. The median time interval from THA to the index metal ion measurement was 5 years (0.5–11). The median time between the initial and the last metal ion measurement was considered as the measurement interval. The individual measurement time points with respect to the (later) THA operation are shown in Figure 2.
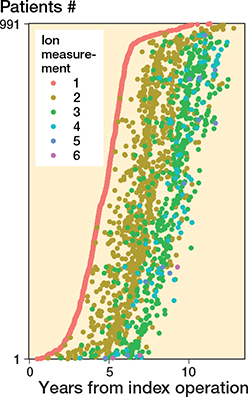
Figure 2. Individual metal ion measurement time points.
1,106 patients had completed a postoperative OHS questionnaire for 1,252 hips. Preoperative OHS scores were not available. Concerning radiographic data, 2 patients (3 hips) did not have anteversion angle data and 84 patients (87 hips) did not have inclination angle data due to missing radiographs.
486 patients (563 THA) had undergone MARS-MRI imaging of the hip, of which 161 hips had had more than 1 MARS-MRI imaging sessions.
Statistics
We used a random coefficient model to assess the individual change between repeated metal ion levels. Due to the positively skewed distribution of metal ion levels, metal ion levels were log transformed in conditional models. The individual change in metal ion levels was presented with spaghetti plots for natural log transformed metal ion values (Figure 3). We used medians with interquartile range (IQR) and geometric means with geometric standard deviation (GSD) were used at both the initial and control measurements for improved interpretability. McNemar’s test was used to determine differences in proportions of patients with metal ion levels above the SUL between the first and the last measurements.
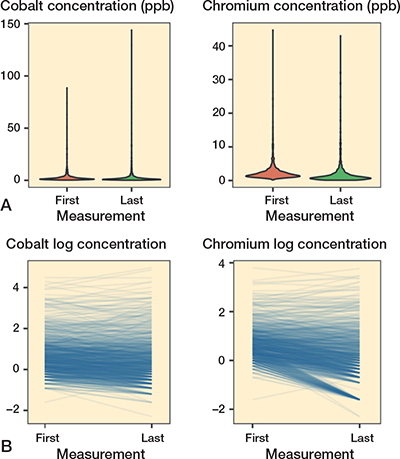
Figure 3. A. Violin plots demonstrating the skewedness of metal ion values. B. Spaghetti plots for individual chromium and cobalt ion levels.
The overall survivorship for unilateral and bilateral ReCap-M2a-Magnum THA implants with 95% confidence intervals (CI) was calculated using the Kaplan–Meier estimator (revision surgery for any reason as the endpoint). Additionally, separate Kaplan–Meier analysis (with CI) was performed to assess the survivorship of ReCap-M2a-Magnum THA in terms of metal-related adverse events (metal ions above SUL, revision due to ARMD, pseudotumor visible in MARS-MRI) as endpoint. Regarding this metal-related adverse event analysis, the hips that were revised for reasons other than ARMD previously were censored at the time of revision. Kaplan–Meier analyses were hip-specific considering both implants from bilateral patients.
We manually checked all revisions from the electronic medical records of Hospital District of Southwest Finland. Metal ion measurements that were taken after revision were excluded, also in bilateral patients, unless the THA had the same bearing surface after the revision, as in many periprosthetic femoral fracture revisions. In these patients, metal ion measurements after revision were included in metal ion level analysis.
A directed acyclic graph (DAG) was constructed under these assumptions:
- Metal-related adverse events and revision surgery are dependent on age, sex, bilateral surgery, anteversion angle, inclination angle, and head diameter.
- Bilateral surgery is dependent on age, as both hips are not as commonly operated on in older patients.
- Head diameter is dependent on sex, as head diameter is on average larger in men.
We used Cox proportional hazards (PH) regression analysis to estimate hazard ratios (HR) and their CI for each potential risk factor for metal-related adverse events and revision surgery. As suggested by the DAG analysis (Figure 4), the HR for head diameter was adjusted for confounding from sex whereas the estimates for other variables remained unadjusted. PH assumption for all Cox analyses was evaluated with visual inspection of Kaplan–Meier plots, and using a statistical analysis based on weighted Schoenfeld residuals. The HR estimates for metal-related events in different age groups showed minor violation of the PH assumption but the estimates were left as is, without dividing follow-up time into intervals, after inspection of corresponding Kaplan–Meier survival plots. All Cox PH models were stratified by THA brand.
