Rapid rise in prevalence of knee replacements and decrease in revision burden over past 3 decades in Finland: a register-based analysis
Konsta J PAMILO 1, Jaason HAAPAKOSKI 2, Tuulikki SOKKA-ISLER 3,4, Ville REMES 5,6, and Juha PALONEVA 3,4
1 Coxa Hospital for Joint Replacement, Tampere; 2 National Institute for Health and Welfare, Helsinki; 3 Hospital Nova of Central Finland, Central Finland Health Care District, Jyväskylä; 4 University of Eastern Finland, Kuopio; 5 SYNLAB Suomi, Helsinki; 6 Jokilaakso Hospital, Jämsä, Finland
Background and purpose — The prevalence of knee joint replacements (KJR) has been less investigated in situations where the increase in incidence is known. This study investigated the annual and population-based prevalence of KJR and the relationship between the prevalence of KJRs and the incidence of revision surgery.
Patients and methods — All KJRs performed between 1980 and 2020 were identified from the Finnish Arthroplasty Register (FAR). KJR revisions and removals were extracted from the FAR and hospital discharge registers and patient deaths from Finnish Digital and Population Data Services Agency. We analyzed the annual prevalence by dividing the number of KJR survivors by the population aged 40 or older. The revision burden factor (RBF) was determined by dividing the annual number of revisions by the number of primary and revision KJRs in the population. Proportions of bilateral implants and patients with older KJRs performed 10 or more years earlier were identified.
Results — KJR prevalence in Finland increased by 298% between 2000 and 2020, reaching 4.0% in 2020. The proportion of patients with bilateral KJRs and those with older KJRs had increased to 37% and 34%, respectively, by 2020. The annual RBF decreased statistically significantly from 1.9% to 0.7% between 1996 and 2020 (proportion ratio, PR 0.37 [95% CI 0.33–0.42]) and was higher among males (PR 1.23 [CI 1.20–1.26]).
Interpretation — Although the recent rapid increase in KJRs is abating and the RBF is diminishing, it is important to take the continuing increase in the prevalence of KJRs into account when assessing hospitals’ future resources.
Citation: Acta Orthopaedica 2022; 93: 382–389. DOI http://dx.doi.org/10.2340/17453674.2022.2266.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2021-09-14. Accepted: 2022-02-17. Published: 2022-04-06.
Correspondence: konsta.pamilo@kolumbus.fi
KJP, JH, TSI, VR, and JP wrote the manuscript. JH performed the data analysis. All contributed to the conception and design of the study, critical analyses of the data, interpretation of the findings, and critical revision of the manuscript.
The authors would like to thank Mikko Peltola from the National Institute for Health and Welfare for his comments on the manuscript.
Acta thanks Ove Furnes and Rob Nelissen for help with peer review of this study.
Knee joint replacement (KJR) surgery involves risks such as bacterial infection, aseptic loosening, patellar or tibiofemoral instability, polyethylene dislocation, polyethylene wear-induced osteolysis, and fractures, all of which also often require revision surgery.
In the United States, depending on the modeling method used, the need for KJR surgery in 2050 is predicted be 143–855% higher than in 2012 (1). Other studies have also projected a substantial increase in the future incidence of KJR (2,3). In Finland, the incidence of KJR surgery has increased, especially in the younger age groups (4,5).
Incidence is useful in assessing the burden of early revisions. However, prevalence may be more important when assessing the overall future burden of KJR revisions. The incidence of revisions may increase due not only to the increase in the number of KJRs, but also to the lower mean age of patients at the time of surgery and the longer life expectancy of patients with implants. The increasing prevalence of obesity may also have an effect on the incidence of KJR revisions by increasing both KJR need and infection revision risk (6-8).
Data on the prevalence of KJR is limited (9-11). The only statistics not based on mathematical estimates are those that have been published annually since 2003 in the Swedish Knee Arthroplasty Register. In 2020, the register reported peak prevalence at age 80–85 years, with 10% of women and 8% of men having received at least one KJR and 25% of patients bilateral implants (11).
By combining data from nationwide registers, we sought to determine the annual prevalence of KJRs and revision burden in Finland.
Patients and methods
All public and private hospitals in Finland are obliged to report all arthroplasties to the Finnish Arthroplasty Register (FAR) and all surgical procedures to the National Institute for Health and Welfare. This study is based on 3 registers: the Finnish Arthroplasty Register (FAR), Finnish Hospital Discharge Register (FHDR), both maintained by the National Institute for Health and Welfare, and the Finnish Population Information System maintained by the Digital and Population Services Agency. These registers are regulated by law and tests have been performed to ensure their reliability (12-14).
The study population was formed by extracting from the FAR all primary total knee replacements (TKRs), unicompartmental arthroplasties (UKAs), and patellofemoral arthroplasties (PFAs) reported since 1980. Revision knee replacement operations and KJR removals were identified from the FAR and from 1996 onwards double checked in the FHDR, applying the following criteria drawn from the Finnish version of the Nordic Medico-Statistical Committee (NOMESCO): NGC00–NGC99 (including addition of patellar component) for revision knee replacements and NGU00 for removals of knee replacements. All KJR removals were accounted as revision surgery.
