Minor effect of patient education for alcohol cessation intervention on outcomes after acute fracture surgery: a randomized trial of 70 patients
Julie Weber Melchior EGHOLM 1,2, Bolette PEDERSEN 2, Kristian OPPEDAL 3, Bjørn Lindegård MADSEN 4, Jes Bruun LAURITZEN 5, Mette RASMUSSEN 2,6, Anders HELANDER 7, Johanna ADAMI 8, and Hanne TØNNESEN 1,2,6
1 Orthopaedic Department, Hospital of Southern Jutland, University of Southern Denmark, Aabenraa, Denmark; 2 Clinical Health Promotion Centre, WHO-CC, the Parker Institute, Bispebjerg & Frederiksberg Hospital, Copenhagen University Hospitals, Denmark; 3 Alcohol and Drug Research Western Norway, Stavanger University Hospital, Norway; 4 Orthopaedic Department, Amager & Hvidovre Hospital, Copenhagen University Hospitals, Denmark; 5 Orthopaedic Department, Bispebjerg & Frederiksberg Hospital, Copenhagen University Hospitals, Denmark; 6 Clinical Health Promotion Centre, WHO-CC, Department of Health Sciences, Lund University, Lund, Sweden; 7 Department of Laboratory Medicine, Karolinska Institutet & Karolinska University Laboratory, Stockholm, Sweden; 8 Sophiahemmet University, Stockholm, Sweden
Background and purpose — High alcohol intake is associated with increased risk of postoperative complications. Alcohol cessation intervention is recommended prior to elective surgery. We investigated short- and long-term effects of perioperative intensive alcohol intervention in relation to acute ankle fracture surgery.
Patients and methods — 70 patients requiring ankle fracture surgery and consuming ≥ 21 drinks weekly (1 drink = 12 g ethanol) were randomized to a manual-based 6-week intensive standardized alcohol cessation program, the Gold Standard Program (GSP-A), or treatment as usual (TAU), on the day of operation. GSP-A included 5 personal meetings, patient education, and motivational and pharmacological support (alcohol withdrawal prophylaxis, B vitamins, and low-dose disulfiram). Complications requiring treatment were measured after 6 weeks and 1 year. Alcohol intake was validated by biomarkers. Quality of life (QoL) was measured by the SF-36. Hospital costs were obtained from the National Hospital Costs Register.
Results — Postoperatively, complete alcohol cessation was higher in the GSP-A than in the TAU group (18/35 vs. 5/35, number needed to treat = 3, p ≤ 0.001), but not lowrisk consumption in the long term (10/35 vs. 7/33, p = 0.5). Number of complications in the short and long term (12/35 vs. 14/33, 16/35 vs. 18/33), the SF-36 score, or hospital costs in the short and long term (€6,294 vs. €8,024, €10,662 vs. €12,198), were similar between the groups.
Interpretation — Despite an effect on alcohol cessation and a positive tendency as regards the other outcomes, the postoperative complications, QoL, and costs were similar. Better perioperative strategies for acute surgical patients with high alcohol intake therefore need to be developed.
Citation: Acta Orthopaedica 2022; 93: 424–431. DOI http://dx.doi.org/10.2340/17453674.2022.2482.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2021-11-03. Accepted: 2022-03-22. Published: 2022-04-12.
Correspondence: julie.weber.melchior.egholm@regionh.dk
The authors would like to thank project nurse Ina Stark from Hvidovre Hospital for data collection, and Hjalte Sass Frandsen, Marianne Aalykke, and Erika Wernheden from Bispebjerg-Frederiksberg Hospital for helping with follow-up visits.
The project was conceptualized by HT and all authors participated in the design and protocol of the study. JWME drafted the manuscript. JWME, BP, and HT coordinated the study. JWME and BP included patients. BLM and JBL conducted follow-ups for postoperative complications. AH analyzed the alcohol biomarkers. MR performed the statistical analyses. All authors contributed to the interpretation of the data, critically revised, and approved the final manuscript.
Acta thanks Åsa Magnusson and Mikael Sundfeldt for help with peer review of this study.
A daily intake of 28 and 20 g ethanol, respectively, has been reported to increase postoperative complications and mortality (1,2), and therefore social drinking was included in the ASA score from 2015. For ankle fracture surgery, an older study showed 30% complications for patients consuming at least 60 g ethanol daily compared with 10% for matched patients drinking less than 24 g per day (3).
Until now, only 3 randomized studies of the effects of perioperative alcohol intervention on postoperative complications have been published, all relating to elective surgery. 2 studies on 60 patients evaluating intensive alcohol cessation intervention were summarized in a recent review (4). It showed that 4–8 weeks of intensive intervention, such as the Gold Standard Program (GSP-A) (5), reported a high quit rate and improved alcohol-induced organ dysfunction preoperatively, and halved complication rates with number needed to treat (NNT) of 2–4 patients (6). In contrast, the 3rd study on 68 orthopedic patients testing a brief intervention aiming at reduction or cessation of drinking did not identify statistically significant changes (7).
