Long-term clinical and radiological outcomes following surgical treatment for symptomatic pediatric flexible flat feet: a systematic review
Maria Anna SMOLLE, Martin SVEHLIK, Katharina REGVAR, Andreas LEITHNER, and Tanja KRAUS
Department of Orthopaedics and Trauma, Medical University of Graz, 8036 Graz, Austria
Background and purpose — Albeit pediatric flexible flat foot (FFF) is a common condition, only a minority of patients become symptomatic. Long-term outcomes of surgically treated pediatric patients with symptomatic FFF are largely unknown. In this systematic review, studies providing outcomes at a mean follow-up of at least 4 years after the procedure in these patients were analyzed.
Material and methods — A PubMed search was undertaken involving original articles published up to July 2021 on outcome in children aged 6 to 14 with surgically treated FFF and mean (or minimum) follow-up of at least 4 years. Radiographic and clinical outcomes were analyzed.
Results — Of initially 541 entries, 10 could be included in the systematic review (all level IV), involving 846 pediatric patients with 1,536 symptomatic FFF. Pooled mean radiological (n = 8) and clinical follow-up (n = 10) was 5.3 (range 0.5–15) and 7.0 (range 4.1–15) years, respectively. Surgical procedures included arthroereisis (n = 8), lateral column lengthening (n = 1), and Horseman procedure (n = 1). Overall relative frequency of implant-associated complications and wound-healing problems was 3.2% and 1.3%, as well as 2.8% and 1.6% following subtalar arthroereisis only. From preoperative to latest radiological assessment following subtalar arthroereisis (including 3 studies with radiological follow-up < 48 months), pooled median decrease in talonavicular coverage angle (TNCA; –9.2°), anteroposterior talocalcaneal angle (A-TCA; –6.5°), lateral talocalcaneal angle (L-TCA; –3.5°), talar declination angle (TDA; –14°), Moreau Costa Bertani angle (MCB; –13°), and talo-firstmetatarsal angle (L-T1MA; –10°) was observed, as was an increase in calcaneal pitch (4.5°).
Interpretation — In symptomatic pediatric FFF patients, surgery is associated with a manageable complication profile, and results in satisfactory long-term clinical as well as radiological outcome. Yet scientific evidence is low, warranting larger scaled studies in the future.
Citation: Acta Orthopaedica 2022; 93: 367–374. DOI http://dx.doi.org/10.2340/17453674.2022.2254.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2021-12-05. Accepted: 2022-02-24. Published: 2022-03-18.
Correspondence: tanja.kraus@medunigraz.at
Conceptualization was carried out by TK, MS, and KR. MAS was responsible for data curation and visualization, and carried out the formal analysis. Validation was performed by KR, AL, MS, and TK. AL, TK, KR, and MS were responsible for supervision. MAS, TK, and MS wrote the original manuscript. Reviewing and editing was performed by AL and KR.
Acta thanks Jaakko Sinikumpu and Michael Sussman for help with peer review of this study.
A flexible flat foot (FFF)—or pes planovalgus—is usually found as a norm variant in children before the age of 5 years (1). Thereafter, constant increase of the foot’s medial arch leads to reduction of this innocuous physiologic norm variant (1). FFF may persist in some children, with the prevalence being higher in boys and obese children (2). However, only a minority of children with persistent idiopathic FFF will become symptomatic—usually with pain and shoe-wearing problems. Nevertheless, FFF (both symptomatic and asymptomatic) is considered the most frequent condition leading to referral to a pediatric orthopedist (3-5). Moreover, up to 20% of adults have a persisting flat foot deformity (1).
Apart from evident alterations in gait pattern due to advanced FFF, reasons why FFF become symptomatic in some people are largely unknown (6). Related to this, the effect of orthopedic arch supports vs. no treatment at all appears to be comparable in pediatric FFF, particularly in asymptomatic cases, although long-term results (beyond 2 years) are largely missing (7-9). For example, in the study by Whitford and Esterman, no difference in pain, exercise efficiency, self-perception, or gross motor proficiency was found at 3 or 12 months between children with symptomatic FFF treated by ready-made or custom-made orthopedic insoles, or no intervention (10). Prior to any surgical intervention, nonoperative treatment is obligatory in symptomatic, non-syndromic symptomatic FFF (11). Thus, initial treatment focuses on nonoperative interventions such as stretching of the triceps surae and orthopedic insoles based on the notion that FFF persisting beyond 5 years of age may be a residual norm variant (1). If nonoperative treatment fails, decision for surgical therapy may be made. However, surgery should be performed only after careful evaluation of changes in patient-reported symptoms and/or foot deformity following conservative treatment, and is almost never indicated in the first decade of life (11).
The type of surgery depends on the extent of abnormalities present (1,12,13). Surgical approaches consist of repositioning procedures such as joint-preserving osteotomies, arthroereisis, and—though seldom performed—also arthrodesis. The Evans osteotomy is a joint-preserving procedure, constituting a calcaneal lengthening osteotomy aimed at reconstructing the insufficient length of the foot’s lateral column, and consecutively leading to varus displacement (1). Yet, complications such as graft subsidence, wound dehiscence, and injury to the sural nerve have to be anticipated (14).
