Fracture pattern and risk factors for reoperation after treatment of 156 periprosthetic fractures around an anatomic cemented hip stem
Ali SATTAR 1, Johan KÄRRHOLM 2-4, Michael MÖLLER 3,4, and Georgios CHATZIAGOROU 3
1 Department of Orthopaedics, Alingsås Hospital, Alingsås; 2 The Swedish Arthroplasty Register, Gothenburg; 3 Department of Orthopaedics, Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Gothenburg; 4 Department of Orthopaedics, Sahlgrenska University Hospital, Gothenburg/Mölndal, Sweden
Background and purpose — The Lubinus SP2 stem has been associated with a very low risk of periprosthetic femoral fractures (PPFFs). We aimed, primarily, to study the radiographic morphology of PPFFs close to a Lubinus SP2 stem. Secondarily, we analyzed whether higher reoperation rate was correlated to the revision method chosen or to the characteristics of the fracture and of the bone.
Patients and methods — The study included 156 femoral fractures close to a Lubinus cemented stem. These fractures were treated in 40 hospitals in Sweden between 2006 and 2011 and were followed up until 2019. Data from the Swedish Arthroplasty Register was used. Medical records and radiographs were studied. The fractures were classified according to the Vancouver classification. The fracture location and anatomy were delineated. We also measured the remaining attachment index (RAI) and the canal thickness ratio.
Results — Vancouver type C (n = 101) and spiral fractures (n = 67, 41 in Vancouver C and 26 in Vancouver B) were the most common fracture types. 4 fractures were avulsion of the greater trochanter. The remaining 51 fractures occurred around the stem (B1: 25, B2: 16, and B3: 10). B fractures were more commonly reoperated on (18 of 51, 35%) than type C fractures (11 of 101, 11%, P = 0.001). In most femurs with type B3 fracture, the fracture line covered an area only around the stem, but in all B1 and in 11 of 16 B2 fractures, it was extended even distal to the stem. ORIF instead of stem revision in B2 fractures, use of short stems or plates, and inadequate reduction of the fractures were risk factors for subsequent reoperations.
Conclusion — The higher reoperation rate in type B fractures, compared with fractures distal to the stem, could be caused by their higher degree of complexity and reduced capacity for healing in the region around the stem.
Citation: Acta Orthopaedica 2023; 94: 438–446. DOI: https://doi.org/10.2340/17453674.2023.18263.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-08-24. Accepted: 2023-06-29. Published: 2023-08-16.
Correspondence: ali.sattar@hotmail.com
All authors contributed to planning of the research, collection of the material, analysis of the material, and writing the manuscript.
Handling co-editors: Søren Overgaard and Robin Christensen
Acta thanks Geir Hallan and Chloe Scott for help with peer review of this manuscript.
Periprosthetic femoral fracture (PPFF) has the highest mortality rate and is among the 4 most common complications after total hip replacement (THR) surgery in Sweden [1]. The incidence of this complication is increasing and the number of periprosthetic fractures is expected to rise over the coming decades [2,3]. Therefore, much research on risk factors has been performed to facilitate prevention of this complication. Uncemented fixation of the femoral stem is one of the most commonly reported risk factors [2,4], and several studies around the world have suggested cemented fixation for specific patient categories [5]. Cemented stems have predominated in primary THRs in Sweden. The most commonly used design is the anatomical Lubinus SP2 (Waldermar LINK GmbH & Co. KG, Germany) [6]. This femoral component is reported to have the lowest risk of postoperative PPFFs, even in comparison with other cemented designs [2,7]. In comparison with a considerably large number of publications regarding the fracture pattern of cemented stems with force-closed design [8-10], little is known about fractures around anatomical cemented stems. We aimed primarily, to study the radiological morphology of PPFFs close to a Lubinus SP2 stem. Secondarily, we analyzed whether higher reoperation rate was correlated to the surgical method chosen or to the characteristics of the fracture and of the bone.