An older Danish cost analysis estimated the extra costs of postoperative complications from high alcohol intake at €160–270 million per year (8), indicating potentially lower costs through effective risk reduction. Furthermore, effective alcohol intervention influences long-term health.
For patients with trauma, the preoperative period is short. However, intensive smoking cessation intervention in the post-fracture period almost halved complications in a randomized study of smokers, with an NNT of 6 (9). Similar trials have not yet been conducted among patients with high alcohol consumption.
We compared the effect of the 6-week GSP-A with treatment as usual (TAU) for patients undergoing acute ankle fracture surgery and drinking 21 or more drinks (1 drink equals 12 g ethanol) per week. The main hypothesis was that GSP-A improved postoperative complications and secondly the alcohol intake, hospital stay, hospital costs, and quality of life (QoL) in the short and long term.
Patients and methods
Study design
This randomized controlled trial followed the CONSORT recommendations for reporting. After informed consent, patients were allocated 1:1 to the GSP-A or TAU using a computergenerated list (www.sealedenvelope.com) of random numbers with stratification for each center in random block sizes. The allocation sequence was concealed in sequentially numbered, opaque, sealed envelopes. Due to the nature of the study, it was not possible to blind the patients or the therapist, but the primary outcome and all analyses were performed blinded.
Patient selection
Patients were recruited by alcohol screening of all adults undergoing ankle fracture surgery at the orthopedic departments of Bispebjerg and Hvidovre University Hospitals in the Capital Region, Denmark (Figure 1). Patients above 18 years of age scheduled for operative intervention of ankle fracture and drinking at least 21 drinks (252 g ethanol) per week in the past 3 months were eligible to participate. Exclusion criteria were major trauma, pregnancy and lactation, allergy to benzodiazepines or disulfiram, uncompensated chronic diseases (including fulminant liver or cardiac insufficiency, which are contraindications for disulfiram), reduced ability to provide informed consent due to a severe psychiatric disorder or other conditions, and withdrawal of informed consent. Patients with cancelled surgery were still included in the analysis of alcohol cessation.
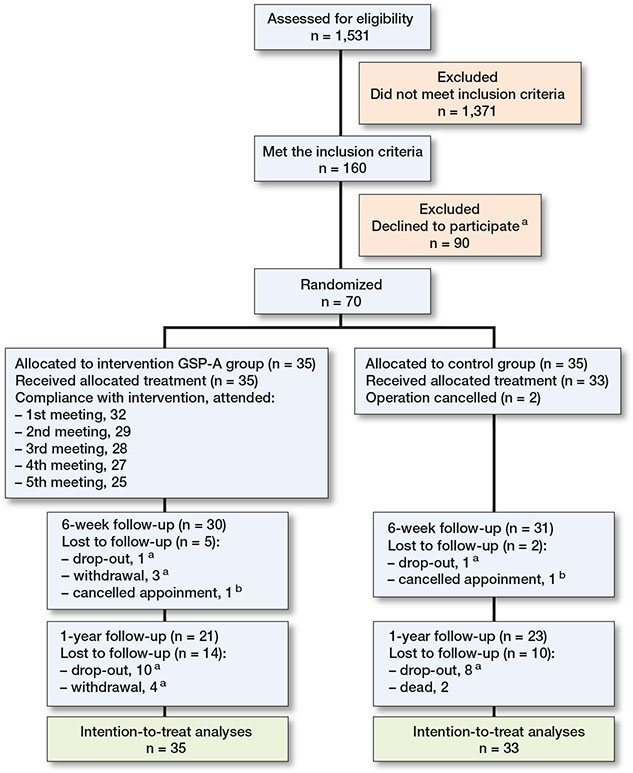
Figure 1. Trial profile. a Allowed to follow via medical record system. b Data collected at the following meeting.
Perioperative procedures
All patients received general information materials, plus thromboembolic and antibiotic prophylaxis, before undergoing standardized surgical and anesthetic procedures for internal fixation of ankle fractures. Patients with open fracture continued antibiotics postoperatively.
Patients were allowed immediate full weightbearing, except those having a syndesmosis fixation. After 6 weeks, they had a follow-up visit.
Intervention
The intervention group underwent a manual-based 6-week GSP-A treatment aiming for complete alcohol abstinence, delivered by trained project staff, and starting within 36 hours after admission. It included 5 x 30-minute sessions using a structured patient education program, motivational support, and supervised use of disulfiram (200 mg twice weekly), B vitamins, and alcohol withdrawal symptom prophylaxis/treatment (chlordiazepoxide; 10 mg p.n.) as described previously (5). Medications and transportation were free.
