Do changes in outcomes following primary and revision hip replacement differ and relate to markers of socio-economic status? A 1-year population-based cohort study
Martin B STISEN 1,2, André N KLENØ 1,2, Julie S JACOBSEN 3,4, Matthew D L O’CONNELL 5, Salma AYIS 5, Catherine SACKLEY 5, Alma B PEDERSEN 1,6, and Inger MECHLENBURG 2,6
1 Department of Clinical Epidemiology, Aarhus University Hospital, Aarhus N, Denmark; 2 Department of Orthopaedic Surgery, Aarhus University Hospital, Aarhus N, Denmark; 3 Research Centre for Health and Welfare Technology, Programme for Rehabilitation, VIA University College, Aarhus, Denmark; 4 Research Unit for General Practice in Aarhus, Aarhus, Denmark; 5 Department of Population Health Sciences, School of Population Health and Environmental Sciences, Kings College London, London, UK; 6 Department of Clinical Medicine, Aarhus University, Aarhus, Denmark
Background and purpose — There is little evidence on improvement after revision total hip replacement (THR). Moreover, improvements may be associated with socioeconomic status (SES). We investigated whether changes in Harris Hip Score (HHS) differ among patients undergoing primary and revision THR, and their association with markers of SES.
Patients and methods — We conducted a population-based cohort study on 16,932 patients undergoing primary and/or revision THR from 1995 to 2018 due to hip osteoarthritis. The patients were identified in the Danish Hip Arthroplasty Registry. Outcome was defined as mean change in HHS (0–100) from baseline to 1-year follow-up, and its association with SES markers (education, cohabiting, and wealth) was analyzed using multiple linear regression adjusting for sex, age, comorbidities, and baseline HHS.
Results — At 1-year follow-up, HHS improved clinically relevant for patients undergoing both primary THR: mean 43 (95% CI 43–43) and revision THR: mean 31 (CI 29–33); however, the increase was 12 points (CI 10–14) higher for primary THR. For primary THR, improvements were 0.9 points (CI 0.4–1.5) higher for patients with high educational level compared with low educational level, 0.4 points (CI 0.0–0.8) higher for patients cohabiting compared with living alone, and 2.6 points higher (CI 2.1–3.0) for patients with high wealth compared with low wealth.
Interpretation — Patients undergoing primary THR achieve higher improvements on HHS than patients undergoing revision THR, and the improvements are negatively related to markers of low SES. Health professionals should be aware of these characteristics and be able to identify patients who may benefit from extra rehabilitation to improve outcomes after THR to ensure equality in health.
Citation: Acta Orthopaedica 2022; 93: 397–404. DOI http://dx.doi.org/10.2340/17453674.2022.2430.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2021-11-17. Accepted: 2022-03-05. Published: 2022-04-06.
Correspondence: mstisen@clin.au.dk
MBS drafted the manuscript. MBS, ANK, JSJ, MOC, SA, CS, ABP and IM conceived and designed the study, interpreted the results, and revised the manuscript.
Acta thanks David N. Bernstein and the anonymous reviewer for help with peer review of this study.
Clinically relevant improvements in pain and hip function are slightly poorer for revision total hip replacement (THR) than for primary THR (1). Furthermore, there is sparse evidence on revision THR, regarding the effect on pain and hip function (2).
During the last decades, inequality in healthcare has been a concern across countries (3). Consequently, evidence of inequality in healthcare has accumulated, pointing to socioeconomic factors such as income, wealth, and education as strong factors, shaping health across settings and populations (3). For various diseases, low socioeconomic status (SES) may influence the effect of healthcare (4,5). In fact, a socioeconomic gradient has been found for functional limitations in people aged 55 to 84 years, meaning that SES is inversely related to functional limitations (6). In patients undergoing THR, associations between outcome of THR and low SES have been reported in small-sample studies and in selective populations (7-10). However, evidence of differences in outcome of primary and revision THR and an association to SES have not been proven in larger population-based studies. Therefore, we investigated whether changes in Harris Hip Score (HHS) differed between patients undergoing primary and revision THR, and if these changes were associated with markers of SES.
Patients and methods
Study design and population
This is a population-based cohort study in patients undergoing primary or revision THR during 1995–2018 due to hip osteoarthritis (OA) identified in the Danish Hip Arthroplasty Register (DHR).
