Perspective
Locking plate osteosynthesis in geriatric shoulder fractures: why do we continue to perform a low-value procedure?
Stig BRORSON
Centre for Evidence-Based Orthopaedics, Department of Orthopaedic Surgery, Zealand University Hospital, Denmark
Citation: Acta Orthopaedica 2022; 93: 355–357. DOI http://dx.doi.org/10.2340/17453674.2022.2208.
Copyright: © 2022 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-01-18. Accepted: 2022-02-15. Published: 2022-02-24.
Correspondence: sbror@regionsjaelland.dk
Acta thanks Antti P Launonen and Hans Rahme for help with peer review of this Perspective.
The use of locking plates
In several countries, locking plate osteosynthesis is the treatment of choice for the majority of displaced proximal humeral fractures, geriatric patients included. Despite national differences, an increasing use of the procedure has been reported. In Germany, a 39% increase in surgical procedures for proximal humeral fractures was reported between 2007 and 2016 with 69% of the surgeries performed in geriatric patients. Osteosyntheses accounted for 72% of these surgeries with more than 35,000 procedures performed in 2016. Locking plate fixation was the most commonly performed procedure (1). In Finland, the incidence of surgery raised from 5 per 100,000 per year in 1987 to 20 per 100,00 per year in 2016. From 2002, following the advent of locking plates, a more than threefold increase in the incidence of osteosynthesis was reported (2). In Sweden, the rate of surgically treated patients increased by 75% between 2001 and 2012. The percentage of fractures treated by plate osteosynthesis rose from 6% in 2001 to 46% in 2012 (3). In the United States, a study in a Medicare population before and after the introduction of locking plates reported a relative increase in surgery of 26% with an increase in osteosyntheses of 29% (4). In South Korea, the operation rate for proximal humeral fractures increased from 25% in 2008 to 37% in 2016, of which osteosynthesis accounted for 72% in 2008 and 86% in 2016 (5).
Benefits and harms: the evidence base
Within the last decade, several high-quality randomized clinical trials on the benefits of locking plates have been conducted. They have been unable to demonstrate superiority of surgery over non-surgical management in geriatric 2-, 3-, and 4-part fractures. The only difference between the groups has been a higher risk of additional surgery after surgical management (6). Olerud et al. (7) randomized 60 patients with 3-part fractures to locking plate or non-surgical treatment. No statistically significant between-group difference was found. Fjalestad et al. (8) randomized 50 patients with 3- and 4-part fractures to locking plate or non-surgical treatment. They reported no evidence of any difference in functional outcome between surgical treatment and non-surgical treatment. Rangan et al. (9) randomized 250 patients to surgeon’s choice or non-surgical treatment. In the surgery group 47% were 2-part surgical neck fractures and 36% were 3-part fractures. Locking plates were used in 83% of all surgeries. Separate data on locking plates was not reported but patient-reported outcome was similar between surgical and non-surgical treatment at 2 or 5 years (9,10). Launonen et al. (11) randomized 88 patients with 2-part fractures to locking plate or non-surgical treatment. They found similar clinical outcome between the groups and suggested that the current practice of performing surgery on the majority of 2-part fractures may not be beneficial.
High complication and failure rates have persistently been associated with the use of locking plates, especially screwrelated problems (Figure 1). Several systematic reviews and large cohort studies have reported failure rates of about 30% (12-15). Recently, a reputable shoulder clinic published a retrospective series of 173 geriatric locking plate osteosyntheses. They reported complication rates of 44% and failure rates of 34% defined as reoperation or radiographic evidence of implant failure. The failure rates tended to increase with age, with a 26% failure rate for patients in their 60s, 40% failure rate for patients in their 70s, and 48% failure rate for patients in their 80s (16). However, they did not consider treating these patients without locking plates.
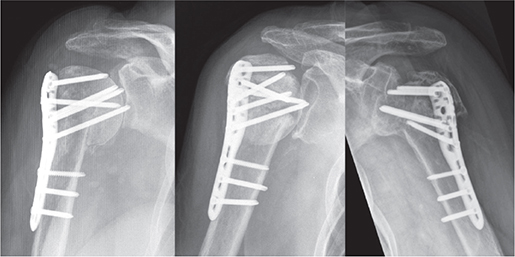
Figure 1. Examples of failed locking plate osteosynthesis in geriatric shoulder fractures. The osteoporotic humeral head has collapsed, and the locking screws have penetrated into the glenohumeral joint causing pain and damage to the cartilage and the glenoid surface.