Control group
Patients in the control group received standard treatment (TAU), which included the official folder concerning alcohol and surgery from the Danish National Board of Health and Welfare (10).
Preoperative evaluations
At the time of inclusion, the project staff interviewed the patients about their alcohol consumption in number of standard drinks (12 g ethanol) (2,6) using the Timeline Follow-back (11), the Alcohol Use Disorders Identification Test (AUDITC) (12), ICD-10 Criteria for Alcohol Dependency, and the revised Clinical Institute Withdrawal Assessment for Alcohol scale (13). In addition, tests for biomarkers were performed, a breath ethanol test (Dräger) was performed, and blood was sampled for blinded analyses of mean corpuscular volume (MCV) (Sysmex XE-5000/Sysmex XN-9000; Sysmex Corp, Kobe, Japan), gamma-glutamyl transferase (GGT) (Roche Diagnostics, Cobas 6000/Cobas 8000; Roche Diagnostics, Basel, Switzerland), carbohydrate-deficient transferrin (CDT) (IFCC-approved HPLC reference method) (14), indicating high alcohol consumption over the past weeks to 1 month, and phosphatidyl ethanol (PEth 16:0/18:1) (LC–MS/MS) (15), indicating any alcohol consumption over the past days to weeks. Furthermore, daily smoking, overweight, risk of malnutrition and physical inactivity, comorbidities, ASA scores, and pre-trauma ankle function (16) were registered. The fractures were classified according to the AO classification (17).
Postoperative evaluations
At the 6-week and 12-month follow-up visits, the collection of baseline data was repeated. The primary outcome was originally defined as the number of patients developing at least 1 complication requiring treatment (5). This was pre-understood as a composite outcome consisting of the different types of predefined complications. To make that clearer, on September 17, 2013, we changed the wording for the outcome to include the term composite, thus including the same predefined complications including the ultimate complication, death (www. clinicaltrials.gov). Complications were verified by 2 blinded orthopedic specialists (BML and JBL) and categorized according to Clavien–Dindo classification after 6 weeks (18). Other long-term conditions requiring hospital treatment within 12 months were also evaluated blinded. Clinical data including length of hospital stay was retrieved from the medical record system. Complete alcohol abstinence in the 6-week perioperative period and following the non-risky intake was verified by the alcohol biomarkers. The 36-item Short Form Health Survey (SF-36) ranging from 0 to 100, with higher scores indicating better health, was used to measure health-related QoL (HRQoL) (19).
Data on direct hospital costs was collected for each patient from the National Hospital Costs Registry, where all data were available with a delay of about 3 years due to national control procedures. At 12-month follow-up, the ankle function was measured as self-reported and using the Olerud Molander ankle score (16), and development of osteoarthritis diagnosed blinded by radiographs. The AO classification of the fractures was evaluated blindly at the same time.
Statistics
According to the literature, the postoperative complication rate is 30% for patients with high alcohol intake vs. 10% for matched patients consuming little or no alcohol (3). The studies on preoperative intervention were based on a minimal relevant difference up to 50% and the related effect of complete alcohol abstinence was 90% vs. less than 10% (4). From a clinical perspective, it would be relevant to investigate an effect of the main outcome with the 20% through post-traumatic alcohol intervention, which in this study represented the minimal clinical and statistical relevant difference. Using a power of 80% and a risk of type-I failure of 5%, 2 x 59 patients were needed to assess the primary outcome. This number would also cover the secondary outcome on complete alcohol abstinence at 6-week follow-up. The inclusion period was limited to about 4 years.
Data was analyzed as intention-to-treat. Fisher’s exact tests and chi-square tests were used for frequencies, and Mann– Whitney tests for continuous data. Significance was considered at p < 0.05. We have per tradition used a parametric power calculation, but we have, however, used non-parametric analyses for the results, because we did not expect a normal distribution of those results; all this is reported in the protocol article.
The absolute risk reduction (ARR) was calculated as the events in the control group minus the events in the intervention group, and the relative risk reduction (RRR) as the ARR divided by the events in the control group. The NNT was calculated by 1/ARR. As per tradition, costs were reported with means and standard error (SE), mean difference (MD), and 95% confidence interval (CI). Bootstrapping procedures were used to calculate the cost-effectiveness plane and the acceptability curve by repeatedly resampling the data (1,000 incremental cost and effect pairs). A dropout analysis was performed, while a nonparticipant analysis has been published previously (20).
Ethics, registration, data sharing, funding, and potential conflicts of interest
The trial was approved by The National Committee on Health Research Ethics (main protocol H-1-2009-087), the Danish Data Protection Agency (2009-41-3741), registered with ClinicalTrials.gov number NCT00986791, and followed the Helsinki-II Declaration.
