Plate-assisted bone-segment transport in the femur with 2 internal lengthening nails: a technical note and a case report
Ulrik KÄHLER OLESEN 1, John E HERZENBERG 2, Klaus HINDSØ 1, Upender Martin SINGH 1, and Michael Mørk PETERSEN 1
1 Department of Orthopedic Surgery, Limb Reconstruction, Rigshospitalet, Copenhagen, Denmark; 2 Rubin Institute of Advanced Orthopedics, Baltimore, USA
Citation: Acta Orthopaedica 2023; 94: 466–470. DOI: https://doi.org/10.2340/17453674.2023.18493.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-08-20. Accepted: 2023-08-07. Published: 2023-09-13.
Correspondence: ulrik.kaehler@gmail.com
UKO: developed the technique, sketched the custom-made implants and illustrations, and wrote the article manuscript. KH, UMS, MMP: proofread the manuscript. JH: proofread the manuscript, added calculations and references, supervised and provided medical drawings.
The authors wish to thank machine technician S Shakoor and medical illustrator J Marlowe, MA, CMI for their contributions.
Handling co-editor: Ivan Hvid
Acta thanks Andreas Heinrich Krieg and Martin McNally for help with peer review of this manuscript.
A novel technique to resolve large bone defects, using 2 internal lengthening nails (ILNs), one antegrade and one retro-grade, aligned in a custom-made tube is presented. A 28-year-old, healthy, asymptomatic male presented with a slowly growing mass in the left femur. Physical examination revealed a large, non-tender tumor on the medial side of the mid-femur. Plain radiographs (Figure 1) and MRI were suspicious for a malignant bone tumor. Imaging with F-18 FDG PET/CT confirmed the suspicion, showing a 6 x 6 x 8 cm tumor involving the medial and lateral cortex of the femoral shaft. No metastases were found. An initial biopsy was inconclusive, but when repeated, was positive for an unspecified low-malignant bone sarcoma.
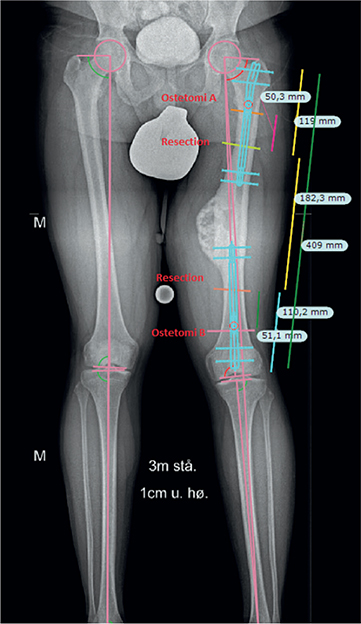
Figure 1. Long-leg standing radiographs, demonstrating mild valgus and anisomelia due to tumor-induced overgrowth.
Based on the staging studies, wide resection of the tumor was performed. Pathology confirmed wide margin removal, and the histological classification of the tumor remained unchanged. The patient was not treated with chemotherapy and remained without any signs of metastases or local recurrence during 1.5 years of follow-up.
Planning and technique
The treatment goal was to maintain normal length and alignment of the femur, avoiding deformities. Using calibrated, long-leg standing radiographs, a 17 cm resection of the diaphyseal tumor and simultaneous metaphyseal (distal) and diaphyseal (proximal) bone transport procedures were undertaken, assisted by a custommade titanium tube that housed the 2 ILNs. Initial stability was augmented by a unilateral 2-pin external fixator. For longer-term construct stability, we planned to implant a spanning locking plate from the greater trochanter to the distal lateral epicondyle. The medial overgrowth of the tumor produced a limb length discrepancy (LLD) of 1 cm longer on the involved side, and a mild valgus. A 3D printed plastic model based on a CT scan was produced to test the various steps of the procedure (Figure 2). The stroke of the 2 ILNs was 5 cm each. Therefore, with the defect size of 17 cm, an additional procedure to “rewind” the mechanisms was planned, midway through the treatment (Figure 3), using the “rapid distractor” tool from the manufacturer (NSO, NuVasive Specialized Orthopedics, Aliso Viejo, CA, USA). Location of screws and cables in the transport segments, as well as both insertion and removal strategies for the hardware, were also planned (Figure 3A–G). It is important to always keep full length control of the regenerate bone segments, as they will act like a spring and shorten, if tension is not maintained during the rewinding procedures (Figure 4).
