No difference in short-term readmissions following day-case vs. one overnight stay in patients having hip and knee arthroplasty: a nationwide register study of 51,042 procedures from 2010–2020
Christian Bredgaard JENSEN 1, Anders TROELSEN 1, Nicolai Bang FOSS 2, Christian Skovgaard NIELSEN 1, Martin LINDBERG-LARSEN 3, and Kirill GROMOV 1
1 Department of Orthopaedic Surgery, Clinical Orthopaedic Surgery Hvidovre (CORH), Copenhagen University Hospital Hvidovre, Hvidovre; 2 Department of Anesthesiology, Copenhagen University Hospital Hvidovre, Hvidovre; 3 Department of Orthopaedic Surgery, Orthopaedic Research Unit (ORU), Odense University Hospital, Odense, Denmark
Background and purpose — Day-case hip and knee arthroplasty has gained in popularity, but there are conflicting results regarding readmissions. We aimed to investigate differences in 30- and 90-day readmission rates between day-case patients and patients with a single overnight stay following primary total hip arthroplasty (THA), total knee arthroplasty (TKA), and unicompartmental knee arthroplasty (UKA).
Patients and methods — We identified day-case (DC) and overnight (ON) THA, TKA, and UKA patients, operated on between 2010 and 2020, from the Danish National Patient Register. Day-case surgery was defined as discharge on the day of surgery. Overnight readmissions within 30 or 90 days of surgery were considered readmissions. We compared readmission rates between DC and ON patients within arthroplasty types using logistic regression adjusted for patient characteristics and year of surgery. We included 29,486 THAs (1,353 DC and 28,133 ON), 15,116 TKAs (617 DC and 14,499 ON), and 6,440 UKAs (1,528 DC and 4,914 ON).
Results — The 30-day readmission rates were: DC-THA 4.4% vs. ON-THA 4.4% (adjusted odds-ratio [aOR] 1.2, 95% confidence interval [CI] 0.91–1.6), DC-TKA 4.7% vs. ON-TKA 4.4% (aOR 1.1, CI 0.69–1.5), and DC-UKA 3.0% vs. ON-UKA 3.0% (aOR 1.1, CI 0.78–1.5). Similarly, no significant differences were present between DC and ON THA, TKA, and UKA regarding 90-day readmissions or time to readmission.
Conclusion — We found no differences in readmission rates between day-case THA, TKA, and UKA patients and patients with a single overnight stay.
Citation: Acta Orthopaedica 2023; 94: 516–522. DOI: https://doi.org/10.2340/17453674.2023.18658.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2023-05-01. Accepted: 2023-09-02. Published: 2023-10-13.
Correspondence: christian.bredgaard.jensen@regionh.dk
CBJ and KG had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: CBJ, AT, and KG. Acquisition, analysis, and interpretation of data: all authors. Drafting of the manuscript: CBJ and KG. Critical revision of the manuscript for important intellectual content: all authors.
Handling co-editors: Li Felländer-Tsai and Philippe Wagner
Acta thanks Harald Brismar and Rami Madanat for help with peer review of this manuscript.
Improvements in the surgical procedure and the implementation of rapid recovery protocols in arthroplasty centers have reduced length of stay (LOS), morbidity, and mortality, and improved convalescence [1,2].
Day-case surgery (outpatient surgery/day of surgery discharge) may offer cost reductions due to shorter hospital stay and may decrease bed occupancy [3]. Previous investigations of readmission and complications following day-case hip and knee arthroplasty offer conflicting results. It has been indicated that day-case patients are less likely to be readmitted [4]; however, higher complication rates after day-case surgery have been reported as well [5,6]. Comparing day-case patients with patients with a single overnight stay might increase comparability between the groups. This would also increase the likelihood that both groups could have been suitable candidates for a day-case procedure, as day-case use remains low and varying [7] compared with the proportion of suitable candidates [8].
We therefore aimed to investigate the frequency of 30- and 90-day readmissions in day-case patients (DC patients) compared with patients with a single overnight stay (ON patients) following THA, TKA, and UKA on a national level in Denmark. Secondarily, we investigated 30- and 90-day complications as a measure of readmissions more directly related to surgery, as well as cases of mortality within 90 days of surgery.
Patients and methods
This study was based on data from the Danish National Patient Register (DNPR) and complies with the REporting of studies Conducted using Observational Routinely-collected Data ( RECORD) statement.