We excluded patients who were residents of Åland (0.5% of the population), not Finnish citizens, or were reported with an incorrect personal ID. Although the first KJRs were performed, if rarely, in the 1970s, we could not include them as they were not reported in the registers used in this study. Moreover, accurate annual mortality statistics have been available only since 1987. Thus, the annual prevalence of KJRs before 1990 is not reported here or compared with that in later years.
Data on patient deaths and statistics on the general population was requested from the Digital and Population Data Services Agency. The prevalence of KJR was defined as the proportion of primary or revision KJR survivors (on December 31 in each study year) of the general population aged 40 years or more, irrespective of how long ago the initial procedure was performed. The total number of KJRs is also given. The prevalence and revision incidence were stratified by year, age group (< 55, 55–64, 65–74, and ≥ 75 years) and sex. The prevalence in each age group was calculated by dividing the number of individuals with 1 or 2 KJRs (TKR, UKA, or PFA) by the same-age general population on December 31 of the same year. In addition, the prevalence of bilateral KJRs and prevalence of subjects with an older KJR (KJR operation performed more than 10 years earlier) were calculated separately.
To calculate the incidence of annual revision KJRs, searches for revision KJR (including additions) and KJR removal were conducted in both the FAR and FHDR using the above-mentioned NOMESCO codes. The proportions of revision and infection revision KJRs reported in the FHDR but not FAR are given in Figure 1 (see Supplementary data). The revision burden factor (RBF) was defined as the annual number of revisions divided by the annual total number of primary and revision KJRs in the population. The annual proportion of infection revisions in the KJR (primary and revision) population (infection RBF) was also calculated. It was considered that the revision was due to deep infection if infection was reported as the indication for revision in the FAR or if the revision was associated with the code for infection of the endoprosthesis or postoperative infection (ICD-10 codes T84.5 or T81.4).
Statistics
Prevalences and RBFs are expressed as binomial proportions. Adjusted ratios of proportions (PR) between any 2 groups and their 95% confidence intervals (CI) were estimated by generalized linear models (GLM) with binomial distribution and log-link. Proportions were considered as dependent variables, and population counts (denominators) were treated as prior weights. Age and sex were adjusted for by including them as covariates in the model when studying calendar time trends. Age and time were similarly adjusted for when analyzing ratios between men and women. Patient age group at the end of each year was also treated as a factor. Calculations were performed using the function glm in R stats package version 4.0.0 (15).
Ethics, data sharing, funding, and potential conflicts of interest
Permission for the study was obtained from each register. No ethical permission was required to perform this registry study. Data sharing can be made available on request to the corresponding author. Grants for the study were received from the Finnish Rheumaorthopedic Society and the Finnish Medical Research Foundation. No conflicts of interest are declared.
Results
Prevalence of KJRs
The prevalence of KJRs in the general population increased annually during the study period (Figure 2 and Figure 3 in Supplementary data). However, the annual increase in prevalence decelerated among both females and males and in each age group (Figure 4 and Figure 5 in Supplementary data). Prevalence was 1.1% in 2000, 2.6% in 2010, and 4.0% in 2020. Thus, between 2000 and 2020, prevalence rose by 270% and between 2010 and 2020 by 56%. The total number of KJR implants in the study population increased from 7,535 in 1990 to 34,884 in 2000 and thereafter to 162,711 in 2020. The population of inhabitants aged 40 years or over in Finland was 2,210,500 in 1990, 2,541,055 in 2000, and 2,977,677 in 2020. In 2020, the prevalence of KJR in females was 5.0% and thus statistically significantly higher than the 2.8% in males (age- and time-adjusted proportion ratio (PR) 0.57 (CI 0.57–0.57). In 2020, the prevalence peaked in the group aged 75 years or older at 11.6% for females and 8.0% for males. A statistically significant increase in prevalence was seen in all age groups during the study period. The prevalence of KJR by sex and age group is presented in Figure 3 (see Supplementary data) and goodness-of-fit of the models in Figure 6 (see Supplementary data).
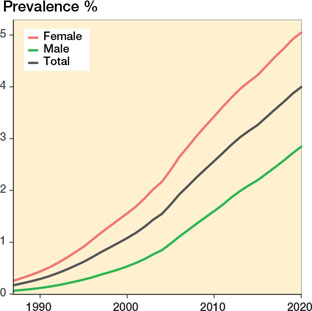
Figure 2. Prevalence of KJRs (patients with ipsilateral or bilateral implants) in the population aged 40 years or older. Between 1990 and 2020, the total number of KJRs increased from 7,535 to 162,711 and the number of patients with KJR from 6,447 to 118,982.