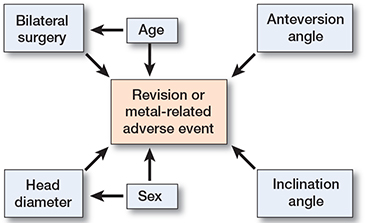
Figure 4. DAG demonstrating the direct causal effects of hip characteristics.
A p-value of less than 0.05 was considered to be statistically significant. R statistical computing environment version 4.0.3 was used to execute data analysis (15). We used R packages ggplot2 (version 3.3.3) and survival (version 3.2-10) for visualizations and survival analysis.
Ethics, funding, and potential conflicts of interest
This study was based on the national recommendations for MoM THA patient screening in Finland. Study data was gathered from register and electronic patient records. Patients were not contacted directly. For these reasons approval by the local ethical committee was not required. Data sharing is not possible. SP reports funding from Turku University and MSV has received funding from the Academy of Finland (grant no. 322123). AL, HM, IL, PL, and KTM have nothing to disclose.
Results
The geometric mean of WB Cr decreased from 1.8 ppb (GSD 1.8) to 1.0 ppb (GSD 2.8, p < 0.001) and the geometric mean of Co decreased from 1.7 ppb (GSD = 2.4) to 1.4 ppb (GSD 2.8, p < 0.001) in unilateral ReCap-M2a-Magnum patients. In bilateral patients WB Cr decreased from 2.9 ppb (GSD 1.9) to 1.7 ppb (GSD 2.4, p < 0.001) and WB Co decreased from 3.1 ppb (GSD 2.2) to 2.4 ppb (GSD 2.5, p < 0.001). The median measurement interval was 4 years (IQR 1.6) in unilateral patients and 4 years (IQR 1.9) in bilateral patients. Metal ion changes with p-values are given in Table 2.
In the whole cohort, 74 (7%) patients had Cr levels above the SUL and 135 (14%) patients had Co levels above the SUL in the first metal ion measurement, while 72 (7%) patients had their Cr levels above the SUL and 135 (14%) patients had their Co levels above the SUL in the last metal ion measurement. The proportion of patients above the SUL did not change during the follow-up. In unilateral patients, only 63 (7%) had a Cr value above the SUL in the first measurement while 62 (7%) had Cr values above the SUL in the last measurement. 110 (13%) unilateral patients had their Co value above the SUL in the first measurement and 115 (13%) had Co above the SUL in the last measurement (p = 0.6). In bilateral patients, 11 (8%) had Cr above the SUL in the first measurement and 10 (8%) had a Cr value above the SUL in the last measurement. 25 (19%) bilateral patients had Co above the SUL in the first measurement and 20 (15%) had Co above the SUL in the last measurement (p = 0.3). Individual metal ion change is demonstrated in Figure 2.
The combined implant survival for ReCap-M2a-Magnum THA with revision for any reason as the endpoint was 88% (CI 86–89) at 10 years and 85% (CI 83–88) at 14 years. For unilateral implants specifically, the 14-year survival was 85% (CI 83–88) and for bilateral implants it was almost similar, 86% (CI 81–90) at 14 years. The total number of revised hips during the follow-up time was 197 (12% of all hips), of which 121 were revised before two blood metal ion measurements. ARMD was the reason for revision in 100 hips (6% of all hips, 50% of revisions). Median time for revision due to ARMD was 6.4 years (IQR 3.2), infection 1.6 years (IQR 3.2), and for any other reason 0.8 years (IQR 5.0) from the implantation.
Kaplan–Meier results for implant survival for any reason of revision are presented in Figure 5, and reasons for revision in Table 3.
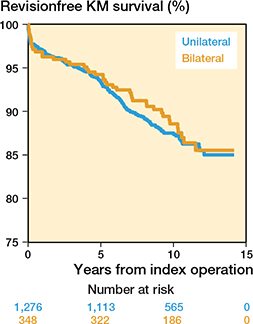
Figure 5. Kaplan–Meier curve for unilateral and bilateral implants separately with revision due to any reason as endpoint.
The 14-year survival for metal-related adverse events (pseudotumor, metal ions above the SUL, or revision due to ARMD) was 69% (CI 65–73) for unilateral implants and 60% (CI 55–67) for bilateral implants. The number of metal-related adverse events was 433 (314 unilateral and 118 bilateral hips). Kaplan–Meier survival curves are shown in Figure 6.