Grouped data or tables of data without possibility of identification are available.
The study was funded by the Danish Health Authorities, Bispebjerg-Frederiksberg Hospital, Hospital of Southern Jutland, University of Southern Denmark, the OAK Foundation, the Swedish Institute of Public Health, Stockholm County Council (ALF), and Region Skåne, Sweden. The sponsors had no role in the study design, collection, analysis, interpretation of data, article writing, or in the decision to submit the paper.
The authors had no conflicts of interest.
Results
The patient characteristics of both groups were similar (Table 1). Between 2011 and 2014, 70 (2 x 35) patients were recruited with 30/35 participating in the follow-up in the intervention group and 31/33 in the control group at 6 weeks, and 21/35 and 23/33 respectively at 12 months. For 2 patients, the operation was cancelled, and they were included only in the analyses on alcohol abstinence. The time from injury to operation was similar in both groups: 1 day (range 0–24) and 1 day (0–10), respectively.
| Factor | GSP-A (n = 35) | Control (n = 33) |
| Age | 48 (22–77) | 53 (20–78) |
| Male sex | 25 | 22 |
| Alcohol intake in the last week (units) a | 35 (9–106) | 31 (2-114) |
| AUDIT score (0–40 points, 0 being no consumption) | 18 (7–40) | 17 (4–31) |
| Alcohol dependency (ICD-10) | 12 | 12 |
| Other lifestyle factors | ||
| Risk of malnutrition | 9 | 14 |
| Overweight (BMI > 25) | 27 | 25 |
| Physical inactivity (< 30 min/day) | 23 | 13 |
| Daily smoking (any amount) | 27 | 17 |
| Working status/employed | 15 | 13 |
| Education | ||
| None | 8 | 11 |
| < 3 years | 17 | 11 |
| > 3 years | 9 | 11 |
| Homeless | 0 | 1 |
| Marriage/partners | 8 | 13 |
| Comorbidity (no patients had decompensated comorbidity) | ||
| Any comorbidity | 17 | 13 |
| Lung disease | 5 | 2 |
| Cardiovascular disease | 8 | 5 |
| Diabetes | 1 | 0 |
| Liver disease | 1 | 2 |
| Psychiatric disorder further to alcohol | 10 | 7 |
| Other | 16 | 10 |
| ASA scores from the anesthesiological record | ||
| 1 | 19 | 14 |
| 2 | 16 | 16 |
| 3 | 0 | 3 |
| Self-reported ankle function prior to trauma (1–5 points) | ||
| 1 | 20 | 21 |
| 2 | 8 | 7 |
| 3 | 3 | 3 |
| 4 | 2 | 2 |
| 5 | 0 | 0 |
| Fracture type | ||
| Open | 2 | 4 |
| Closed | 33 | 29 |
| AO classification: | ||
| 44-A1 | 0 | 1 |
| 44-A2 | 1 | 0 |
| 44-A3 | 0 | 0 |
| 44-B1 | 12 | 12 |
| 44-B2 | 10 | 12 |
| 44-B3 | 9 | 4 |
| 44-C1 | 2 | 2 |
| 44-C2 | 1 | 2 |
| 44-C3 | 0 | 0 |
| Syndesmosis fixation, including LCP b | 7 | 5 |
| Planned removal | 2 | 2 |
| Actually removed | 2 | 2 |
| a All patients had an average alcohol intake > 21 units of 12 g ethanol per week in the preceding 3 months. | ||
| b Locking compression plate | ||
Due to the time limit to include patients, we were not able to include the 118 patients required according to the power calculation, but all non-participating patients agreed to be followed up via the medical record system (20) (Figure 1).
Postoperative complications and hospital stay within 30 days and 12 months
A lower, although not statistically significant, complication rate within 30 days was observed in the intervention group, 12/35 (34%), compared with the control group, 14/33 (42%). The ARR and RRR were 8% (42% minus 34% = 8%) and 19% (8/42 = 0.2), respectively (p = 0.5). The NNT was 1/8 patients. There were no statistically significant differences between the groups regarding complication rates or hospitalization in the follow-up period (Tables 2 and 3).