Arthroereisis, another surgical method to treat FFF, aims at restricting subtalar joint eversion (15-17). Notably, pain in the sinus tarsi area, nerve injuries, and wound complications, as well as screw loosening or breakage, constitute potential complications following subtalar arthroereisis (18). Furthermore, soft tissue procedures may either be added as corrective treatments following joint-preserving osteotomies or arthroereisis (e.g., Achilles tendon lengthening), or constitute a primary technique for FFF correction (e.g., Young procedure). However, sole soft tissue correction is nowadays largely avoided due to unsatisfactory results by insufficient correction of all underlying deformities (15,19).
Arthrodesis (e.g., of the talonavicular or subtalar joint) is another treatment option in FFF, though because of its negative impact on pedal-loading forces with increased risk of premature degenerative changes of adjacent joints, this should be considered with great caution (15,20-22). Moreover, this procedure in particular presents a certain risk of under- or over-correction.
Whilst short-term effects—also within randomized controlled trials (23,24)—are frequently reported after surgical treatment of FFF, only a few studies have concentrated on long-term results, with often non-standardized and heterogeneous assessment of outcomes (6,25,26).
Considering that loss of correction, complications, and patient discomfort may increase with time, the current systematic review was performed to collectively analyze long-term outcomes in children with surgically treated, symptomatic FFF providing a mean follow-up of at least 4 years after the procedure.
Material and methods
In this systematic review initiated in July 2021, all original, English or German full-text articles indexed in PubMed up to July 2021 (with no retroactive time limit) and analyzing the outcome in children (aged between 6 and 14 years) treated surgically for symptomatic FFF and reporting a mean (or minimum) follow-up of at least 4 years were potentially eligible. The age range was chosen based on the definition proposed by the American Academy of Pediatrics, with middle childhood defined as age range between 5 and 10 years, and early adolescence between 11 and 14 years (27). The following search terms were used (see Supplementary Table 1 for PubMed query): “pediatric pes planovalgus,” “pediatric pes planovalgus AND long term,” “pediatric pes planovalgus AND pain,” and “pediatric pes planovalgus AND surgery.”
Exclusion criteria were case reports, expert opinions, (systematic) reviews, or meta-analyses. Furthermore, publications dealing with FFF in adults, reporting on mean follow-up of less than 48 months (clinical and/or radiological), articles involving cohorts with more than 50% of patients affected by underlying disease (e.g., cerebral palsy, residual club-foot deformity), and diagnostic studies only were excluded.
The literature search and selection process were performed adhering to the PRISMA guidelines.
Data items
The following variables were ascertained from each study and included: type of study (nonoperative vs. operative), detailed type of intervention (e.g., subtalar arthroereisis, lateral column lengthening), number of patients, number of feet, mean age of patients at time of intervention (or minimum/maximum, if no measure of central tendency provided), information on preceding nonoperative treatment, mean/median clinical follow-up (or minimum, if no measure of central tendency available), mean/median radiological follow-up (or minimum, if no measure of central tendency provided), additional soft tissue or bone surgery, complications (hardware failure, wound healing deficits), outcome parameter AOFAS (American Orthopaedic Foot & Ankle Society) score, and radiographic measurements based on AP and lateral radiographs of the foot. On the AP view, these included: talonavicular coverage angle (TNCA) and talocalcaneal angle (A-TCA; Kite’s angle; Figure 1). The following radiographic measurements based on the lateral view of the foot were obtained: talocalcaneal angle (L-TCA), talo-first-metatarsal angle (L-T1MA; Meary’s angle), calcaneal pitch, talar declination angle (TDA), and Moreau Costa Bertani angle (MCB; angle formed by line from lower point of medial sesamoid bone to lower point of talonavicular joint, and line from lower point of talonavicular joint to lower point of posterior calcaneal tuberosity (28); Figure 1). As studies provided complication rates either for patients or feet (or both), relative frequencies were calculated based on the number of patients or feet analyzed. The overall relative frequency was derived from calculated percentages (per feet or patients). Evidence level was assessed as defined by the Oxford Centre for Evidence-Based Medicine (OCEBM) (29).
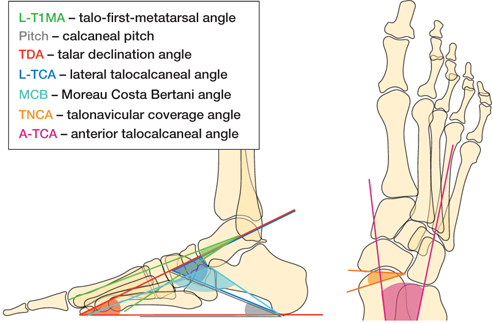
Figure 1. Graphical depiction of angles analyzed.
The Newcastle Ottawa Scale (NOS) for case-control and non-randomized cohort studies was used for quality assessment (30). The NOS ranges between 0 and 9 points, with higher values indicative of higher quality studies (30). Points are allocated in categories selection (max. 4 points), comparability (max. 2 points), and exposure (for case-control studies; max. 3 points) or outcome (for cohort studies; max. 3 points) (30).
Statistics
As none of the studies meeting the defined inclusion criteria compared 2 different treatment modalities, only descriptive and exploratory analyses of pooled results deriving from all studies included were performed. Means (SD) were reported for normally distributed continuous variables, and medians (IQR) for non-normally distributed continuous variables. In subgroup analysis, as 8 out of 10 studies reported on outcomes following subtalar arthroereisis, results of these studies were pooled, whereas results of the latter 2 studies were given—if applicable—as single values only.