Data sources
The DNPR supplied data on patient characteristics, comorbidity, surgical procedures, and contacts with Danish hospitals. It is an administrative database that offers data on all contacts to Danish hospitals with a completeness of > 99% [9]. All Danish hospitals are required to report to the DNPR. Surgical codes in the DNPR are based on the Nordic Medico-Statistical Committee (NOMESCO) classification of surgical procedures (NCSP) whereas diagnosis codes are based on the International Classification of Diseases and Related Health Problems 10th Revision (ICD-10). The Danish Civil Registration System (CPR) register supplied data on mortality. Using the civil registration number of Danish inhabitants, mortality from CPR was linked to the data from DNPR.
Study population
We screened primary, unilateral THA, TKA, or UKA procedures registered in the DNPR between January 2010 and February 2020 for inclusion (THA: NFB20, NFB30, NFB40. TKA: NGB20, NGB30, NGB40. UKA: NGB01, NGB02, NGB11, NGB12). We excluded simultaneous bilateral procedures. The following ways of identifying simultaneous bilateral procedures were used: (1) 2 procedures on the same patient performed on the same date, but coded as right and left side, respectively, or (2) 1 procedure coded as both right and left side. We included only procedures performed as treatment for hip or knee osteoarthritis (OA) (M16n or M17n) and only each patient’s first procedure of each type within the study period. Any subsequent contralateral procedures of the same type were excluded. Based on the date of surgery and the discharge date, day-case (DC, discharge on the day of surgery) and single overnight stay (ON, discharge on the day after the surgery) patients were identified and included. Overall patient characteristics for DC, ON, and patients admitted > 1 night are displayed in Table 1 (see Appendix). How long patients were scheduled to be admitted for is unknown. We calculated the Charlson Comorbidity Index (CCI) score for all patients based on diagnosis codes from 10 years prior to surgery [10,11].
Outcome measures
We defined length of stay as the number of nights spent in hospital. Readmissions within 30 and 90 days were reported. Time from discharge to readmission was reported as the number of days from the discharge date and the date of the first readmission. Readmissions registered with a diagnosis code previously associated with arthroplasty complications were also registered as complications [12,13] (Table 2, see Appendix). Readmissions less than 4 hours after discharge from the primary surgical admission were not considered readmissions. They were instead joined with the primary surgical admission in accordance with recommendations from the Danish Health Data Authority for investigating readmissions [14,15] and counted as total number of nights spent across the joined admissions. Admissions not related to OA or physiotherapy, but with an overnight stay occurring more than 4 hours after discharge from the primary surgical admission, were registered as readmissions [14,15]. Admissions with an OA or physiotherapy diagnosis code were not registered as readmissions as these occurred routinely and represent routine follow-up and rehabilitation visits. Readmissions and complications within 30 and 90 days of surgery were reported. Cases of mortality within 90 days of surgery were also reported.
Statistics
We evaluated normality using QQ plots and histograms and presented continuous variables as mean and standard deviation (SD) or median and interquartile range (IQR) depending on distribution. Proportions of categorical outcome variables are presented as percentages and 95% confidence intervals (CI) using binomial exact calculation (Clopper-Pearson method [16]). Indications of imbalance in demographics and comorbidity between the DC patients and ON patients were evaluated using the standardized mean difference (SMD) with an SMD > 0.1 indicating imbalance. We included variables in adjusted analyses based on causal diagram analyses determining whether the variables have a confounding relationship with day-case surgery and readmissions [17]. We used logistic regression to compare 30-day and 90-day readmissions, 30-day and 90-day complications, and 90-day mortality between the DC group and the ON group. For 30-day and 90-day readmission, we also conducted logistic regression analyses adjusted for age (10-year increments), CCI (groups: 0, 1, 2, and > 2), sex, surgical year (groups: 2010–2013, 2014–2017, 2018–2020), and hospital type (private or publicly funded). Adjusted analyses for complications and mortality were not conducted because the number of cases was too low compared with the number of adjusting variables [18]. The results from the logistic regressions were presented as odds ratios (OR), 95% confidence intervals (CI). The fit of the regression models was evaluated using binned residual plots. Adjusting variables were investigated for multicollinearity using variance inflation factors, with a VIF > 5 indicating collinearity. We compared median time to readmission between DC and ON procedures using a Mann–Whitney U-test. P < 0.05 was considered significant. The statistical analyses were performed using R version 4.1.3 (R Core Team, 2022; R Foundation for Statistical Computing, Vienna, Austria) and R Studio version 2022.07.2 (R Studio Team, 2022).