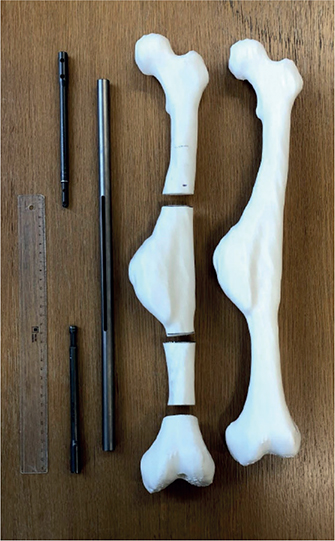
Figure 2. 3-D printed model for testing the setup.
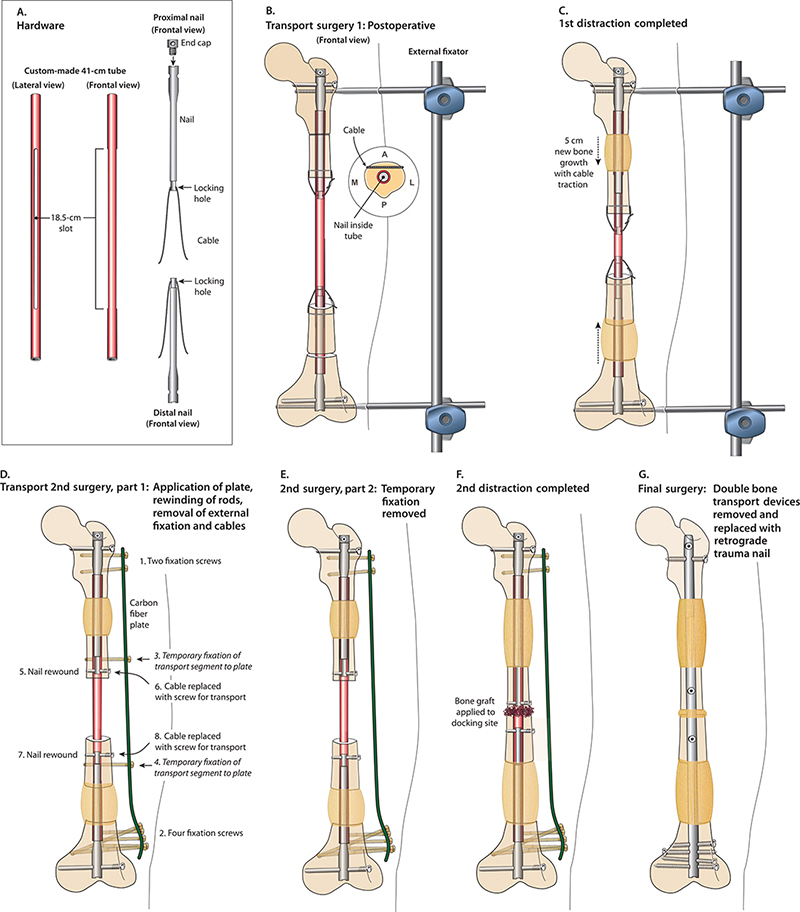
Figure 3. A–G. Step-by-step illustration of the procedure (©2023 Sinai Hospital of Baltimore).

Figure 4. Rewinding procedure (procedure # 3).
The total cost of implants was roughly 2.5 times the price of a single ILN.