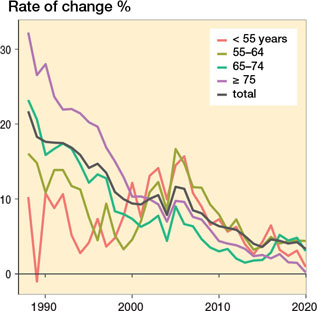
Figure 4. Annual rate of change in the prevalence of KJRs (patients with 1 or 2 KJRs) in the population by age group. Note: The acceleration of this change between 2004 and 2005 is explained by the deadlines for non-urgent surgery set by the Finnish government in 2005.
The proportion of bilateral KJRs in the KJR population increased during the study period, reaching 38% for females and 36% for males in 2020, and was more pronounced in the early study period (Figure 7). The proportion of bilateral KJRs increased in all age groups except the under 55s.
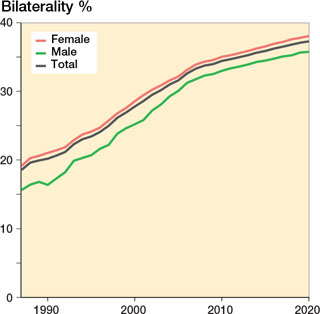
Figure 7. Percentage of bilateral KJRs by sex and in total. Between 1990 and 2020, the number of patients with bilateral KJRs increased from 1,301 to 44,350.
Prevalence of patients with older KJRs
In 1990, the first KJRs were already at least 10 years old. During the study period, the annual proportion of KJR patients with a KJR performed at least 10 years earlier showed a significant increase in each decade: from 11% in 2000 to 19% in 2010 and 34% in 2020 (Figure 8). Older KJRs were more common in females than males (age- and time-adjusted PR 1.22 [CI 1.21–1.23]). In 2020, 29% of male and 36% of female patients had an older KJR, with the highest proportions of older KJRs occurring in those aged 75 or older: 42% in males and 48% in females. After 1990, the prevalence of individuals with an older KJR continued to rise, reaching 1.3% in 2020.
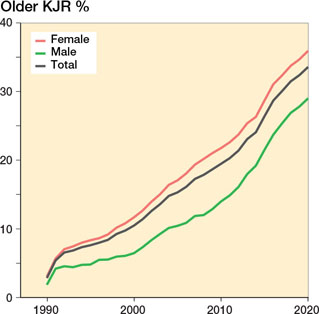
Figure 8. Proportions of patients with KJR received over 10 years earlier (older KJR) in the total KJR population by sex and in total. Between 1990 and 2020, the total number of patients with KJR received over 10 years earlier increased from 184 to 39,970.
Revision burden factor (RBF)
Revisions from 1996 were double-checked from the FAR and FHDR. The annual number of KJR revisions increased from 399 to 1,086 between 1996 and 2020. The proportion of revisions reported only in the FHDR are given in Figure 1 (see Supplementary data). We also evaluated the coverage of the FAR from 1987 and 1995 to be between 88% and 97% (data not shown). RBF was 1.5% in 1990 and 2.0% in 1998. Between 1998 and 2020 this ratio decreased to 0.7%. The decrease from 1.2% to 0.7% between 2010 and 2020, however, remained significant (age- and sex-adjusted PR 0.56 [CI 0.51–0.60]). The annual RBFs and prevalence ratios with CIs are presented in Figure 9 and Figure 10 in Supplementary data. Between 1998 and 2020, the RBF decreased in the female KJR population from 1.8% to 0.6% (age-adjusted PR 0.32 [CI 0.28–0.36]) and in the male KJR population from 2.4% to 0.8% (age-adjusted PR 0.36 [CI 0.30–0.43]). The RBF was higher in the male than female population (age- and time-adjusted PR 1.23 [CI 1.20–1.26]). From 2009 onwards, the RBF was lower the older the age group (Table).
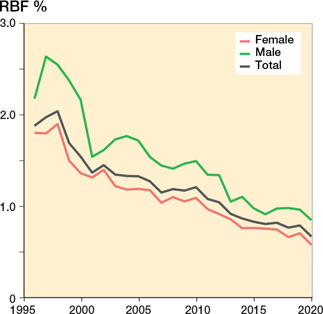
Figure 9. Revision burden factor (RBF) by sex and in total (annual number of revisions divided by annual total number of KJRs in the population). The total annual number of revisions increased from 113 to 1,086 between 1990 and 2020.
The infection revision burden factor ranged between 0.2% and 0.4% during 1996–2016, since when it has remained around 0.3%. No significant change between 1996 and 2020 was found except for the years 2011, 2012, and 2015, when the infection RBF was statistically significantly lower than in 1996 (Figure 11 and Figure 12 in Supplementarydata). The infection RBF was higher in males than in females: in 2020, it was 0.2% in females and 0.5% in males (age- and time-adjusted PR 1.23 [CI 1.18–1.27]; Figure 11).
