Outcome of patients with osteoarthritis aged 90 to 101 years after cemented total hip arthroplasty: 1,385 patients from the Swedish Arthroplasty Register
Mattias SCHAUFELBERGER 1,2, Ola ROLFSON 2–4, and Johan KÄRRHOLM 2–4
1 Department of Surgery and Orthopaedics, Kungälvs Hospital, Kungälv; 2 Department of Orthopaedics, Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Gothenburg; 3 Sahlgrenska University Hospital, Gothenburg; 4 Swedish Arthroplasty Register, Gothenburg, Centre of Registers Västra Götaland, Gothenburg, Sweden
Background and purpose — Few studies have focused on nonagenarians treated with total hip arthroplasty (THA). We investigated 30- and 90-day postoperative mortality, patient-reported outcome measures (PROMs), reoperation rate, risk factors for reoperation, and relative patient survival in nonagenarians or older.
Patients and methods — 167,091 patients with primary cemented THA performed for osteoarthritis between 1992 and 2019 were identified in the Swedish Arthroplasty Register. Patients were divided into age groups based on age at time of surgery: 60–74 (n = 90,285), 75–89 (n = 75,421), and > 90 years (n = 1,385). Mortality rate, PROMs (pain–Likert scale, satisfaction–Likert scale, EQ-VAS, n = 67,553), reoperation rate, risk factors for reoperation, and relative patient survival were studied.
Results — The nonagenarians had the highest postoperative mortality rate, 1.7% and 2.6% at 30 and 90 days, respectively. Nonagenarian females reported significantly lower pre- and postoperative EQ-VAS compared with patients aged 60–89 years but reported least pain and highest patient satisfaction 1 year after surgery. At 2 years the nonagenarians had highest reoperation frequency—2.7%—due to infection (1.5%), dislocation (0.8%), and periprosthetic fracture (0.4%). Increasing age, male sex, and polished stem were associated with higher risk of reoperation within 2 years. 8-year age- and sex-matched relative survival was highest among nonagenarians (study group/matched population: ≥ 90 years 3.4, 95% confidence interval [CI] 3.0–3.8; 75–89 years: 1.4, CI 1.4–1.4, and 60–74 years: 1.1, CI 1.1–1.1).
Conclusion — 30- and 90-day postoperative mortality and reoperation rates were higher in nonagenarians but PROM data showed least pain and highest patient satisfaction 1 year after surgery with THA among female nonagenarians with primary osteoarthritis.
Citation: Acta Orthopaedica 2023; 94: 477–483. DOI https://doi.org/10.2340/17453674.2023.18656.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-11-07. Accepted: 2023-08-23. Published: 2023-09-22.
Correspondence: mattias.schaufelberger@vgregion.se
MS, JK, and OR conceived and planned the study. Statistical analyses were performed by JK except for calculations of relative survival, which were performed by Emma Nauclér, professional statistician. The results were discussed within the author group. All authors contributed to writing the manuscript, which was drafted by MS.
Handling co-editors: Keijo Mäkelä and Philippe Wagner
Acta thanks Martin Clauss, Esa Jämsen, and Lene Bergendal Solberg for help with peer review of this manuscript.
Nonagenarians and centenarians are growing age groups globally [1]. Together, these age groups increased in Sweden by 117% from 1992 to 2019 compared with 19% for the population in general. This increase is expected to continue resulting in a more than doubling of this age group before 2050 [2]. As the population is getting older, the demand for primary total hip arthroplasty (THA) and revision hip arthroplasty (RHA) is expected to rise. Previous studies have reported higher mortality and complication rate among nonagenarians and centenarians compared with younger cohorts [3-6] whereas others [7] claim that comorbidities rather than age should be considered as part of the decision-making.
There is lack of solid data on nonagenarians receiving an all-cemented primary THA due to osteoarthritis, including patient-reported outcomes (PROMs) and relative patient survival. Our aim was to investigate 30- and 90-day postoperative mortality, PROMs, reoperation rate, risk factors for reoperation in nonagenarians, and centenarians receiving a THA compared with patients 60–74 and 75–89 years of age. We also evaluated the relative patient survival in the 3 age groups compared with age- and sex-matched individuals in the general population.
Patients and methods
Study population
Only patients receiving an all-cemented THA were included. In patients who had surgery on both sides, only the second hip was included [8]. In patients operated on bilaterally the same day only 1 hip was selected. We excluded all surgeries performed for reasons other than primary osteoarthritis and patients younger than 60 years (Figure 1). This study was performed in accordance with the STROBE guidelines [9].