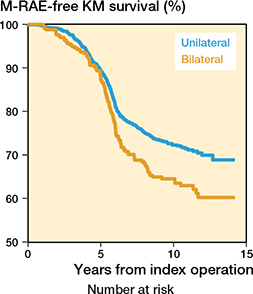
Figure 6. Kaplan–Meier estimates for unilateral and bilateral implants, with metal-related adverse events (M-RAE) as endpoints.
In Cox proportional hazards regression analysis, cup retroversion (HR 3.5, p < 0.001), inclination angle above 50 degrees (HR 2.2, p < 0.001), and female sex (HR 1.9, p < 0.001) were associated with higher risk of revision in unilateral patients. Furthermore, retroversion of the cup (HR 2.3, p = 0.006) was associated with a higher risk of metal-related adverse events. Femoral head diameter of 46–52 mm was associated with better implant survival as compared with head diameter of > 52 mm (HR 0.5, p = 0.004). Female sex (HR 1.8, p < 0.001) was associated with a higher risk of metalrelated adverse events in unilateral patients. Cox regression analysis data is given in Tables 4 and 5.
| Unilateral patients | Bilateral patients | |||
| HR (95% CI) | p-value | HR (95% CI) | p-value | |
| Age (ref. < 60) | ||||
| 60–69 | 0.9 (0.6–1.3) | 0.6 | 1.2 (0.6–2.3) | 0.7 |
| ≥ 70 | 1.0 (0.7–1.5) | 0.9 | 1.3 (0.6–2.1) | 0.5 |
| Sex (ref. male) | ||||
| Female | 1.9 (1.4–2.7) | < 0.001 | 1.3 (0.7–2.3) | 0.4 |
| Inclination angle (ref. 30–49°) | ||||
| < 30° | 0.5 (0.1–2.1) | 0.4 | 3.6 (0.9–15) | 0.08 |
| ≥ 50° | 2.2 (1.5–3.2) | < 0.001 | 0.9 (0.4–2.2) | 0.8 |
| Anteversion angle (ref. > 0°) | ||||
| ≤ 0° | 3.5 (1.9–6.6) | < 0.001 | 2.1 (0.5–8.7) | 0.3 |
| Head diameter, mm (ref. > 52) | ||||
| 46–52 | 0.5 (0.3–0.8) | 0.004 | 1.0 (0.4–2.6) | 1.0 |
| < 46 | 0.8 (0.4–1.4) | 0.4 | 2.3 (0.7–7.8) | 0.2 |
| For footnotes, see Table 4. | ||||
Of the 563 THAs with MARS-MRI there was a pseudotumor in 338 hips (60%, 21% of all hips), and in 225 (40%) THAs the MRI was considered normal. Hart 1 pseudotumor was diagnosed in 132 THAs, Hart 2A pseudotumor in 71 THAs, and Hart 2B was seen in 107 THAs. Solid Hart 3 pseudotumor was identified in 28 hips.
In addition to this, we evaluated 161 hips with repeated MARS-MRI imaging. 39 patients did undergo 3 MARS-MRI imaging sessions and 6 patients had 4 MARS-MRI. Of these, 66 patients had normal initial MARS-MRI and 46 of these were normal in the repeated imaging. There was a new pseudotumor in 20 hips that had normal initial MRI. In 14 hips with initially diagnosed pseudotumor, the repeated MARS-MRI was considered normal. 11 were Hart 1 pseudotumors, 2 were Hart 2A pseudotumors, and 1 was Hart 2B pseudotumor. 47 hips with pseudotumors were evaluated to be similar in size and grade in the repeated MRI. In 10 hips the pseudotumor was smaller in the repeated MARS-MRI. However, in 24 hips the pseudotumor had increased in size and in 4 of these the grade of the pseudotumor had also increased.
We reviewed postoperative OHS questionnaire data regarding 1,252 hips. Median OHS score was 43 (excellent outcome) and mean was 40 (good outcome). The majority, 729 (58%), of hips had excellent functional outcome, while 228 (18%) hips had a good patient-reported outcome. Further, 136 (11%) hips had a moderate functional outcome and 159 (13%) hips had a poor functional outcome.
Discussion
We found that WB Cr and Co levels decreased during median 10-year follow-up. 14-year survival was 85% for any reason for revision, and 69% for metal-related adverse events.