Results
Literature search retrieved 541 entries, of which 10 studies could be finally included in the qualitative and quantitative analysis (Figure 2; Table 1).
| Study | Treatment type a | Soft tissue procedures | Level of evidence | NOS | Males: Females | Patients (n) | Feet (n) | Mean age b | Mean | |
| follow-up radiological | (months) clinical | |||||||||
| Mazzotti (26) | SA | Achilles tendon lengthening (23 feet) | IV | 5 | 21:13 | 34 | 64 | 12.0 | 180 | 180 |
| Bernasconi (33) | SA | IV | 4 | 22:9 | 31 | 62 | 10.5 | 62 | 62 | |
| Memeo (36) | SA | IV | 6 | Unknown | 201 c | 402 | 13.2 | 12 d | 130 e | |
| Pavone (28) | SA | IV | 4 | 38:30 | 68 | 136 | 12.7 | 36 d | 578 | |
| Dana (25) | HP | Achilles tendon lengthening (10 feet) | IV | 5 | 16:7 | 23 | 41 | 6.6 | 107 | 107 |
| Faldini (31) | SA | IV | 5 | 107:66 | 173 | 283 | 11.2 | 50 | ||
| Giannini (35) | SA | Achilles tendon lengthening (24 feet) | IV | 6 | 31:13 | 44 | 88 | 11.7 | 48 d | 56 |
| Das (34) | SA | Achilles tendon lengthening (7 feet) | IV | 4 | 10:5 | 15 | 25 | 12.0 | 54 | 54 |
| Akimau (32) | LCL | Peroneus brevis-to-longus transfer (13 feet), Tibialis posterior advancement to navicular (11 feet), Plantar fascia release (4 feet), Achilles tendon lengthening (2 feet), | IV | 4 | 9:3 | 15 | 25 | 12.5 | 54 | |
| Pavone (37) | SA | Achilles tendon lengthening (18 feet) | IV | 6 | 157:85 | 242 | 410 | 10.3 | 6.0 | 88 |
| a Treatment type: SA – subtalar arthroereisis; HP – Horseman procedure; LCL – lateral column lengthening b at surgery in years. c approximately; d minimum; e median. |
||||||||||
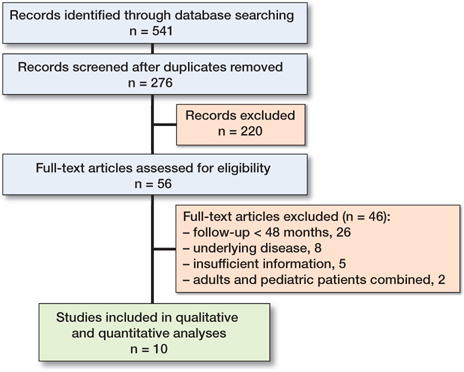
Figure 2. Flowchart showing selection of studies.
Study characteristics
Overall, the 10 studies comprised 846 children with 1,536 symptomatic FFF (25,26,28,31-37). The male to female ratio was 1.8:1. Patients’ mean age at intervention was 11.3 years (1.9). All articles included reported on level IV studies. Mean NOS was 4.9 points (0.8). Mean radiological follow-up of the 8 studies reporting on radiological outcomes was 63 months (57; 3 studies provided minimum follow-up time only). Pooled mean clinical follow-up over the entire cohort was 84 months (43; 1 provided median follow-up only).
8 of 10 studies reported on long-term outcomes after subtalar arthroereisis, and 1 study each on results following lateral column lengthening or Horseman procedure. The optional use of additional soft tissue procedures (e.g., Achilles tendon lengthening) was reported in 6 out of 10 studies (Table 1). In 5 of the 10 studies, unsuccessful nonoperative treatment had preceded the operative therapy, whilst in the remaining studies this had not been explicitly stated. 20% of patients analyzed following lateral column lengthening had an associated condition (32), whereas the remaining 9 studies included only patients with idiopathic symptomatic FFF.
Clinical and functional outcomes
All studies provided numbers on implant-associated complications (i.e., screw loosening or breakage), with an overall relative frequency of 3.2% (Table 2) (25,26,28,31-37). Information on wound-healing problems was likewise available for all studies, occurring at an overall relative frequency of 1.3% (25,26,28,31-37). Following subtalar arthroereisis only (26,28,31,33-37), screw loosening/breakage and wound-healing problems were reported at a relative frequency of 2.8% and 1.6%, respectively (Table 2). Conversion of the initial procedure to another one due to malcorrection was reported in 1 study (5 feet with lateral column lengthening requiring further bony procedures [32]). 4 studies (26,28,31,34) provided information on the patients’ ability to perform sports following surgery (Table 2). At latest follow-up, chronic pain was present in 4.0% of patients, regardless of the procedure (based on 8 studies [25,26,28,31,34-37]), and in 2.8% of patients following subtalar arthroereisis (based on 7 studies [26,28,31,34-37]). Mean AOFAS at an average follow-up of 86 months (50) was 88 points (13; based on the results of 6 studies [25,26,28,32-34]). 3 of these also reported on preoperative AOFAS scores (mean 68 points [29]), with an average improvement of 19 points (9) until latest follow-up (25,28,34). For patients with subtalar arthroereisis only, preoperative and latest follow-up AOFAS (at a mean of 88 months [53]) were reported by 2 (28,34) and 4 studies (26,28,33,34), respectively, amounting to a mean of 57 points (crude values: 34 and 79 points) and 86 points (14) points. In patients with subtalar arthroereisis, mean AOFAS improvement from preoperative to latest follow-up was 23 points (crude values: 18 and 28 points).