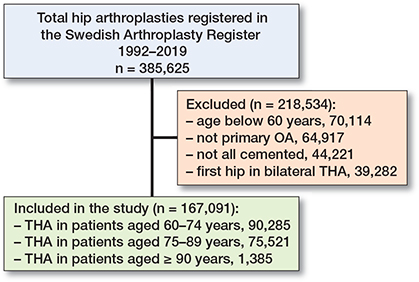
Figure 1. Patient flowchart. THA = total hip arthroplasty. OA = osteoarthritis.
Data sources
Since 1992 the Swedish Arthroplasty Register (SAR) has registered patient-specific data on primary THA. This national joint register covers all hospitals performing THA in Sweden and has a completeness of 98% for primary THA and 90–95% for revisions [10].
Outcome measures
Age at surgery, sex, date of death, 30- and 90-day mortality, PROMs, presence of any reoperation, and reasons for reoperation were extracted or computed based on data from the SAR. Reoperation was defined as any surgical procedure related to the operated hip regardless of whether any part of the implant was exchanged, extracted, or not. Included patients were followed until either reoperation, death, or December 31, 2019. In the statistical analyses patients in all 3 age groups were censored at the last day of observation. Historical number of inhabitants and population estimations were obtained from Statistics Sweden. The PROMs used were the EuroQol-visual analogue scale (EQ-VAS) and pain reported on a Likert scale before and 1 year after the operation. Patient satisfaction, i.e., satisfaction with the outcome of surgery, was reported 1 year after the operation on a Likert scale. The EQ-VAS records patients’ self-rated health on a vertical visual analogue scale where 100 represents “the best health you can imagine” and 0 “the worst health you can imagine.” PROM answers were separated into 2 groups depending on sex. For PROMs analyses, only patients responding to pre-, and 1-year postoperative questionnaires were included. SAR introduced PROM values in 2002, which were to become implemented nationwide in 2011 [11]. Due to the late introduction of PROM values, complete data before and 1 year after the operation were available in 42%, 39%, and 38% of the patients in the 3 age groups (60–74, 75–89, and ≥ 90 years of age).
Statistics
The risk of reoperation for the age groups 75–89 years and ≥ 90 years with use of the youngest age group as reference was analyzed using Cox regression analysis with adjustment for sex, matt or polished stem, and year of operation (1992–2005, 2006–2013, 2014–2019). Adjustment for stem surface finish was performed due to the increased risk of periprosthetic fracture with polished stems and especially in the older patients. Evaluation based on survival curves, log minus log plots, and Schoenfeld residuals confirmed proportionality up to 2 years. Thereafter, there were few observations in the oldest age group. We therefore abstained from further analyses based on time intervals after 2 years.
Life tables were computed to study the probability of reoperation due to any reason. Hazard ratios (HR) are presented with 95% confidence intervals (CI). All design parameters were classified using the group with highest number of observations as reference (age group 60–74 years). The cumulative relative patient survival was computed as the quotient between the observed survival in the study group and the expected survival in the population with the same sex and age. Information regarding expected survival in the Swedish population was extracted from publicly available mortality tables separated for sex and age [2,12,13].
Comparison of PROM data was performed with use of oneway ANOVA with Bonferroni correction. The minimum clinical important improvement (MCII) was defined as improvement of at least 1 step on the 5-grade Likert scale for pain [14], and at least 7 units of improvement on EQ-VAS between the preoperative and the 1-year evaluations [15]. Comparison between nonagenarians and the 2 other age groups was performed using Fisher’s exact test. Mean differences in PROM values refer to 1 of the 2 younger groups minus data for the nonagenarians.
Statistical evaluation was performed using SPSS version 25 (IBM Corp, Armonk, NY, USA) except from calculation of relative survival and diagram design which was performed using R statistics version 3.5.1 (R Core Team 2022; R Foundastion for Statistical Computing, Vienna, Austria).