Ethics, funding, and disclosures
The Knowledge Centre on Data Protection Compliance in the Capital Region of Denmark approved this study (approval nr. P-2021-132). As this was an observational study with no clinical intervention, no approval from regional or national research ethical committees was required and informed consent was waived. No funding was received specifically for this study. CBJ has received PhD funding from a grant from the Novo Nordisk Foundation unrelated to this study. KG and AT have received research support and speaker fees from Zimmer Biomet, and AT has received research support from Pfizer. NBF has received speaker fees from the Masimo Corporation and Edwards Lifesciences. All the above conflicts are unrelated to this study. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.18658
Results
During the 10-year period, 166,851 patients with a hip or knee OA diagnosis were treated with a unilateral THA, TKA, or UKA (Figure 1). 3,498 (2%) were DC patients and 47,544 (28%) were ON patients. Across the study period length of stay decreased from median 3 days to 1 day and the use of day-case surgery increased, as previously reported based on the same study population [7].
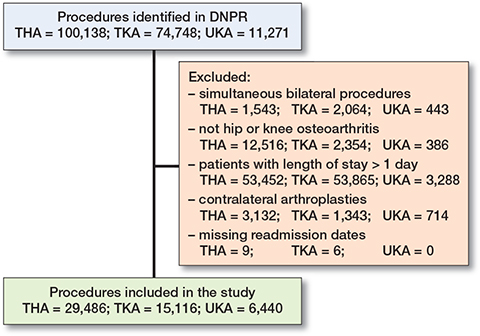
Figure 1. Flowchart showing exclusion of procedures and the final cohort of primary unilateral hip and knee arthroplasty procedures admitted for 0 days (day case) or 1 day (overnight). DNPR = Danish National Patient Register, THA = total hip arthroplasty, TKA = total knee arthroplasty, and UKA = unicompartmental knee arthroplasty.
Day-case patients were younger and had lower CCI except in the UKA patients (Table 3). The proportion of men was also higher in the DC-THA group. In the UKA group imbalance was not indicated between DC and ON patients regarding sex and CCI groups and in TKA no imbalance was indicated in sex.
We found no significant differences in short-term readmission or complication rates between DC and ON THA, TKA, or UKA patients (Table 4). DC-THA and ON-THA patients were both readmitted in 4.4% of cases within 30 days and in 6.8% vs. 6.9% of cases within 90 days of surgery corresponding to a difference in proportions of 0.02% (CI –1.2 to 1.5) and –0.13% (CI –1.8 to 1.5) regarding 30- and 90-day readmission rates, respectively. DC-TKA and ON-TKA patients were readmitted in 4.7% vs. 4.4% of cases within 30 days and in 7.8% vs. 6.9% of cases within 90 days corresponding to a difference in proportions of 0.3% (CI –1.2 to 3.0) and 0.9% (CI –0.5 to 4.6) regarding 30- and 90-day readmission rates, respectively. DC-UKA and ON-UKA patients had the fewest readmissions, as both groups were readmitted in 3.0% of cases within 30 days of surgery, and in 4.8% vs. 5.3% within 90 days corresponding to a difference in proportions of –0.03% (CI –1.3 to 1.4) and –0.43% (CI –2.5 to 0.94) regarding 30- and 90-day readmission rates, respectively.
