Unchanged incidence but change in treatment trends from 1996 to 2018: 23,718 humeral shaft fractures from the Danish National Patient Registry
Dennis KARIMI 1, Søren Wacher QVISTGAARD 1, Per Hviid GUNDTOFT 1,2, Stig BRORSON 3, and Bjarke VIBERG 1,4
1 Department of Orthopedic Surgery and Traumatology, Lillebaelt Hospital, University Hospital of Southern Denmark; 2 Department of Orthopedic Surgery and Traumatology, Aarhus University Hospital; 3 Centre for Evidence-Based Orthopedics, Zealand University Hospital and Department of Clinical Medicine, University of Copenhagen; 4 Department of Orthopedic Surgery and Traumatology, Odense University Hospital and Department of Clinical Research, University of Southern Denmark, Denmark
Background and purpose — Humeral shaft fractures (HSF) can be treated surgically or non-surgically. National trends and distributions are sparsely reported. We present the temporal trends in epidemiology of adult HSF in Denmark, with the primary aim of reporting HSF incidences, and the secondary aim of reporting on the primary treatment management.
Patients and methods — The diagnosis (International Classification of Diseases Version 10 [ICD-10]: S42.3) and surgical procedure codes for HSF were obtained from the Danish National Patient Registry (DNPR) covering 1996–2018. The diagnosis code for HSF is validated in the DNPR with a positive predictive value of 89%. Patients aged 18 years and above were included. Surgical treatment was defined as a diagnosis of HSF combined with a surgical procedure within 3 weeks of injury. Cases without relevant registered procedures within 3 weeks were defined as nonsurgical treatment cases.
Results — 23,718 HSF (62% female) were identified in the DNPR. The overall mean incidence was 25/100,000/year and was stable over 23 years. The population above 50 years accounted for 78% of all HSF. Non-surgical treatment accounted for 87% of treatments and was stable during the study period. Temporal changes were observed regarding surgical procedures; intramedullary nailing decreased from 57% to 26% and plate osteosynthesis increased from 12% to 69%.
Conclusion — The overall incidence for HSF remained stable from 1996 to 2018. Most cases were females aged 50 years and above. The preferred primary treatment for HSF was non-surgical for all ages. Plate osteosynthesis became more popular than intramedullary nailing over the study period.
Citation: Acta Orthopaedica 2023; 94: 523–529. DOI: https://doi.org/10.2340/17453674.2023.21125.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2023-03-15. Accepted: 2023-09-16. Published: 2023-10-13.
Correspondence: Dennis.karimi@rsyd.dk
DK, PG, and BV conceived the idea for the study. All authors participated in planning the study. BV provided the dataset. DK performed the data analyses. DK drafted the manuscript.
Handling co-editor: Taco Gosens
Acta thanks Nicholas David Clement, Hanna Cecilia Björnsson Hallgren, Michiel Verhofstad and an anonymous reviewer for help with peer review of this manuscript.
Humeral shaft fractures (HSF) are commonly managed either through non-surgical treatment with a functional brace or surgical intervention utilizing plate osteosynthesis or intramedullary nailing [1]. However, high-quality data comparing the treatments is sparse and is limited by high risk of bias due to unclear treatment indications in observational studies and the relatively younger age of participants in the randomized trials compared with the population mean age [2,3].
The management of adult HSF is debated, and only a few register-based studies have reported on treatment [4,5]. These studies have reported a high and increasing proportion of surgical treatment. In contrast to Scandinavian countries, the reported prevalence of surgical treatment elsewhere appears to be higher [6,7].
Recent epidemiological research consistently indicates that the HSF population predominantly comprises patients with fragility fractures, which is likely associated with a growing prevalence of osteoporosis [4,5,7-12]. However, these studies are hampered by low completeness, which is why there is lack of good quality national register studies.