| Study | Feet/patients | Screw loosening/breakage | Wound complications | Conversion to another procedure | Chronic pain | Sporting ability |
| Subtalar arthroereisis | ||||||
| Mazzotti (26) | 34/34 | 0 (0) | 0 (0) | 0 (0) | Sports performed on regular basis by 18 patients (53%), and occasionally by 10 patients (29%) | |
| Bernasconi (33) | 62/31 | 0 (0) | 0 (0) | |||
| Memeo (36) | 402/201 a | 14 f (4) | 0 (0) | 43 f (11) b | ||
| Pavone (28) | 136/68 | 4 f (5) | 4 f (3) | 0 (0) | Desired sport carried out by 65 patients (96%), non-weight-bearing sports performed by 3 patients (4%) | |
| Faldini (31) | 283/173 | 3 p (2) | 0 (0) | 1 p (1) | Average period of 4.5 months to resume sports | |
| Giannini (35) | 88/44 | 2 p (5) | 0 (0) | 0 (0) | ||
| Das (34) | 25/15 | 1 p (7) | 1 p (7) | 1 p (7) | Slight restriction in sporting activities according to OAFQC item “sports” | |
| Pavone (37) | 410/242 | 2 p (1) | 7 p (3) | 10 p (4) | ||
| Relative frequency | (2.8) | (1.6) | NA | (2.8) | NA | |
| Horseman procedure | ||||||
| Dana (25) | 41/23 | 4 f (10) | 0 (0) | 4 f (10) | ||
| Lateral column lengthening | ||||||
| Akimau (32) | 25/15 | 0 (0) | 0 (0) | 5 f (20) | ||
| Overall relative frequency | (3.2) | (1.3) | NA | (4) | NA | |
| Relative and cumulative frequencies provided for studies on subtalar arthroereisis only (n = 8), and all studies combined (n = 10), respectively. a approximately; b at 3 months post-surgery. NA = not applicable. |
||||||
Radiological outcomes
Results on radiographic angles of the foot obtained prior to intervention and at latest follow-up were available in 8 of 10 studies (25,26,28,33-37), with 3 of these reporting on radiological parameters obtained at a mean time of less than 48 months following surgery (28,36,37) and 7 analyzing patients with subtalar arthroereisis (26,28,33-37). One study on patients undergoing Horseman procedure revealed a mean increase of 2.6° for calcaneal pitch at a follow-up of 8.9 years (25). For all studies on subtalar arthroereisis combined, a decrease in TNCA was observed from preoperative to latest follow-up (–9.2°), as was a decrease in A-TCA (–6.5°), L-TCA (–3.5°), L-T1MA (–10°), TDA (–13.5°), and MCB (–12.7°; Table 3). Calcaneal pitch showed an overall increase from preoperative to latest follow-up (+4.5°; Table 3).
| Study | Follow-up (months) | TNCA | A-TCA | L-TCA | L-T1MA | Pitch | TDA | MCB | |
| Subtalar arthroereisis | |||||||||
| Radiological follow-up ≥ 48 months | |||||||||
| Mazzotti (26) | 180 | Preoperative | 27° (14°) | 26° (8°) | 43° (6°) | 13° (8°) | 15° (4°) | 138° (10°) | |
| Latest FU | 15° (9°) | 22° (7°) | 43° (5°) | 7° (7°) | 17° (4°) | 129° (7° | |||
| Difference | –12° | –4.2° | 0.1° | –6.3° | 1.8° | –9.3° | |||
| p-value | < 0.001 | < 0.05 | n.s. | < 0.001 | < 0.05 | < 0.001 | |||
| Bernasconi (33) | 62 | Preoperative | 19° (7°) | 29° (4°) | 40° (5°) | 12° (3°) | 144° (8°) | ||
| Latest FU | 12° (8°) | 21° (3°) | 33° (4°) | 17° (5°) | 135° (6°) | ||||
| Difference | –6.9° | –8.0° | –7.0° | 4.8° | –8.9° | ||||
| p-value | n.s. | 0.04 | 0.004 | < 0.001 | < 0.001 | ||||
| Das (34) | 54 | Preoperative | 31° (1°) | 33° (0.4°) | 15° (1°) | 44° (2°) | 148° (3°) | ||
| Latest FU | 23° (1°) | 18° (0.4°) | 22° (1°) | 25° (1.1° | 136° (3°) | ||||
| Difference | –7.8° | –15° | 6.7° | –20° | –12° | ||||
| p-value | < 0.05 | < 0.05 | < 0.05 | < 0.05 | < 0.05 | ||||
| Giannini (35) | 48 | Preoperative | 40° (5°) | 19° (8°) | |||||
| Latest FU | 29° (4°) | 9.4° (7°) | |||||||
| Difference | – 11° | –10.0° | |||||||
| p-value | < 0.001 | < 0.001 | |||||||
| Radiological follow-up < 48 months | |||||||||
| Pavone (28) | 36 | Preoperative | 31° (1°) | 13° (2°) | 44° (6°) | 156° (4°) | |||
| Latest FU | 25° (2°) | 16° (1°) | 31° (3°) | 136° (7°) | |||||
| Difference | –5.9° | 3.7° | –14° | –20° | |||||
| p-value | < 0.001 | < 0.001 | < 0.001 | < 0.001 | |||||
| Memeo (36) | 12 | Preoperative | 28° (3°) | 13° (1°) | 35° (4°) | 137° (4°) | |||
| Latest FU | 22° (5°) | 18° (3°) | 30° (5°) | 124° (6°) | |||||
| Difference | –6.5° | 4.7° | –4.9° | –13° | |||||
| p-value | NA | NA | NA | NA | |||||
| Pavone (37) | 6 | Preoperative | 31° (1°) | 13° (1°) | 43° (5°) | 155° (3°) | |||
| Latest FU | 25° (2°) | 17° (1°) | 30° (2°) | 133° (6°) | |||||
| Difference | –6.1° | 4.2° | –13° | –22° | |||||
| p-value | < 0.001 | < 0.001 | < 0.001 | < 0.001 | |||||
| Overall difference | Median | –9.2° | –6.5° | –3.5° | –10° | 4.5° | –13.5° | –12.7° | |
