Patient injury claims for posterior cruciate ligament injury: a nationwide registry study in Finland
Kirsi-Maaria NYRHINEN 1, Teemu HELKAMAA 1, Ville BISTER 1,2, Arne SCHLENZKA 1, Henrik SANDELIN 3,4, Jerker SANDELIN 5, and Arsi HARILAINEN 5
1 Department of Orthopaedics and Traumatology, University of Helsinki and Helsinki University Hospital, Helsinki; 2 Department of Surgery, Faculty of Medicine, University of Helsinki, Helsinki; 3 Department of Orthopaedics and Traumatology, Vaasa Central Hospital, Vaasa, and University of Helsinki, Helsinki; 4 Mehiläinen Sports Hospital, Vaasa; 5 Orton Orthopaedic Hospital, Helsinki, Finland
Background and purpose — Posterior cruciate ligament (PCL) injuries usually occur in combination with other ligamentous knee injuries. The outcome varies and may be poor due to suboptimal treatment. We investigated claims following PCL injury treatment on a nationwide scale.
Patients and methods — All patient PCL injury claims filed in Finland from 1997 to 2015 were collected from the Patient Insurance Centre (PIC) register. We reviewed and analyzed all records to determine the causes of claims. General background data were obtained from the National Care Register for Social Welfare and Health Care (HILMO).
Results — We found out from HILMO background data that, during the 19-year study period, 1,891 PCL and 1,380 multiligament reconstructions were performed in 99 different hospitals. The number of PCL injuries treated conservatively is unknown. During this same period, 49 claims arrived at the PIC, and 39/49 of these patients were operated on. 12/49 claims were compensated. Of these 12 claims, 6 were compensated for technical errors and 4 were compensated for diagnostic delays.
Conclusion — The number of patient injury claims was few, and compensated claims were even fewer. Technical errors and diagnostic delays were the most common reasons for reimbursement.
Citation: Acta Orthopaedica 2023; 94: 426–431. DOI: https://doi.org/10.2340/17453674.2023.18265.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2023-01-26. Accepted: 2023-07-06. Published: 2023-08-16.
Correspondence: kirsi-maaria.nyrhinen@hus.fi
K-MN: collection, analysis, and interpretation of the data; writing of the manuscript. TH, VB: conception of the study, collection and interpretation of the data, writing of the manuscript. HS: design of the data matrix. AS: collection of the data. JS, AH: conception of the study, interpretation of the data, writing of the manuscript.
The authors wish to thank Saija Lehtinen for the PIC material, Topias Kuosmanen and Joona Klemetti for the HILMO material, and Leena Ristolainen for help with statistics.
Handling co-editor: Li Felländer-Tsai
Acta thanks Pelle Gustafson and Per-Henrik Randsborg help with peer review of this manuscript.
Posterior cruciate ligament (PCL) injuries can be isolated ruptures accounting for only 3.5% of all acute knee injuries, but they often occur concomitantly with other ligamentous or capsular injuries [1-6]. In 5–20% of knee ligament injuries, a PCL injury is involved [3], and in 79% of multiligament (ML) injuries the PCL is damaged [7]. According to Sanders et al. (2017), annual incidence of isolated PCL injury is 2 per 100,000 inhabitants [8].
The rarity of isolated PCL injuries makes them difficult to diagnose, and it is not uncommon for patients to be unable to tell that such an injury has occurred. Typical injury mechanisms include hyperextension of the knee joint, or a direct trauma to the anterior aspect of the proximal tibia. Often, as time passes, the patient seeks medical attention for knee pain and/or discomfort [2,3].
There are many potential complications associated with the technical aspects of PCL reconstruction (PCLR), of which neurovascular complications are the most serious. Common technical complications include fractures during tunnel drilling and graft harvesting, and other reported complications include loss of range of motion and stiffness, knee laxity, and heterotopic ossification [9,10].
We aimed to determine the causes of patient claims following PCL injury treatments and uncover underlying root causes, and to understand how patient injuries can be avoided by acting differently [11-15].