Patients and methods
Data collection and exclusion criteria
We investigated Lubinus SP2 stems reoperated on in Sweden between 2006 and 2011 due to PPFF. This period was chosen because of availability of digital radiographs. To collect all PPFFs, matching was done between 2 national registers, the former Swedish Hip Arthroplasty Register (SHAR, since 2021 the Swedish Arthroplasty Register, SAR) and the National Patient Register (NPR). Reporting to the NPR has been obligatory since 2001 for both private and public healthcare providers. This register started in 1964 and holds information on all inpatient care since 1987 and all outpatient care since 2001. The registration of PPFF in the NPR is expected to approach 100%. The matching of data between the SHAR and the NPR is discussed in detail in a previous publication [3]. In this previously published study we reported 351 PPFFs close to a primary Lubinus SP2 femoral stem occurring between 2001 and 2011. Excluded were intraoperative fractures, pathological and iatrogenic fractures, and cases with active deep infection. From these 351 fractures, 234 had occurred during 2006–2011.
All medical records were collected and scrutinized to enable exclusion of incorrect recordings and duplicates. The SHAR started to register primary hip replacements prospectively in 1992 and therefore only Lubinus stems inserted after 1991 were included. To minimize factors that could predispose to PPFF or influence the type of fracture, 8 cases were excluded due to specific diagnosis at the time of primary THR (Figure 1). 60 PPFFs were excluded due to the presence of a total knee replacement (TKR). This is a risk factor both for a PPFF close to a hip prosthesis [11], and for higher reoperation rates after the treatment of PPFFs [12]. Information on the presence of an ipsilateral TKR was derived from both medical records and data linkage between the former SHAR and the former Swedish Knee Arthroplasty Register (SKAR) [12]. These 2 registers are now included in SAR. The exclusions above resulted in 166 cases from a total of 41 hospitals. Pre- and postoperative radiographs were acquired from 40 radiological departments (165 cases), while 1 department did not reply (1 case). 9 cases were further excluded after reviewing radiographs of the 165 PPFFs for various reasons accounted for in Figure 1. Thus, 156 femoral fractures close to a primary Lubinus SP2 stem were analyzed. All fractures were followed up until 2019, death, or further reoperation. Reoperation was defined as any type of operation in the femur following the PPFF, irrespective of whether the prosthesis or parts of it remained untouched or not.
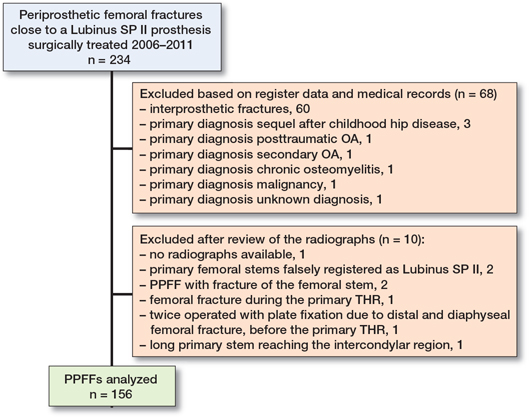
Figure 1. Exclusion criteria and the number of cases analyzed in this study. Abbreviations: PPFF = periprosthetic femoral fracture, OA = osteoarthritis, THR = total hip replacement.
Variables
Fractures were divided into proximal, diaphyseal, and distal, depending on the anatomical position of the center of the fracture line (Figure 2). The fracture pattern was noted (transverse, oblique, spiral, comminuted, and presence of an intermediate fragment) and all fractures were classified according to the Vancouver classification and the United Classification System (UCS) [13,14]. The Vancouver classification was assessed independently by 3 authors (AS, GC, JK) and consensus was obtained. In 5 cases, where the classification was uncertain, review of the medical records was done. Vancouver type C fractures were defined as fractures distal to the tip of the stem, irrespective of how close the proximal end of the fracture line was in relation to the tip of the stem or the cement mantle.
