Surgical approach had minor association with femoral stem migration in total hip arthroplasty: radiostereometric analysis of 61 patients after 5-year follow-up
Kristin HAUGAN 1, Olav A FOSS 1,2, Otto S HUSBY 1,2, Vigdis S HUSBY 1,3, Svein SVENNINGSEN 4, and Siri B WINTHER 1
1 Department of Orthopaedic Surgery, St Olavs Hospital HF, Trondheim; 2 Department of Neuromedicine and Movement Science, Faculty of Medicine and Health Science, Norwegian University of Science and Technology, Trondheim; 3 Department of Health Sciences Aalesund, Faculty of Medicine and Health Science, Norwegian University of Science and Technology, Aalesund; 4 Orthopaedic Department, Sørlandet Hospital, Arendal, Norway
Background and purpose — Total hip arthroplasty (THA) is usually performed using 1 of 3 surgical approaches: direct lateral (DLA), posterior (PA), or anterior (AA). AA is different from DLA and PA owing to limited intraoperative visibility of the femoral canal. This could affect stem positioning and therefore migration. We aimed to perform an exploratory radiostereometric analysis (RSA) study with 3 groups for surgical approach assessing stem migration up to 5 years postoperatively.
Patients and methods — 61 patients with unilateral osteoarthritis of the hip were included. 21 patients were allocated to the DLA, 20 to the PA, and 20 to the AA group. All patients received an uncemented, collarless, double-tapered, fully hydroxyapatite-coated Profemur Gladiator stem. Migration was measured with model-based RSA. Baseline RSA was on day 1 postoperatively. The follow-ups were at day 8, at 5 weeks, and at 3, 6, 12, 24, and 60 months after surgery. Generalized linear mixed models were used to analyze maximum total point motion (MTPM) migrations.
Results — Group mean differences in MTPM were 0.4 mm (95% confidence interval [CI] –1.5 to 2.4) for DLA vs. PA, 1.1 mm (CI –1.0 to 3.3) for AA vs. DLA, and 1.6 mm (CI –0.8 to 3.9) for AA vs. PA, when adjusted for sex and age as covariates. 2 stems in the AA group had excessive early migration. For all stems the migrations occurred mainly within 5-week follow-up and then stabilized.
Conclusion — At 5-year follow-up, there were no statistically significant differences in stem migration associated with the 3 surgical approaches used in this study.
Citation: Acta Orthopaedica 2023; 94: 410–415. DOI https://doi.org/10.2340/17453674.2023.18264.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-04-27. Accepted: 2023-06-19. Published: 2023-08-09.
Correspondence: kristinpost@gmail.com
KH performed the RSA analysis and RSA patient follow-up, interpreted the results, drafted, wrote, and revised the manuscript. OAF performed the statistical analysis, interpreted the results, and revised the manuscript. OSH planned the study, performed the surgery, discussed, and revised the manuscript. VSH administered and performed the follow-up and revised the manuscript. SS performed the surgery and revised the manuscript. SBW planned and administered the study, performed follow-up, and revised the manuscript. All authors approved the final version.
Handling co-editors: Bart Swierstra and Robin Christensen
Acta thanks Lennard Koster and Inari Laaksonen for help with peer review of this manuscript.
In total hip arthroplasty (THA) the direct lateral (DLA), posterior (PA), and anterior (AA) surgical approaches are most used. A review [1] concluded that DLA and PA give good exposure of the acetabulum and femur whereas AA gives good visualization of the acetabulum but not the femur. The AA approach is associated with increased early risk of major surgical complications and revision including femoral loosening, but also better functional recovery [2-7]. A possible explanation could be the more difficult preparation of the femur.
Cementless femoral stems rely on good initial press-fit fixation to achieve bony fixation. If this fails, the consequences can be continuous stem subsidence, with increased risk of early revision [8]. Radiostereometric analysis (RSA) can be used to quantify motion between implants and the surrounding bone, with only a small number of patients included [9]. We expected that a further RSA study could contribute useful information on the early loosening of stems inserted via AA.