Patients and methods
In this nationwide registry study, injury claims between 1997 and 2015 were collected. Research data was obtained from the Patient Insurance Centre (PIC) [16], and collected by reviewing the original patient records and imaging studies of claims that involved injuries related to specific diagnosis codes (International Classification of Diseases 10th edition [ICD-10]) or Nordic Medico-Statistical Committee (NOMESCO) procedure codes (Tables 1 and 2). All patient injury claims related to PCL injuries were included. We classified the PCL injuries into 3 types: grade I partial PCL ruptures, grade II total PCL rupture, and grade III PCL rupture combined with other capsuloligamentous structures [3,17,18].
The patient insurance systems in Nordic countries are nofault systems [16,19-20]. In Finland, all healthcare providers in the private and public sectors are mandated to have patient injury insurance, and insurance companies providing this type of insurance are members of PIC. Therefore, all patients are covered against financial losses from possible patient injuries. The Patient Injury Act (1986) defines patient injuries and possible compensation [16,21]. When a patient injury occurs, the goal of the PIC is to determine the root causes of the injury and reimburse the claimant if the compensation criteria are met. The 2 most common criteria that lead to reimbursement are potentially avoidable injuries and intolerable injuries. When assessing if an injury was avoidable, the main question is whether an experienced healthcare professional would have treated the patient differently and, by doing so, avoided the undesirable outcome. For tolerability, the PIC decides whether the consequences are such that no patient should tolerate them (e.g., severe infection leading to multiple revisions). An intolerable outcome must also be unexpected [14,16,22], and for an injury to be considered unexpected, the claimant’s individual preoperative complication risk must have been less than 2% (index operation).
To obtain background data on PCL injury operations, we collected registry data from the Care Register for Social Welfare and Health Care (HILMO), which is maintained by the National Institute for Health and Welfare (THL). The same NOMESCO codes (Table 2) were used as when collecting PIC data. Because most PCL injuries occur with other ligament injuries [1-5] and in 79% of ML injuries the PCL is also damaged [6], the NOMESCO codes NGE50 and NGE55 were included. It is not possible in the HILMO register to separate ML injuries where the PCL is intact.
Hospitals were categorized based on their PCLR and ML reconstructions (MLR) volumes from 1997 to 2015. High-volume hospitals each performed > 250 operations (≥ 14 operations per hospital per year), medium-volume hospitals 100–250 operations (5–13 operations per hospital per year), and low-volume hospitals < 100 operations (< 5 operations per hospital per year). The 3 groups were roughly evenly represented in the sample, with each group having completed nearly 1/3 of the operations under study.
Statistics
The data was analyzed using SPSS (Released 2019. IBM SPSS Version 26.0. IBM Corp, Armonk, NY, USA). The differences between hospital volumes and compensated claims were determined using the 2 × 3 chi-square test.
Ethics, funding, and disclosures
Permission for this study was provided by the PIC and the Ethical Board of Helsinki University (Dnr 376/13/03/02/2015). This work was supported by Orton Evo grants from the Ministry of Social Affairs and Health, Finland (A2500/464). The authors have no conflicts of interest. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.18265
Results
HILMO surgery data
1,891 PCLRs and 1,380 MLRs were performed from 1997 to 2015 at 99 different hospitals (Figure 1). The yearly averages for PCLR and MLR were 100 and 73 operations, respectively. 2 hospitals performed the most surgeries, 1/4 (26%) of all injuries. The low-volume hospitals (n = 90) performed over 1/3 of all the operations with less than 1 PCLR performed per year (Figure 2).
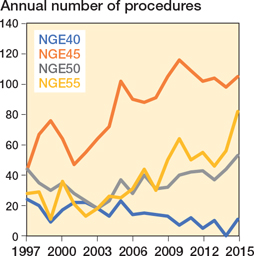
Figure 1. Posterior cruciate ligament and multiligament injury-related procedures in Finland from 1997 to 2015 from the Care Register for Social Welfare and Health Care (HILMO). For Abbreviations, see Table 2.