| IQR, lower | –11.5° | –8.0° | –7.0° | –14.7° | 3.7° | –16.6° | –20.3° | ||
| IQR, upper | –6.9° | –5.9 | 0.1 | 6.3° | 4.8° | –9.1° | –9.3° | ||
| Horseman procedure | |||||||||
| Dana (25) | 107 | Preoperative | 11° (5°) | ||||||
| Latest FU | 13° (5°) | ||||||||
| Difference | 2.6° | ||||||||
| p-value | 0.03 | ||||||||
| n.s. = not significant. NA = not applicable. | |||||||||
For those 4 subtalar arthroereisis studies with an individual mean radiological follow-up of ≥ 48 months only (25,26,33-35), median final TNCA was 13.8° (IQR 12.3°–15.2°), and median L-TCA 38° (IQR 33°–43°). Median A-TCA was 23° (IQR 22°–26°), median L-T1MA 9° (7°–18°), and median calcaneal pitch 17° (IQR 17°–22°; Figure 3). Furthermore, median MCB was 135° (IQR 129°–136°). In other words, a decrease in TNCA (–9.2°), A-TCA (–7.9°), L-TCA (–3.5°), L-T1MA (–10°), and MCB (–9.3°) was observed, as was an increase in calcaneal pitch (+4.8°). Notably, TDA at followup ≥ 48 months was reported by 1 study only (34), being 24.7° and having decreased by 19.6° from preoperative to last assessment (Figure 3).<
a id="F0003_2254">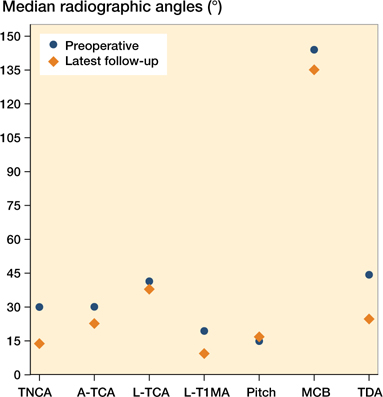
Figure 3. Pooled median preoperative radiographic angles of the foot in comparison with radiographic angles at latest follow-up in studies on subtalar arthroereisis with a mean follow-up of ≥ 48 months (n = 4).
Discussion
The 10 studies included in this review were all low evidence (level IV). The resulting average Newcastle Ottawa Scale amounted to 4.9 points, being lower than the 5.7 points reported in a systematic review on risk of fall after orthopedic procedures upon peripheral nerve blockage (38), and the 6.7 points resulting from a systematic review on treatment of plantar fasciopathy (39). Systematic reviews and meta-analyses of common adult pathologies such as anterior cruciate ligament injuries and arthroplasties frequently include more than 20 studies, and usually several with high evidence levels (40-43). Furthermore, there are only a few randomized controlled trials on treatment of FFF, all with short-to-mid-term follow-up only (23,24,44-46); therefore they were not considered in this systematic review with a focus on long-term effects. Albeit based on retrospective, non-randomized cohort studies, the pooled results herein following surgery for symptomatic FFF appear promising in terms of complications and radiological outcome.
An important part of outcome measure reporting following orthopedic procedures should be presentation of surgical complications. The observed wound healing problem rate in the current study is comparable to that for other pediatric foot surgeries, e.g., split tibialis anterior tendon transfer for spastic equinovarus feet (between 0.8% and 5.9% wound complication rates) (47,48). It should be noted, though, that surgery-associated complications were not uniformly defined (e.g., by using the definition of the Modified Clavien–Dindo System [MCD] (49)), so that comparison of complication severity between studies, as well as with studies on other pathologies, is generally impaired. Furthermore, the 4.0% chronic pain rate is slightly higher than the 2.6% described following implant removal in pediatric trauma surgery (50), albeit it has to be considered that 1 study in the present systematic review (36) provided 3-month results on complications only, and that the relative frequency for chronic pain following subtalar arthroereisis was lower at 2.8%.
Regarding functional outcomes, the average AOFAS for all studies combined, and for studies on subtalar arthroereisis only, revealed a “good” outcome (51). Moreover, an average increase of 18.8 points was observed from preoperative to last follow-up based on 3 studies on functional outcome. Although this is an evident improvement, there is currently no consensus on the extent to which the AOFAS would have to increase in order to be of clinical relevance (51). Nevertheless, the observed average AOFAS herein is higher than that reported 12 months following orthopedic foot surgeries in general (52) but compares favorably with that observed in children after tarsal coalition surgery (53), and after surgery in children for osteochondral lesions of the talus (54). However, the usefulness of the AOFAS in children has been questioned due to limited validity and reliability (55-57). Therefore, more attention should be paid to patient-reported outcome measures in the future.