Our previous mid-term metal ion report was based on 319 unilateral ReCap-Magnum patients who were operated on in Turku University Hospital with a mean follow-up time of 7 years. A decrease in both WB Cr and Co ion levels with time was noted. Metal ion levels stayed mostly below the SUL if the values were initially low. The same trend was seen in 61 bilateral ReCap-Magnum patients with repeated measurements (7,8).
In the current study we have included all ReCap-M2a-Magnum THA patients operated on in the Hospital District of Southwest Finland. 859 unilateral and 132 bilateral ReCap-Magnum patients with at least 2 metal ion level measurements and a median follow-up of 10 years demonstrated a decreasing trend in WB metal ion levels. Compared with the previous studies, our results demonstrate that the decrease in WB Cr and Co ion levels continues further in long-term follow-up (7,8). The number of patients with metal ion levels above the SUL did not increase during this longer follow-up period either. This is the largest study of repeated WB Cr and Co ion measurements of ReCap-Magnum THA patients that we are aware of.
The decreasing trend of metal-ion levels in well-functioning MoM hip patients has been reported also in other studies (12,16,17). In some implants a longer “run-in” phase, or phase of elevated metal ion release, has been observed. Sangaletti et al. found an increase of Co but not Cr ions from 5 to 10 years after implantation in a cohort of 36 mm Pinnacle-Ultamet MoM THA patients (18). Bernstein et al. reported a “runin” period that peaked 4 years after implantation but declined thereafter and stayed steady until 10 years from the operation. However, their implants were 2nd-generation Metasul implants and thus not directly comparable to our study (19). It has been suggested that beyond 10 years from surgery the appropriate follow-up interval for MoM hip resurfacing patients could be 5 years (4). Based on our data and these previous data we suggest that 5-year measurement interval for asymptomatic ReCap-M2a-Magnum patients may be sufficient in the future.
Our overall 10-year survival of 88% is in line with previous literature. In our previous report the 5-year survival of ReCap-M2a-Magnum THA was 93% for any reason for revision. 104 (8%) of 1,329 hips were revised after a median follow-up of 5 years, and ARMD was reported as the reason for revision in 33 hips (32% of revisions) (9). In the present study 197 hips (12%) had been revised and ARMD was the reason for revision in 50% of these reoperations at median of 10 years from the implantation. Lainiala et al. reported almost similar 10-year survival of 89% for ReCap-M2a-Magnum THA in a Finnish population (20). Both AOANJRR and FAR report a revision rate of 11% at 10 years and FAR has a 15-year revision rate of 14% for ReCap-M2a-Magnum THA (6,21). In a study based on the Finnish Arthroplasty Register the 10-year survivorship was 88% (22).
The Kaplan–Meier survival for metal-related adverse events was a proxy for functional failure of ReCap-M2a-Magnum THA implants. Even though the amount of metal-related adverse events was rather high, patients were mainly satisfied with their hip and revision surgery was relatively rarely required. Indications for revision surgery after MoM THA are severe symptoms caused by ARMD, large pseudotumors with tissue necrosis, and high WB metal ions (23). The revision decision is multifactorial, even though early revision may be associated with improved outcome (1).
We found pseudotumors in 338 hips (60%) of 563 hips undergoing MARS-MRI. However, MARS-MRI was performed only on patients with metal ions above 5 ppb, and/or those patients with a symptomatic hip. Therefore, the relatively high proportion of patients with a pseudotumor in MARS-MRI does not represent the whole cohort. Nevertheless, 338 of 1,624 hips (21% of all hips) were diagnosed with a pseudotumor, and the true incidence of pseudotumors would probably be higher. For preference, we would have had MARS-MRI images of all the hips. On the other hand, patients reported mainly good to excellent OHS scores postoperatively, suggesting that a substantial number of pseudotumors were asymptomatic. Similarly, Borgwardt et al. reported good to excellent functional outcomes up to 7 years after ReCap-M2a-Magnum THA implantation (24). In our study, repeated MARS-MRI images were normal most of the time if the initial MARS-MRI was considered normal, and the grade of the pseudotumors rarely changed. Reito et al. have previously reported similar findings in their study of 154 ASR patients (25). It has been suggested that routine MARS-MRI imaging after 10 years of MoM hip implantation might not be beneficial (4).