Therefore, a nationwide overview of the epidemiology and management of adult HSF is required to describe temporal trends. The primary aim was to report the overall and age-specific incidence of HSF and the secondary aim was to estimate the distribution of primary non-surgical and surgical treatment.
Patients and methods
Design
This is a national register-based study on HSF in adults. The reporting of this study conforms to the Reporting of studies Conducted using Observational Routinely-collected health Data (RECORD) Statement [13].
Setting
The study was conducted in Denmark, where all persons with permanent citizenship are registered in a national register and are provided with a unique identification number [14]. This allows for exact individual-level record linkage between registers [15]. The identification number follows the person until death or emigration, and the Civil Registration System continuously updates this information with accurate censoring upon event. The Danish healthcare system is tax-supported and includes free access to general practitioners, hospitals, outpatient specialty clinics, and services for all persons granted a residence permit [16]. Emergency diagnosis with radiographic imaging is possible only in Danish public hospitals, and the healthcare services are registered for reimbursements. Therefore, all patients with an HSF are registered in the Danish National Patient Registry (DNPR).
Data source
The DNPR is a population-based administrative register used for continuous monitoring of hospitals and healthcare services in Denmark [17]. It records data per visit, and patients may have several records linked by their unique identification number. In 1978, the register achieved national coverage in collecting information on inpatient admissions to somatic departments. Diagnoses have been registered using the International Classification of Diseases Version 10 (ICD-10) with national extensions since 1994, and surgeries have been coded using the Nordic Medico-Statistical Committee Classification of Surgical Procedures since 1996 [17,18]. The completeness of patient registration in the DNPR is 98.8%, as departments are required by law to report administrative data including diagnosis and procedure codes [17,19]. The authors were able to access individual-level data from 1996 to 2018 from the DNPR and population estimations were accessible from Statistics Denmark [20].
Participants
The study population included all adult patients 18 years or older who were registered at Danish emergency departments with an HSF (ICD-10: S42.3) in the DNPR from 1996 through 2018. The accuracy of the HSF diagnosis code in the DNPR has been validated with a positive predictive value (PPV) of 89% [21]. All new HSF diagnoses that were reported from an emergency department within 90 days after the primary HSF diagnosis were removed from the dataset to minimize errors in coding due to possible reencounters. After this period, the same patient could re-enter the dataset with a new HSF diagnosis. Diagnoses reported from outpatient clinics were not included in the dataset.
Variables
Surgical procedure codes indicated whether patients were primarily treated non-surgically or surgically. Surgical procedures were defined as those with relevant surgical procedure codes (Table A, see Supplementary data) within 21 days from the first registered contact. If no relevant procedure codes were reported within the first 21 days, the treatment was defined as non-surgical. Similarly, all patients with a relevant surgical procedure code within the first 21 days were coded as primary surgical treatment. Surgical procedure codes were further divided into 3 categories: plate osteosynthesis (KNBJ61), nail osteosynthesis (KNBJ51), and “other procedures” (external fixation [KNBJ21], K-wire fixation [KNBJ41], screw fixation [KNBJ71], and combined fixation [KNBJ81]).
199 cases of HSF with a registered shoulder arthroplasty procedure code were omitted prior to the analysis due to the likelihood of misclassification issues of proximal humeral fractures. An HSF that requires arthroplasty must involve the proximal end to an extent that the fracture entity is consistent with a proximal humeral fracture.
Statistics
Descriptive statistics were used to report on age, sex, number of HSF, and primary treatment approach. Crude, age-adjusted, and age-specific incidence rates for age strata of 5 years were estimated using the number of new HSF cases per 100,000 persons for each calendar year. The mid-year populations for adults (≥ 18 years) for each calendar year were estimated using data from Statistics Denmark [20]. To reflect the increased risk of fractures with age and to account for the ageing population, direct standardization and age stratification were used to estimate the age-adjusted rate. European population data was used to represent the standard population [22]. Temporal changes were visually summarized using line charts with 95% confidence intervals (CI) to account for the uncertainty associated with the point estimates. Crude incidence rates were used to calculate CIs for incidence rates, stratified by both sex and age strata of 20 years. Population proportions were used to calculate CIs for treatment approach and procedure estimates. A clinically relevant trend was defined as a change of more than 10% in the study period.