| Day case | Overnight | Unadjusted OR (CI) | Adjusted | ||||||
| n | % (CI) | Day case | Day case | OR a (CI) | |||||
| THA cases | 1,353 | 28,133 | |||||||
| 30-day readmissions | 60 | 4.4 (3.4–5.7) | 1,242 | 4.4 (4.2–4.7) | 1.0 (0.76–1.3) | 1.2 (0.91–1.6) | |||
| 30-day complications | 34 | 2.5 (1.7–3.5) | 675 | 2.4 (2.2–2.6) | 1.1 (0.73–1.5) | ||||
| 90-day readmissions | 92 | 6.8 (5.5–8.3) | 1,949 | 6.9 (6.6–7.2) | 0.98 (0.78–1.2) | 1.2 (0.94–1.5) | |||
| 90-day complications | 50 | 3.7 (2.8–4.8) | 966 | 3.4 (3.2–3.7) | 1.1 (0.80–1.4) | ||||
| 90-day mortality | < 5 | – (<0.01–0.41) b | 45 | 0.16 (0.12–0.21) | 0.46 (0.03–2.1) | ||||
| TKA cases | 617 | 14,499 | |||||||
| 30-day readmissions | 29 | 4.7 (3.2–6.7) | 634 | 4.4 (4.0–4.7)) | 1.1 (0.72–1.6) | 1.0 (0.69–1.5) | |||
| 30-day complications | 6 | 0.9 (0.36–2.1) | 197 | 1.4 (1.2–1.6) | 0.71 (0.28–1.5) | ||||
| 90-day readmissions | 48 | 7.8 (5.8–10) | 1,000 | 6.9 (6.5–7.3)) | 1.1 (0.83–1.5) | 1.2 (0.89–1.7) | |||
| 90-day complications | 11 | 1.8 (0.89–3.2) | 325 | 2.2 (2.0–2.5) | 0.79 (0.41–1.4) | ||||
| 90-day mortality | < 5 | – (<0.01–0.90) b | 23 | 0.16 (0.10–0.24) | 1.0 (0.05–4.9) | ||||
| UKA cases | 1,528 | 4,912 | |||||||
| 30-day readmissions | 45 | 3.0 (2.2–3.8) | 146 | 3.0 (2.5–3.5) | 0.99 (0.70–1.4) | 1.1 (0.78–1.5) | |||
| 30-day complications | 20 | 1.3 (0.80–2.0) | 49 | 1.0 (0.74–1.3) | 1.3 (0.75–2.1) | ||||
| 90-day readmissions | 74 | 4.8 (3.8–6.0) | 259 | 5.3 (4.7–5.9) | 0.91 (0.70–1.2) | 0.96 (0.73–1.3) | |||
| 90-day complications | 32 | 2.1 (1.4–2.9) | 84 | 1.7 (1.4–2.1) | 1.2 (0.80–1.8) | ||||
| 90-day mortality | < 5 | – (<0.01–0.36) b | < 5 | – (<0.01–0.18) b | 1.1 (0.05–8.4) | ||||
| a Adjusted for age, sex, comorbidity, year of surgery, and type of hospital. | |||||||||
| b When < 5 cases were present exact numbers and percentages are not displayed. | |||||||||
| For abbreviations, see Table 3 and CI = 95% confidence interval. | |||||||||
The median number of days from discharge to readmission ranged from 17–25 days across all groups, with no significant differences between DC and ON patients (Figure 2).
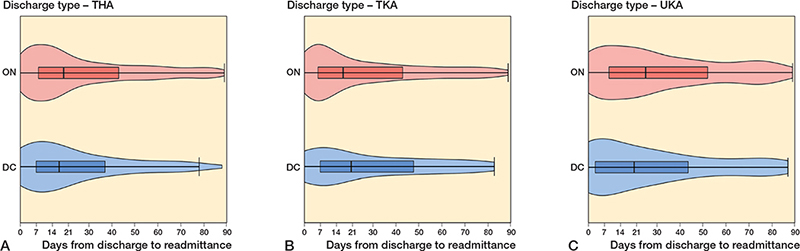
Figure 2. Violin plots (mirrored density curves) display probability density for days from discharge to readmission. As such, a higher density (amplitude) is present on the number of days where readmissions more frequently happen. Boxplots shows 25, 50, and 75 percentiles (box) as well as 5 and 95 percentiles (whiskers) for days from discharge to readmission. DC = day case, ON = overnight, THA = total hip arthroplasty, TKA = total knee arthroplasty, and UKA = unicompartmental knee arthroplasty.
A. Median time to readmission in DC-THAs was 17 days (IQR 7–37) compared with 19 days (IQR 8–43) in ON-THAs (P = 0.3).
B. Median time to readmission in DC-TKAs was 21 days (IQR 7–48) compared with 17 days (IQR 6-43) in ON-TKAs (P = 0.7).
C. Median time to readmission in DC-UKAs was 20 days (IQR 3–44) compared with 25 days (IQR 9–52) in ON-UKAs (P = 0.07).
Very few cases of mortality occurred in both DC and ON patients and due to data ethical restrictions we are not able report absolute numbers or percentages with less than 5 cases. However, no statistically significant differences were present in mortality rates between DC and ON patients irrespective of arthroplasty type (Table 4).