Data sources and study population
We used data linkage between the DHR, the Civil Registration System (CRS), Statistics Denmark, and the Danish National Patient Register (DNPR).
The study population included all patients undergoing primary or revision THR during 1995–2018 identified in the DHR, and date of THR was considered as index date. The DHR is a national clinical database, including THRs and follow-up examinations. It was established in 1995 and all public orthopedic departments and private hospitals in Denmark performing THRs report to this register. Registration is compulsory and completeness for primary THR was 95% and 85% for revision THR in 2018 (11,12); however, recording of follow-up examinations is voluntary and therefore notably lower. CRS contains information on all Danish citizens, and every citizen is given a unique 10-digit personal identification number (13). This allows for unambiguous individual-level record linkage of Danish registers, where daily updated information on migration and vital status allows for complete long-term follow-up. Information on age, sex, and cohabiting status was retrieved from the CRS.
Statistics Denmark is the central authority for Danish statistics, and collects, processes, and publishes statistical information concerning the Danish society. The database is updated yearly. Information on educational level was retrieved from the Population Education Register and information on family income and family liquid assets was retrieved from the Income Statistics Register.
The DNPR contains information on all patients from hospitals since 1977, and outpatient clinic and emergency room visits since 1995. Diagnoses are classified according to the International Classification of Diseases (ICD-10) (14).
Markers of socioeconomic status
SES markers were educational level, cohabiting status, and family wealth. Highest obtained educational level was classified into either low, medium, or high educational level. Low level was defined as none or high school completed. Medium level was defined as vocational education or higher general and preparatory examinations programs completed. High level was defined as bachelor’s degree completed or higher. Cohabiting status was classified into living alone, cohabiting, or other. Cohabiting was defined as married couples and couples in general, whereas other was defined as households with multiple families. To examine family wealth, family liquid assets were used for patients ≥ 65 years of age, and family income for patients < 65 years of age (15). Given that a large proportion of patients were ≥ 65 years of age and received state pension, liquid assets for this group are a more precise estimate than income. To account for annual deviations, family liquid assets and family income were obtained for the 5 years prior to THR and categorized into 3 thirds: low, medium, or high family wealth.
Harris Hip Score
The outcome in this study was change in HHS measured from before to 1-year after primary and revision THR. HHS is a valid, reliable, and widely used physician-completed instrument designed to evaluate outcome after THR (16), though ceiling effects are common and may affect the validity (17). HHS consists of subscales for pain, function, absence of deformity, and range of motion.
Higher HHS score indicated less dysfunction, and a total score of 90–100 points is considered an excellent result, 80–90 points is a good result, 70–80 points is a fair result, and < 70 is considered a poor result. An 18-point change in HHS after treatment is considered a minimal clinically important improvement and a 40-point change is considered a moderate improvement (16). Data on HHS is retrieved from the DHR, but registration regarding HHS is not compulsory.
Covariates
Relevant covariates affecting the association between HHS and SES were age, sex, comorbidities, and baseline HHS. All these covariates are individually predictive of HHS, associated with markers of SES, and are not intermediates between markers of SES and HHS (9,18-21). Therefore age, sex, comorbidities, and baseline HHS were adjusted for in the multiple linear regression analyses to reduce confounding bias.
Age was divided into categories of < 46, 46–55, 56–65, 66–75, and > 75 years. Information on comorbidities was retrieved up to 10 years prior to THR and measured by the Charlson Comorbidity Index (CCI). In this study CCI was divided into categories of low (i.e., score of 0), medium (i.e., score of 1-2) or high (i.e., score of 3 or more) (22).
Statistics
Patient characteristics were presented for primary and revision THR with frequencies (n) and percentages (%) at index date.
Baseline and 1-year follow-up data on HHS and changes in HHS from baseline to 1-year follow-up were presented for all patients and separately for primary and revision THR. Moreover, the data was further presented by SES markers.
Welch’s unpaired t-test was performed to examine differences in mean changes in HHS between patients undergoing primary THR and revision THR.