| At 6 weeks | At 12 months | |||
| GSP-A n = 35 | Control n = 33 | GSP-A n = 35 | Control n = 33 | |
| Surgical site complications | ||||
| Superficial wound complication (treated with antibiotics, repeated dressings, or similar) | 6 | 8 | 7 | 10 |
| Deep wound infection (treated with antibiotics and/or surgical intervention) | 1 | 1 | 2 | 2 |
| Plaster cast complication (skin abrasions and pain, verified by clinical assessment) | 1 | 4 | 2 | 4 |
| Severe pain and/or discomfort | – | – | 3 | 3 |
| Dislocated fracture (verified by radiographic examination) | 3 | 2 | 3 | 3 |
| Malunion (verified by radiographic examination) | – | – | 1 | 0 |
| Alcohol-related complications | ||||
| Withdrawal symptoms (verified by CIWA-Ar) | 5 | 2 | 6 | 18 |
| Delirium (psychosis requiring psychiatric treatment) | 0 | 1 | 0 | 3 |
| Severe ebrietas (treated with detoxification) | – | – | 0 | 11 |
| Hepatic coma (confusion and liver failure) | 0 | 2 | 0 | 2 |
| Others | ||||
| Sepsis (fever, impaired general condition and bacteraemia) | 0 | 1 | 0 | 1 |
| Urinary infection (treated with antibiotics) | 1 | 2 | 1 | 3 |
| Hypertension (systolic BP > 140 and diastolic BP > 90 and anti-hypertensive treatment) | 1 | 0 | 1 | 0 |
| Deep vein thrombosis (verified by ultrasound) | 1 | 0 | 1 | 0 |
| Other severe mental illness (requiring psychiatric treatment) | 0 | 0 | 6 | 0 |
| Other | 0 | 0 | 4 | 7 |
| Death | 0 | 0 | 0 | 2 |
| Total number of complications | 19 | 23 | 37 | 69 |
| Complications per patient developing complications | 1.6 | 1.6 | 2.4 | 3.8 |
| Grade according to the Clavien-Dindo classification | ||||
| I (any deviation with or without treatment) | 1 | 4 | ||
| II (requiring pharmacological treatment, blood or TPN) | 14 | 14 | ||
| IIIa (requiring surgical intervention—no general anesthesia) | 2 b | 1 + 1 b | ||
| IIIb (requiring surgical intervention—general anesthesia | 2 | 0 | ||
| IVa (life-threatening single-organ dysfunction) | 0 | 3 | ||
| IVb (life-threatening multi-organ dysfunction) | 0 | 0 | ||
| V (death) | 0 | 0 | ||
| a For each patient 6 weeks from operation day. Only the most severe complication is included. | ||||
| b Indicates the need for follow-up to fully evaluate the complication. | ||||
| None of the patients experienced compartment syndrome, neurological complications, pneumonia, respiratory failure, emboli, cardiac failure, acute myocardial infarction, atrial fibrillation, or retention of urine. | ||||
Successful alcohol abstinence within 30 days and non-risky intake within 12 months
Significantly more patients in the intervention group succeeded in complete alcohol abstinence perioperatively at 6-week follow-up (18/35 vs. 5/35, p ≤ 0.001), and a reduced weekly alcohol consumption (median 0 g ethanol/week [range 0–512] vs. 252 g/week [0–864]), but there was no difference at 12-month follow-up (Figure 2).
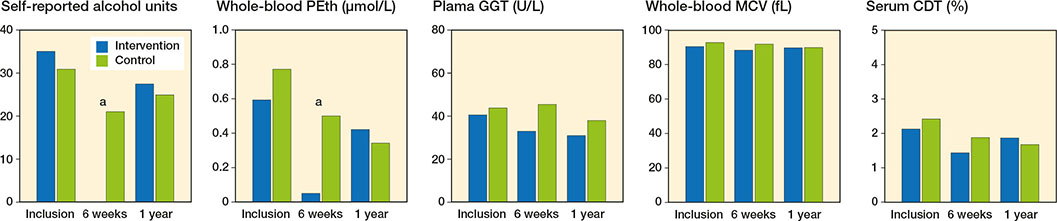
Figure 2. Alcohol consumption and alcohol biomarkers (PEth: phosphatidyl ethanol, GGT: gamma-glutamyl transferase, MCV: mean corpuscular volume, and CDT: carbohydrate-deficient transferrin) in relation to perioperative intensive alcohol intervention compared with standard perioperative care among patients undergoing acute ankle fracture surgery. a Statistically significant.
Ankle function at 12-month follow-up
The ankle function was similar in the intervention and control groups. The self-reported ankle function was 2 (range 1–5) vs. 2 (1–4) on a scale from 1 to 5 with 1 being the best. The Olerud Molander ankle score was 88 (range 10–100) vs. 90 (45–100) and the radiographs showed that 2 patients in each group had from moderate reduction to dislocated fracture (Table 4, see Supplementary data).
Quality of life
The HRQoL did not differ statistically significantly between the 2 study groups (Figure 3).