We compared the 5-year migration of an uncemented femoral stem among 3 surgical approaches for THA. By reporting group mean results as well as individual results, possible cases with excessive migration could be identified.
Patients and methods
This RSA study with stem migration at 5 years as primary outcome is part of a project evaluating surgical approach in THA. Studies from the project reporting on muscular strength and physical function are previously published [10,11].
The present RSA study should be regarded as an exploratory study, as no a-priori statistical power analysis was made.
The study is reported in accordance with the STROBE guidelines.
In the original study, patients with unilateral osteoarthritis (OA) and scheduled for primary THA were assessed for eligibility. Those aged 70 years or younger, with a BMI of less than 34, with ASA I, II, and stable III were included. The exclusion criteria were any other disease or illness that entailed difficulty with leg strength testing. The inclusion period was between June 2011 and June 2013.
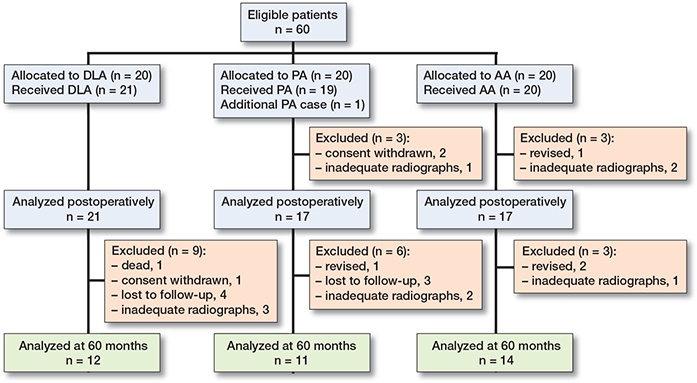
All 3 surgeons in this study had extensive experience in the type of approach they used. Our hospital used DLA as the standard approach for THA with limited experience in performing AA. Therefore, 1 external surgeon (SS) with long experience performing AA was included in the team to limit learning curve effects of AA [12,13]. This external surgeon was only available for surgery on predetermined weeks. This resulted in a block-wise allocation and surgery of patients into the 3 groups: the 1st 21 patients to the DLA group, the next 19 patients to the PA group, and the last 20 patients to the AA group. For this RSA study we added 1 more patient to the PA group so as to have at least 20 in each group (Figure 1).
The patients were mobilized 3 to 4 hours after surgery. All patients followed the standard postoperative rehabilitation recommended for hip and knee arthroplasty patients at our hospital. This included a prescription for outpatient physical therapy for 3 months, and the patients contacted a physiotherapist of their own choice.
Implants
All patients received an uncemented, collarless, double-tapered, fully hydroxyapatite (HA)-coated femoral stem, size 1–9 (Profemur Gladiator, Wright Medical Technology Inc, Memphis, TN, USA) (Figure 2). All stems were combined with a modular neck of the same alloy and a ceramic head. The acetabular component was an uncemented, porous-coated shell with a highly cross-linked polyethylene liner (Reflection, Smith & Nephew, London, UK). All patients in the DLA group and 2 in the PA group received a 28-mm head. The 3rd patient in the PA group experienced a hip dislocation. Hence, the remaining patients in the PA group, and all the patients in the AA group received a 32-mm head.
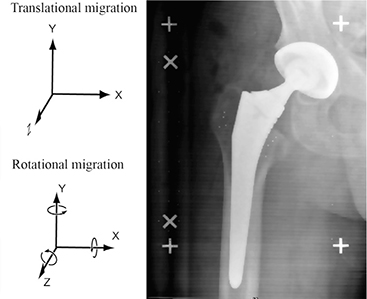
Figure 2. Gladiator stem, labelled with the axes and directions of the rotations used. Positive translations are defined as: X (medial translation), Y (proximal translation), Z (anterior translation). Corresponding rotations are defined as: X (anterior tilt), Y (retroversion), Z (valgus tilt). Tantalum markers embedded in the bone are visible.