Associations between SES subgroups and mean HHS changes were analyzed with multiple linear regression analyses, adjusting for the covariates age, sex, comorbidities, and HHS baseline. The assumptions of the multiple linear regression analyses were based on plots of observed versus predicted values, scatter plots, residual plots, histogram, and Q–Q plot. Results of the analyses for primary and revision THR were presented as coefficients for each SES subgroup with 95% confidence intervals (CI). The analyses were based on patients with complete data on HHS and SES markers at baseline and 1-year follow-up. Missing data was investigated by comparing patient characteristics of those with complete HHS and those without. Stata16.0 was used for statistical analyses (StataCorp, College Station, TX, USA).
Ethics, funding, data sharing, and potential conflicts of interest
According to Danish law, ethics committee approval is not required for registry-based studies. The Danish Data Protection Agency (Aarhus University record number 2016-051-000001, id.nr. 880) approved the study. This research was partly funded by the Orthopedic-Surgical Research Foundation. As part of the Data Use Agreement at the Danish Hip Arthroplasty Register, authors are not allowed to provide raw data. Upon reasonable request, the corresponding author will provide statistical programming codes used to generate the results. The authors declare no conflict of interest.
Results
Study population
We identified 121,890 THR patients with hip OA. Baseline HHS and 1-year follow-up HHS data were available on 17% of the primary THR and 5% of the revision THR in the dataset, and patients with missing data on HHS (n = 102,610) or on SES markers (n = 2,348) were excluded. Our study population comprised data on 16,932 patients, of whom 16,436 had undergone primary THR and 496 had undergone revision THR (Figure 1).
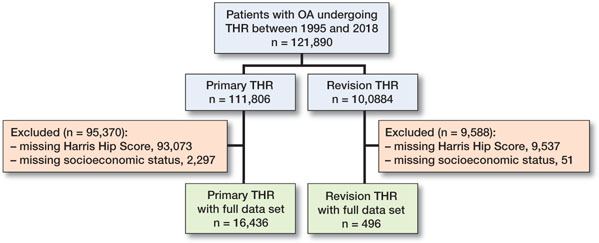
Figure 1. Flowchart illustrating inclusion and exclusion process of the study population. OA = osteoarthritis. THR = total hip replacement.
The proportion of females in the study population was 52% for primary THR and 49% for revision THR. Mean age at index date was 67 years (SD 9) for primary THR and 63 years (SD 10) for revision THR, and the majority of primary THR (85%) and revision THR patients (75%) had no comorbidities (Table 1). The primary THR and revision THR cohorts differed with respect to some baseline characteristics. Patients undergoing revision THR were on average 4 years younger and had more comorbidities than primary THR (Table 1). Patients with low educational level and patients living alone were more likely to be females and older, and patients with high educational level, cohabiting, and high wealth tended to have fewer comorbidities (Table 2).
Changes in HHS
In primary and revision THR, HHS improved from baseline to 1-year follow-up (Table 3 and Figure 2). Patients undergoing primary THR reported higher improvements compared with patients undergoing revision THR (Table 4). Comparison of the HHS improvements in all THRs, and separately for primary THR and revision THR among the patients in each stratum of educational level, cohabiting status, and family wealth is presented in Table 3 and Figure 3.
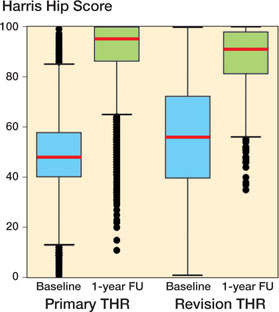
Figure 2. Box plot of baseline Harris Hip Score and 1-year follow-up Harris Hip Score for primary and revision total hip replacement (THR).
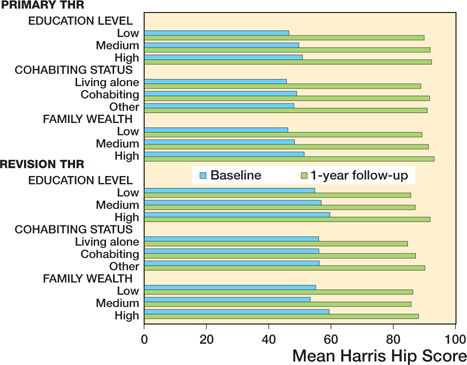
Figure 3. Bar chart showing baseline Harris Hip Score and 1-year follow-up Harris Hip Score categorized by subgroups of socioeconomic status markers on patients undergoing primary and revision total hip replacement (THR).