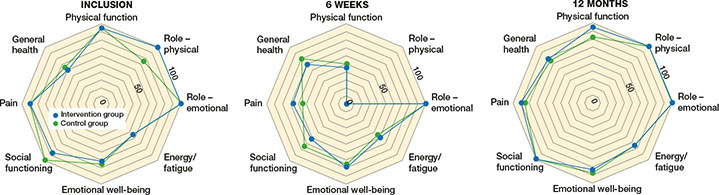
Figure 3. Mean score of the domains in the HRQoL Scale SF-36 after perioperative intensive alcohol intervention compared with standard perioperative care among patients undergoing acute ankle fracture surgery.
Hospital costs within 30 days and 12 months
The average hospital costs were about €1,000 and €2,000 lower per patient, respectively, in the intervention group compared with the control group at 6-week and 12-month follow-low up, but this was not statistically significant (Table 5). The intervention was cost-effective with 81% probability, without incurring additional costs for one extra patient without complications. The cost-effectiveness ratio increased to 83% at a willingness to pay of €3,500 per patient without complications.
Dropout analysis
The analysis of dropouts compared with completers showed no statistically significant differences between the groups (20).
Discussion
Despite a statistically significant effect of the 6-week GSP-A on complete abstinence in half of the patients, compared with 1 in 7 patients in the control group, in the perioperative period, effect measures were similar between the study groups in the short or longer term.
The good short-term effect of the GSP-A program was independent of excessive or addictive consumption. This is similar to other studies on intensive intervention programs (4), thus in contrast to the minor effect of brief interventions in general (21). A recent Danish cost-effectiveness study reported the effects of different brief intervention programs in primary care on a reduction in alcohol intake of only about half a drink per day, an outcome with questionable surgical relevance (22). The intensive GSP-A treatment in the present study included supervised disulfiram at low dose as an important element to support successful cessation of alcohol consumption (21,23). Notably, the short-term alcohol cessation rate of GSP-A was in line with that following the GSP aiming for smoking cessation at 6 weeks, while the longterm rate was lower after GSP-A than could be expected from the GSP for smoking cessation intervention (24).
However, the good effect on perioperative alcohol cessation was not followed by a similar effect on the primary outcome, the rate of postoperative complications. This is disappointing, as previous trials on elective surgery showed a higher absolute risk reduction of 26–43% and a low NNT at 2–4 patients, compared with 8% and 13 patients, respectively, in our study (4). The previous studies did not include HrQoL, cost analyses, or a 12-month follow-up.
A reason for the low impact of the successful alcohol cessation on the other perioperative outcomes is probably that the intervention took place too close to the operation to sufficiently improve alcohol-induced organ dysfunction responsible for the increased development of complications in this patient group (6). This involves immune suppression, hemostatic imbalance, cardiac insufficiency, delayed tissue and bone healing, and increased stress response, most of which require from 1 to 4 weeks to improve (6). As bone healing takes even longer, this could also benefit from postoperative alcohol cessation, although is not reflected in our study.
The rather high complication rate in our study is close to that reported retrospectively 30 years ago after ankle fracture surgery among patients drinking at least 5 drinks per day (3). In contrast to other studies (2,25), a recent cohort study on fast-track surgery reported a reduced complication rate among patients with excessive alcohol consumption (26). Although the authors collected a relevant alcohol history, the outcomes were a hospital stay exceeding 4 days and readmission, and thereby associations with complications may have been overlooked. Another study also questioned the association between risky alcohol intake and complications, by comparing patients who had no alcohol intake with patients with any alcohol intake (27). This categorization seems to introduce a systematic bias, as most persons categorized as having any alcohol intake often drink below the risky limits, thus developing no increased alcoholrelated risk of complications at surgery and diluting the impact from higher alcohol intake.
Cost analyses are sparse on alcohol interventions aiming to improve patient pathways. A previous Danish study estimated the extra direct cost caused by postoperative complications for surgical patients with high alcohol intake to €1,869 at 1996 value (8). In our study, the intervention group saved €1,041 per person at 2017 value, and the cost of GSP-A was approximately €800. An international review reported very low costs of brief intervention, ranging €2 to €172 at 2009 value, but without a reduction in alcohol intake (28).
Bias and limitations
This study has a substantial risk of a type-II failure, as it is underpowered regarding the primary outcome due to including only 59% of the estimated number of patients, and therefore an effect cannot be excluded. We tried to take precautions early against a low inclusion rate in the patient information by applying the lessons learned from pre-study interviews of similar patients. These lessons included the stage of change and the understanding of the association between risky drinking and development of complications (29). The trauma situation itself, leaving only a short period for considering participation, may also have been important.
The randomized design with blind assessment supports a high internal validity, together with the use of a manual-based intervention, trained staff, a high follow-up rate, use of objective alcohol biomarkers for validation, the pre-study definition of complications (5), and national registries with high data completeness. Fulfilling the requirements for a validated alcohol history and careful documentation of postoperative complications is a strength of the study.