Surgical procedures
DLA was performed with the patient in the lateral position. A posterior curved lateral incision as described by Hardinge was used [14]. The anterior third of the gluteus medius and the vastus lateralis was dissected from the greater trochanter as 1 unit. The anterior aspect of this common muscle plate was reconstructed using a combination of non-resorbable and slowly resorbable sutures (PremiCron, B. Braun, Melsungen, Germany).
PA was also performed with the patient in the lateral position. The method described by Kocher and Langenbech, and modified by Gibson, was used [15]. The external rotators (piriformis muscle and gemelli muscles) and the posterior capsule were divided close to the greater trochanter and folded posteriorly to protect the sciatic nerve. For reconstruction, the capsule and the muscles were reinserted with 2 non-resorbable osteo-sutures (PremiCron).
AA was performed with the patient in the supine position. The method described by Smith-Peterson and modified by Berend et al. [16] was used. The blunt dissection was made between the sartorius muscle and the tensor fascia lata muscle, lateral to the rectus muscle.
RSA
The implant manufacturer provided computer-aided design surface models of each stem size. The models were converted to the model-based format (RSAcore, Department of Orthopedic Surgery, Leiden University Medical Center, Leiden, The Netherlands). Tantalum markers (1.0 mm) were embedded in the bone during surgery, 5 in the trochanter major and 4 in the trochanter minor. RSA was performed according to RSA guidelines [9].
During radiographic examination the patient was in the supine position with the calibration cage positioned under the examination table (cage 43, RSA Biomedical, Umeå, Sweden) using 1 ceiling mounted and 1 portable X-ray tube. The baseline RSA examination was performed on the 1st postoperative day after having partly loaded the joint. Subsequent examinations were performed on day 8, at 5 weeks, and at 3-, 6-, 12-, 24-, and 60-month follow-up. The precision of the RSA technique was measured by 30 double examinations at the 24-month follow-up (Table 1). 2 pairs of radiographs were taken within a time interval of 10 minutes. The patient was off the table between the examinations; the radiographic equipment remained unchanged.
The analysis was performed with model-based RSA (RSAcore, Department of Orthopedic Surgery, Leiden University Medical Center, Leiden, The Netherlands). The upper limit threshold of the mean rigid body error (ME) was set to 0.35, and the condition number (CN) threshold was set to 120. The coordinate system reference was set to the right hand-side of the body when calculating migration (Figure 2).
Migration results were expressed in 2 ways: (1) Maximum total point motion (MTPM) was used presenting group mean results and used in the statistical analysis. For model-based RSA, MTPM is the length of the translation vector of the point on the model that moved the most. We see this as a valid approach as all patients received implants of the same design [9]. (2) Individual results are presented as rotations and translations related to the 3 orthogonal axes (Figure 2). Thereby, results of 6 degrees of freedom are presented to facilitate the visualization of possible stems with larger and combined migrations.
Statistics
Categorical variables were presented as frequencies. Continuous variables were presented as mean with min–max and standard deviation (SD). MTPM on group level is depicted as mean values with 95% confidence interval (CI) of the mean, as was the RSA translation along and rotation about the Y-axis. Individual rotations and translations related to the 3 orthogonal axes at stem level are depicted in 6 line charts.
Generalized linear mixed models (GLMM) were used to analyze MTPM migrations. Fixed factors were groups and time points, modelled with a random subject intercept and an interaction term between group and timepoints. Sex and age were included as covariates because bone mineral density (BMD) affects initial stability in cementless THA [18] and BMD is correlated with these factors [18]. The group differences in MTPM at 5-year follow-up were calculated without and with the inclusion of covariates, using sequential Bonferroni adjustment of p-values. The residuals were normally distributed; this was verified with histograms.
To determine the precision of RSA measurements, the following was calculated: (1) the difference between each of the double measurements (xi); (2) the SD of the differences, with respect to zero (not to the mean) (√((∑n(i=1)(xi)2)/n) [19]; and (3) multiplying the SD by 2.042, representing the 2-tailed 95% t-distribution for a sample size of 30. Statistical analyses were performed using SPSS (version 27; IBM Corp, Armonk, NY, USA).