Socioeconomic status
For primary THR, patients with higher educational level, cohabiting, and higher wealth had higher HHS change scores compared with patients with lower educational level, living alone, and lower wealth, adjusted for sex, age, comorbidities, and baseline HHS (Table 5). The mean improvements in HHS were 0.9 points (CI 0.4–1.5) higher for patients with high educational level than low educational level, 0.4 points (CI 0.0–0.8) higher for patients cohabiting than living alone, and 2.6 points (CI 2.1–3.0) higher for patients with high wealth than low wealth, when adjusting for covariates.
| Crude coefficient (95% CI) | Adjusted a coefficient (95% CI) | |
| Educational level | ||
| Low | Reference | Reference |
| Medium | -1.2 (-1.7 to -0.6) | 0.5 (0.1-0.8) |
| High | -1.8 (-2.6 to -1.0) | 0.9 (0.4-1.5) |
| Cohabiting status | ||
| Alone | Reference | Reference |
| Cohabiting | -0.4 (-0.9 to 0.1) | 0.4 (0.0-0.8) |
| Other | -0.2 (-1.2 to 0.8) | 0.1 (-0.7-0.8) |
| Family wealth | ||
| Low | Reference | Reference |
| Medium | -0.5 (-1.1 to 0.1) | 1.3 (0.9-1.7) |
| High | -1.1 (-1.7 to -0.5) | 2.6 (2.1-3.0) |
| a Adjusted for sex, age, comorbidities, and baseline HHS. Coefficient refers to the β-coefficient from the multiple linear regression, which is interpreted as the degree of change in the HHS for every change in SES subgroup in the predictor variable, e.g., educational level. | ||
Multiple linear regression analyses for patients with revision THR were based on a small study cohort and are shown in Table 6 (see Supplementary data).
Missing data
The missing data analysis showed that patients without data on HHS tended to be females, were on average 3 years older, had more comorbidities, were more likely to live alone, and have higher educational level than patients with HHS data (Table 7, see Supplementary data).
Discussion
We showed that clinically relevant improvements in HHS can be expected 1 year after primary- and revision THR. However, the improvements were statistically significantly higher in patients undergoing primary THR compared with revision THR. In primary THR, better outcome in HHS was significantly associated with higher educational level, cohabiting status, and higher wealth. The poorer improvement for patients undergoing revision THR may be due to higher levels of comorbidity (Table 1). Furthermore, this could be due to a more technically demanding and longer procedure with higher rates of complications such as mechanical failures and infections. The socioeconomic inequalities between patients with low SES and high SES measured by pain and function after THR may be due to a combination of multiple factors. The fact that patients with low educational level have poorer improvements compared with patients with high educational level might be associated with medical knowledge, health literacy, patient education, and tendency to use the healthcare system. Furthermore, patients living alone may experience poorer improvements than patients cohabiting, as a result of lack of social support. Moreover, it may be more crucial for patients with low family wealth to return to work early with a possible negative effect on the physical rehabilitation, and as a consequence likely also the outcome. Of note, the results of previous studies have shown an association between SES and utilization of THR, which might indicate inequality in access to THR (15,23).
Comparison with other studies
To our knowledge, no previous studies have investigated whether changes in hip pain and disability after primary and revision THR are associated with markers of SES.
A small prospective study with 123 patients compared changes in pain and hip function after primary and revision THR over 1-year follow-up, using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) (24). Similar to our results, mean changes in pain and hip function after revision THR tended to be smaller compared with changes after primary THR. Another study with 248 patients also found similar results using WOMAC over a 4-year follow-up period (25). Patient-reported outcomes improved for primary and revision THR, and, similar to our results, improvements in hip function and activity were smaller in patients undergoing revision THR compared with patients undergoing primary THR.