The intervention group had more risk factors for complications, such as frequency of smoking, male sex, higher alcohol intake, lower physical activity, and overweight. A better distribution of risk factors between the two groups could have impacted the results, but probably not to a significant degree. In contrast, 2 and 4 patients in the intervention and the control group, respectively, had open fractures, and all 6 developed complications. This may have impacted the difference between the groups. Furthermore, cost analyses are difficult to generalize due to a limited external validity caused by different timeframes, productivity, level, and type of costs (10,22).
Clinical and research impact
An effective alcohol intervention program for perioperative quitting would impact the clinical guidelines. The 8% improvement (not statistically significant) of postoperative complications and savings of €1,000 to €2,000 per intervention patient may be of clinical relevance.
In acute surgical practice, it is important to be trained in obtaining the alcohol history and informing patients about high alcohol consumption as a common risk factor in relation to complications.
Further strategies to improve surgical outcome for acute patients who are heavy drinkers may build on the present knowledge. New research should also consider combining more lifestyle interventions, such as smoking (9), and other elements of multimodal programs for perioperative care, like the early recovery after surgery program (ERAS). Measurements of pathophysiological recovery in alcohol-related dysfunction during interventions should be performed, to identify the shortest preoperative intervention required to obtain a risk reduction among this vulnerable high-risk group of patients undergoing acute surgery.
Conclusion
This intensive alcohol intervention program showed successful alcohol cessation in relation to ankle fracture surgery. The 8% fewer postoperative complications and €1,000–2,000 lower costs per patient may be of clinical relevance. Future strategies for risk reduction should consider combining more lifestyles interventions and other elements such as the ERAS program.
- Rubinsky A D, Bishop M J, Maynard C, Henderson W G, Hawn M T, Harris A H, et al. Postoperative risks associated with alcohol screening depend on documented drinking at the time of surgery. Drug Alcohol Depend 2013; 132: 521-7. doi: 10.1016/j.drugalcdep.2013.03.022.
- Eliasen M, Grønkjær M, Skov-Ettrup L S, Mikkelsen S S, Becker U, Tolstrup J S, et al. Preoperative alcohol consumption and postoperative complications: a systematic review and meta-analysis. Ann Surg 2013; 258: 930-42. doi: 10.1097/SLA.0b013e3182988d59.
- Tønnesen H, Pedersen A, Jensen M R, Møller A, Madsen J C. Ankle fractures and alcoholism: the influence of alcoholism on morbidity after malleolar fractures. J Bone Joint Surg Br 1991; 73: 511-13. doi: 10.1302/0301-620X.73B3.1670461.
- Egholm J W, Pedersen B, Møller A M, Adami J, Juhl C B, Tønnesen H. Perioperative alcohol cessation intervention for postoperative complications. Cochrane Database Syst Rev 2018; 11: CD008343. doi: 10.1002/14651858.CD008343.pub3.
- Tønnesen H, Egholm J W, Oppedal K, Lauritzen J B, Madsen B L, Pedersen B. Patient education for alcohol cessation intervention at the time of acute fracture surgery: study protocol for a randomised clinical multi-centre trial on a gold standard programme (Scand-Ankle). BMC Surg 2015; 15: 52. doi: 10.1186/s12893-015-0035-z.
- Tønnesen H, Nielsen P R, Lauritzen J B, Møller A M. Smoking and alcohol intervention before surgery: evidence for best practice. Br J Anaesth 2009; 102: 297-306. doi: 10.1093/bja/aen401.
- Snowden C, Lynch E, Avery L, Haighton C, Howel D, Mamasoula V, et al. Preoperative behavioural intervention to reduce drinking before elective orthopaedic surgery: the PRE-OP BIRDS feasibility RCT. Health Technol Assess 2020; 24: 1-176. doi: 10.3310/hta24120.
- Ministry of Health Denmark. [The socioeconomic consequences of alcohol consumption]. Copenhagen: Nyt Nordisk Forlag Arnold Busck; 1999.
- Nåsell H, Adami J, Samnegård E, Tønnesen H, Ponzer S. Effect of smoking cessation intervention on results of acute fracture surgery: a randomized controlled trial. J Bone Joint Surg Am 2010; 92: 1335-42. doi: 10.2106/JBJS.I.00627.
- Danish Health Authority. [Alcohol and surgery—prevent complications when undertaking surgery]; 2017.
- National Institutes of Health. Assessing alcohol problems : a guide for clinicians and researchers, 2nd ed. Bethesda, MD: NIAAA Publishing; 2003. https://www.worldcat.org/title/assessing-alcohol-problems-a-guide-for-clinicians-and-researchers/oclc/54056649.