Discussion
The aim of our study was to investigate differences in readmission rates between DC and ON hip and knee arthroplasty patients. We found no significant differences in readmission or complication rates between DC and ON THA, TKA, or UKA patients. DC-THA and DC-UKA patients could at worst have readmission rates 1.5% higher, but at best 2.5% lower, than ON patients. However, DC-TKA patients could at worst have readmission rates 4.6% higher, but at best 1.5% lower, than ON-TKA patients.
In a review of DC TKAs compared with inpatient TKAs, the 90-day readmission rates ranged from 2.3–9.9% [19]. Our readmission rate of 7.8% in DC-TKAs seems to be at the higher end of the spectrum, potentially due to our wide definition of readmissions. Previous studies have varying conclusions regarding the risk of readmissions following DC surgery, with some finding lower readmission rates and some reporting increased risk of specific complications [4-6]. A recent metaanalysis of randomized clinical trials and observational studies found no difference in complication rates between DC procedures and inpatient procedures [3].
In a recent study, DC-TKAs had a slightly higher risk of allcause 90-day readmission compared with inpatient TKA [20] but no difference was found between DC-THAs and inpatient THAs. The study used a readmission definition based on standardized arthroplasty complications measures, while ours was based on all readmissions within 90 days of surgery, potentially explaining differences in results. The study also reported that DC patients were younger and less comorbid, as in our study. The study did, however, compare DC patients with all non-DC patients.
In our study, the median number of days from discharge to readmission ranged between 17 and 25 days depending on the procedure. DC-UKAs were readmitted at median 20 days compared with median 25 days in ON-UKAs. Both DC- and ON-UKAs were, however, readmitted later than THAs and TKAs. This coincides with the results from a previous study, where the median days-to-readmission was 20 days in the DC-group and 23 days in the inpatient group [21]. As such, days-to-readmission does not indicate earlier readmission due to complications that could have been prevented during one overnight admission.
Strengths and limitations
As this is a retrospective study, one important limitation is that the DC patients likely represent a selected group compared with the ON patients, as the less comorbid and less frail patients may have been selected for day-case surgery. The eligibility criteria for discharge on the day of surgery and on postoperative day 1 may also differ between centers, and centers use DC surgery to varying degrees. Data on how long patients were preoperatively scheduled to be admitted is, however, not available. Another limitation is that we do not have access to the electronic patient charts to investigate the direct connection between a readmission and the surgery.
One strength of this study is the comparison of DC patients with ON patients, instead of a diverse patient group not discharged on the day of surgery, making the groups more comparable, as patients with a LOS > 1 day are not likely to have been eligible for day-case surgery. Second, this study is a large retrospective study on prospective routinely collected nationwide data with high completeness. We also presented data on both readmissions (all readmission within 90 days) and complications (readmissions with specific diagnosis codes related to surgery [12,13]), giving both a liberal and conservative estimate of the readmission rate.
Conclusion
We found no differences in 30- and 90-day readmission rates when comparing DC with ON stay in THA, TKA, and UKA. Also, no difference in the number of days from discharge to readmission was present between DC and ON patients.
- Memtsoudis S G, Fiasconaro M, Soffin E M, Liu J, Wilson L A, Poeran J, et al. Enhanced recovery after surgery components and perioperative outcomes: a nationwide observational study. Br J Anaesth 2020; 124(5): 638-47. doi: 10.1016/J.BJA.2020.01.017.
- Soffin E M, Yadeau J T. Enhanced recovery after surgery for primary hip and knee arthroplasty: a review of the evidence. Br J Anaesth 2016; 117 iii62-iii72. doi: 10.1093/BJA/AEW362.
- Bemelmans Y F L, Keulen M H F, Heymans M, van Haaren E H, Boonen B, Schotanus M G M. Safety and efficacy of outpatient hip and knee arthroplasty: a systematic review with meta-analysis. Arch Orthop Trauma Surg 2021; doi: 10.1007/S00402-021-03811-5.
- Dey S, Gadde R, Sobti A, Macdonald N, Jacob J, Unnithan A. The safety and efficacy of day-case total joint arthroplasty. Ann R Coll Surg Engl 2021; 103(9): 638-44. doi: 10.1308/RCSANN.2021.0066.
- Arshi A, Leong N L, D’Oro A, Wang C, Buser Z, Wang J C, et al. Outpatient total knee arthroplasty is associated with higher risk of perioperative complications. J Bone Joint Surg Am 2017; 99(23): 1978-86. doi: 10.2106/JBJS.16.01332.