In a prospective study, impact of social, educational, and occupational factors on THR outcome were investigated in 1,007 patients over a 6-month follow-up period (7). Similar to our results, the study indicated that WOMAC increased with increasing length of education and that patients living alone improved less than patients cohabiting. Another prospective study investigated the effect of social deprivation on THR outcome in 1,312 patients over a 1-year follow-up period (8). In line with our results, improvements in pain and hip function after THR were found in all deprivation categories, with greater improvements in the most affluent patients compared with the most deprived patients. In another prospective study, the influence of deprivation on hip function after THR was investigated in 1,744 patients over an 18-month follow-up (9). Similar to our findings, the patients experienced improvement in HHS. However, contrary to our findings, they did not find statistically significant differences in changes in HHS between deprivation groups. In another study, associations between socioeconomic factors and THR outcome were examined in 102 patients over 2 years and lower outcome scores were found to be associated with socioeconomic factors including low educational level and low income (10).
In summary, in line with our results, the aforementioned studies found improvements in pain and hip function after primary and revision THR with higher improvements for primary THR, and improvements were associated with SES with only a few divergent findings.
Strengths and limitations
Our study has several strengths. 1st, it was based on registry data from several registers with high completeness and long timespan (1995–2018). 2nd, SES markers were derived from Statistics Denmark on an individual basis. 3rd, HHS is a valid and reliable outcome instrument designed to investigate THR (16). 4th, applying multiple linear regression analysis enabled us to adjust for sex, age, comorbidities, and baseline HHS, which were assessed as potential confounders for the association between markers of SES and HHS.
Our study also has limitations. First, it is not compulsory to register the HHS in the DHR, which causes information on HHS to be incomplete. To investigate differences between patients with HHS and those without, a missing data analysis was performed, comparing patient characteristics. The patients without data on HHS tended to be females, were on average 3 years older, had more comorbidities, and were more likely to live alone and have higher educational level than patients with HHS data (Table 7, see Supplementary data). Females, older age, more comorbidities, and living alone were associated with poorer outcome on HHS, possibly leading to an overestimation of the HHS change score in this study. However, variables like higher educational level are associated with better outcome on HHS, pointing towards an underestimation. Therefore, the overall effect of the missing data is probably a minor overestimation of HHS change scores. Further, a sub-analysis showed that patients with missing data on only 1 of the HHS measurements (baseline or 1-year follow-up) have similar scores on HHS compared with the study population. In other words, no systematic differences were seen as to whether patients who do not have complete HHS data have better or worse function and pain than the study population. Noteworthy is that the missing data of HHS was not related to geographic location or type of hospitals, indicating that the data was missing at random, probably due to limited time at hospital visit and because the HHS is not mandatory to register in the DHR, many surgeons will omit it. Furthermore, since there has been a change from surgeon-reported to PROM generally, HHS is now used less, which may explain the fewer HHS data over time. Moreover, the change limits the possibility of comparison of this study’s results with other studies using PROMs. Information on PROMs is not available in the DHR, otherwise it would have been beneficial to use WOMAC, Oxford Hip Score (OHS), or Hip Disability and Osteoarthritis Outcome Score (HOOS) as outcome instead of HHS or as comparators of outcomes. Although a large proportion of the study population is excluded due to missing or incomplete HHS, we have justified that it is reasonable to assume that this data is missing by random. As such, our study population is comparable to the general THR patient, and therefore provides highly clinical important results.
2nd, there were missing data on SES in approximately 12% of the study population. The missing data wase equally distributed between primary and revision THR, and the majority of the missing SES data was in older patients without information on educational level. This could introduce minor selection problems, as age is associated with changes in HHS (18,19), potentially leading to a minor overestimation on the HHS change score in both groups.
3rd, it was not possible to adjust for all potential confounders in the regression models. Due to lack of data on weight and height, it was not possible to adjust for body mass index, which is partly associated with both HHS and SES (18,19). Similar, physical activity level and medication use may be other potential unmeasured confounders.
4th, although HHS is a valid instrument to evaluate outcome after THR, ceiling effects are common, which limits the validity and possibly cause an underestimation of our results (17).
5th, it was not possible to investigate changes in HHS over a longer follow-up period, possibly not presenting the full effect of the treatment for primary and revision THR. Further, there may also be difference in recovery time for primary and revision THR respectively, possibly affecting the differences in outcome for the two groups.
Sixth, it is important to acknowledge that the improvements found in this study may not only be a result of the surgeries, as regression to the mean may have had an impact on the estimates. This suggest that patients with lower baseline scores on average have a greater improvement compared with patients with higher preoperative scores. However, it was not possible to estimate the effect of regression to the mean since we had no comparable control group.