- Babor T, Higgins-Biddle J C, Saunders J B, Monteiro M G. AUDIT— the alcohol use disorders identification test: guidelines for use in primary care. New York: World Health Organizaton Department of Mental Health and Substance Abuse; 2001.
- Sullivan J T, Sykora K, Schneiderman J, Naranjo C A, Sellers E M. Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar). Br J Addict 1989; 84: 1353-7. doi: 10.1111/j.1360-0443.1989.tb00737.x.
- Helander A, Husa A, Jeppsson J O. Improved HPLC method for carbohydrate-deficient transferrin in serum. Clin Chem 2003; 49: 1881-90. doi: 10.1373/clinchem.2003.023341.
- Zheng Y, Beck O, Helander A. Method development for routine liquid chromatography-mass spectrometry measurement of the alcohol biomarker phosphatidylethanol (PEth) in blood. Clin Chim Acta 2011; 412: 1428-35. doi: 10.1016/j.cca.2011.04.022.
- Olerud C, Molander H. A scoring scale for symptom evaluation after ankle fracture. Arch Orthop Trauma Surg 1984; 103: 190-4. doi: 10.1007/BF00435553.
- Müller M E, Allgöwer M, Schneider R, Willenegger H. Manual of internal fixation: techniques recommended by the AO Group. Berlin, Heidelberg: Springer; 1979. https://www.springer.com/gp/book/9783642965074.
- Clavien P A, Barkun J, de Oliveira M L, Vauthey J N, Dindo D, Schulick R D, et al. The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg 2009; 250: 187-96. doi: 10.1097/SLA.0b013e3181b13ca2.
- Ware J E Jr, Gandek B. Overview of the SF-36 Health Survey and the International Quality of Life Assessment (IQOLA) Project. J Clin Epidemiol 1998; 51: 903-12. doi: 10.1016/s0895-4356(98)00081-x.
- Aalykke M, Wernheden E, Pedersen B, Egholm J W, Madsen B L, Lauritzen J B, et al. Participants and non-participants in the Scand-Ankle study: an alcohol cessation intervention at the time of fracture surgery. Clin Heal Promot 2015; 5: 49-53. doi: 10.29102/clinhp.15008.
- McQueen J, Howe T E, Allan L, Mains D, Hardy V. Brief interventions for heavy alcohol users admitted to general hospital wards. Cochrane Database Syst Rev 2011; 8: CD005191. doi: 10.1002/14651858.CD005191.pub3.
- Holm A L, Veerman L, Cobiac L, Ekholm O, Diderichsen F. Costeffectiveness of preventive interventions to reduce alcohol consumption in Denmark. PLoS One 2014; 9: e88041. doi: 10.1371/journal.pone.0088041.
- Jørgensen C H, Pedersen B, Tønnesen H. The efficacy of disulfiram for the treatment of alcohol use disorder. Alcohol Clin Exp Res 2011; 35: 1749-58. doi: 10.1111/j.1530-0277.2011.01523.x.
- Rasmussen M, Fernández E, Tønnesen H. Effectiveness of the Gold Standard Programme compared with other smoking cessation interventions in Denmark: a cohort study. BMJ Open 2017; 7: e013553. doi: 10.1136/bmjopen-2016-013553.
- Best M J, Buller L T, Gosthe R G, Klika A K, Barsoum W K. Alcohol misuse is an independent risk factor for poorer postoperative outcomes following primary total hip and total knee arthroplasty. J Arthroplasty 2015; 30: 1293-8. doi: 10.1016/j.arth.2015.02.028.
- Jørgensen C C, Kehlet H; Lundbeck Foundation Centre for Fasttrack Hip and Knee Replacement Collaborative Group. Outcomes in smokers and alcohol users after fast-track hip and knee arthroplasty. Acta Anaesthesiol Scand 2013; 57: 631-8. doi: 10.1111/aas.12086.
- Elsamadicy A A, Adogwa O, Vuong V D, Sergesketter A, Reddy G, Cheng J, et al. Impact of alcohol use on 30-day complication and readmission rates after elective spinal fusion (≥ 2 levels) for adult spine deformity: a single institutional study of 1,010 patients. J Spine Surg 2017; 3: 403-10. doi: 10.21037/jss.2017.08.12.
- Bray J W, Zarkin G A, Hinde J M, Mills M J. Costs of alcohol screening and brief intervention in medical settings: a review of the literature. J Stud Alcohol Drugs 2012; 73: 911-9. doi: 10.15288/jsad.2012.73.911.
- Pedersen B, Alva-Jørgensen P, Raffing R, Tønnesen H. Fractures and alcohol abuse: patient opinion of alcohol intervention. Open Orthop J 2011; 5: 7-12. doi: 10.2174/187432500110501000.