Female sex was associated with an increased revision risk and also an increased risk of metal-related adverse events. It has also been stated previously that female patients have a higher revision rate associated with MoM THA implants than men, even with the same head size (1). Cup retroversion was associated with a higher incidence of metal-related adverse events and higher revision rate in unilateral patients in the current study. High inclination angle was associated with an increased risk of metal-related adverse events in unilateral implants. Cup malposition in ReCap-M2a-Magnum THA patients has also been associated with elevated metal ion levels in an earlier publication (26). The ability to tolerate implant malposition is clearly decreased using the ReCap-Magnum device, which is a major weakness.
Our study has several limitations. First, the study setting was retrospective. Our results may be prone to selection bias. The worst ARMD hips were revised relatively early on, and therefore they did not undergo repeated metal ion measurements. Many of these revised patients would probably have had elevated whole-blood metal ion levels without the early revision to conventional THA. Also, some of the patients were reoperated on early due to fracture or infection and were not involved in metal ion measurements. MARS-MRI was performed only on patients with elevated metal ions above 5 ppb, or a symptomatic hip. Even though the angle measurements were performed using a standardized method, the intraclass correlation was not separately assessed. Further, our findings are implant specific, and not generalizable to other MoM THA brands.
In conclusion, WB Cr and Co ion levels decreased in median 10-year follow-up in the largest ReCap-Magnum series of repeated measurements we are aware of. Based on our findings, we suggest that after 10 years from the implantation the appropriate measurement interval for asymptomatic ReCap-M2a-Magnum THA patients might be longer, e.g., 5 years in the future. The amount of metal-related adverse events was relatively high, but patient satisfaction was acceptable.
Reference
- van der Merwe J M. Pseudotumors in total joint arthroplasty. JBJS Rev 2021; 9(4). doi: 10.2106/JBJS.RVW.20.00125.
- Reito A, Moilanen T, Puolakka T, Pajamäki J, Eskelinen A. Repeated metal ion measurements in patients with high risk metal-on-metal hip replacement. Int Orthop 2014; 38(7): 1353-61. doi: 10.1007/s00264-014-2300-7.
- Lainiala O, Karsikas M, Reito A, Eskelinen A. Whole blood chromium concentration is very rarely elevated independently of whole blood cobalt. Sci Rep 2021; 11(1). doi: 10.1038/s41598-021-91512-9.
- van der Weegen W, Hoekstra H, Brakel K, Sijbesma T. Limited need for screening of metal-on-metal hip resurfacing patients beyond 10 years of follow-up. Hip Int 2022; 32(1): 106-12. doi: 10.1177/1120700020917939.
- Matharu G S, Mellon S J, Murray D W, Pandit H G. Follow-up of metal-on-metal hip arthroplasty patients is currently not evidence based or cost effective. J Arthroplasty 2015; 30(8): 1317-23. doi: 10.1016/j.arth.2015.03.009.
- FAR. Finnish Arthroplasty Register.
- Pietiläinen S, Mäntymäki H, Vahlberg T, Reito A, Eskelinen A, Lankinen P, et al. Repeated cobalt and chromium ion measurements in patients with bilateral large-diameter head metal-on-metal ReCap-M2A-Magnum total hip replacement. Acta Orthop 2020; 3674(4): 378-82. doi: 10.1080/17453674.2020.1751940.
- Mäntymäki H, Lankinen P, Vahlberg T, Reito A, Eskelinen A, Mäkelä K. Repeated cobalt and chromium ion measurements in patients with large-diameter head metal-on-metal ReCap-M2A-Magnum total hip replacement. Acta Orthop 2019; 90(3): 243-8. doi: 10.1080/17453674.2019.1595469.
- Mäntymäki H, Junnila M, Lankinen P, Seppänen M, Vahlberg T, Mäkelä K T. Systematic screening of adverse reactions to metal debris after Recap-M2A-Magnum Metal-on-Metal total hip arthroplasty. Scand J Surg 2017; 106(4): 342-9. doi: 10.1177/1457496916683093.
- van der Straeten C, Grammatopoulos G, Gill H S, Calistri A, Campbell P, de Smet K A. The 2012 Otto Aufranc Award: The interpretation of metal ion levels in unilateral and bilateral hip resurfacing. Clin Orthop Relat Res 2013; 471(2): 377-85. doi: 10.1007/s11999-012-2526-x
- Bosker B H, Ettema H B, Boomsma M F, Kollen B J, Maas M, Verheyen C C P M. High incidence of pseudotumour formation after large-diameter metal-on-metal total hip replacement. J Bone Joint Surg Br 2012; 94-B(6): 755-61. doi: 10.1302/0301-620X.94B6.28373.