Clinical aspect
Primary and revision THR are associated with clinically relevant improvements in HHS. However, the improvements were higher in patients undergoing primary THR compared with revision THR, and the improvements tend to be even greater in patients with higher SES as compared with lower SES. Clinicians should be aware of these disparities, and patients eligible to undergo revision THR should receive appropriate information on postoperative outcome. Although the associations between markers of SES and changes in pain and hip function are only statistically significant and not clinically significant, this study provides important socioeconomic characteristics of subgroups of patients who may benefit from extra attention from healthcare professionals or community care service workers to improve outcomes after THR. By allocating more rehabilitation resources or social interventions pre- and postoperatively to patients undergoing revision THR and patients with low SES, health outcomes after surgery are likely to improve, while possibly reducing the need for future healthcare visits, readmissions, and repeated revision surgeries. This knowledge is highly important for decision-makers because it suggests how to prioritize rehabilitation to achieve equal health for all. Future studies may investigate whether stratified rehabilitation for patients with revision hip replacement is feasible and effective.
Conclusion
Patients undergoing primary and/or revision THR can expect clinically important improvements on HHS 1 year after surgery. However, higher improvement can be expected after primary THR, and the improvements are negatively related to markers of low SES, which may help to direct healthcare resources to the patients with the highest need.
- Lübbeke A, Katz J N, Perneger T V, Hoffmeyer P. Primary and revision hip arthroplasty: 5-year outcomes and influence of age and comorbidity. J Rheumatol 2007; 34: 394-400.
- Singh J A, Lewallen D G. Patient-level clinically meaningful improvements in activities of daily living and pain after total hip arthroplasty: data from a large US institutional registry. Rheumatology (Oxford) 2013; 52: 1109-18. doi: 10.1093/rheumatology/kes416.
- Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep 2014; 129(Suppl. 2): 19-31. doi: 10.1177/00333549141291s206.
- Sahni S, Talwar A, Khanijo S, Talwar A. Socioeconomic status and its relationship to chronic respiratory disease. Adv Respir Med 2017; 85: 97-108. doi: 10.5603/arm.2017.0016.
- Singh G, Jemal A. Socioeconomic and racial/ethnic disparities in cancer mortality, incidence, and survival in the United States, 1950–2014: over six decades of changing patterns and widening inequalities. J Environ Public Health 2017; 2017: 1-19. doi: 10.1155/2017/2819372.
- Minkler M, Fuller-Thomson E, Guralnik J M. Gradient of disability across the socioeconomic spectrum in the United States. N Engl J Med 2006; 355: 695-703. doi: 10.1056/NEJMsa044316.
- Schäfer T, Krummenauer F, Mettelsiefen J, Kirschner S, Günther K P. Social, educational, and occupational predictors of total hip replacement outcome. Osteoarthritis Cartilage 2010; 18: 1036-1042. doi: 10.1016/j.joca.2010.05.003.
- Clement N D, Muzammil A, Macdonald D, Howie C R, Biant L C. Socioeconomic status affects the early outcome of total hip replacement. J Bone Joint Surg Br 2011; 93: 464-9. doi: 10.1302/0301-620x.93b4.25717.
- Jenkins P J, Perry P R, Yew Ng C, Ballantyne J A. Deprivation influences the functional outcome from total hip arthroplasty. Surgeon 2009; 7: 351-6. doi: 10.1016/s1479-666x(09)80109-1.
- Allen Butler R, Rosenzweig S, Myers L, Barrack R L. The Frank Stinchfield Award: the impact of socioeconomic factors on outcome after THA: a prospective, randomized study. Clin Orthop Relat Res 2011; 469: 339-47. doi: 10.1007/s11999-010-1519-x.
- Gundtoft P H, Varnum C, Pedersen A B, Overgaard S. The Danish Hip Arthroplasty Register. Clin Epidemiol 2016; 8: 509-14. doi: 10.2147/clep.S99498.
- Danish Hip Athroplasty Register. Annual Reports; 2019. Availablke from: http://danskhoftealloplastikregister.dk/en/publications/annual-reports/.
- Schmidt M, Pedersen L, Sorensen H T. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol 2014; 29: 541-9. doi: 10.1007/s10654-014-9930-3.