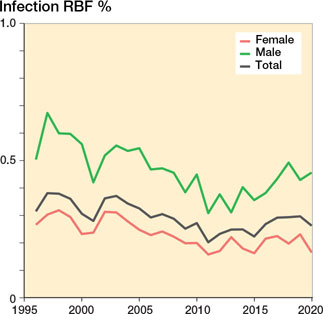
Figure 11. Infection revision burden factor (infection RBF) by sex and in total (annual number of revisions performed due to infection divided by annual total number of KJRs in the population). The total number of annual infection revision KJRs increased from 67 to 428 between 1996 and 2020.
Discussion
Our main observation was that the prevalence of KJRs and of subjects with older KJRs increased rapidly throughout the study period, while the revision burden factor decreased.
| Age group | PR (95% CI) |
| < 55 | 1 (references) |
| 55–64 | 0.53 (0.50–0.57) |
| 65–74 | 0.37 (0.35–0.40) |
| ≥ 75 | 0.20 (0.19–0.22) |
Prevalence of KJRs
In 2020, 12,702 primary KJRs and 990 revision KJRs were reported to FAR (16). An increasing incidence of KJR (number of new cases relative to the population) has previously been reported (5) and it has also been estimated that the annual need for primary knee replacement will substantially increase (1,2,17), including among young patients (4). On the other hand, the increase in the incidence of KJR surgery has shown signs of slowing down (18,19). The incidence of KJR is useful when assessing the need for annual primary KJRs, early revisions, and early unplanned revisits. However, little is known about the prevalence of KJR, which may be more useful when assessing the overall burden of KJR revisions, revisits, and follow-up visits. In a US cohort study, the prevalence of individuals over age 50 living with a KJR was estimated to be about 4.2% in 2009 (9). In turn, Maradit Kremers et al. (10) estimated the total prevalence of knee replacement in the same age group to be 4.6% in 2010. Both studies reported a higher prevalence in females than males. Weinstein et al. (9) estimated a prevalence of 3.4% in males and 4.8% in females aged 50 or older. This is in line with our finding of 4.0% in the over-40s in 2020. We also found a higher prevalence in females (5.0%) than males (2.8%). This is also consistent with the higher prevalence of knee OA among females. In the Health 2000 Survey (2000–2002), the prevalence of symptomatic knee osteoarthritis (OA) was estimated to be 6% in males and 8% in females aged 30 or over (20). Assuming the prevalence of OA has remained the same, a significant proportion of knee OA patients will have received a KJR in 2020. This may explain our finding of a deceleration in the increase in prevalence as the amount of care debt has decreased. Our finding of a higher prevalence in females is also consistent with previous studies showing a higher incidence and lifetime risk of KJR in females (5,21).
This study demonstrates that the annual prevalence of KJR and the number of KJRs has increased rapidly. Between 2010 and 2020, the overall prevalence of KJR increased by 56% and an increase was seen in all 4 age groups. The Swedish Knee Arthroplasty Register has also reported an increased annual prevalence in all age groups (11). In the latest report (2020), the 80- to 85-year-olds showed the highest prevalence, with almost 10% of women and 8% of men having at least 1 knee replacement. This accords with our finding of the highest prevalence (12% in females and 8% in males) in those aged 75 or older in 2020. The proportion of bilateral cases also increased during the study period, reaching 37% in 2020. The Swedish Knee Arthroplasty Register reported the proportion of bilateral cases to be 25% in 2019 (11). In Finland, the incidence of KJRs increased during the period 1998–2006 and again after 2015 (5,16), as also did life expectancy and the mean age of the population (22). The last-mentioned explains, at least partially, the increase in the prevalence of KJR. One potential explanation for the increase in incidence in Finland could be increased obesity (6), a known risk factor for knee osteoarthritis. A multicenter study in the United States reported that 26% of KJRs were likely to have been performed based on inappropriate indications (23). Thus, it is possible that good KJR outcomes have led to KJRs being performed applying less stringent criteria than in previous years.
Compared with the other Nordic countries, KJR prevalence rates may be a little higher in Finland since KJR incidence (number of new KJRs per population) is also higher (5). In addition, the lifetime risk of KJR (probability of having KJR over an individual’s lifetime) is higher in Finland (especially in the female population) than in the other Nordic countries or in Australia (21).
Revision burden factor (RBF)
The revision burden has been defined as the percentage of revision arthroplasties relative to the total number of primary and revision arthroplasties (24,25). Similarly, the infection burden has been defined as the number of KJR revisions performed due to infection divided by the total number of primary and revision arthroplasties in a given period (26).We defined RBF as the ratio of the annual number of revision KJRs to the total number of KJRs in the population. This definition has not previously been used. We found that the proportion of persons with older KJRs increased during the study period, while the revision burden factor decreased slightly. A few possible reasons for this can be suggested: the number of re-revisions has decreased, KJRs last longer, and early revisions after KJR have been less needed. The indications for revision surgery have likely changed over time, especially owing to a decreased willingness to perform revisions due to patellofemoral pain or pain due to an undetermined cause. While a reduction in the incidence of PFAs with higher revision risk could explain the decrease in RBF, this is not the case in Finland, as the proportion of PFAs in all KJRs has increased slightly. Moreover, the proportion of PFAs was only 0.7% between 2006 and 2016 in Finland (27).