Reconstructive surgery # 1: initial implantation with removal of tumor, insertion of double nails, external fixator support (Figure 3A, B)
A temporary external fixator (until biopsies confirmed clear margins), supported the construct, maintaining axis, length, and rotation during and after the first surgery. A custom-made, optional “end cap” cylinder with an additional screw hole was mounted on top of the proximal nail, to enhance stability and fine tune the length of the construct. The canal was prepared by reaming to 12 mm to accommodate the 11 mm diameter of the slotted titanium tube. The “end cap” and tube were custom made at Rigshospitalet, Copenhagen, Denmark. Specifications and CAD drawings are available as “open-source” (see Supplementary data). The 2 ILNs were Precice 2.0 generation (NSO, NuVasive Specialized Orthopedics, Aliso Viejo, CA, USA), 8.5 mm in diameter (except the expanded end, which was 10.7 mm in diameter). Each nail was 15 cm long with a single interlocking hole proximally and distally. The complete setup was inserted through the anterior access used to remove the tumor and with an infrapatellar knee approach. The 2 osteotomies were made (10 cm from the tip of the trochanter and 9 cm from the knee joint). The 2 transport segments were connected to the tips of the 2 ILNs by cables (DePuy Synthes, Raynham, MA, USA).
Reconstructive surgery # 2: staged transport (Figure 3C, D)
As the stroke of the lengthening nails was limited to 5 cm each, totaling 10 cm, and as the defect size was greater than this, a 2-stage approach was chosen. After the cabled attachment to the distal pole of the 2 transport segments achieved the first 5 cm each, we returned to the OR to add a 350-mm distal lateral carbon fiber locking plate (CarboFix Orthopedics Ltd, Herzeliyah, Israel), to rewind the nails to gain more stroke, and to eliminate the “collision” of the 2 male ends of the nails. Removing the cables and rewinding the nails without control of the transport segments may lead to collapse (acute shortening) of the regenerate bone segments. Therefore, we inserted temporary screw fixation from the locking plate into the 2 transport segments (Figure 4). We then removed the cables and acutely shortened (“rewound”) the 2 nails using the “Rapid Distractor” (NSO). Interlocking standard pegs were inserted into the 2 ILNs through the 2 transport segments to continue the bone transport process. The plate was lateralized 2.5 cm to avoid contact with the regenerate.
Reconstructive surgery # 3: docking (Figure 3E, F)
After the 2 transport “napkin rings” of bone touched in the middle of the diaphysis, we secured the docking zone by opening the site and applying graft, composed of autogenous iliac crest bone augmented with bone marrow aspirate concentrate (BMAC), around the docking site. The regenerate bone was also augmented with BMAC.
Reconstructive surgery # 4: removal of implant, exchange nailing (Figure 3G)
At 12 months, the docking site was healed. To enhance consolidation of the 2 regenerated bone segmnets, and to avoid ingrowth into the slotted tube, the double bone transport device was extracted and replaced with a Stryker SCN 380/11 mm retrograde trauma nail (Stryker, Kalamazoo, MI, USA). Flushing of the canal was done with careful, slow reaming to 13 mm. This also to stimulated consolidation of the regenerate bone segments (Figure 5). During the exchange nailing, the femur was spanned with an external fixator. Extraction was not trivial, and was performed by applying pressure from above with a 3.5 mm K-wire and by pulling out the nails and the tube from below with forceps. A mild, closed brisement brought knee flexion to 90 degrees.

Figure 5. Long standing radiographs after exchange nailing. There is mild residual shortening and varus of the distal femur.
Distraction rate and rhythm, indices
After an initial latency period of 5 days, the distal (metaphyseal) segment was distracted by 0.25 mm, 4 times per day, and the proximal (diaphyseal) segment by 0.25 mm, 3 times per day. The distraction index was 170 mm/105 days = 1.6 days/mm. Consolidation index was 330 days/17 cm = 20 days/cm (11 months from insertion to exchange nailing); the standard is ~ 30 days/cm. We kept compression on the docking site by applying 0.25 mm of lengthening twice weekly (from each nail) for 5 weeks after the docking procedure, to induce healing.
The patient was allowed 20 kg weightbearing for the first 5 months of treatment, and then full weightbearing.
Discussion
Large segmental bone defects are challenging clinical problems requiring long treatment time, often 12 months or more. Surgical options include distraction osteogenesis, the Masquelet [1] technique of bone grafting into induced membranes, double-barrel free vascularized fibula [2], allograft donor bone, custom-made endoprosthesis, intercalary spacers, and even amputation.