Apart from clinical and functional outcome, radiologically measured angles of the foot at final follow-up in comparison with preoperative angles showed improvements towards the values of a normal pediatric foot. For subtalar arthroereisis studies with an individual mean radiological follow-up of ≥ 48 months, a median A-TCA of 23° was found at latest follow-up, being within the normal range of 20° to 40° for infants and children reported by Vanderwilde et al. (58). Likewise, median L-TCA and median calcaneal pitch were slightly below the values defined for normal pediatric feet (13,58), but had overall improved by 5° from preoperative to latest follow-up. With a median L-T1MA of 9.4° at final follow-up, there was still a remnant pes planus component (58), although an overall reduction of 3.5° had been achieved. The radiographic results obtained in the current study are slightly poorer than those reported by Tan et al. in a meta-analysis on subtalar arthroereisis (59). Reasons for this could be differing inclusion criteria deployed, with Tan et al. likewise incorporating studies on short-term outcomes, patients up to the age of 21, and those with flexible, rigid, or spastic flat feet (59).
Notably, 8 out of 10 studies meeting the inclusion criteria reported on long-term outcomes following subtalar arthroereisis, whilst only 2 had analyzed results following other procedures, e.g., lateral column lengthening. This discrepancy may be explained by the fact that subtalar arthroereisis is considered a rather simple and theoretically reversible procedure, whilst definite bony corrections may be associated with complex revision surgeries in case of over- or under-correction. Therefore, long-term studies on the outcome following “definite” surgical procedures are warranted to allow comparison with “temporary” techniques in FFF treatment. None of the 8 studies on subtalar arthroereisis herein analyzed described necessity for conversion to other treatments due to malcorrection. On the other hand, additional bony corrections became necessary in 20% of feet with lateral column lengthening (32). In line with this, the rate of chronic pain as reported in one study on the Horseman procedure was higher (9.4%) than theat observed in patients following subtalar arthroereisis (2.8%).
The pathophysiology of pediatric FFF is complex. Besides bony changes, shortening of the gastro-soleus group is one of the causative factors. Therefore, rebalancing of the gastrosoleus muscle–tendon complex was reported to be part of the surgical procedure in 6 out of 10 studies (25,26,32,34,35,37), achieved by Achilles tendon lengthening in all studies. However, the rate of this procedure was very variable, ranging from 4.4% (37) to 35.9% (26) of feet. In most cases, limited dorsiflexion—defined as < 5° with extended knee—was used as an indication criterion.
There are limitations of our study. First, all studies meeting the defined inclusion criteria were based on level IV retrospective cohorts with a mean NOS of 4.9 points. Our findings must be interpreted bearing a potential selection bias in mind. Second, 3 different surgical procedures were included in this systematic review, with 8 of 10 studies reporting on outcomes following subtalar arthroereisis. Therefore, pooled results were given both for all studies combined as well as for those on subtalar arthroereisis only, to enable a better interpretation of the data depending on the surgical procedure performed. Third, information on clinical and radiological parameters was inconsistently reported by individual studies, complicating a comprehensive data analysis. Related to this, there was a considerable diversity of participants included, as was similarly the definition of indication for surgical correction of the FFF. Consequently, more homogeneous patient cohorts should be strived for in the future, allowing for distinct conclusions to be drawn.
Conclusion
In children with symptomatic FFF refractory to conservative treatment, surgical therapy is associated with a manageable complication profile, and eventually results in satisfactory long-term clinical as well as radiological outcome. Although a clear correlation between clinical and radiological outcomes following surgery for pediatric flexible FFF is yet to be clarified (6), the current pooled results point towards concordant overall improvement in radiological and clinical parameters by surgical therapy. Yet, evidence of studies included herein is low, few provide patient-reported outcome measures, and long-term results on definite bony corrections are still missing. Therefore, larger scaled studies in symptomatic pediatric FFF are warranted, ideally comparing different therapeutic approaches.
- Thévenin-Lemoine C, Khouri N. Surgical treatment of idiopathic pes planovalgus in paediatric patients. Orthop Traumatol Surg Res 2019; 105(1s): S187-98.
- Pfeiffer M, Kotz R, Ledl T, Hauser G, Sluga M. Prevalence of flat foot in preschool-aged children. Pediatrics 2006; 118(2): 634-9.
- Staheli L T. Evaluation of planovalgus foot deformities with special reference to the natural history. J Am Podiatr Med Assoc 1987; 77(1): 2-6.
- Evans A M, Rome K. A Cochrane review of the evidence for non-surgical interventions for flexible pediatric flat feet. Eur J Phys Rehabil Med 2011; 47(1): 69-89.
- El O, Akcali O, Kosay C, Kaner B, Arslan Y, Sagol E, et al. Flexible flatfoot and related factors in primary school children: a report of a screening study. Rheumatol Int 2006; 26(11): 1050-3.
- Bernasconi A, Lintz F, Sadile F. The role of arthroereisis of the subtalar joint for flatfoot in children and adults. EFORT Open Rev 2017; 2(11): 438-46.
- MacKenzie A J, Rome K, Evans A M. The efficacy of nonsurgical interventions for pediatric flexible flat foot: a critical review. J Pediatr Orthop 2012; 32(8): 830-4.
- Dars S, Uden H, Banwell H A, Kumar S. The effectiveness of non-surgical intervention (foot orthoses) for paediatric flexible pes planus: a systematic review: update. PLoS One 2018; 13(2): e0193060.
- Evans A M, Rome K, Carroll M, Hawke F. Foot orthoses for treating paediatric flat feet. Cochrane Database Syst Rev 2022; 1: Cd006311.