Centralizing KJR operations in higher volume hospitals could explain the decrease in the need for KJR revisions. However, findings on the association between hospital volume and revision rate after TKR are conflicting (28,29). In Finland, lower hospital volume is not unambiguously associated with a higher TKR revision rate (19). It is also possible that process standardization such as fast-track (enhanced recovery) could lessen the need for revisions. However, no significant difference in revision rates before and after fast-track KJR has been found (30,31). Other explanatory factors may be the national guidelines for TKR surgery published in 2010 and 2015, and a possible increase in the annual volume of surgeons’ procedures over time.
The increasing prevalence of obesity may affect revision risk due to infections (6-8). However, since no significant change was observed in the infection RPF between 1996 and 2020, the decrease in the RBF is due to a diminution in revisions performed for reasons other than infection. This finding is supported by Dyrhovden et al. (32), who found that while revision risk after TKR had decreased, revision risk due to early infection had increased. They proposed that possible reasons are better polyethylene and more patella-friendly prosthetic designs (32). It is possible that the effect on the RBF of early revisions is greater than that of late revisions, because the RBF was higher in the younger age groups, which also had a lower proportion of individuals with an older KJR. However, one reason is the higher revision incidence in the younger age groups reported by FAR (16). The infection revision burden was also statistically significantly higher for males than females. This supports previous studies that have shown an increased infection risk after KJR in males (33-36). Springer et al. (26) combined data from six registers and found an increase in the infection revision burden for KJR between 2010 and 2015. In our study, the infection RBF did not increase during the corresponding period. Under-reporting of infections in our study is an unlikely explanation for this difference between our study and that of Springer et al. (26), as we double-checked the FHDR against the FAR for the number of infection revisions. One reason for this difference is that the infection RBF takes into account all persons with KJR, irrespective of how long ago the surgery was done, whereas the infection burden is calculated based solely on the KJRs performed during the same year.
In our study, the prevalence of patients with an older KJR increased, reaching 1.3% in 2020. The proportion of patients with an older KJR among the total number of patients with KJRs had risen to 34% in 2020. Maradit Kremers et al. (10) estimated that in 2010, 28% of individuals in the total knee replacement (TKR) prevalence pool had a TKR that had been performed over 10 years earlier.
The increasing number of KJRs will cause healthcare systems more costs, not only from primary operations but also from unplanned revisits due to KJR-related problems, follow-up visits, and revisions. Every effort must be made to decrease the risks for revision KJRs by selecting patients who fulfil the appropriate indications and by preoperatively optimizing modifiable factors that are known to affect revision risk (37).
Limitations
The level of completeness and accuracy of the FHDR is good. More than 95% of discharges can be found in this register (12,14). The coverage of primary KJRs in the FAR is also good (89–97%) (12,16). In our study, the percentages of revisions reported solely in the FHDR, and hence not in the FAR, are given in Figure 1 (see Supplementary data. We also estimated the coverage of the FAR to be between 88% and 97% between 1987 and 1995 (data not shown). The strength of our study is the inclusion of data from all the private and public hospitals in Finland. We also took patient deaths into account.
The first operation of a 2-stage infection revision is often reported with the code NGU00 (removal of KJR). Patients who do not undergo the intended reimplantation (second stage) continue living with spacer implants while those who undergo reimplantation continue with new TKRs. Thus, removals of KJRs were taken into account only for revisions but not for calculations of prevalence. We assumed that the annual number of patients left without any knee implant was low. This may have induced upward bias in our prevalence estimates. However, the bias resulting from excluding these patients would bias our results even more. Amputations and knee arthrodesis without reported removals were excluded. This degree of bias will be small, as the number of amputations and knee arthrodesis procedures after KJR is generally also low. In addition, mortality after a trans-femoral amputation is high (38,39).
The coverage of revision KJRs in the FAR is somewhat lower than that of primary KJRs. To minimize the risk of bias arising from this, RBF searches for revision KJR (including additions) and KJR removal were conducted in both the FAR and FHDR. In Denmark, a discrepancy in the number of infection revisions between the national arthroplasty register and microbiology database has been shown by Gundtoft et al. (40). In Finland, infection revisions are occasionally performed in some hospitals by orthopedic surgeons not familiar with the FAR’s online reporting program, leading to under-reporting. In addition, it takes time for bacterial cultures to be identified, and thus an infection diagnosis is not always known in the operating room, where the FAR report is filed. To minimize this risk of bias arising from the FAR, we double-checked the FAR data against the FHDR data, including for infection revisions.
In Finland, the first KJRs were performed in the 1970s. We did not have data on these operations. Thus, our prevalence rates in the early study period are downward biased. However, after 1990 this downward bias is negligible as KJR operations were rare in the 1970s and the survival rates of KJRs were lower. In addition, patient deaths and the rapid rise in prevalence reduces the bias introduced by those early operations.