Ethics, data sharing, funding, and disclosures
This study was approved by the Regional Ethical Review Board in Gothenburg (Dnr 271-14). Funding was received from the Swedish State under the agreement between the Swedish government and the county councils, the ALF-agreement (ALFGBG 721791 and ALFGBG 965217). Parts of the used data are publicly available information such as population by year, estimated population growth, and annual number of THAs performed in Sweden. Patient registration in SAR is regulated by Swedish law (SFS 2008:355). Before entering the register, hospitals inform all patients about SAR. There is no requirement for any signed patient consent and withdrawal is accepted whenever requested. The authors report no conflicts of interest. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.18656
Results
385,625 patients aged 40 years or older who had undergone primary THA in Sweden between January 1, 1992, and December 31, 2019, were identified in the SAR. 167,091 operations (patients) were identified and divided into 3 age groups based on age at time of surgery: 60–74 (n = 90,285), 75–89 (n = 75,421), and 90 years or older (n = 1,385) (Figure 1).
Demographics
The mean follow-up time was 8.1 years (SD 5.6). 1,385 of the 167,091 patients included were between 90 and 101 years old. There was an surplus of women with 73% in the nonagenarian group (Table 1). During the study period, there was an increase in operation frequency in all age categories. The greatest increase was seen in the nonagenarian group with an increasing frequency from 16 operations per year in 1992–1994 to 88 operations per year in 2017–2019 (Figure 2).
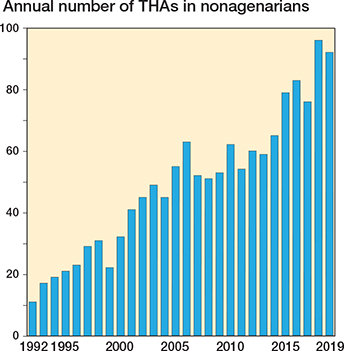
Figure 2. Number of nonagenarians operated on with a cemented THA due to primary osteoarthritis 1992–2019.
Mortality
The overall 30- and 90-day mortality was 0.29% and 0.51%, respectively. The lowest mortality rate was seen in the youngest study group (60–74 years) with 0.15% and 0.28% 30- and 90-day mortality. The nonagenarian group had the highest mortality rate, 1.7% and 2.6% 30- and 90-day mortality (Table 1). At 5 years their cumulative mortality reached 52% (SD 3.1) (Figure 3).
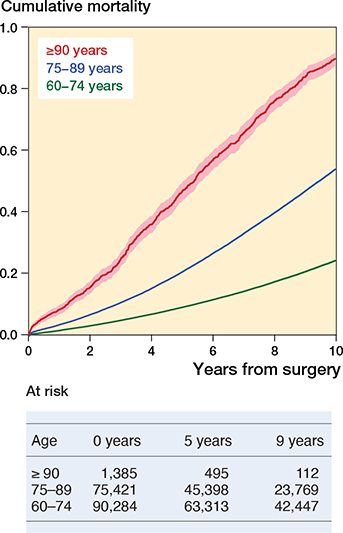
Figure 3. Cumulative overall observed mortality with 95% confidence limits. Number of available observations at each time point in the table.
Patient-reported outcomes
67,553 patients (366 females and 155 males aged 90 years or older) had complete reports of hip pain, satisfaction, and EQ-VAS both before and 1 year after the operation (Tables 2 and 3). More patients in the youngest age group (44% of the females, 45% of the males) reported PROMs than did patients in the 2 older age groups (75–89 years: 40% and 41%; ≥ 90 years: 34% and 31%, respectively). The highest mean satisfaction among females was seen in the nonagenarian group, whereas among males the ≥ 90 group did not significantly differ from the 2 younger groups (Tables 2 and 3).