Trifocal bone transport (BT) with external fixation frames is demanding on soft tissues, particularly in the femur, though it has been described in both tibial and femoral defects [3,4]. Newer improvements over classical external fixator bone transport include accelerated, partly or fully internal, bone transport techniques, such as a bone transport nail (BTN), plate-assisted bone-segment transport (PABST), lengthening over nails (LON), and lengthening and then nailing (LATN) [5,6]. However, with 2 counter-opposed internal lengthening nails (ILN), the soft tissues are spared, and treatment time is theoretically cut in half.
All strategies mentioned above each have their specific advantages, limitations, and shortcomings, the details of which are outside the scope of this technical note. For example, Masquelet’s technique may fail to consolidate. Vascularized fibulas will frequently break. Arthroplasty will need revision, and cadaver allografts may fail to incorporate or be subject to late fracture etc. In our view, distraction osteogenesis remains the gold standard for bone loss substitution, fully and physiologically replacing all bone lost—other methods will not have comparable lifelong stability and endurance—and this is particularly relevant in young individuals with a normal life expectancy. Furthermore, internal techniques avoid the well-known problems associated with external fixation (scarification, muscle and joint fibrosis, pin site infection). However, internal fixation assumes the soft tissues are intact and any previous infection is cleared, as the placement of a foreign object in the medullary canal will generate biofilm and increase infection risk. This risk can be lowered by adding local antibiotics [7]. The recent “Fixit” study [8] has shown that internal fixation is equivalent, if not superior, to external fixation in open fracture cases, and has comparable complication rates. Furthermore, the internal device maintains full mechanical support of the bone, should recurrence, reinfection, or metastatic disease incur. In cancer cases, concomitant radiation and chemotherapy may delay consolidation of the regenerate and call for the reconstruction to be postponed, using a temporary nail to span the defect in the meantime, or using alternative methods as mentioned earlier.
The trifocal transport strategy is advantageous over classic bifocal (one level) transport for defects of larger size to avoid prohibitively long treatment time. In a review of 21 papers on 67 bone transports after resection of malignant tumors, Jacobs et al. found an average frame time of 365 days [9], successful limb salvage in 64 patients, including 6 cases with trifocal transport in larger defects (10–23 cm), and a local recurrence rate of 1.5%. Accadbled et al. [10] likewise demonstrated that, for selected tumor patients, internal distractions osteogenesis is an excellent option, provided the tumor does not involve articular surfaces, and no concomitant chemo- and radiation therapy is undertaken, as these will slow down regenerate bone maturation.
Quinnan [11], Catagni [3], Liu [4], and others have described trifocal techniques to combine double external bone transport and lengthening, also demonstrating reduced frametime. However, for soft tissues, external trifocal transport is particularly harsh, producing scarifications and fibrosis. As an alternative to this technique, Kähler Olesen et al. [5,6] described the plate-assisted bone-segment transport with a lengthening nail (PABST) and internal bone transport. Krettek et al. [12] demonstrated a custom-made device that allowed for combined transport and lengthening in conjunction with a single ILN. Hwanget al. [13] used a single nail and wires to transport 2 segments to cover a tibial defect of comparable size. Rachbauer et al. [14] demonstrated a fibula-assisted tibial bone transport, avoiding the use of plates. In spite of some reported mechanical failures [15,16], the overall progress in internal lengthening and bone transport is a noteworthy improvement for the patient.
Ethics, funding, and disclosures
The patient gave his informed consent for this study and its publication. No funding was received. We have checked the manuscript to be in compliance with the CARE guidelines. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.18493
Supplementary data
Technical (CAD) drawings of tube and “end caps” are available as Supplementary data on the article page, doi: 10.2340/17453674.2023.18493
- Morris R, Hossain M, Evans A, Pallister I. Induced membrane technique for treating tibial defects gives mixed results. Bone Joint J 2017; 99-B(5): 680-5. doi: 10.1302/0301-620X.99B5.BJJ-2016-0694.R2.
- Petersen M M, Hovgaard D, Elberg J J, Rechnitzer C, Daugaard S, Muhic A. Vascularized fibula grafts for reconstruction of bone defects after resection of bone sarcomas. Sarcoma 2010; 2010: 524721. doi: 10.1155/2010/524721.