Ethics, funding, and disclosures
Data approval was obtained (Region of Southern Denmark, jr.nr. 20/187). According to Danish legislation, no further approval was needed. No funding was obtained, and the authors have no conflicts of interest to declare. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.21125
Results
All adults diagnosed with HSF between 1996 and 2018 were included for analysis apart from cases with registered shoulder arthroplasty. 23,718 were included for analysis (Figure 1).

Figure 1. Flowchart of patients.
Epidemiology
Females accounted for 62% of the patients (Table 1). The age distribution for females was unimodal, with the highest number of HSFs in the 75–79-year age group (Figure 2). The age distribution for males was bimodal, with the highest number of HSFs in the 18–24-year and 55–59-year age groups. The second peak started to increase around the age of 50 years. The population over 50 years of age accounted for 78% of all HSF cases.
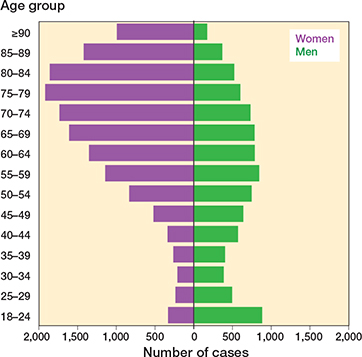
Figure 2. Humeral shaft fracture distribution by age group and sex.
Between 1996 and 2018, the absolute increase in HSF was 21%. Female HSFs increased by 28% and male HSFs increased by 7%. The absolute increase stratified by age group was 1% in the 18–64-year age group, and 39% in the ≥ 65-year age group. The mean incidence rate was 25 fractures (range 21–28) per 100,000 persons per year (Table B, see Supplementary data). The trend was stable for crude and age-standardized incidence rates. The trend remained stable following stratification by sex and age strata of 20 years; however, in men 80 years and older, the trend declined (Figure 3).
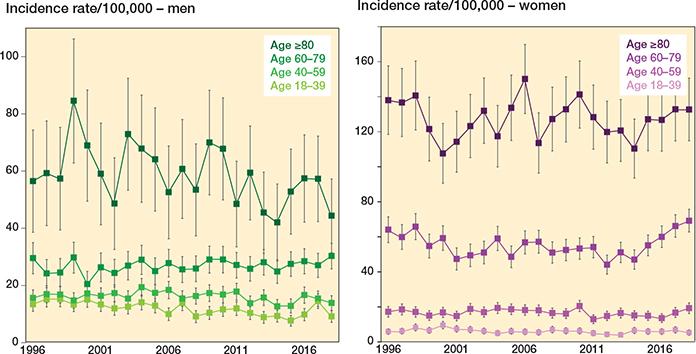
Figure 3. National incidence rates with 95% CIs for humeral shaft fractures by age group and sex from 1996 to 2018.
The overall and sex-stratified age-specific incidence rates increased gradually with age. The overall rate increased from 11 to 141 fractures per 100,000 persons per year (Figure 4). Incidence rates by sex were almost equal from 18 to 50 years of age, with higher incidence rates for males. The incidence rates for sexes crossed at 50–54 years of age. Mean differences for male incidence rates were 5 points higher than females until 50 years; this difference changed to 37 points, favoring females from 50 years and older (Table B, see Supplementary data).
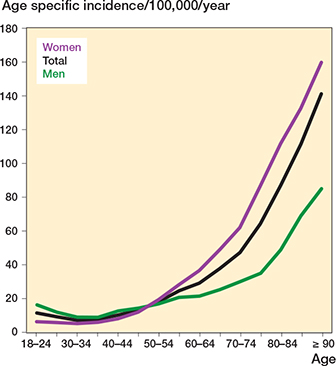
Figure 4. Age-specific incidence rates for humeral shaft fractures from 1996 to 2018.