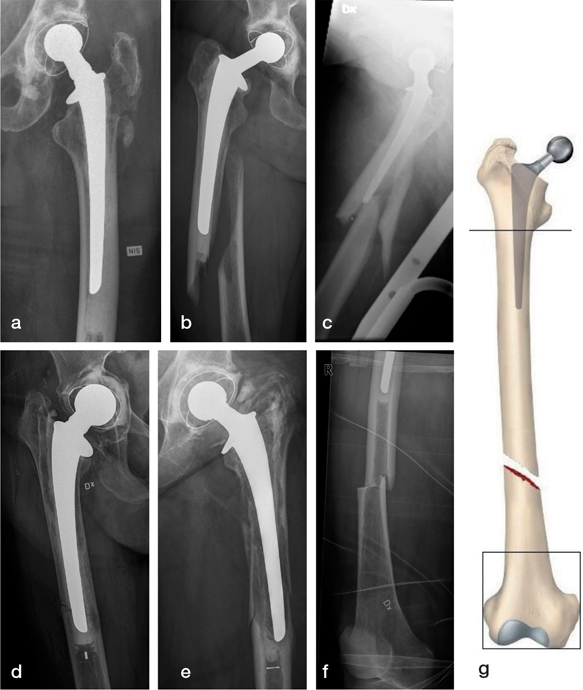
Figure 2. Preoperative radiographs showing fracture patterns and fracture types according to the Vancouver classification: (a) oblique Vancouver A, (b) spiral Vancouver B1, (c) B1 with intermediate fragment, (d) oblique Vancouver B2 with osteolysis, (e) comminuted Vancouver B3 with osteolysis, (f) transverse Vancouver C. Diaphyseal fractures had the center of the fracture line between the lesser trochanter proximally, and the proximal line of a square formed from the femoral condyle, distally (g).
Furthermore, the following variables were studied: (i) the interspace (distance) between the tip of the stem and the proximal end of the fracture in Vancouver type C fractures; (ii) the canal thickness ratio (CTR, Figure 3) [9], and (iii) the remaining attachment index (RAI, Figure 4) [15]. The CTR, defined as the ratio of the total width of both cortices to the whole diameter of the femur (in AP projection), was measured at a distance of 1 femoral width distal to the tip of the stem. Thus, femurs with thicker cortices have a higher CTR than those with thinner cortices. The ratio between the length of the proximal femoral fragment that surrounds the femoral stem and the total stem length has been previously described as remaining attachment index (RAI) or as “index de fixation restante (IFR)” [16]. A higher RAI indicates a shorter area of the stem surrounded by the fracture line. The RAI was calculated only in type B fractures, while the CTR was calculated in all fractures where radiographs including the tip of the stem were available. Calibration of the radiographs was not possible in all cases, because of absence of calibration sphere in cases with type C fractures and in several B fractures with pelvis projections. Therefore, the femoral width at the tip of the stem was used as the unit for measuring the distance between the tip of the stem and the fracture. All measurements were performed on DICOM files.
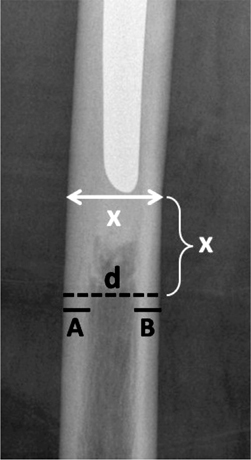
Figure 3. The canal thickness ratio (CTR) was measured one femoral width (x) distal to the tip of the stem. CTR is the ratio of the total cortical width (A+B) to the whole diameter of the femur (d), CTR = (A+B)/d.
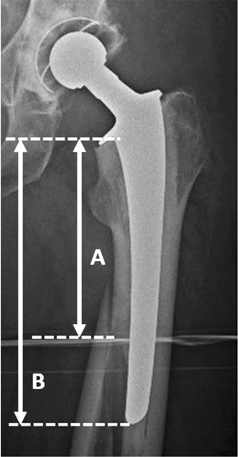
Figure 4. The remaining attachment index (RAI) is the ratio of the proximal femoral fragment that surrounds the femoral stem (A) to the total stem length (B), RAI = A/B.