- Catagni M A, Azzam W, Guerreschi F, Lovisetti L, Poli P, Khan M S, et al. Trifocal versus bifocal bone transport in treatment of long segmental tibial bone defects. Bone Joint J 2019; 101-B(2): 162-9. doi: 10.1302/0301-620X.101B2.BJJ-2018-0340.R2. PMID: 30700126.
- Liu K, Liu Y, Cai F, Fan C, Ren P, Yusufu A. Efficacy comparison of trifocal bone transport using unilateral external fixator for femoral and tibial bone defects caused by infection. BMC Surgery 2022; 22(1): 141. doi: 10.1186/s12893-022-01586-z.
- Kähler Olesen U, Nygaard T, Prince D E, Gardner M P, Singh U M, McNally M A, et al. Plate-assisted bone segment transport with motorized lengthening nails and locking plates: a technique to treat femoral and tibial bone defects. J Am Acad Orthop Surg Glob Res Rev 2019; 3(8): e064. doi: 10.5435/JAAOSGlobal-D-19-00064.
- Kähler Olesen U, Herzenberg J E. Bone transport with internal devices. Techniques in Orthopaedics 2020; 35(3): 219-24. doi: 10.1097/BTO.0000000000000474.
- Morgenstern M, Vallejo A, McNally M A, Moriarty T F, Ferguson J Y, Nijs S, et al. The effect of local antibiotic prophylaxis when treating open limb fractures: a systematic review and meta-analysis. Bone Joint Res 2018; 7(7): 447-56. doi: 10.1302/2046-3758.77.BJR-2018-0043.R1. PMID: 30123494; PMCID: PMC6076360.
- Major Extremity Trauma Research Consortium (METRC). Modern external ring fixation versus internal fixation for treatment of severe open tibial fractures: a randomized clinical trial (FIXIT study). J Bone Joint Surg 2022; 104(12): 1061-7. doi: 10.2106/JBJS.21.01126.
- Jacobs N, Stubbs D, McNally M. Ilizarov distraction osteogenesis for reconstruction of long bone defects following primary malignant bone tumour resection. Int J Orthop 2019; 2(2): 58-69.
- Accadbled F, Thévenin Lemoine C, Poinsot E, Baron Trocellier T, Dauzere F, Sales de Gauzy J. Bone reconstruction after malignant tumour resection using a motorized lengthening intramedullary nail in adolescents: preliminary results. J Child Orthop 2019; 13(3): 324-9. doi: 10.1302/1863-2548.13.190016.
- Quinnan S M, Lawrie C. Optimizing bone defect reconstruction: balanced cable transport with circular external fixation. J Orthop Trauma 2017; 31(10): e347-e355.
- Krettek C, El Naga A. All internal segmental bone transport and optional lengthening with a newly developed universal cylinder-kombitube module for motorized nails: description of a surgical technique. J Orthop Trauma 2017; 31(Suppl. 5): S39-S41.
- Hwang J, Sems S, Yuan B. Trifocal tibial bone transport using a magnetic intramedullary nail: a case report. JBJS Case Connect 2021; 11(4). doi: 10.2106/JBJS.CC.20.01036.
- Rachbauer A, Laufer A, Gosheger G, Toporowski G, Frommer A, Jacob E, et al. Fibula-assisted segment transport (FAST) for defect reconstruction after resection of tibial adamantinoma: report of two treatments. Case Rep Orthop 2021; 2021: 5563931. doi: 10.1155/2021/5563931.
- Jellesen M S, Lomholt T N, Hansen R Q, Mathiesen T, Gundlach C, Kold S, et al. The STRYDE limb lengthening nail is susceptible to mechanically assisted crevice corrosion: an analysis of 23 retrieved implants. Acta Orthop 2021; 92(5): 621-7. doi: 10.1080/17453674.2021.1927506.
- Rölfing J H D, Kold S, Nygaard T, Mikuzis M, Brix M, Faergemann C, et al. Pain, osteolysis, and periosteal reaction are associated with the STRYDE limb lengthening nail: a nationwide cross-sectional study. Acta Orthop 2021; 92(4): 479-84. doi: 10.1080/17453674.2021.1903278.