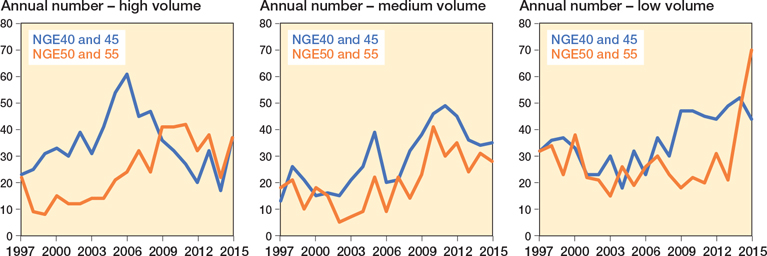
Figure 2. Number of posterior cruciate ligament reconstructions (PCLR = NGE40 + NGE45) and multiligament reconstructions (MLR = NGE50 + NGE 55) in different hospital groups. In high-volume hospitals left panel), the peak years of PCLR are between 2003 and 2006, and of MLR are between 2008 and 2011. In medium-volume hospitals (middle panel), the peak years of PCLR are between 2007 and 2011, and of MLR are between 2009 and 2011. In low-volume hospitals (right panel), the peak years of PCLR are between 2009 and 2014, and the number of MLR has started to rise since 2013. For Abbreviations, see Table 2.
The average age of the patients was 36 (median 35) years, and 2,246/3,271 (69%) of the patients were male. This proportion was consistent throughout the study period in both the PCLR and MLR groups.
PIC research data
From 1997 to 2015, the PIC received 49 patient injury claims in which PCL injury was involved (Figure 3). In 18 of the 49 claims, treatment was started conservatively, but was later changed to surgery, so in the end 39 of the 49 claims were operated on for PCL injuries. The average age of the compensated claimants was 36 years, and 28/49 (57%) patients were male. Sports- and traffic-accident-related injuries were the 2 most common injury types among claimants. The mechanisms of the injuries were often high-energy accidents and/or knee hyperextension. 17/49 (35%) of the claimants reported sports-related injuries, 13/49 (27%) traffic-accident-related injuries, and 10/49 (20%) work-related injuries.
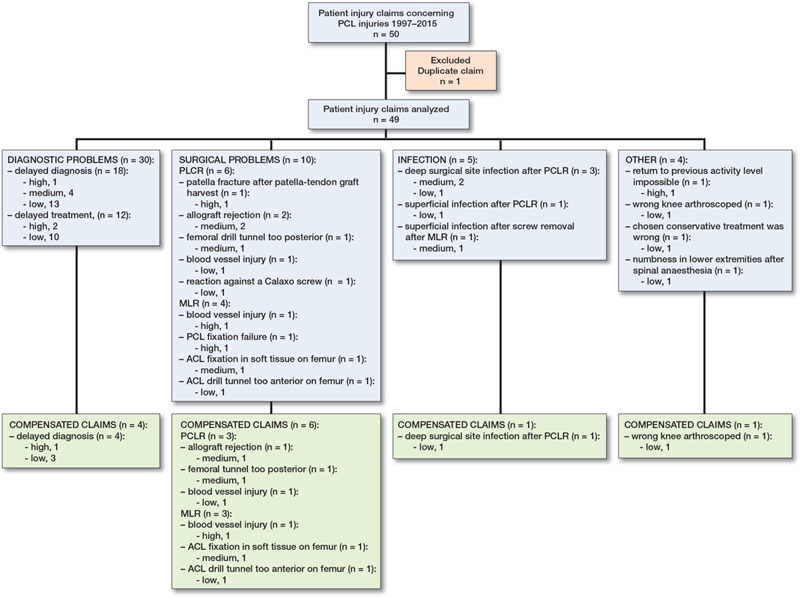
Figure 3. All patient injury claims and compensated claims from the Patient Injury Centre (PIC) from 1997 to 2015, divided into 4 categories according to the contents of the claims and the decisions of the PIC. DSSI = deep surgical site infection. ML = multiligament. MLR = ML reconstruction. PCL = posterior cruciate ligament. PCLR = PCL reconstruction. High = high-volume hospital. Medium = medium-volume hospital. Low = low-volume hospital.