Treatment
The proportion of cases with primary non-surgical treatment was 87% (range 84–89%, n = 20,534) (Table C, see Supplementary data). HSF was predominately treated non-surgically between 1996 and 2018, without any considerable changes in the distribution between surgical and non-surgical treatment (Figure 5).

Figure 5. Annual distribution with CI for primary treatment of humeral shaft fractures by sex from 1996 to 2018.
The predominant choice of implants (Figure 6) also changed throughout the study period when stratified by age (Figure 7). In 1996, intramedullary nails were the preferred choice of treatment implant and were used in 57% of surgically treated HSFs, equaling 7% of the total number of HSFs in 1996. Over the period 2007 to 2018, plate osteosynthesis became the preferred method. By 2018, plate osteosynthesis was used in 69% of surgical cases. The use of other techniques decreased from 30% to 5% and included external fixation, screw fixation, K-wire fixation, and combined fixation.

Figure 6. Annual distribution with CI of surgical treatment implants for humeral shaft fractures from 1996 to 2018.
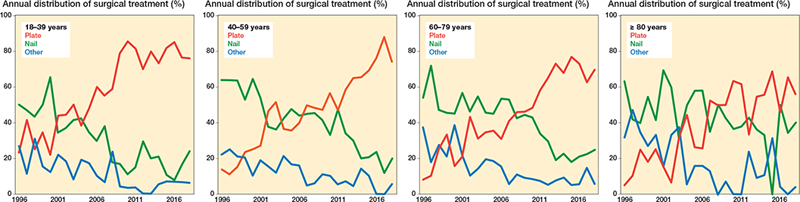
Figure 7. Annual distribution of surgical treatment implants in 4 age groups of humeral shaft fractures.
Surgical treatment was more frequently used in younger patients (Figure 8).

Figure 8. Age-specific treatment distribution for humeral shaft fractures from 1996 to 2018.
Discussion
We aim to report HSF incidences and distribution of primary treatments in Denmark from 1996 to 2018. We showed a stable incidence rate of 25 fractures/100,000 persons per year with an overall increase of HSF that was 20% driven by the age group 65 years and older. Regarding surgery, we showed stable trends in choice of treatment with a strong preference for non-surgical treatment; however, plate osteosynthesis surpassed intramedullary nailing as the preferred surgical method.
Epidemiology
The absolute increase in the elderly population (≥ 65 years) by 40% indicates that population ageing and the underlying increase in the prevalence of osteoporosis may be a risk for HSF.
The incidence rate gradually increased with age; for women, the rate increased exponentially from the sixth decade. Most HSFs occurred in women (62%), and 78% of all HSFs were sustained over the age of 50 years. This supports the statement that most HSFs should be considered osteoporosis-related fractures. Previous epidemiological studies have reported comparable fracture incidences and distribution of HSF by age and sex [5,8-12]. The incidence has been reported as between 7 and 20 fractures/100,000 persons per year. Mahabier et al. [5] also included pediatric humeral shaft fractures, which explains the lower reported incidence. The other studies report slightly higher incidences ranging from 12 to 20 fractures/100,000 persons per year [8-12]. Comparable to the Danish setting, the 2 Swedish studies based on 401 and 262 HSFs estimated an overall incidence rate of approximately 14 fractures/100,000 per year for 1998–1999 and 2011–2013, respectively [10,11]. Furthermore, similar to our findings, the incidence rate reported in these studies increased with age and showed the same steep increase from the sixth decade.
This study reported higher overall incidence compared with other countries, which could be due to a higher rate of identified HSF. To mitigate inaccuracies caused by readmissions, a 90-day “quarantine period” was established [23].