- Whitford D, Esterman A. A randomized controlled trial of two types of in-shoe orthoses in children with flexible excess pronation of the feet. Foot Ankle Int 2007; 28(6): 715-23.
- Hell A K, Döderlein L, Eberhardt O, Hösl M, von Kalle T, Mecher F, et al. [S2-Guideline: Pediatric Flat Foot]. Z Orthop Unfall 2018; 156(3): 306-15.
- Besse J. Que faut-il faire et surtout ne pas faire chez l’enfant? Le point de vue de l’orthopédiste adulte. In: Le pied, de l’enfance à l’adolescence—SOFOP. Sauramps Médical 2014: 339-41.
- Bresnahan P J, Juanto M A. Pediatric flatfeet: a disease entity that demands greater attention and treatment. Front Pediatr 2020; 8:19.
- Jara M E. Evans osteotomy complications. Foot Ankle Clin 2017; 22(3): 573-85.
- Mosca V S. Flexible flatfoot in children and adolescents. J Child Orthop 2010; 4(2): 107-21.
- Haraldsson S. Pes plano-valgus staticus juvenilis and its operative treatment. Acta Orthop Scand 1965; 35: 234-56.
- Miller G R. The operative treatment of hypermobile flatfeet in the young child. Clin Orthop Relat Res 1977(122): 95-101.
- Usuelli F G, Montrasio U A. The calcaneo-stop procedure. Foot Ankle Clin 2012; 17(2): 183-94.
- Jones B S. Flat foot: a preliminary report of an operation for severe cases. J Bone Joint Surg Br 1975; 57(3): 279-82.
- Angus P D, Cowell H R. Triple arthrodesis: a critical long-term review. J Bone Joint Surg Br 1986; 68(2): 260-5.
- Saltzman C L, Fehrle M J, Cooper R R, Spencer E C, Ponseti I V. Triple arthrodesis: twenty-five and forty-four-year average follow-up of the same patients. J Bone Joint Surg Am 1999; 81(10): 1391-402.
- Southwell R B, Sherman F C. Triple arthrodesis: a long-term study with force plate analysis. Foot Ankle 1981; 2(1): 15-24.
- Tahririan M A, Ramtin S, Taheri P. Functional and radiographic comparison of subtalar arthroereisis and lateral calcaneal lengthening in the surgical treatment of flexible flatfoot in children. Int Orthop 2021; 45(9): 2291-8.
- Nagy M, Kholeif A, Mansour A M R, Abdelhameed S, Radwan Y A, Khedr A, et al. Comparison between Malerba osteotomy and combined Evans/medial displacement calcaneal osteotomies for the management of flexible pes planus in young adults: a prospective randomised control trial, three years follow-up. Int Orthop 2021; 45(10): 2579-88.
- Dana C, Péjin Z, Cadilhac C, Wicart P, Glorion C, Aurégan J C. Long-term results of the “Horseman” procedure for severe idiopathic flatfoot in children: a retrospective analysis of 41 consecutive cases with mean 8.9 year duration of follow-up. J Foot Ankle Surg 2019; 58(1): 10-6.
- Mazzotti A, Di Martino A, Geraci G, Casadei C, Panciera A, Giannini S, et al. Long-term results of subtalar arthroereisis for the treatment of symptomatic flexible flatfoot in children: an average fifteen year follow-up study. Int Orthop 2021; 45(3): 657-64.
- Hagan J F, Shaw J S, Duncan P M. Bright futures: guidelines for health supervision of infants, children, and adolescents. 4th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2017.
- Pavone V, Vescio A, Di Silvestri C A, Andreacchio A, Sessa G, Testa G. Outcomes of the calcaneo-stop procedure for the treatment of juvenile flatfoot in young athletes. J Child Orthop 2018; 12(6): 582-9.
- Group OLoEW. The Oxford 2011 levels of evidence. Oxford: Oxford Centre for Evidence-Based Medicine; 2011.
- Wells G A. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- Faldini C, Mazzotti A, Panciera A, Persiani V, Pardo F, Perna F, et al. Patient-perceived outcomes after subtalar arthroereisis with bioabsorbable implants for flexible flatfoot in growing age: a 4-year follow-up study. Eur J Orthop Surg Traumatol 2018; 28(4): 707-12.
- Akimau P, Flowers M. Medium term outcomes of planovalgus foot correction in children using a lateral column lengthening approach with additional procedures “à la carte”. Foot Ankle Surg 2014; 20(1): 26-9.
- Bernasconi A, Iervolino C, D’Alterio R, Lintz F, Patel S, Sadile F. Midterm assessment of subtalar arthroereisis for correction of flexible flatfeet in children. Orthop Traumatol Surg Res 2020; 106(1): 185-91.
- Das S P, Das P B, S G, Sahu M C. Effectiveness of surgically treated symptomatic plano-valgus deformity by the calcaneo stop procedure according to radiological, functional and gait parameters. J Taibah Univ Med Sci 2017; 12(2): 102-9.
- Giannini S, Cadossi M, Mazzotti A, Persiani V, Tedesco G, Romagnoli M, et al. Bioabsorbable calcaneo-stop implant for the treatment of flexible flatfoot: a retrospective cohort study at a minimum follow-up of 4 years. J Foot Ankle Surg 2017; 56(4): 776-82.