| FEMALES | 60–74 years n = 22,264 | 75–89 years n = 18,807 | 90 –98 years n = 366 |
| Pain, preoperatively | |||
| 1 none | 200 (0.9) | 199 (1.1) | 6 (1.6) |
| 2 very mild | 256 (1.1) | 182 (1.0) | 4 (1.1) |
| 3 mild | 773 (3.5) | 751 (4.0) | 5 (1.4) |
| 4 moderate | 8,154 (37) | 6,506 (35) | 84 (23) |
| 5 severe | 12,881 (58) | 11,169 (54) | 267 (73) |
| Mean score (CI) | 4.5 (4.5–4.5) | 4.5 (4.5–4.5) | 4.6 (4.6-4.7) |
| Mean difference (CI) a | –0.15 (–0.24 to –0.06) – | 0.1 (–0.5 to 0.2) | – |
| Pain, 1 year | |||
| 1 none | 10,696 (48) | 8,172 (44) | 200 (55) |
| 2 very mild | 5,442 (24) | 4,861 (26) | 73 (20) |
| 3 mild | 3,271 (15) | 3,111 (17) | 58 (16) |
| 4 moderate | 2,311 (10) | 2,149 (11) | 28 (7.7) |
| 5 severe | 544 (2.4) | 200 (2.7) | 7 (1.9) |
| Mean score (CI) | 2.0 (1.9–2.0) | 2.0 (2.0–2.0) | 1.8 (1.7-1.9) |
| Mean difference (CI) a | 0.1 (0.02 to 0.3) | 0.2 (0.1–0.4) | – |
| Satisfaction, 1 year | |||
| 1 very dissatisfied | 946 (4.2) | 857 (4.6) | 9 (2.5) |
| 2 dissatisfied | 1,436 (6.4) | 1,414 (7.5)12 (3.3) | |
| 3 neither nor | 2,781 (13) | 2,781 (17) | 41 (11) |
| 4 satisfied | 5,828 (26) | 5,549 (30) | 109 (30) |
| 5 very satisfied | 11,273 (51) | 7,892 (42) | 195 (53) |
| Mean score (CI) | 4.1 (4.1–4.1) | 4.0 (4.0–4.0) | 4.3 (4.2–4.4) |
| Mean difference (CI) a | –0.2 (–0.3 to –0.01) | –0.3 (–0.5 to –0.2) | – |
| EQ VAS, preoperatively | |||
| Mean score (CI) | 54.6 (54.3-54.9) | 54.5 (54.2–54.8) | 51.2 (49.0–53.5) |
| Mean difference (CI) a | 3.4 (0.6 to 6.2) | 3.3 (0.5 to 6.1) | – |
| EQ VAS, 1 year | |||
| Mean score (CI) | 77.0 (76.7–77.2) | 71.9 (71.6–72.1) | 67.2 (65.0–69.3) |
| Mean difference (CI) a | 9.8 (7.3 to 12) | 4.7 (2.1 to 7.3) | – |
| a Mean difference (CI) between indicated group and the oldest group. | |||
| MALES | 60–74 years n = 15,399 | 75–89 years n = 10,562 | 90–98 years n = 155 |
| Pain, preoperatively | |||
| 1 none | 212 (1.4) | 154 (1.5) | 4 (2.6) |
| 2 very mild | 258 (1.7) | 198 (1.9) | 1 (0.6) |
| 3 mild | 935 (6.1) | 786 (7.4) | 6 (3.9) |
| 4 moderate | 6,771 (44) | 4,596 (44) | 49 (32) |
| 5 severe | 7,223 (47) | 4,828 (46) | 95 (61) |
| Mean score (CI) | 4.3 (4.3–4.3) | 4.3 (4.3–4.3) | 4.5 (4.4–4.6) |
| Mean difference (CI) a | –0.15 (–0.3 to 0.0) | –0.2 (–0.3 to –0.03) | – |
| Pain, 1 year | |||
| 1 none | 8,027 (52) | 4,926 (47) | 80 (52) |
| 2 very mild | 3,755 (24) | 2,758 (26) | 41 (27) |
| 3 mild | 2,069 (13) | 1,628 (15) | 12 (7.7) |
| 4 moderate | 1,250 (8.1) | 996 (9.4) | 20 (13) |
| 5 severe | 298 (1.9) | 254 (2.4) | 2 (1.3) |
| Mean score (CI) | 1.8 (1.8–1.9) | 2.0 (1.9–2.0) | 1.9 (1.7–2.0) |
| Mean difference (CI) a | –0.03 (–0.2 to 0.2) | 0.1 (–0.1 to 0.3) | – |
| Satisfaction, 1 year | |||
| 1 very dissatisfied | 498 (3.2) | 425 (4.0) | 2 (1.3) |
| 2 dissatisfied | 728 (4.7) | 650 (6.2) | 10 (6.5) |
| 3 neither nor | 1,671 (11) | 1,503 (14) | 23 (15) |
| 4 satisfied | 4,013 (26) | 3,050 (29) | 35 (23) |
| 5 very satisfied | 8,489 (55) | 4,934 (47) | 85 (54) |
| Mean score (CI) | 4.3 (4.2–4.3) | 4.1 (4.1–4.1) | 4.2 (4.1–4.4) |
| Mean difference (CI) a | 0.02 (–0.10 to 0.22) | –0.2 (–0.4 to 0.1) | – |
| EQ VAS, preoperatively | |||
| Mean score (CI) | 60.1 (59.7–60.4) | 59.7 (59.2–60.1) | 56.5 (52.9-60.0) |
| Mean difference (CI) a | 3.6 (–0.5 to 7.7) | 3.2 (–0.9 to 7.3) | – |