Reasons for the claims were most often delay in diagnosis, care, and rehabilitation in 29 cases and pain in 21 cases (Table 3). Of the 49 injuries, 5 were grade I, 23 grade II, and 21 grade III. In the 21 grade III injuries, the anterior cruciate ligament (ACL) was injured in 16 cases, the medial collateral ligament (MCL) in 8 cases, and the lateral collateral ligament (LCL) in 6 cases. The most common injury combinations were PCL and ACL (6/21) and PCL, ACL, and MCL (5/21).
12 of 49 patient injury claimants were reimbursed. All of them had been treated surgically, and 8 required reoperation(s). In 11 cases, the injury was work-, sports-, or traffic-accidentrelated. In 2 cases, the reason for compensation was PCL injury diagnostic delay; in both cases, PCL injuries had been missed repeatedly, despite many arthroscopies and reconstruction of a partially ruptured ACL. A further 2 cases were compensated due to diagnostic delays in primary care. Furthermore, 5 cases were compensated for technical failures during surgery, 1 for allograft rejection, and 1 for deep surgical site infection (DSSI). Additionally, 1 case was reimbursed because the operation (arthroscopy) had been performed on the wrong knee. Figure 3 shows the contents of all claims as well as the contents of reimbursed claims and how the claims (reimbursed or not) were directed at different hospital groups.
Comparison of HILMO and PIC data
There is no clear correlation between the number of surgeries and claims (Figure 4). There was no statistically significant difference between a hospital’s surgical volume and the number of compensated claims it received (Table 4). When surgery-related compensated cases were examined (technical errors [n = 6] and arthroscopy of the wrong knee [n = 1]), there was no statistically significant difference between hospitals with different volumes (Table 4).
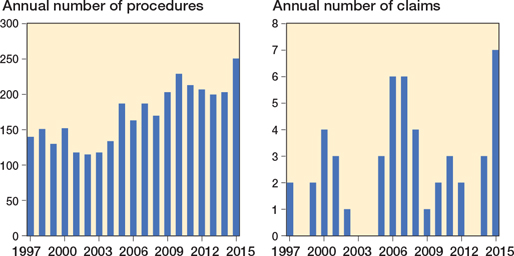
Figure 4. Annual number of posterior cruciate ligament reconstructions (PCLR) and multiligament reconstructions (MLR) (left panel) and annual number of claims submitted to the PIC (right panel) from 1997 to 2015.
| Hospital volume a | No. of hospitals | Total | Non-compensated | Compensated | Technical error, n | ||||
| n (%) | range | n (%) | P value | No | Yes | P value | |||
| High (≥ 14) | 3 | 1,121 | 1,119 (34) | 265–545 | 2 (17) | 1,120 | 1 | ||
| Medium (5–13) | 6 | 930 | 927 (28) | 123–229 | 3 (25) | 0.3 | 927 | 3 | 0.5 |
| Low (< 5) | 90 | 1,220 | 1,213 (37) | 1–81 | 7 (58) | 1,217 | 3 | ||
| Total | 3,271 | 3,259 | 12 | 3,264 | 7 | ||||
| There is no statistically significant difference in the compensated claims received by hospitals in different categories related to the treatment of PCL injuries. HILMO = Care Register for Social Welfare and Health Care. PIC = Patient Insurance Centre. a PCLR and/or MLR operations per year in parentheses. |
|||||||||
Discussion
This study shows that patient injuries related to the treatment of PCL injuries are rare. The main causes were delay in diagnosis and technical errors during surgery.
Aae et al. (2020) studied patient injury claims related to treatments concerning focal knee cartilage defects in Scandinavian countries, combining data from patient injury claim systems from Norway, Denmark, and Sweden. They found only 103 (0.2%) patients complained about their treatment, of whom 0.08% received compensation [23]. Randsborg et al. (2021) studied patient injury claims after knee arthroplasty in Norway between 2008 and 2018. 572/64,241 (0.9%) claims were filed, and 0.5% were compensated [24]. In these studies, like ours, the number of people who applied for compensation was small. A large proportion of patients who would be entitled to compensation after a patient injury do not apply for it [25], of whom up to 97% of patients entitled to compensation do not apply [26].