- Otero J E, Gholson J J, Pugely A J, Gao Y, Bedard N A, Callaghan J J. Length of hospitalization after joint arthroplasty: does early discharge affect complications and readmission rates? J Arthroplasty 2016; 31(12): 2714-25. doi: 10.1016/j.arth.2016.07.026.
- Jensen C B, Troelsen A, Foss N B, Nielsen C S, Lindberg-Larsen M, Gromov K. 10-year evolution of day-case hip and knee arthroplasty: a Danish nationwide register study of 166,833 procedures from 2010 to 2020. Acta Orthop 2023; 94: 178-84. doi: 10.2340/17453674.2023.11961.
- Gromov K, Kjaersgaard-Andersen P, Revald P, Kehlet H, Husted H. Feasibility of outpatient total hip and knee arthroplasty in unselected patients. Acta Orthop 2017; 88(5): 516-21. doi: 10.1080/17453674.2017.1314158.
- Schmidt M, Schmidt S A, Sandegaard J L, Ehrenstein V, Pedersen L, Sorensen H T. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 2015; 7 449-90. doi: 10.2147/clep.S91125.
- Charlson M E, Pompei P, Ales K L, MacKenzie C R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40(5): 373-83. doi: 10.1016/0021-9681(87)90171-8.
- Raedkjaer M, Maretty-Kongstad K, Baad-Hansen T, Jørgensen P H, Safwat A, Vedsted P, et al. The impact of comorbidity on mortality in Danish sarcoma patients from 2000–2013: a nationwide population-based multicentre study. PLoS One 2018; 13(6): e0198933. doi: 10.1371/JOURNAL.PONE.0198933.
- Ohnuma T, Raghunathan K, Fuller M, Ellis A R, JohnBull E A, Bartz R R, et al. Trends in comorbidities and complications using ICD-9 and ICD-10 in total hip and knee arthroplasties. J Bone Joint Surg Am 2021; 103(8): 696-704. doi: 10.2106/JBJS.20.01152.
- Storesund A, Haugen A S, Hjortås M, Nortvedt M W, Flaatten H, Eide G E, et al. Accuracy of surgical complication rate estimation using ICD-10 codes. Br J Surg 2019; 106(3): 236-44. doi: 10.1002/BJS.10985.
- Gubbels S, Nielsen K S, Sandegaard J, Mølbak K, Nielsen J. The development and use of a new methodology to reconstruct courses of admission and ambulatory care based on the Danish National Patient Registry. Int J Med Inform 2016; 95: 49-59. doi: 10.1016/J.IJMEDINF.2016.08.003.
- The Danish Health Data Authority. Afrapportering fra teknikergruppe om opgørelse af indlæggelsesforløb baseret på Landspatientregisteret. https://www.ft.dk/samling/20191/almdel/suu/spm/13/svar/1597313/2088474.pdf.
- Clopper C J, Pearson E S. The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika 1934; 26(4): 404-13. doi: 10.2307/2331986.
- Hernán M A, Hernández-Diaz S, Werler M M, Mitchell A A. Causal knowledge as a prerequisite for confounding evaluation: an application to birth defects epidemiology. Am J Epidemiol 2002; 155(2): 176-84. doi: 10.1093/AJE/155.2.176.
- Wynants L, Bouwmeester W, Moons K G, Moerbeek M, Timmerman D, Van Huffel S, et al. A simulation study of sample size demonstrated the importance of the number of events per variable to develop prediction models in clustered data. J Clin Epidemiol 2015; 68(12): 1406-14. doi: 10.1016/j.jclinepi.2015.02.002.
- Thompson J W, Wignadasan W, Ibrahim M, Plastow R, Beasley L, Haddad F S. The introduction of day-case total knee arthroplasty in a national healthcare system: a review of the literature and development of a hospital pathway. Surgeon 2022; 20(2): 103-14. doi: 10.1016/j.surge.2021.01.017.
- Debbi E M, Mosich G M, Bendich I, Kapadia M, Ast M P, Westrich G H. Same-day discharge total hip and knee arthroplasty: trends, complications, and readmission rates. J Arthroplasty 2022; 37(3): 444-8.e1. doi: 10.1016/J.ARTH.2021.11.023.
- Reddy N C, Prentice H A, Paxton E W, Hinman A D, Navarro R A. Frequency and timing of complications and catastrophic events after same-day discharge compared with inpatient total hip arthroplasty. J Arthroplasty 2021; 36(7): S264-S271. doi: 10.1016/j.arth.2021.01.079.
Appendix