Treatment
We found that non-surgical treatment was the preferred choice for HSF management in 87% of cases, with surgical treatment gradually decreasing with advancing age. In cases aged 18–24 years, 20% had surgical treatment, whereas this proportion gradually decreased to 7% in cases aged 90 years or older in agreement with Swedish data but higher than Finnish data with 53% of cases non-surgically treated [7]. In 2 register-based studies from the USA and the Netherlands, the predominant choice of management was surgical treatment with rates of 68% and 67%, respectively [4,5]. However, a similar decrease in surgical utilization with increasing age was reported.
The variation in treatment management between countries is likely due to the lack of large randomized trials with sufficient external validation and low risk of bias.
While the overall treatment management remained stable throughout the study period, there was a notable shift in method preference in our study. Intramedullary nailing was gradually replaced by plate osteosynthesis as the primary choice across all age groups, with the use of plates surging from 12% to 69% between 1996 and 2018. This trend corresponded with findings from studies conducted in the USA and Finland [4,24]. This may be caused by the increased risk of shoulder complaints with an antegrade humeral nail, but no clinically relevant risk differences have been demonstrated between the implants [25]. Furthermore, this shift in implant preference may be closely linked to technological advancements with the introduction of locking plates in the early 2000s, corresponding to a period of increased plate usage as seen in other studies [26,27], underlining the role of innovation in driving this shift in implant preference.
In Denmark, non-surgical treatment for HSF is favored, with a higher proportion compared with other Western countries. The preference for non-surgical treatment may be explained by the high treatment threshold: 7 patients need surgery to avoid 1 nonunion [2]. Yet, the serious risks of surgery, such as infection, nerve injury, and re-intervention, must be considered. However, in other Western countries patients do not have similar rights to full pay during sick leave, which may change patients’ preference towards surgery, as it typically yields faster recovery.
Strengths and limitations
The DNPR has national coverage, and hospitals are required by law to continuously report administrative data to the authorities. This ensures high completeness of the DNPR regarding HSF. We cannot dismiss that some patients are treated in the private sector; however, it became a requirement in 2003 that all private healthcare was reported to the DNPR, and private emergency departments do not exist [17]. Therefore, the missed data would only include patients who did not receive emergency treatment for an HSF, which we believe is few.
A further limitation is the lack of data accuracy for procedure codes in the DNPR for HSF. However, the registration of orthopedic procedures is generally high in Denmark [28], and the classification of surgical procedures has not changed since 1996. Therefore, we assume that the coding practice was stable throughout the study period. Fractures are not registered in the DNPR using a fracture classification system, and erroneous coding cannot be detected through the register.
A strength of this study is that the HSF diagnosis in the DNPR has been validated and has a high PPV (89%). However, there may have been an overestimation of the incidence as the accuracy is not optimal [21]. Furthermore, the validity study showed that a majority of the misclassified cases consisted of proximal humeral fractures. In Denmark, non-surgical treatment is the common approach for proximal humeral fractures [26]. Consequently, this misclassification would be primarily attributed to 1 treatment, leading to an overestimation of non-surgical treatment.
The definition of primary treatment for HSF within a 21-day timeframe is representative of the Danish healthcare context [26,27]. In Denmark, surgical treatment of a humeral shaft fracture is rarely performed on the same day but most likely the extended 21-day window ensures all procedures are included and accurate documentation of the actual prevalence of such interventions without including secondary procedures. Currently, the DNPR cannot be used to report on secondary procedures following HSF. Comprehensive validation procedures for nonunion diagnosis and reoperation procedure codes are necessary to ensure accurate reporting of nonunion and reoperation rates.
Conclusion
In Denmark, most HSFs occur after the age of 50 years and the incidence increases with age. Between 1996 and 2018, the overall incidence remained stable. Non-surgical treatment was the preferred choice for all ages, although surgery was more common in younger patients. Over time, plate osteosynthesis replaced intramedullary nailing as the preferred method for all ages.