| EQ VAS, 1 year | |||
| Mean score (CI) | 79.1 (78.8–79.4) | 74.8 (74.4–75.1) | 72.8 (69.3–76.3) |
| Mean difference (CI) a | 6.3 (2.7 to 10) | 1.9 (–1.7 to 5.6) | – |
| a Mean difference (CI) between indicated group and the oldest group. | |||
Females showed more pain reduction at 1 year among nonagenarians than in the youngest group (mean difference –0.3, CI –0.4 to –0.1) and the group aged 75–89 (–0.4, CI –0.5 to –0.2). In males a corresponding difference was only found when compared with the group aged 75–89 years (–0.3, CI –0.5 to –0.03; nonagenarians vs. age 60–74: –0.1, CI –0.4 to 0.1)
The EQ-VAS improvement in females at 1 year was lower in the youngest group compared with nonagenarians (mean difference: –6.4, CI –9.7 to –3.2), whereas comparison with the age group 75–89 showed no difference (–1.4, CI –4.7 to 1.9). In males the improvement values in the 2 younger groups did not differ from those observed in the oldest group (mean difference 60–74 years: –2.7, CI –7.4 to 2.0; 75–89 years: 1.2, CI –3.4 to 5.9).
Separation of the patients into those who reported at least 1 step of improvement on the Likert scale for pain (MCII) and those who did not revealed that a higher proportion of females aged ≥ 90 years (94%) reported an improvement compared with patients aged 75–89 years (91%, P = 0.04) but not when compared with the youngest group (92%, P = 0.1). The corresponding comparisons among males revealed no differences.
The share of females or males aged ≥ 90 who reported improved EQ-VAS of 7 or more (MCII) did not differ when compared with the corresponding groups 75–89 years of age. More females aged 60–74 years did, however, report an improvement of at least 7 when compared with the nonagenarians (72% vs. 64%, P < 0.001). In males the corresponding comparison did not reach statistical significance.
Reoperation and risk factors
At 2 years the nonagenarians had the highest reoperation rate, 2.7% compared with 1.8% in the youngest group (adjusted hazard ratio 1.8, CI 1.3–2.4) (Tables 1 and 4). Deep infection was the most common reason for reoperation in all groups with an overall rate of 0.8%, which increased with age and reached 1.5% in the nonagenarian group. Periprosthetic fractures occurred in 0.1% with the highest percentage of reoperation in the nonagenarian group (0.4%). The highest rate of reoperation because of dislocation (0.8%) was observed in the age groups 75–89 and ≥ 90. Past 2 years’ follow-up, 16 reoperations occurred in the group of nonagenarians, of which 13 were due to periprosthetic fracture (Figure 4).
| Unadjusted HR (CI) | Adjusted a HR (CI) | |
| Sex (reference: male) | ||
| Female | 0.7 (0.6–0.7) | 0.7 (0.6–0.7) |
| Age group (reference: 60–74) | ||
| 75–89 | 1.2 (1.1–1.3) | 1.2 (1.2–1.3) |
| ≥ 90 | 1.6 (1.2–2.2) | 1.8 (1.3–2.4) |
| Stem type (reference: polished) | ||
| Matte | 0.9 (0.8–1.0) | 0.9 (0.8–0.9) |
| Year of operation (reference: 2014–2019) | ||
| 2006–2013 | 1.0 (0.9–1.1) | 1.0 (0.9–1.1) |
| 1992–2005 | 1.2 (1.1–1.3) | 1.2 (1.1–1.3) |
| a Adjusted for sex, age, stem type, and year of operation. | ||
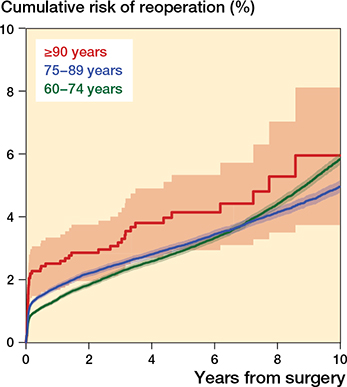
Figure 4. Cumulative overall observed reoperation rate with 95% confidence limits. For number of available observations at each time point see Figure 3.