Ethics, registration, data sharing plan, funding, and disclosures
The study was approved by the regional ethics committee (Dnr 2011/450) and registered at ClinicalTrials.gov (NCT01959360). All methods were in accordance with the relevant guidelines and regulations. Prior to surgery, the patients provided written informed consent to participate. Grouped data or tables of data without possibility of identification are available. This study did not receive any form of grants or funding. The authors declare no conflict of interests. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.18264
Results
55 patients were available for follow-up after postoperative RSA (Table 2); 37 patients attended final follow-up (Figure 1).
There was no difference in the mean MTPM at 5 years for the 3 groups at 2.2 (SD 1.4) mm, 1.7 (0.8) mm, and 3.1 (3.7) mm for the DLA, PA, and AA group, respectively (Table 3 and Figure 3). The effect of the covariates on the results was negligible when adjusting for sex and age (p = 0.3) (Table 4). Mean MTPM showed initial migration outside precision level (1.4 mm) for the AA group from 8-day follow-up, and for the DLA and PA group from 5-week follow-up (Figure 3).
| MTPM (mm) | DLA (n = 12) | PA (n = 11) | AA (n = 14) |
| Mean (SD) | 2.2 (1.4) | 1.7 (0.8) | 3.1 (3.7) |
| Median (IQR) | 1.7 (1.1–3.6) | 1.4 (1.1–2.3) | 2.6 (1.2–3.4) |
| Min–max | 0.8–4.8 | 0.7–3.3 | 0.6–15 |
| For abbreviations, see Table 2. | |||
| Model estimates | Group mean MTPM differences (95% CI) | ||
| DLA vs. PA | AA vs. DLA | AA vs. PA | |
| Without covariates | 0.5 (–1.5 to 2.6) | 0.9 (–1.3 to 3.1) | 1.4 (–1.0 to 3.8) |
| With covariates | 0.4 (–1.5 to 2.4) | 1.1 (–1.0 to 3.3) | 1.6 (–0.8 to 3.9) |
| For abbreviations, see Table 2. | |||
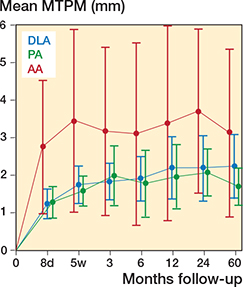
Figure 3. Group MTPM means with 95% CIs at all follow-ups.
All 3 groups subsided along and rotated about the Y-axis; the AA group migrated the most in all directions (Figure 4). Migrations of the individual stems showed that 2 stems in the AA group had early large migrations along the Y-axis, with subsidence of 8.3 mm and 2.6 mm and rotation of 19.1° and 11.5°, respectively. They were both stable after the 3-month follow-up. Nearly all migration in all 3 groups occurred within 5 weeks; the migration then flattened, and stabilized after 3 months (Figure 5).
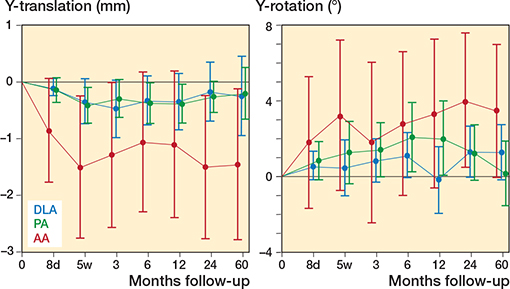
Figure 4. Translation along and rotation about the Y-axis. Values are mean with 95% CI on group level at all follow-ups.