Supplementary data
Tables A–C are available as supplementary data on the article page, doi: 10.2340/17453674.2023.21125
- Gallusser N, Barimani B, Vauclair F. Humeral shaft fractures. EFORT Open Rev 2021; 6(1): 24-34. doi: 10.1302/2058-5241.6.200033.
- Oliver W M, Bell K R, Molyneux S G, White T O, Clement N D, Duckworth A D. Surgical versus nonsurgical management of humeral shaft fractures: a systematic review and meta-analysis of randomized trials. J Am Acad Orthop Surg 2023; 31(2): e82-93. doi: 10.5435/JAAOS-D-22-00432.
- Van Bergen S H, Mahabier K C, Van Lieshout E M M, Van der Torre T, Notenboom C A W, Jawahier P A, et al. Humeral shaft fracture: systematic review of non-operative and operative treatment. Arch Orthop Trauma Surg 2023; (0123456789). doi: 10.1007/s00402-023-04836-8.
- Schoch B S, Padegimas E M, Maltenfort M, Krieg J, Namdari S. Humeral shaft fractures: national trends in management. J Orthop Traumatol 2017; 18(3): 259-63. doi: 10.1007/s10195-017-0459-6.
- Mahabier K C, Hartog D Den, Van Veldhuizen J, Panneman M J M, Polinder S, Verhofstad M H J, et al. Trends in incidence rate, health care consumption, and costs for patients admitted with a humeral fracture in the Netherlands between 1986 and 2012. Injury 2015; 46(10): 1930-7. doi: 10.1016/j.injury.2015.07.025.
- Ekholm R, Tidermark J, Törnqvist H, Adama J, Ponzer S. Outcome after closed functional treatment of humeral shaft fractures. J Orthop Trauma Surg 2006; 20(9): 591-6. doi: 10.1097/01.bot.0000246466.01287.04.
- Mattila H, Keskitalo T, Simons T, Ibounig T, Rämö L. Epidemiology of 936 humeral shaft fractures in a large Finnish trauma center. J Shoulder Elbow Surg 2023; 206-15. doi: 10.1016/j.jse.2022.10.020
- Kim S H, Szabo R M, Marder R A, Marder A. Epidemiology of humerus fractures in the United States: nationwide emergency department sample, 2008. Arthritis Care Res (Hoboken) 2012; 64(3): 407-14. doi: 10.1002/acr.21563.
- Oliver W M, Searle H K C, Ng Z H, Duckworth A D, Wickramasinghe N R L, Molyneux S G, et al. Fractures of the proximal- and middle-thirds of the humeral shaft should be considered as fragility fractures: an epidemiologic AI study of 900 consecutive injuries. Bone Joint J 2020; 102-B(11): 1475-83. doi: 10.1302/0301-620X.102B11.BJJ-2020-0993.R1.
- Bergdahl C, Ekholm C, Wennergren D, Nilsson F, Möller M. Epidemiology and patho-anatomical pattern of 2,011 humeral fractures: data from the Swedish Fracture Register. BMC Musculoskelet Disord 2016; 1-10. doi: 10.1186/s12891-016-1009-8.
- Ekholm R, Adami J, Tidermark J, Hansson K, Törnkvist H, Ponzer S. Fractures of the shaft of the humerus: an epidemiological study of 401 fractures. J Bone Joint Surg Br 2006; 88(11): 1469-73. doi: 10.1302/0301-620X.88B11.17634.
- Tytherleigh-Strong G, Walls N, McQueen M M. The epidemiology of humeral shaft fractures. J Bone Joint Surg Br 1998; 80(2): 249-53. doi: 10.1302/0301-620x.80b2.8113.
- Benchimol E I, Smeeth L, Guttmann A, Harron K, Moher D, Peteresen I, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) Statement. PLoS Med 2015; 12(10): 1-22. doi: 10.1371/journal.pmed.1001885.