Relative patient survival
In all 3 patient groups there was an increased expected survival when compared with Swedish inhabitants of the same age and sex. This increase was most pronounced among nonagenarians, with an increase 8 years after the operation of 3.4, CI 3.0–3.8; 75–89 years: 1.4, CI 1.4–1.4, and 60–74 years: 1.1, CI 1.1–1.1 (Figure 5).
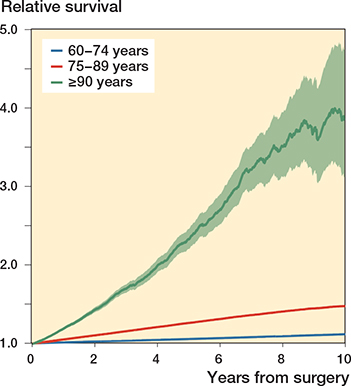
Figure 5. Age- and sex-matched relative patient survival compared with the background population, with 95% confidence limits.
Discussion
We aimed to investigate mortality rates, PROMs, reoperation rates, and risk factors for reoperation in nonagenarians receiving all-cemented primary THA due to osteoarthritis in Sweden between the years 1992 and 2019. We showed that nonagenarians had significantly higher 30- and 90-day mortality rate and 2-year reoperation rate than patients 60–89 years of age. Our 30-day mortality rate (1.7%) was higher compared with previous studies whereas the 90-day mortality rate (2.6%) was in line with previously published data [7,16-18].
Nonagenarian females reported least pain and highest patient satisfaction 1 year after surgery. Deep infection was the most common reason for reoperation. The 8-year relative survival was considerably higher among nonagenarians.
As expected, the nonagenarians had the highest mean preoperative pain, which strengthens the indication for surgical treatment despite high age. Previous studies [19-21] have reported decreased pain after surgery among nonagenarians, but not separately for females and males. PROMs differ between sex and age [11,22] and with increasing age the relative share of females will increase because of their longer life expectancy. Therefore, any comparison between age groups of these parameters should preferably be performed for males and females separately. In our study nonagenarian females were the most satisfied 1 year after surgery whereas there was no significant difference in males. Our results should, however, be viewed cautiously because the number of patients with complete PROM data were few among the nonagenarians and especially in the male group. EQ-VAS improved in all age groups after surgery but contrary to Skinner et al. [3], who used the EQ-5D instead of EQ-VAS, the biggest improvement was seen among the youngest patients. The 1-year 92% nonagenarian satisfaction rate reported by Skinner et al. is, however, well in line with our results. Nonagenarian females reported significantly lower EQ-VAS pre- and postoperatively compared with patients 60–89 years of age. The same patient group, at the same time, reported least pain and highest patient satisfaction 1 year after surgery. This may be explained by lower performance requirements parallel with more prevalent comorbidities among nonagenarians.
Our study shows that nonagenarians had a higher 2-year reoperation rate than patients 60–89 years of age, 2.7% compared with 1.8%. This finding is in line with previous studies [17,21]. A 1.5% reoperation rate due to deep infection is in accordance with other studies [20,21]. Dagneaux et al. [20] reported 7% reoperations because of postoperative fracture, beyond 4% intraoperative fractures, which is far higher than the 0.4% in our study. Use of uncemented femoral stems in about one-third of the patients and a doubled follow-up time (mean 4 years) may have contributed to the higher numbers of fractures described by Dagneaux et al. In contrast, Dimitriou et al. [21] described no revisions at all due to periprosthetic fracture with 100% uncemented components and the same follow-up time as in the study by Dagneaux et al. However, there were fewer females and a lower mean age in the study by Dimitriou et al.
In accordance with 2 previous studies [17,23], but in contrast to Dimitriou et al. [21], we found that male sex was associated with increased risk of reoperation. It has previously been shown that polished femoral stems are associated with higher revision or reoperation rate due to periprosthetic fracture [24,25], which justifies correction for this factor in our regression model (Table 4).
The increase in age- and sex-matched patient relative survival was far higher among nonagenarians (3.4) compared with 60–89-year-old patients. Berend et al. [19] showed an at least equal survival curve comparing operated nonagenarians with an age-matched population. Dagneaux et al. [20] reported a 5.3-year median observed survival after THA surgery in nonagenarians compared with an expected 3.5 years when matching for age and sex. Together this reflects that those nonagenarians receiving THA live longer probably due to patient selection. However, the operation itself might also have contributed to improved patient survival through improved mobility and quality of life.