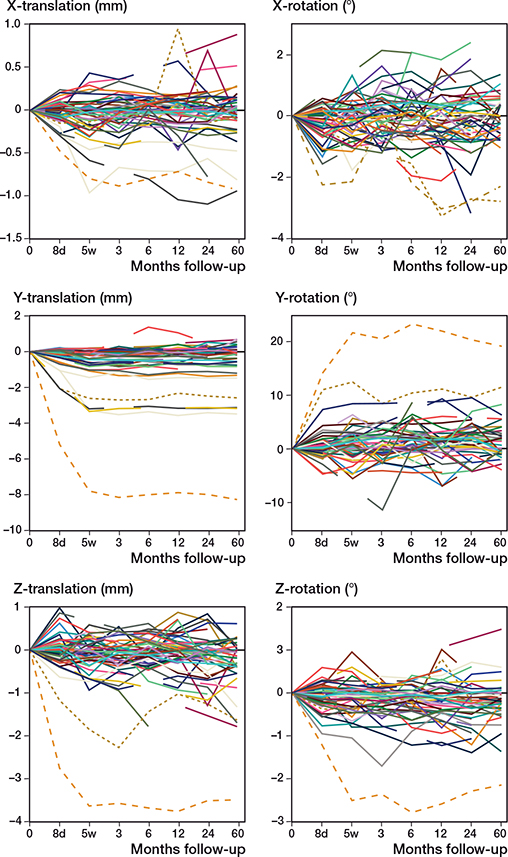
Figure 5. Migration of all individual stems at all follow-ups. 2 stems with excessive migration were in the AA group and are highlighted using dotted lines. Note differences in the scale of the Y-axis.
4 patients underwent revision surgery. 1 patient in the PA group (male) was revised because of dislocation and newly discovered osteoporosis. 3 patients in the AA group were revised for the following reasons: 1 patient (male) had an implant neck fracture 3 years postoperatively, following a trauma accident. For 1 patient (male) the liner was not properly inserted and dislocated from the shell immediately post-operatively. This patient also had a periprosthetic fracture 1 week postoperatively. For 1 patient (female) the femoral offset was 6 mm reduced. She had revision surgery with a change of the modular neck into a longer version. No implants were revised for aseptic loosening.
Discussion
We found negligible differences between 3 surgical approaches with regard to MTPM of the femoral stem at 5-year follow-up. The migration pattern showed an initial stem migration mainly within the 1st 5 weeks, which then levelled out with no continuous migration after 3 months. When considering the individual migration patterns among approaches, 2 stems in the AA group initially had larger subsidence and rotation compared with the other stems. However, the 2 stems stabilized at 3 months and no further subsidence or rotation was observed.
Early and continuous migration is related to risk of aseptic loosening [8]. However, the literature does not conclude an acceptable magnitude of clinical migration measured by RSA for uncemented stems. A review stated that the stabilization of migration can be more relevant than the absolute value of migration, when defining acceptable migration thresholds for uncemented stems [20]. Others have suggested that a continuous migration after 3 to 6 months could be a risk factor for later loosening, describing a “gold standard” type of migration, where postoperative migration is followed by almost complete stabilization within 3–6 months after surgery [21].
The Gladiator uncemented stem used in our study is anatomically similar to the Corail uncemented stem (DePuy Orthopaedics Inc, Warsaw, IN, USA). An RSA study showed that stems inserted via AA had significantly more migration in the first 2 weeks after surgery for both stem designs [22]. Thereafter, the implants were stable in both groups like the findings in our study.
A systematic review reported implant position among several surgical approaches for THA [23]. The AA had the worst and the PA the best result compared with the reference value.
Somewhat limited intraoperative visibility of the femur with the AA could cause difficulties with component placement and could explain our high early migration in the AA group, which indicates looser initial stem fixation.
1 study reported no influence of surgical approach on the canal fill of the proximal femur [24]. Another reported increased risk of stem undersizing with AA [25]. In our study the median stem size was equal in the DLA and PA group and 1 size smaller in the AA group. With the number of patients included we cannot draw any conclusion as to the possible effects on approach and stem size.
Low BMD reduces immediate implant stability in cementless THA [18]. As BMD is influenced by age and sex, these 2 variables were included as covariates in the statistical analyses. When comparing the results from the analysis without and with inclusion of the covariates, the results were almost similar. The CIs were smaller when including the covariates with almost no effect on differences in mean MTPM among the 3 approaches.