Conclusion
The continuing rapid increase in the prevalence of KJRs poses a challenge for healthcare due to both KJR-related problems and the long-term follow-up of KJRs. This is exacerbated by the increasing prevalence in the younger age group and increasing proportion of older KJRs. The reduction in the revision burden factor is a positive sign.
- Inacio M C S, Paxton E W, Graves S E, Namba R S, Nemes S. Projected increase in total knee arthroplasty in the United States: an alternative projection model. Osteoarthritis Cartilage 2017; 25(11): 1797-803. doi: 10.1016/j.joca.2017.07.022.
- Ackerman I N, Bohensky M A, Zomer E, Tacey M, Gorelik A, Brand C A, et al. The projected burden of primary total knee and hip replacement for osteoarthritis in Australia to the year 2030. BMC Musculoskelet Disord 2019; 20(1): 90. doi: 10.1186/s12891-019-2411-9.
- Sloan M, Premkumar A, Sheth N P. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am 2018; 100(17): 1455-60. doi: 10.2106/JBJS.17.01617.
- Leskinen J, Eskelinen A, Huhtala H, Paavolainen P, Remes V. The incidence of knee arthroplasty for primary osteoarthritis grows rapidly among baby boomers: a population-based study in Finland. Arthritis Rheumatism 2012; 64(2): 423-8. doi: 10.1002/art.33367;10.1002/art.33367.
- Niemeläinen M J, Mäkelä K T, Robertsson O, W-Dahl A, Furnes O, Fenstad A M, et al. Different incidences of knee arthroplasty in the Nordic countries. Acta Orthop 2017; 88(2): 173-8. doi: 10.1080/17453674.2016.1275200.
- Koskinen S, Sääksjärvi K, Lundqvist A, Borodulin K, Koponen P. FinnTerveys2017—tukimus [Online] 2018 [cited 2020 Jan 19]. p 45-9. Available from: http://www.julkari.fi/bitstream/handle/10024/136223/pubmedRap_4_2018_FinTerveys_verkko.pdf?sequence=1&isAllowed=y
- Sezgin E A, W-Dahl A, Lidgren L, Robertsson O. Weight and height separated provide better understanding than BMI on the risk of revision after total knee arthroplasty: report of 107,228 primary total knee arthroplasties from the Swedish Knee Arthroplasty Register 2009-2017. Acta Orthop 2020; 91(1): 94-7. doi: 10.1080/17453674.2019.1688006.
- Overgaard A, Frederiksen P, Kristensen L E, Robertsson O, W-Dahl A. The implications of an aging population and increased obesity for knee arthroplasty rates in Sweden: a register-based study. Acta Orthop 2020; 91(6): 738-42. doi: 10.1080/17453674.2020.1816268.
- Weinstein A M, Rome B N, Reichmann W M, Collins J E, Burbine S A, Thornhill T S, et al. Estimating the burden of total knee replacement in the United States. J Bone Joint Surg Am 2013; 95(5): 385-92. doi: 10.2106/JBJS.L.00206.
- Maradit Kremers H, Larson D R, Crowson CS, Kremers W K, Washington R E, Steiner C A, et al. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am 2015; 97(17): 1386-97. doi: 10.2106/JBJS.N.01141.
- Robertsson O, W-Dahl A, Lidgren L, Sundberg M. Annual Report 2020, Swedish Knee Arthroplasty Register. Lund; 2020. https://www.myknee.se/pdf/SVK_2020_Eng_1.0.pdf
- Turppo V, Sund R, Sirola J, Kröger H, Huopio J. Cross-validation of arthroplasty records between arthroplasty and hospital discharge registers, self-reports, and medical records among a cohort of 14,220 women. J Arthroplasty 2018; 33(12): 3649-54. doi: 10.1016/j.arth.2018.08.010.
- Sokka T. National databases and rheumatology research I: longitudinal databases in Scandinavia. Rheum Dis Clin North Am 2004; 30(4): 851-67, viii. doi: 10.1016/j.rdc.2004.07.002.
- Sund R. Quality of the Finnish Hospital Discharge Register: a systematic review. Scand J Public Health 2012; 40(6): 505-15. doi: 10.1177/1403494812456637.
- DataCamp. glm:Fitting Generalized Linear Models [Online]. Version 3.6.2 2021 [cited 2021 Jun 7]. Available from: https://rdocumentation.org/packages/stats/versions/3.6.2/topics/glm
- FAR. Finnish Arthroplasty Register [Online]. National Institute for Health and Welfare; 2021. Available from: https://www.thl.fi/far//#data/cphd
- Nemes S, Rolfson O, W-Dahl A, Garellick G, Sundberg M, Kärrholm J, et al. Historical view and future demand for knee arthroplasty in Sweden. Acta Orthop 2015; 86(4): 426-31. doi: 10.3109/17453674.2015.1034608.