Demographic information regarding age, sex, date of primary THR and PPFF, diagnosis at primary THR, and date of death were derived from the SAR. Details regarding the surgical treatment were extracted from both the medical records and the postoperative radiographs. Information on the type of the primary and revision stems was registered in the SAR and controlled during the review of the radiographs.
Statistics
Statistical analysis was conducted using SPSS version 25 (IBM Corp, Armonk, NY, USA). Comparisons between median values were done with the Mann–Whitney test. Fisher’s exact test was performed to compare categorical variables. To investigate the correlation between 2 variables, Spearman’s correlation coefficient was used. P values were 2-sided with a significance level < 0.05, and 95% confidence intervals (CI) were calculated. The risk of further reoperation after surgical treatment of either type B or type C fracture was studied in a Cox regression model adjusted for age and sex. Our study followed the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) checklist.
Ethics, funding, and disclosures
The study was approved by the Central Ethical Review Board in Gothenburg (entry number: 198-12, date: 2012-04-05). The study was partially supported financially by the Felix Neubergh’s Foundation. The authors declare no conflict of interest. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.18263
Results
156 fractures in 154 patients were analyzed. 2 patients were operated on bilaterally for fractures that occurred on different occasions. Demographic characteristics and Vancouver classification of all PPFFs are given in Table 1. Approximately 2/3 of all fractures occurred distal to the tip of the stem, and 29 fractures (19%) were reoperated on at least once. At the end of 2019, 109 of 156 patients (70%) had died.
| Female sex, n (%) | 112 (72) |
| Left side, n (%) | 72 (46) |
| Mean age, years (SD) | |
| At primary THR | 72 (10.2) |
| At PPFF | 79 (10.3) |
| At death | 86 (8.3) |
| Diagnosis at primary THR, n (%) | |
| Primary osteoarthritis | 99 (63) |
| Hip fracture | 39 (25) |
| Femoral head necrosis | 9 (5.8) |
| Inflammatory arthritis | 9 (5.8) |
| Vancouver classification of fractures: | |
| cases treated with ORIF only / all cases | |
| Vancouver A a | 3 / 4 |
| Vancouver B1 | 23 / 25 |
| Vancouver B2 | 6 / 16 |
| Vancouver B3 | 0 / 10 |
| Vancouver C | 99 / 101 |
| a All type A fractures were avulsion of the greater trochanter. | |
Fracture pattern and fracture localization
The most common fracture pattern in both type B and type C fractures was spiral (26 of 51 and 41 of 101, respectively). The length of the fracture line in 1 B3 fracture could not be fully recorded on plain radiographs but was documented in the medical record. Spiral fractures were commonly seen around the tip of the stem (Table 2), whereas comminuted fractures were most common in distal type C fractures (> 2 femoral widths distal to the stem tip). Most B fractures (39 of 51) continued distal to the tip of the stem (Table 2), including all B1 and 11 B2 fractures. 7 of 10 B3 fractures were located only around the stem. No correlation was found between the fracture pattern and the reoperation rate.