Results below the precision level could be due to measurement errors. In Figure 3 the group mean MTPM with wide CIs of the mean is depicted. With a higher number of patients included at 5-year follow-up the intervals would have been narrower. As it stands, most of the lower limit of CIs is lower than the precision level. RSA holds high precision, enabling detection of an excessively migrating prosthesis with the use of small sample sizes [9]. However, with small samples, the CIs for the estimates can be too wide to enable accurate prediction regarding the general outcome of prosthesis design. To overcome such shortcoming, minimum sample sizes of 50 would be appropriate [26]. Our sample size at 5-year follow-up was 37. However, by presenting results of the individual stems, we were able to identify stems with excessive migration.
There were several limitations of the study. The high number of missing cases were caused by inadequate radiograph quality, and by patients who failed to attend scheduled follow-ups. The initial frequent examinations, i.e., 5 examinations within the first year, may have had a negative impact on patients’ willingness to attend the follow-ups, though a GLMM statistical analysis was used to overcome missing values. The planned randomized study design was hampered by our limited experience with the AA. This led us to a non-randomized study and a block-wise performance of surgery as the external surgeon was available only on a weekly basis. However, including a surgeon performing the specific approach also limited erroneous results in the AA group due to a learning curve.
In conclusion, there were no statistically significant differences in stem migration associated with the 3 surgical approaches used in this study at the 5-year follow-up, but 2 stems inserted via AA had excessive early migration.
- Petis S, Howard J L, Lanting B L, Vasarhelyi E M. Surgical approach in primary total hip arthroplasty: anatomy, technique and clinical outcomes. Can J Surg 2015; 58(2): 128-39. doi: 10.1503/cjs.007214.
- Pincus D, Jenkinson R, Paterson M, Leroux T, Ravi B. Association between surgical approach and major surgical complications in patients undergoing total hip arthroplasty. JAMA 2020; 323(11): 1070-6. doi: 10.1001/jama.2020.0785.
- Hoskins W, Bingham R, Lorimer M, Hatton A, de Steiger R N. Early rate of revision of total hip arthroplasty related to surgical approach: an analysis of 122,345 primary total hip arthroplasties. J Bone Joint Surg Am 2020; 102(21): 1874-82. doi: 10.2106/jbjs.19.01289.
- Wang Z, Hou J Z, Wu C H, Zhou Y J, Gu X M, Wang H H, et al. A systematic review and meta-analysis of direct anterior approach versus posterior approach in total hip arthroplasty. J Orthop Surg Res 2018; 13(1): 229. doi: 10.1186/s13018-018-0929-4.
- Angerame M R, Fehring T K, Masonis J L, Mason J B, Odum S M, Springer B D. Early failure of primary total hip arthroplasty: is surgical approach a risk factor? J Arthroplasty 2018; 33(6): 1780-5. doi: 10.1016/j.arth.2018.01.014.
- Charney M, Paxton E W, Stradiotto R, Lee J J, Hinman A D, Sheth D S, et al. A Comparison of risk of dislocation and cause-specific revision between direct anterior and posterior approach following elective cementless total hip arthroplasty. J Arthroplasty 2020; 35(6): 1651-7. doi: 10.1016/j.arth.2020.01.033.
- Melbye S M, Haug S C D, Fenstad A M, Furnes O, Gjertsen J E, Hallan G. How does implant survivorship vary with different Corail femoral stem variants? Results of 51,212 cases with up to 30 years of follow-up from the Norwegian Arthroplasty Register. Clin Orthop Relat Res 2021; 479(10): 2169-80. doi: 10.1097/corr.0000000000001940.
- Mjöberg B. Is early migration enough to explain late clinical loosening of hip prostheses? EFORT Open Rev 2020; 5(2): 113-17. doi: 10.1302/2058-5241.5.190014.
- Valstar E R, Gill R, Ryd L, Flivik G, Börlin N, Kärrholm J. Guidelines for standardization of radiostereometry (RSA) of implants. Acta Orthop 2005; 76(4): 563-72. doi: 10.1080/17453670510041574.
- Winther S B, Husby V S, Foss O A, Wik T S, Svenningsen S, Engdal M, et al. Muscular strength after total hip arthroplasty: a prospective comparison of 3 surgical approaches. Acta Orthop 2016; 87(1): 22-8. doi: 10.3109/17453674.2015.1068032.