- Bini S A, Sidney S, Sorel M. Slowing demand for total joint arthroplasty in a population of 3.2 million. J Arthroplasty 2011; 26(6 Suppl): 124-8. doi: 10.1016/j.arth.2011.03.043.
- Pamilo K J, Peltola M, Paloneva J, Mäkelä K, Häkkinen U, Remes V. Hospital volume affects outcome after total knee arthroplasty: a nationwide registry analysis of 80 hospitals and 59,696 replacements. Acta Orthop 2015; 86(1): 41-7. doi: 10.3109/17453674.2014.977168.
- Arokoski J, Manninen P, Kröger H, Heliövaara M, Nykyri E, Impivaara O. Hip and knee pain and osteoarthritis. In: Kaila-Kangas L, editor. Musculoskeletal disorders and diseases in Finland: results of the Health 2000 Survey. KTL B25/20. Helsinki: National Public Health Institute; 2007. p 37-41.
- Ackerman I N, Bohensky MA, de Steiger R, Brand CA, Eskelinen A, Fenstad A M, et al. Substantial rise in the lifetime risk of primary total knee replacement surgery for osteoarthritis from 2003 to 2013: an international, population-level analysis. Osteoarthritis Cartilage 2017; 25(4): 455-61. doi: 10.1016/j.joca.2016.11.005.
- Statistics Finland. Statistic Finland [Online]. Statistic Finland 2020 [cited 2020 Jan 19]. Available from: https://www.tilastokeskus.fi/tup/suoluk/suoluk_vaesto.html
- Ghomrawi H M K, Mushlin A I, Kang R, Banerjee S, Singh J A, Sharma L, et al. Examining timeliness of total knee replacement among patients with knee osteoarthritis in the U.S.: results from the OAI and MOST Longitudinal Cohorts. J Bone Joint Surg Am 2020 Jan. doi: 10.2106/JBJS.19.00432.
- Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002 J Bone Joint Surg Am 2005; 87(7): 1487-97. doi: 87/7/1487.
- Malchau H, Herberts P, Eisler T, Garellick G, Söderman P. The Swedish Total Hip Replacement Register. J Bone Joint Surg Am 2002; 84-A(Suppl,): 2-20.
- Springer B D, Cahue S, Etkin C D, Lewallen D G, McGrory B J. Infection burden in total hip and knee arthroplasties: an international registry-based perspective. Arthroplasty Today 2017; 3(2): 137-40. doi: 10.1016/j.artd.2017.05.003.
- Lewis P L, Tudor F, Lorimer M, McKie J, Bohm E, Robertsson O, et al. Short-term revision risk of patellofemoral arthroplasty is high: an analysis from eight large arthroplasty registries. Clin Orthop Relat Res 2020; 478(6): 1222-31. doi: 10.1097/CORR.0000000000001268.
- Badawy M, Espehaug B, Indrekvam K, Engesaeter L B, Havelin L I, Furnes O. Influence of hospital volume on revision rate after total knee arthroplasty with cement. J Bone Joint Surg Am 2013; 95(18): e1311-6. doi: 10.2106/JBJS.L.00943.
- Bozic K J, Maselli J, Pekow P S, Lindenauer P K, Vail T P, Auerbach A D. The influence of procedure volumes and standardization of care on quality and efficiency in total joint replacement surgery. J Bone Joint Surg Am 2010; 92(16): 2643-52. doi: 10.2106/JBJS.I.01477.
- Pamilo K J, Torkki P, Peltola M, Pesola M, Remes V, Paloneva J. Fast-tracking for total knee replacement reduces use of institutional care without compromising quality. Acta Orthop 2018; 89(2): 184-9. doi: 10.1080/17453674.2017.1399643.
- Glassou E N, Pedersen A B, Hansen T B. Risk of re-admission, reoperation, and mortality within 90 days of total hip and knee arthroplasty in fast-track departments in Denmark from 2005 to 2011. Acta Orthop 2014; 85(5): 493-500. doi: 10.3109/17453674.2014.942586.
- Dyrhovden G S, Lygre S H L, Badawy M, Gøthesen Ø, Furnes O. Have the causes of revision for total and unicompartmental knee arthroplasties changed during the past two decades? Clin Orthop Relat Res 2017; 475(7): 1874-86. doi: 10.1007/s11999-017-5316-7.
- Jung P, Morris A J, Zhu M, Roberts S A, Frampton C, Young S W. BMI is a key risk factor for early periprosthetic joint infection following total hip and knee arthroplasty. N Z Med J 2017; 130(1461): 24-34.
- Tayton E R, Frampton C, Hooper G J, Young S W. The impact of patient and surgical factors on the rate of infection after primary total knee arthroplasty: an analysis of 64,566 joints from the New Zealand Joint Registry. Bone Joint J 2016; 98-B(3): 334-40. doi: 10.1302/0301-620X.98B3.36775.