It has been shown that there are more reimbursed claims among hospitals with fewer knee arthroplasties per year than those with more [24]. Also, Helkamaa et al. (2016) showed that hospitals performing more than 400 total hip arthroplasties per year received fewer patient injury claims and compensated those that were due to technical error [14]. However, in our study, a statistically significant difference could not be shown when hospital volumes and compensated claims were compared.
We do not know if the claimants and compensated cases represented all patients who had PCL injuries and had been treated either conservatively or surgically. But, compared with other studies [8,27], the patients in our study seemed to be very similar; that is, the typical PCL rupture patient is over 30 years old and male, and the PCL usually ruptures with other capsuloligamentous structures [27]. In our study, no single surgical complication emerged above others. The complications were the same as those presented in the literature [9,10], and previously known challenges in diagnosing PCL injuries re-emerged in this study [2,3]. Australian researchers identified that between 1998 and 2008, the number of female patients with PCL injury or knee dislocation rose and the gap between males and females narrowed, but the number of male patients remained greater [28]. However, in our study, there was no such trend, with the representation of the sexes remaining constant. According to Bismarck et al. (2006) and Pukk et al. (2003), women fill out a patient injury claim file more often than men [26,29]. Among the Finnish PCL injury patients, men were more likely to fill out a claim file, but the explanation for this may be that there were more men in this study in general.
In our study, more PCLRs were performed than MLRs. From previous studies, we know that isolated PCL rupture is rare, and it is common for other capsuloligamentous structures to be injured at the same time as the PCL [1-4]. Accordingly, the number of surgeries for isolated PCL injuries was low. This has been shown in 2 Scandinavian studies using knee ligament registries in Norway, Denmark, and Sweden [27,30]. When all operations in Norway, Denmark, and Sweden were counted in the study by Owesen et al. (2017), 38% were isolated PCLRs and 62% were PCLRs combined with other capsuloligamentous reconstructions [27]. In the study by Lind et al. (2018), based solely on Danish data, 41% were isolated PCLRs and 59% were combined [30]. Meanwhile, Longo et al. (2021) showed that the incidence of isolated PCLR in Italy was 0.46/100,000 inhabitants [31]. In our study, based on data from the Finnish HILMO register, 58% of treatments were isolated PCLRs and 42% were MLRs, and the incidence of isolated PCLR was 1.9/100,000 inhabitants, while that of MLR was 1.4/100,000 inhabitants. Thus, our results are in opposition to those of other studies and countries.
The above differences between Finland and other countries may be explainable either by the fact that isolated PCL injuries are more common in Finland than elsewhere, or because of inaccuracy in the use of procedure codes for surgeries. In Finland, there is no ligament registry that provides exact injury numbers and specifies whether an injury has occurred to the PCL or ACL. It is unclear how many MLRs included PCL reconstruction. But to get background data from HILMO we included the ML operations because the majority (79%) involves the PCL [6]. Furthermore, it is more common that the PCL ruptures together with other ligaments [1-5]. Information on conservatively treated patients is also lacking, and from the HILMO data it is impossible to tell which cruciate ligament the ICD-10 codes concern.
If information is collected systematically and structurally, as in the Danish Knee Ligament Reconstruction Registry [30], a register will become more accurate and reliable. From the Finnish material, it is not possible to say whether claims and compensated claims have led to changes in diagnostics or treatments. In the study by Randsborg et al. (2018), data was combined from both the Norwegian System of Patient Injury Compensation, which corresponds to the Finnish PIC, and the Norwegian Knee Ligament Registry [32]. The research team studied patient injury claims following ACL treatments. The Norwegian Knee Ligament Registry had shown that use of a hamstring graft led to infection more often than the use of a bone–tendon–bone (BTB) graft; thus, the latter became popular in Norway [32]. This provides a good example of how registers systematically compiled over years can reveal changes and trends and thus guide treatment practices.
Conclusion
There were few patient injury claims related to PCL treatments, and only a very small proportion of operations were reimbursed. The most common reasons for reimbursement were diagnostic delay and technical surgical errors. There was no statistically significant difference between hospital groups with different surgical volumes and compensated claims.