- Winther S B, Foss O A, Husby O S, Wik T S, Klaksvik J, Husby V S. Muscular strength and function after total hip arthroplasty performed with three different surgical approaches: one-year follow-up study. Hip Int 2019; 29(4): 405-11. doi: 10.1177/1120700018810673.
- de Steiger R N, Lorimer M, Solomon M. What is the learning curve for the anterior approach for total hip arthroplasty? Clin Orthop Relat Res 2015; 473(12): 3860-6. doi: 10.1007/s11999-015-4565-6.
- Yue C, Kang P, Pei F. Comparison of direct anterior and lateral approaches in total hip arthroplasty: a systematic review and meta-analysis (PRISMA). Medicine (Baltimore) 2015; 94(50): e2126. doi: 10.1097/md.0000000000002126.
- Hardinge K. The direct lateral approach to the hip. J Bone Joint Surg Br 1982; 64(1): 17-19.
- Gibson A. Posterior exposure of the hip joint. J Bone Joint Surg Br 1950; 32-b(2): 183-6.
- Berend K R, Lombardi A V Jr, Seng B E, Adams J B. Enhanced early outcomes with the anterior supine intermuscular approach in primary total hip arthroplasty. J Bone Joint Surg Am 2009; 91(Suppl. 6): 107-20. doi: 10.2106/JBJS.I.00525.
- Aro H T, Alm J J, Moritz N, Mäkinen T J, Lankinen P. Low BMD affects initial stability and delays stem osseointegration in cementless total hip arthroplasty in women: a 2-year RSA study of 39 patients. Acta Orthop 2012; 83(2): 107-14. doi: 10.3109/17453674.2012.678798.
- Kleerekoper M. Primer on the metabolic bone diseases and disorders of mineral metabolism. 8th ed. Hoboken, NJ: Wiley-Blackwell; 2013. p: 1077.
- Ranstam J, Ryd L, Onsten I. Accurate accuracy assessment: review of basic principles. Acta Orthop Scand 2000; 71(1): 106-8. doi: 10.1080/00016470052944017.
- van der Voort P, Pijls B G, Nieuwenhuijse M J, Jasper J, Fiocco M, Plevier J W, et al. Early subsidence of shape-closed hip arthroplasty stems is associated with late revision: a systematic review and meta-analysis of 24 RSA studies and 56 survival studies. Acta Orthop 2015; 86(5): 575-85. doi: 10.3109/17453674.2015.1043832.
- Weber E, Flivik C, Sundberg M, Flivik G. Migration pattern of a short uncemented stem with or without collar: a randomised RSA-study with 2 years follow-up. Hip Int 2021; 31(4): 500-6. doi: 10.1177/1120700019888471.
- Polus J S, Perelgut M E, Vasarhelyi E M, Teeter M G, Lanting B A. Femoral stem migration after direct lateral and direct anterior total hip arthroplasty: a prospective cohort study. Can J Surg 2022; 65(4): E487-e95. doi: 10.1503/cjs.013221.
- Migliorini F, Eschweiler J, Trivellas A, Rath B, Driessen A, Tingart M, et al. Implant positioning among the surgical approaches for total hip arthroplasty: a Bayesian network meta-analysis. Arch Orthop Trauma Surg 2020; 140(8): 1115-24. doi: 10.1007/s00402-020-03448-w.
- Mattesi L, Cheyrou-Lagrèze A, Odri G A, Duhil A, Flurin L, Severyns M. Does the surgical approach influence the canal fill of the proximal femur for hip arthroplasty? Arthroplast Today 2021; 10: 166-70. doi: 10.1016/j.artd.2021.05.011.
- Rivera F, Leonardi F, Evangelista A, Pierannunzii L. Risk of stem undersizing with direct anterior approach for total hip arthroplasty. Hip Int 2016; 26(3): 249-53. doi: 10.5301/hipint.5000337.
- Derbyshire B, Prescott R J, Porter M L. Notes on the use and interpretation of radiostereometric analysis. Acta Orthop 2009; 80(1): 124-30. doi: 10.1080/17453670902807474.