Strengths and limitations
Our study has high completeness, a large dataset, and the use of reoperation and not revision, as more complications resulting in surgical intervention are caught.
A limitation of our study is that reoperation rates might be falsely low due to underreporting of surgical procedures directed to the hip including plating of periprosthetic fractures and irrigation and synovectomies without exchange or removal of the implant or any of its parts. Further, an increasing number of comorbidities and increasing fragility with age might imply that the threshold to proceed with surgical treatment of complications becomes higher [17]. Thus, despite full coverage and high completeness in SAR, the true need for reoperation and the number of procedures actually performed is probably slightly underestimated. As the study period precedes the introduction of the PROMs program in the SAR, the number of patients with PROMs data was comparatively small and limited to the later part of the study period. Further, the response rate decreased with increasing age—probably partly an effect of increasing mortality and risk of frailty during the postoperative year with increasing age. Also there may be a potential non-respondent bias because satisfied patients more often give feedback than those not satisfied. Further, there were changes in operation indications, improvements in surgery techniques, and changed threshold for surgery during the 27-year inclusion period. Thus, a more liberal approach over time to offer elderly and more frail patients a THA could to a certain extent have skewed our findings. Adjustment for ASA class could to a certain extent reduce this bias, but was not possible as collection of this information was initiated first in 2008 and only became reasonably complete the year after. Finally, type of incision was not recorded by SAR until the year 2000 and could therefore not be adjusted for in the regression analysis.
Conclusions
We found higher mortality among nonagenarians when compared with a younger population. Early reoperations were more common whereas patient satisfaction and pain relief among nonagenarians were as good as or better than in the younger cohorts.
In this perspective, we still think that nonagenarians should not be denied treatment with THA due to primary osteoarthritis if cemented fixation, as here studied, is used. Because of increased fragility compared with the younger patient population we think that preoperative optimization, thorough patient information, and referral to experienced surgeons are key factors for the optimum outcome in this group of patients.
- United Nations. https://population.un.org/wpp/.
- Statistikmyndigheten SCB. https://www.statistikdatabasen.scb.se
- Skinner D, Tadros B J, Bray E, Elsherbiny M, Stafford G. Clinical outcome following primary total hip or knee replacement in nonagenarians. Ann R Coll Surg Engl 2016; 98: 258-64. doi: 10.1308/rcsann.2016.0095.
- Yohe N, Weisberg M D, Ciminero M, Mannino A, Erez O, Saleh A. Complications and readmissions after total hip replacement in octogenarians and nonagenarians. Geriatr Orthop Surg Rehabil 2020; 11: 2151459320940959. doi: 10.1177/2151459320940959.
- Jauregui J J, Boylan M R, Kapadia B H, Naziri Q, Maheshwari A V, Mont M A. Total joint arthroplasty in nonagenarians: what are the risks? J Arthroplasty 2015; 30: 2102-5 e2101. doi: 10.1016/j.arth.2015.06.028.
- Nanjayan S K, Swamy G N, Yellu S, Yallappa S, Abuzakuk T, Straw R. In-hospital complications following primary total hip and knee arthroplasty in octogenarian and nonagenarian patients. J Orthop Traumatol 2014; 15: 29-33. doi: 10.1007/s10195-013-0262-y.
- Sherman A E, Plantz M A, Hardt K D. Outcomes of elective total hip arthroplasty in nonagenarians and centenarians. J Arthroplasty 2020; 35: 2149-2154. doi: 10.1016/j.arth.2020.03.026.
- Bülow E, Nemes S, Rolfson O. Are the first or the second hips of staged bilateral THAs more similar to unilateral procedures? A study from the Swedish Hip Arthroplasty Register. Clin Orthop Relat Res 2020; 478: 1262-70. doi: 10.1097/CORR.0000000000001210.
- Vandenbroucke J P, von Elm E, Altman D G, Gøtzsche P C, Mulrow C D, Pocock S J, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Int J Surg 2014; 12: 1500-24. doi: 10.1016/j.ijsu.2014.07.014..
- Swedish Arthroplasty Register. https://registercentrum.blob.core.windows.net/slr/r/2019-B1xpWMUSPO.pdf.