Why do we use locking plates in geriatric shoulder fractures?
There appears to be a tension between the widespread use of a locking plate in geriatric shoulder fractures and the lack of evidence for adding value to the patients. The origin of the firm belief among surgeons in certain implants and procedures has not been studied but it may be in the interests of several stakeholders to intervene, even if there is no supporting evidence.
A leading manufacturer of locking plates recommends their use in “Dislocated two-, three-, and four-fragment fractures of the proximal humerus, including fractures involving osteopenic bone” (17). This broad indication of the implant is justified with reference to the principles of anatomical reduction followed by stable fixation. However, it remains unclear to what extent these general principles apply to geriatric proximal humeral fractures.
The biomechanical rationale supporting the use of locking plates may be convincing (Figure 2) but whatever the biomechanical properties we cannot escape that it is wishful thinking that this transfers to clinical practice, especially in osteoporotic bone.
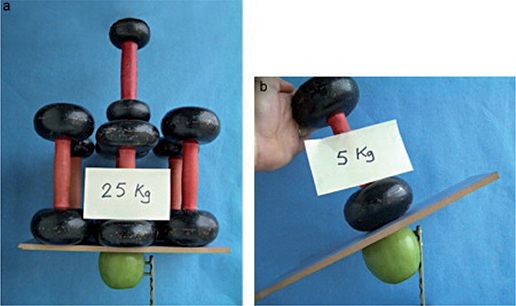
Figure 2. Loading test demonstrating the loading strength of 2 locking screws (a) compared with 2 common screws (b). Published with permissin from (20).
Most orthopedic residents use mobile application platforms to support clinical practice and decision-making. 2 of the most popular platforms recommend the use of locking plates. Orthobullets recommends locking plates in displaced 2-part fractures (18) while AO Surgery Reference recommends locking plates in selected 2-part, 3-part, and 4-part fracture patterns. In 2-part fractures osteoporotic bone is mentioned as a “supporting indication” (19).
Surgeon-related factors supporting a culture of acting may include ignorance of the literature or an unjustified belief in the benefits of their own surgical performance.
Conclusion
Without strong clinical evidence, the use of locking plates in geriatric shoulder fractures was globally adopted 2 decades ago. Despite high failure rates and increasing evidence for non-superiority the procedure is still commonly performed. This may have unfavorable implications. Balancing benefits and harms is essential prior to treatment decisions to avoid harm, especially in fragile elderly patients. No strong evidence supports the use of locking plates in geriatric shoulder fractures and de-implementation seems necessary.
- Klug A, Gramlich Y, Wincheringer D, Schmidt-Horlohé K, Hoffmann R. Trends in surgical management of proximal humeral fractures in adults: a nationwide study of records in Germany from 2007 to 2016. Arch Orthop Trauma Surg 2019; 139(12): 1713-21. doi: 10.1007/s00402019-03252-1.
- Huttunen T T, Launonen A P, Pihlajamäki H, Kannus P, Mattila V M. Trends in the surgical treatment of proximal humeral fractures: a nationwide 23-year study in Finland. BMC Musculoskelet Disord 2012; 13(1): 261. doi: 10.1186/1471-2474-13-261.
- Sumrein B O, Huttunen T T, Launonen A P, Berg H E, Felländer-Tsai L, Mattila V M. Proximal humeral fractures in Sweden: a registry-based study. Osteoporos Int 2017; 28(3): 901-7. doi: 10.1007/s00198-0163808-z.
- Bell J-E, Leung B C, Spratt K F, Koval K J, Weinstein J D, Goodman D C, et al. Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. J Bone Joint Surg Am 2011; 93(2): 121-31. doi: 10.2106/JBJS.I.01505.
- Jo Y-H, Lee K-H, Lee B-G. Surgical trends in elderly patients with proximal humeral fractures in South Korea: a population-based study. BMC Musculoskelet Disord 2019; 20(1): 136. doi: 10.1186/s12891-019-2515-2.
- Handoll H H, Brorson S. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev 2015; (11): CD000434. doi: 10.1002/14651858.CD000434.pub4.