- Schmidt M, Schmidt S A, Sandegaard J L, Ehrenstein V, Pedersen L, Sorensen H T. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 2015; 7: 449-90. doi: 10.2147/clep.S91125.
- Edwards N, Varnum C, Overgaard S, Pedersen A. The impact of socioeconomic status on the utilization of total hip arthroplasty during 1995–2017: 104,055 THA cases and 520,275 population controls from national databases in Denmark. Acta Orthop 2021; 92(1): 29-35. doi: 10.1080/17453674.2020.1840111.
- Söderman P, Malchau H. Is the Harris hip score system useful to study the outcome of total hip replacement? Clin Orthop Relat Res 2001; (384): 189-97. doi: 10.1097/00003086-200103000-00022.
- Wamper K E, Sierevelt I N, Poolman R W, Bhandari M, Haverkamp D. The Harris hip score: Do ceiling effects limit its usefulness in orthopedics? Acta Orthop 2010; 81: 703-7. doi: 10.3109/17453674.2010.537808.
- Buirs L D, Van Beers L W, Scholtes V A, Pastoors T, Sprague S, Poolman R W. Predictors of physical functioning after total hip arthroplasty: a systematic review. BMJ Open 2016; 6: e010725. doi: 10.1136/bmjo-pen-2015-010725.
- Dowsey M M, Nikpour M, Choong P F. Outcomes following large joint arthroplasty: does socio-economic status matter? BMC Musculoskelet Disord 2014; 15: 148. doi: 10.1186/1471-2474-15-148.
- Agabiti N, Picciotto S, Cesaroni G, Bisanti L, Forastiere F, Onorati R, et al. The influence of socioeconomic status on utilization and outcomes of elective total hip replacement: a multicity population-based longitudinal study. Int J Qual Health Care 2007; 19: 37-44. doi: 10.1093/intqhc/mzl065.
- Santaguida P L, Hawker G A, Hudak P L, Glazier R, Mahomed N N, Kreder H J, et al. Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review. Can J Surg 2008; 51: 428-36.
- Schmolders J, Friedrich M J, Michel R, Strauss A C, Wimmer M D, Randau T M, et al. Validation of the Charlson comorbidity index in patients undergoing revision total hip arthroplasty. Int Orthop 2015; 39: 1771-7. doi: 10.1007/s00264-015-2810-y.
- Wetterholm M, Turkiewicz A, Stigmar K, Hubertsson J, Englund M. The rate of joint replacement in osteoarthritis depends on the patient’s socioeconomic status. Acta Orthop 2016; 87: 245-51. doi: 10.3109/17453674.2016.1161451.
- Lenguerrand E, Whitehouse M R, Wylde V, Gooberman-Hill R, Blom A W. Pain and function recovery trajectories following revision hip arthroplasty: short-term changes and comparison with primary hip arthroplasty in the ADAPT Cohort Study. PLoS One 2016; 11: e0164839. doi: 10.1371/journal.pone.0164839.
- Postler A E, Beyer F, Wegner T, Lützner J, Hartmann A, Ojodu I, et al. Patient-reported outcomes after revision surgery compared to primary total hip arthroplasty. Hip Int 2017; 27: 180-6. doi: 10.5301/hipint.5000436.
Supplementary data
| Crude coefficient (95% CI) | Adjusted a coefficient (95% CI) | |
| Educational level | ||
| Low | Reference | Reference |
| Medium | -0.7 (-5.3-3.9) | -0.1 (-2.6-2.4) |
| High | 1.5 (-5.2-8.1) | 4.8 (1.1-8.5) |
| Cohabiting status | ||
| Alone | Reference | Reference |
| Cohabiting | 2.7 (-2.0-7.5) | 0.5 (-2.3-3.3) |
| Other | 5.4 (-3.5-14) | 3.0 (-1.8-7.9) |
| Family wealth | ||
| Low | Reference | Reference |
| Medium | 1.2 (-3.9-6.4) | -0.4 (-3.3-2.5) |
| High | -2.5 (-7.5-2.6) | 1.1 (-2.0-4.1) |
| a Adjusted for sex, age, comorbidities, and baseline HHS. Coefficient refers to the β-coefficient from the multiple linear regression, which is interpreted as the degree of change in the HHS for every change in SES subgroup in the predictor variable, e.g., educational level. | ||