- Rolfson O, Kärrholm J, Dahlberg L E, Garellick G. Patient-reported outcomes in the Swedish Hip Arthroplasty Register: results of a nationwide prospective observational study. J Bone Joint Surg Br 2011; 93: 867-75. doi: 10.1302/0301-620X.93B7.25737.
- Nemes S, Lind D, Cnudde P, Bülow E, Rolfson O, Rogmark C. Relative survival following hemi- and total hip arthroplasty for hip fractures in Sweden. BMC Musculoskelet Disord 2018; 19: 407. doi: 10.1186/s12891-018-2321-2.
- Cnudde P, Bülow E, Nemes S, Tyson Y, Mohaddes M, Rolfson O. Association between patient survival following reoperation after total hip replacement and the reason for reoperation: an analysis of 9,926 patients in the Swedish Hip Arthroplasty Register. Acta Orthop 2019; 90: 226-30. doi: 10.1080/17453674.2019.1597062.
- Danoff J R, Goel R, Sutton R, Maltenfort M G, Austin M S. How much pain is significant? Defining the minimal clinically important difference for the visual analog scale for pain after total joint arthroplasty. J Arthroplasty 2018; 33: S71-S75 e72. doi: 10.1016/j.arth.2018.02.029.
- Paulsen A, Roos E M, Pedersen A B, Overgaard S. Minimal clinically important improvement (MCII) and patient-acceptable symptom state (PASS) in total hip arthroplasty (THA) patients 1 year postoperatively. Acta Orthop 2014; 85: 39-48. doi: 10.3109/17453674.2013.867782.
- Miric A, Inacio M C, Kelly M P, Namba R S. Are nonagenarians too old for total hip arthroplasty? An evaluation of morbidity and mortality within a total joint replacement registry. J Arthroplasty 2015; 30: 1324-7. doi: 10.1016/j.arth.2015.03.008.
- Bloemheuvel E M, Van Steenbergen L N, Swierstra B A. Comparable mortality but higher revision rate after uncemented compared with cemented total hip arthroplasties in patients 80 years and older: report of 43,053 cases of the Dutch Arthroplasty Register. Acta Orthop 2022; 93: 151-7. doi: 10.2340/17453674.2021.886.
- AOANJRRAR https://aoanjrr.sahmri.com/annual-reports-2018%20AOANJRRAR.
- Berend M E, Thong A E, Faris G W, Newbern G, Pierson J L, Ritter M A. Total joint arthroplasty in the extremely elderly: hip and knee arthroplasty after entering the 89th year of life. J Arthroplasty 2003; 18: 817-21. doi: 10.1016/s0883-5403(03)00338-3.
- Dagneaux L, Amundson A W, Larson D R, Pagnano M W, Berry D J, Abdel M P. Contemporary mortality rate and outcomes in nonagenarians undergoing primary total hip arthroplasty. J Arthroplasty 2021; 36: 1373-9. doi: 10.1016/j.arth.2020.10.040.
- Dimitriou D, Antoniadis A, Flury A, Liebhauser M, Helmy N. Total hip arthroplasty improves the quality-adjusted life years in patients who exceeded the estimated life expectancy. J Arthroplasty 2018; 33: 3484-9. doi: 10.1016/j.arth.2018.07.005.
- Teni F S, Gerdtham U G, Leidl R, Henriksson M, Astrom M, Sun S, et al. Inequality and heterogeneity in health-related quality of life: findings based on a large sample of cross-sectional EQ-5D-5L data from the Swedish general population. Qual Life Res 2022; 31: 697-712. doi: 10.1007/s11136-021-02982-3.
- Kandala N B, Connock M, Pulikottil-Jacob R, Sutcliffe P, Crowther M J, Grove A, et al. Setting benchmark revision rates for total hip replacement: analysis of registry evidence. BMJ 2015; 350: h756. doi: 10.1136/bmj.h756.
- Thien T M, Chatziagorou G, Garellick G, Furnes O, Havelin L I, Mäkelä K, et al. Periprosthetic femoral fracture within two years after total hip replacement: analysis of 437,629 operations in the Nordic Arthroplasty Register Association database. J Bone Joint Surg Am 2014; 96: e167. doi: 10.2106/JBJS.M.00643.
- Chatziagorou G, Lindahl H, Kärrholm J. The design of the cemented stem influences the risk of Vancouver type B fractures, but not of type C: an analysis of 82,837 Lubinus SPII and Exeter Polished stems. Acta Orthop 2019; 90: 135-42. doi: 10.1080/17453674.2019.1574387.