- Clancy W G, Sutherland T B. Combined posterior cruciate ligament injuries. Clin Sports Med 1994; 13: 629-47. PMID: 7954888.
- Shelbourne K D, Davis T J, Patel D V. The natural history of acute, isolated, nonoperatively treated posterior cruciate ligament injuries: a prospective study. Am J Sports Med 1999; 27(3): 276-83. doi: 10.1177/03635465990270030201.
- Hettrich C M, Marx R G, Parker RD, Matava M J, Sekiya J K. Ligamentous injuries of the knee. In Boyer MI, editor. AAOS Comprehensive orthopaedic review. Rosemont: American Academy of Orthopaedic Surgeons; 2014. p. 1383-85.
- LaPrade C M, Civitarese D M, Rasmussen M T, LaPrade R F. Emerging updates on the posterior cruciate ligament: a review of the current literature. Am J Sports Med 2015; 43: 3077-92. doi: 10.1177/0363546515572770.
- Bedi A, Musahl V, Cowan J B. Management of posterior cruciate ligament injuries: an evidence-based review. J Am Acad Orthop Surg 2016; 24(5): 277-89. doi: 10.5435/JAAOS-D-14-00326.
- Fanelli G C, Edson C J. Posterior cruciate ligament injuries in trauma patients: Part II. Arthroscopy 1995; 11(5): 526-9. doi: 10.1016/0749-8063(95)90127-2.
- Becker E H, Watson J D, Dreese J C. Investigation of multiligamentous knee injury patterns with associated injuries presenting at a level I trauma center. J Orthop Trauma 2013; 27(4): 226-31. doi: 10.1097/BOT.0b013e318270def4.
- Sanders T L, Pareek A, Barrett I J, Kremers H M, Bryan A J, Stuart M J, et al. Incidence and long term follow up of isolated posterior cruciate ligament tears. Knee Surg Sports Traumatol Arthrosc 2017; 25: 3017-23. doi: 10.1007/s00167-016-4052-y.
- Zawodny S R, Miller M D. Complications of posterior cruciate ligament surgery: review article. Sports Med Arthrosc Rev 2010; 18(4): 269-74. doi: 10.1097/JSA.0b013e3181f2f4c2.
- Marom N, Ruzbarsky J J, Boyle C, Marx R G. Complications in posterior cruciate ligament injuries and related surgery. Sports Med Arthrosc Rev 2020; 28(1): 30-3. doi: 10.1097/JSA.0000000000000247.
- Järvelin J, Häkkinen U, Rosenqvist G, Remes V. Factors predisposing to claims and compensations for patient injuries following total hip and knee arthroplasty. Acta Orthop 2012; 83(2): 190-6. doi: 10.3109/17453674.2012.672089.
- Hakala T, Vironen J, Karlsson S, Pajarinen J, Hirvensalo E, Paajanen H. Fatal surgical or procedure-related complications: a Finnish registry-based study. World J Surg 2014; 38(4): 759-64. doi: 10.1007/s00268-013-2364-3.
- Vallila N, Sommarhem A, Paavola M, Nietosvaara Y. Pediatric distal humeral fractures and complications of treatment in Finland: a review of complication claims from 1990 through 2010. J Bone Joint Surg Am 2015; 97(6): 494-9. doi: 10.2106/JBJS.N.00758.
- Helkamaa T, Hirvensalo E, Huhtala H, Remes V. Patient injuries in primary total hip replacement. Acta Orthop 2016; 87(3): 209-17. doi: 10.3109/17453674.2015.1135662.
- Sandelin H, Waris E, Hirvensalo E, Vasenius J, Huhtala H, Raatikainen T, et al. Patient injury claims involving fractures of the distal radius. Acta Orthop 2018; 89(2): 240-5. doi: 10.1080/17453674.2018.1427966.
- Patient Insurance Centre [Internet]. Potilasvakuutuskeskus; n.d. Available from: www.pvk.fi/en/ (English version).