- Pedersen C B. The Danish civil registration system. Scand J Public Health 2011; 39(7): 22-5. doi: 10.1177/1403494810387965.
- Thygesen L C, Daasnes C, Thaulow I, Brønnum-Hansen H. Introduction to Danish (nationwide) registers on health and social issues: structure, access, legislation, and archiving. Scand J Public Health 2011; 39(7): 12-16. doi: 10.1177/1403494811399956.
- Danish Health Authority. The Danish Healthcare System [Det danske sundhedsvæsen]; 2016. 24 p. Available from: https://www.sst.dk/~/media/294CC6232ACD47E19C5B6B6F737A2512.ashx
- Schmidt M, Schmidt S A J, Sandegaard J L, Ehrenstein V, Pedersen L, Sørensen H T. The Danish National patient registry: a review of content, data quality, and research potential. Clin Epidemiol 2015; 7:449-90. doi: 10.2147/CLEP.S91125.
- NOMESCO Classification of Surgical Procedures 2009. Available from: http://norden.diva-portal.org/smash/get/diva2:968721/FULLTEXT01.pdf.
- Danish Health Authority. Data quality report from DNPR 2019 [Datakvalitetsrapport om LPR 2019] [Internet] 2020. Available from: https://sundhedsdatastyrelsen.dk/-/media/sds/filer/registre-og-services/nationale-sundhedsregistre/sygdomme-laegemidler-og-behandlinger/landspatientregisteret/lpr-i-fremtiden/datakvalitetsrapport-om-lpr-2019-_-overgangen-fra-lpr2-til-lpr3.pdf?la=da
- Statistics Denmark 2022 [Internet]. Available from: https://www.dst.dk/en. Available from: https://www.dst.dk/en
- Karimi D, Houkjær L, Gundtoft P, Brorson S, Viberg B. Positive predictive value of humeral fractures in the Danish National Patient Registry. Dan Med J 2023; 70(4): 1-7. PMID: 36999816.
- Public Health Scotland. Standard Population 2022. Available from: https://www.opendata.nhs.scot/dataset/standard-populations.
- Bergdahl C, Nilsson F, Wennergren D, Ekholm C, Möller M. Completeness in the Swedish fracture register and the Swedish national patient register: an assessment of humeral fracture registrations. Clin Epidemiol 2021; 13: 325-33. doi: 10.2147/CLEP.S307762.
- Huttunen T T, Kannus P, Lepola V, Pihlajamäki H, Mattila V M. Surgical treatment of humeral-shaft fractures: a register-based study in Finland between 1987 and 2009. Injury 2012; 43(10): 1704-8. doi: 10.1016/j.injury.2012.06.011.
- Beeres F J P, van Veelen N, Houwert R M, Link B C, Heng M, Knobe M, et al. Open plate fixation versus nailing for humeral shaft fractures: a meta-analysis and systematic review of randomised clinical trials and observational studies. Eur J Trauma Emerg Surg 2021; 48(4): 2667-82. doi: 10.1007/s00068-021-01728-7.
- Brorson S, Viberg B, Gundtoft P H, Jalal B, Ohrt-Nissen S. Epidemiology and trends in management of acute proximal humeral fractures in adults: an observational study of 137,436 cases from the Danish National Patient Register. Acta Orthop 2022; 750-5. doi: 10.2340/17453674.2022.4578.
- Viberg B, Tofte S, Rønnegaard A B, Jensen S S, Karimi D, Gundtoft P H. Changes in the incidence and treatment of distal radius fractures in adults: a 22-year nationwide register study of 276,145 fractures. Injury 2023 ; 54(May): 110802. doi: 10.1016/j.injury.2023.05.033.
- Lass P, Lilholt J, Thomsen L, Lundbye-Christensen S, Enevoldsen H, Simonsen O H. Kvaliteten af diagnose- og procedurekodning i ortopædkirurgi Nordjylland. Ugeskr Laeger 2006; 168(48): 4212-5. PMID: 17147947.