- Jämsen E, Huhtala H, Puolakka T, Moilanen T. Risk factors for infection after knee arthroplasty: a register-based analysis of 43,149 cases. J Bone Joint Surg Am 2009; 91(1): 38-47. doi: 10.2106/JBJS.G.01686.
- Namba R S, Inacio M C S, Paxton E W. Risk factors associated with deep surgical site infections after primary total knee arthroplasty: an analysis of 56,216 knees. J Bone Joint Surg Am 2013; 95(9): 775-82. doi: 10.2106/JBJS.L.00211.
- Jämsen E, Peltola M, Eskelinen A, Lehto M U K. Comorbid diseases as predictors of survival of primary total hip and knee replacements: a nationwide register-based study of 96 754 operations on patients with primary osteoarthritis. Ann Rheum Dis 2013; 72(12): 1975-82. doi: 10.1136/annrheumdis-2012-202064.
- Ryan S P, DiLallo M, Klement M R, Luzzi A J, Chen A F, Seyler T M. Transfemoral amputation following total knee arthroplasty: mortality and functional outcomes. Bone Joint J 2019; 101-B(2): 221-6. doi: 10.1302/0301-620X.101B2.BJJ-2018-0784.R1.
- Fard B, Dijkstra P U, Voesten H G J M, Geertzen J H B. Mortality, reamputation, and preoperative comorbidities in patients undergoing dysvascular lower limb amputation. Ann Vasc Surg 2019; doi: 10.1016/j.avsg.2019.09.010.
- Gundtoft P H, Pedersen A B, Schønheyder HC, Overgaard S. Validation of the diagnosis “prosthetic joint infection” in the Danish Hip Arthroplasty Register. Bone Joint J 2016; 98-B(3): 320-5. doi: 10.1302/0301-620X.98B3.36705
Supplementary data
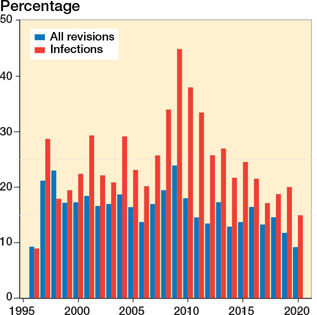
Figure 1. Proportion of revision and infection revision TKRs reported in the Finnish hospital discharge register (FHDR) but not to the Finnish arthroplasty register (FAR).
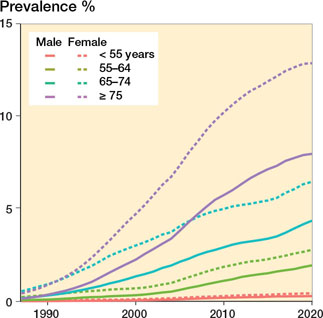
Figure 3. Prevalence of KJRs by age group and sex in in the population.
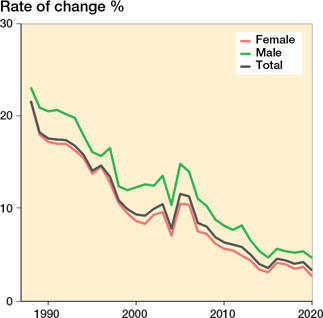
Figure 5. Annual rate of change in the prevalence of KJRs (patients with one or two KJRs) in the population aged 40 years or older. Note: The acceleration of this change between 2004 and 2005 is explained by the deadlines for non-urgent surgery set by the Finnish government in 2005.
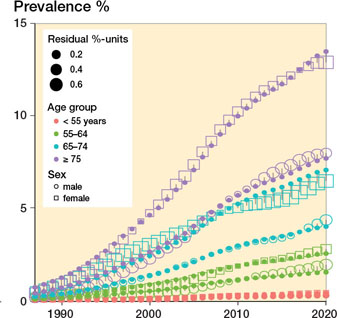
Figure 6. Goodness-of-fit of the models. Open squares and circles represent observed prevalence values, and the solid points the prevalences predicted by the model. The sizes of the observed points indicate the size of the difference between the observed and expected values, i.e., model residuals.
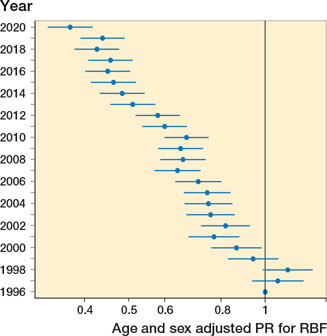
Figure 10. Age- and sex-adjusted proportion ratios (PR) with 95% confidence intervals for the revision burden factor (RBF): reference year is 1996.
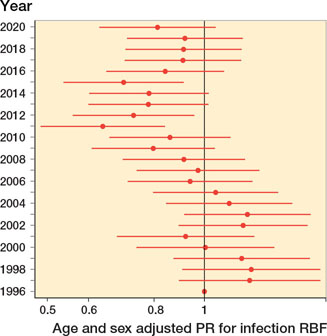
Figure 12. Age- and sex-adjusted proportion ratios (PR) with 95% confidence intervals for the infection revision burden factor (RBF): reference year is 1996