- Shon O J, Park J W, Kim B J. Current concepts of posterolateral corner injuries of the knee: review article. Knee Surg Relat Res 2017; 29(4): 256-68. doi: 10.5792/ksrr.16.029.
- Wind W M, Bergfeld J A, Parker R D. Evaluation and treatment of posterior cruciate ligament injuries: revisited. Am J Sports Med 2004; 32(7): 1765-75. doi: 10.1177/0363546504270481.
- Palonen R, Nio A, Mustajoki P. Potilas- ja lääkevahingot: korvaaminen ja ennaltaehkäisy [Patient and medication injuries – compensation and prevention]. Jyväskylä: Talentum Media Oy; 2005 [in Finnish].
- Järvelin J, Häkkinen U. Can patient injury claims be utilised as a quality indicator? Health Policy 2012; 104: 155-62. doi: 10.1016/j.healthpol.2011.08.012.
- Patient Injury Act 25.7.1986/585. Available from: www.finlex.fi/fi/laki/ajantasa/1986/19860585.
- Mikkonen M. Prevention of patient injuries: the Finnish patient insurance scheme. Med Law 2004; 23: 251-7. PMID: 15270468.
- Aae T F, Lian Ø B, Årøn A, Engebretsen L, Randsborg P H. Compensation claims after knee cartilage surgery is rare: a registry-based study from Scandinavia from 2010 to 2013. BMC Musculoskelet Disord 2020; 21: 287. doi: 10.1186/s12891-020-03311-4.
- Randsborg P H, Aae T F, Bukholm I R K, Fenstad A M, Furnes O, Jakobsen R B. Compensation claims after knee arthroplasty surgery in Norway 2008–2018. Acta Orthop 2021; 92: 189-93. Doi: 10.1080/17453674.2020.1871187.
- Järvelin J. Studies on field and compensated claims for patient injuries. University of Helsinki. Juvenes Print – Finnish University Print Ltd. Tampere, Finland; 2012 [serial online]. Available from: http://urn.fi{URN:ISBN:978-952-245-750-9.
- Bismark M, Brennan T A, Davis P B, Studdert D M. Claiming behaviour in a no-fault system of medical injury: a descriptive analysis of claimants and non-claimants. Med J Aust 2006; 185: 203-7. doi: 10.5694/j.1326-5377.2006.tb00532.x
- Owesen C, Sandven-Thrane S, Lind M, Forssblad M, Granan L-P, Årøen A. Epidemiology of surgically treated posterior cruciate ligament injuries in Scandinavia. Knee Surg Sports Traumatol Arthrosc 2017; 25: 2384-91. doi: 10.1007/s00167-015-3786-2.
- Maniar N, Verhagen E, Bryant A L, Opar D A. Trends in Australian knee injury rates: an epidemiological analysis of 228,344 knee injuries over 20 years. Lancet Reg Health West Pac 2022: 21: 100409. doi: 10.1016/j.lanwpc.2022.100409.
- Pukk K, Lindberg J, Penaloza-Pesantes R V, Brommels M, Gafney F A. Do women simply complain more? National patient injury claims data show gender and age differences. Qual Manag Health Care 2003; 12: 225-31. doi: 10.1097/00019514-200310000-00007.
- Lind M, Nielsen T G, Behrndtz K. Both isolated and multi-ligament posterior cruciate ligament reconstruction results in improved subjective outcome: results from Danish Knee Ligament Reconstruction Registry. Knee Surg Sports Traumatol Arthrosc 2018; 26: 1190-6. doi: 10.1007/s00167-017-4577-8.
- Longo U G, Viganó M, Candela V, de Girolamo L, Cella E, Thiebat G, et al. Epidemiology of posterior cruciate ligament reconstructions in Italy: a 15-year study. J Clin Med 2021; 10: 499. doi: 10.3390/jcm10030499.
- Randsborg P H, Bukholm I R K, Jakobsen R B. Compensation after treatment for anterior cruciate ligament injuries: a review of compensation claims in Norway from 2005 to 2015. Knee Surg Sports Traumatol Arthrosc 2018; 26: 628-33. doi: 10.1007/s00167-017-4809-y.