- Olerud P, Ahrengart L, Ponzer S, Saving J, Tidermark J. Internal fixation versus nonoperative treatment of displaced 3-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elbow Surg 2011; 20(5): 747-55. doi: 10.1016/j.jse.2010.12.018.
- Fjalestad T, Hole M Ø, Hovden I A H, Blücher J, Strømsøe K. Surgical treatment with an angular stable plate for complex displaced proximal humeral fractures in elderly patients: a randomized controlled trial. J Orthop Trauma 2012; 26(2): 98-106. doi: 10.1097/BOT.0b013e31821c2e15.
- Rangan A, Handoll H, Brealey S, Jefferson L, Keding A, Martin B C, et al., PROFHER Trial Collaborators. Surgical vs nonsurgical treatment of adults with displaced fractures of the proximal humerus: the PROFHER randomized clinical trial. JAMA 2015; 313(10): 1037-47. doi: 10.1001/jama.2015.1629.
- Handoll H H, Keding A, Corbacho B, Brealey S D, Hewitt C, Rangan A. Five-year follow-up results of the PROFHER trial comparing operative and non-operative treatment of adults with a displaced fracture of the proximal humerus. Bone Joint J 2017; 99-B(3): 383-92. doi: 10.1302/0301-620X.99B3.BJJ-2016-1028.
- Launonen A P, Sumrein B O, Reito A, Lepola V, Paloneva J, Jonsson K B, et al., as the NITEP group. Operative versus non-operative treatment for 2-part proximal humerus fracture: a multicenter randomized controlled trial. PLoS Med 2019; 16(7): e1002855. doi: 10.1371/journal.pmed.1002855.
- Brorson S, Frich L H, Winther A, Hróbjartsson A. Locking plate osteosynthesis in displaced 4-part fractures of the proximal humerus. Acta Orthop 2011; 82(4): 475-81. doi: 10.3109/17453674.2011.588856.
- Brorson S, Rasmussen J V, Frich L H, Olsen B S, Hróbjartsson A. Benefits and harms of locking plate osteosynthesis in intraarticular (OTA Type C) fractures of the proximal humerus: a systematic review. Injury 2012; 43(7): 999-1005. doi: 10.1016/j.injury.2011.08.025.
- Beeres F J P, Hallensleben N D L, Rhemrev S J, Goslings J C, Oehme F, Meylaerts S A G, et al. Plate fixation of the proximal humerus: an international multicentre comparative study of postoperative complications. Arch Orthop Trauma Surg 2017; 137(12): 1685-92. doi: 10.1007/s00402-017-2790-z.
- Panagiotopoulou V C, Varga P, Richards R G, Gueorguiev B, Giannoudis P V. Late screw-related complications in locking plating of proximal humerus fractures: a systematic review. Injury 2019; 50(12): 217695. doi: 10.1016/j.injury.2019.11.002.
- Barlow J D, Logli A L, Steinmann S P, Sems S A, Cross W W, Yuan B J, et al. Locking plate fixation of proximal humerus fractures in patients older than 60 years continues to be associated with a high complication rate. J Shoulder Elbow Surg 2020; 29(8): 1689-94. doi: 10.1016/j.jse.2019.11.026.
- Synthes Depuy.Philos and Philos Long. Surgical Technique. Synth. GmbH 2016. p. 1-36. http://synthes.vo.llnwd.net/o16/LLNWMB8/INT%20Mobile/Synthes%20International/Product%20Support%20 Material/legacy_Synthes_PDF/DSEM-TRM-0815-0449-1_LR.pdf(Accessed Jan 15 2022).
- Orthobullets. Proximal Humerus Fractures. Lineage Med. Inc 2022. https://www.orthobullets.com/trauma/1015/proximal-humerus-fractures ( Accessed Jan 15 2022).
- Jaeger M, Leung F L W. Proximal humerus. AO Surg. Ref 2011 (Accessed Jan 15 2022). https://surgeryreference.aofoundation.org/ orthopedic-trauma/adult-trauma/proximal-humerus
- Cronier P, Pietu G, Dujardin C, Bigorre N, Ducellier F, Gerard R. The concept of locking plates. Orthop Traumatol Surg Res 2010; 41(12): 1262-5. doi: 10.1016/j.otsr.2010.03.008.