- Memeo A, Verdoni F, Rossi L, Ferrari E, Panuccio E, Pedretti L. Flexible juvenile flat foot surgical correction: a comparison between two techniques after ten years’ experience. J Foot Ankle Surg 2019; 58(2): 203-7.
- Pavone V, Costarella L, Testa G, Conte G, Riccioli M, Sessa G. Calcaneo-stop procedure in the treatment of the juvenile symptomatic flatfoot. J Foot Ankle Surg 2013; 52(4): 444-7.
- Johnson R L, Kopp S L, Hebl J R, Erwin P J, Mantilla C B. Falls and major orthopaedic surgery with peripheral nerve blockade: a systematic review and meta-analysis. Br J Anaesth 2013; 110(4): 518-28.
- Singh P, Madanipour S, Bhamra J S, Gill I. A systematic review and meta-analysis of platelet-rich plasma versus corticosteroid injections for plantar fasciopathy. Int Orthop 2017; 41(6): 1169-81.
- Moyer R, Ikert K, Long K, Marsh J. The value of preoperative exercise and education for patients undergoing total hip and knee arthroplasty: a systematic review and meta-analysis. JBJS Rev 2017; 5(12): e2.
- Lewis G N, Rice D A, McNair P J, Kluger M. Predictors of persistent pain after total knee arthroplasty: a systematic review and meta-analysis. Br J Anaesth 2015; 114(4): 551-61.
- Mouarbes D, Menetrey J, Marot V, Courtot L, Berard E, Cavaignac E. Anterior cruciate ligament reconstruction: a systematic review and meta-analysis of outcomes for quadriceps tendon autograft versus bonepatellar tendon-bone and hamstring-tendon autografts. Am J Sports Med 2019; 47(14): 3531-40.
- Montalvo A M, Schneider D K, Webster K E, Yut L, Galloway M T, Heidt R S, Jr., et al. Anterior cruciate ligament injury risk in sport: a systematic review and meta-analysis of injury incidence by sex and sport classification. J Athl Train 2019; 54(5): 472-82.
- Abd-Elmonem A M, El-Negamy E H, Mahran M A, Ramadan A T. Clinical and radiological outcomes of corrective exercises and neuromuscular electrical stimulation in children with flexible flatfeet: a randomized controlled trial. Gait Posture 2021; 88: 297-303.
- Jafarnezhadgero A, Madadi-Shad M, Alavi-Mehr S M, Granacher U. The long-term use of foot orthoses affects walking kinematics and kinetics of children with flexible flat feet: a randomized controlled trial. PLoS One 2018; 13(10): e0205187.
- Hsieh R L, Peng H L, Lee W C. Short-term effects of customized arch support insoles on symptomatic flexible flatfoot in children: a randomized controlled trial. Medicine (Baltimore) 2018; 97(20): e10655.
- Hosalkar H, Goebel J, Reddy S, Pandya N K, Keenan M A. Fixation techniques for split anterior tibialis transfer in spastic equinovarus feet. Clin Orthop Relat Res 2008; 466(10): 2500-6.
- Lullo B, Nazareth A, Rethlefsen S, Illingworth K D, Abousamra O, Kay R M. Split tibialis anterior tendon transfer to the peroneus brevis or tertius for the treatment of varus foot deformities in children with static encephalopathy: a retrospective case series. J Am Acad Orthop Surg Glob Res Rev 2020; 4(5): e2000044.
- Dindo D, Demartines N, Clavien P A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004; 240(2): 205-13.
- Gorter E A, Vos D I, Sier C F, Schipper I B. Implant removal associated complications in children with limb fractures due to trauma. Eur J Trauma Emerg Surg 2011; 37(6): 623-7.
- Ceccarelli F, Calderazzi F, Pedrazzi G. Is there a relation between AOFAS ankle-hindfoot score and SF-36 in evaluation of Achilles ruptures treated by percutaneous technique? J Foot Ankle Surg 2014; 53(1): 16-21.
- Malviya A, Makwana N, Laing P. Correlation of the AOFAS scores with a generic health QUALY score in foot and ankle surgery. Foot Ankle Int 2007; 28(4): 494-8.
- Mahan S T, Spencer S A, Vezeridis P S, Kasser J R. Patient-reported outcomes of tarsal coalitions treated with surgical excision. J Pediatr Orthop 2015; 35(6): 583-8.
- Park C H, Song K S, Kim J R, Lee S W. Retrospective evaluation of outcomes of bone peg fixation for osteochondral lesion of the talus. Bone Joint J 2020; 102-b(10): 1349-53.
- SooHoo N F, Shuler M, Fleming L L. Evaluation of the validity of the AOFAS clinical rating systems by correlation to the SF-36. Foot Ankle Int 2003; 24(1): 50-5.
- Button G, Pinney S. A meta-analysis of outcome rating scales in foot and ankle surgery: is there a valid, reliable, and responsive system? Foot Ankle Int 2004; 25(8): 521-5.
- Murphy D, Raza M, Khan H, Eastwood D M, Gelfer Y. What is the optimal treatment for equinus deformity in walking-age children with clubfoot? A systematic review. EFORT Open Rev 2021; 6(5): 354-63.
- Vanderwilde R, Staheli L T, Chew D E, Malagon V. Measurements on radiographs of the foot in normal infants and children. J Bone Joint Surg Am 1988; 70(3): 407-15.
- Tan J H I, Tan S H S, Lim A K S, Hui J H. The outcomes of subtalar arthroereisis in pes planus: a systemic review and meta-analysis. Arch Orthop Trauma Surg 2021; 141(5): 761-73.