- Pietiläinen S, Smedberg E, Laaksonen I, Venäläinen M S, Lankinen P, Mäkelä K T. Repeated metal ion measurements and long-term outcome of Durom/MMC total hip arthroplasty. Acta Orthop 2022; 93: 241-8. doi: 10.2340/17453674.2022.1444.
- Pietiläinen S, Lindström M, Laaksonen I, Venäläinen M S, Lankinen P, Mäkelä K T. Long-term blood metal ion levels and clinical outcome after Birmingham hip arthroplasty. Scand J Surg 2022; 111(1): 145749692110661. doi: 10.1177/14574969211066197.
- Hart A J, Satchithananda K, Liddle A D, Sabah S A, McRobbie D, Henckel J, et al. Pseudotumors in association with well-functioning metal-on-metal hip prostheses. J Bone Joint Surg Am 2012; 94(4): 317-25. doi: 10.2106/jbjs.j.01508.
- R Core Team. A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2016. Available from: https://www.r-project.org/.
- van der Straeten C, van Quickenborne D, de Roest B, Calistri A, Victor J, de Smet K. Metal ion levels from well-functioning Birmingham Hip Resurfacings decline significantly at ten years. Bone Joint J 2013; 95-B(10): 1332-8. Doi: 10.1302/0301-620X.95B10.32022.
- Daniel J, Ziaee H, Pradhan C, McMinn D J W. Six-year results of a prospective study of metal ion levels in young patients with metal-onmetal hip resurfacings. J Bone Joint Surg Br 2009; 91(2): 176-9. doi: 10.1302/0301-620X.91B2.21654.
- Sangaletti R, Spreafico A, Barbieri F, Ferrari R, Castelli C C. Metal ion trend in patients with metal-on-metal total hip arthroplasty: a 10-year prospective study. Hip Int 2018; 28(2_suppl): 43-7. doi: 10.1177/1120700018812991.
- Bernstein M, Desy N M, Petit A, Zukor D J, Huk O L, Antoniou J. Long-term follow-up and metal ion trend of patients with metal-on-metal total hip arthroplasty. Int Orthop 2012; 36(9): 1807-12. doi: 10.1007/s00264-012-1570-1.
- Lainiala O S, Reito A P, Nieminen J J, Eskelinen A P. Declining revision burden of metal-on-metal hip arthroplasties. J Arthroplasty 2019; 34(9): 2058-2064.e1. Doi:10.1016/j.arth.2019.04.058.
- AOANJRR. Annual Report 2021. Available from: https://aoanjrr.sahmri.com/documents/10180/712282/Hip%2C+Knee+%26+Shoulder+Arthroplasty/bb011aed-ca6c-2c5e-f1e1-39b4150bc693 (Accessed Feb 11, 2022).
- Seppänen M, Laaksonen I, Pulkkinen P, Eskelinen A, Puhto A P, Kettunen J, et al. High revision rate for large-head metal-on-metal THA at a mean of 7.1 Years: a registry study. Clin Orthop Relat Res 2018; 476(6): 1223-30. doi: 10.1007/s11999.0000000000000159.
- Matharu G S, Eskelinen A, Judge A, Pandit H G, Murray D W. Revision surgery of metal-on-metal hip arthroplasties for adverse reactions to metal debris: a clinical update. Acta Orthop 2018; 89(3): 278-88. doi: 10.1080/17453674.2018.1440455.
- Borgwardt A, Borgwardt L, Zerahn B, Daugaard H, Borgwardt L, Ribel-Madsen S. A randomized seven-year study on performance of the Stemmed Metal M2a-Magnum and Ceramic C2a-Taper, and the Resurfacing ReCap hip implants. J Arthroplasty 2018; 33(5): 1412-20. doi: 10.1016/j.arth.2017.11.061.
- Reito A, Elo P, Puolakka T, Pajamäki J, Nieminen J, Eskelinen A. Repeated magnetic resonance imaging in 154 hips with large-diameter metal-on-metal hip replacement. Acta Orthop 2014; 85(6): 570-6. doi: 10.3109/17453674.2014.961868.
- Larsen B M, Borgwardt A, Ribel-Madsen S, Zerahn B. False profile view is independently associated with serum metal levels in patients with metal-on-metal hip arthroplasty. Eur J Orthop Surg Traumatol 2021; 31(6): 1029-36. doi: 10.1007/s00590-020-02839-4.