| Factor | Spiral | Oblique | Transverse | Comminute | Intermediary fragment | Total |
| Vancouver B | ||||||
| Fracture line ends in relation to the stem tip | ||||||
| proximal to it | 4 | 3 | 3 | 1 | 0 | 11 |
| distal to it | 22 | 2 | 3 | 9 | 3 | 39 |
| Vancouver C | ||||||
| Interspace measured in femoral widths b | ||||||
| < 2 | 22 | 1 | 3 | 5 | 1 | 32 |
| ≥ 2 | 19 | 5 | 4 | 38 | 3 | 69 |
| a The fracture line in 1 B3 fracture could not be fully recorded on plain radiographs. Therefore, 50 B fractures are reported in this table. b Distance between the stem tip and the proximal end of the fracture. |
||||||
Canal thickness ratio (CTR)
The CTR could be measured in 50 type B and 96 type C fractures. In 1 B1 and 5 C fractures, the CTR could not be computed due to inadequate radiographs. There was no significant difference in the CTR between Vancouver B and Vancouver C fractures (mean difference –0.01, CI –0.04 to 0.03, P = 0.7). A lower CTR was noted with increasing age (Pearson correlation –0.19, CI –0.34 to –0.03, P = 0.02). Women had a statistically significant lower CTR (median 0.40, interquartile range [IQR] 0.17) in comparison with men (median 0.47, IQR 0.16, P = 0.002). In type B fractures, a lower CTR was correlated with a lower reoperation rate (Table 3, Spearman’s correlation coefficient 0.29, CI 0.005 to 0.53, P = 0.04). No correlation was noted between CTR and reoperation rate in Vancouver C fractures (Spearman’s correlation coefficient –0.08, CI –0.28 to 0.13, P = 0.5).
| Factor | n | Median CTR (IQR) | P value |
| Vancouver B | |||
| Reoperated | 18 | 0.47 (0.13) | 0.04 |
| Not reoperated | 32 | 0.35 (0.21) | |
| Vancouver C | |||
| Reoperated | 10 | 0.37 (0.30) | 0.5 |
| Not reoperated | 86 | 0.40 (0.14) | |
| a CTR could not be computed in 1 B1 and 5 C fractures due to inadequate radiographs. | |||
Remaining attachment index (RAI)
RAI was registered both as a continuous and as a dichotomized (≤ 2/3 or > 2/3) variable. It could be computed in 49 of 51 Vancouver B fractures. In 1 B1 and 1 B3 fracture, it could not be calculated due to difficulty in identifying the proximal end of the fracture line. In the B1 fracture, the fracture line was described as reaching the lesser trochanter proximally and therefore this fracture was included as RAI ≤ 2/3. In 2 B fractures, the fracture line engaged only the intertrochanteric region, while in the other 49 it stayed distal to the lesser trochanter.
No correlation between the RAI and the reoperation rate was noted, either when only B fractures with plate fixation were analyzed, or when all B fractures irrespective of treatment method were studied. Within the subgroup of B1 fractures treated only with plate fixation (22 cases), those with RAI > 2/3 had a numerically higher reoperation rate (5 of 13 cases) than those with RAI ≤ 2/3 (2 of 9), but this difference did not reach statistical significance (Fisher’s exact test, OR 0.46, CI 0.07 to 3.14, P = 0.6). This finding was not altered when 6 cases of B2 fractures treated only with plate fixation were added into the analysis. 1 B1 fracture treated only with cerclage was excluded from this analysis.
Interspace between tip of stem and most proximal part of the fracture line in Type C fractures
The interspace (distance) between the tip of the stem and the most proximal part of the fracture was registered both as a continuous (95 cases) and as a dichotomized (all 101 cases, < 2 or ≥ 2 femoral widths) variable. It was not possible to measure the interspace in 6 cases (≥ 2 femoral widths), because the fractures were in the distal segment and the tip of the stem was not visible on the radiographs that reproduced the fracture region. Most of the 101 type C fractures were situated in the diaphyseal area (n = 66) and the majority had their proximal fracture end more than 2 femoral diameters from the tip of the stem (Table 2). 2 fractures were treated with stem revision.
Both had an interspace smaller than 1 femoral diameter, and none of them underwent reoperation. For the other 99 fractures treated with ORIF, no statistical difference in the reoperation rate was noticed when comparing PPFFs with interspace < 2 femoral widths (4 reoperations of 30 cases) with those with interspace ≥ 2 femoral widths (7 of 69, Fisher’s exact test, OR 0.7, CI 0.2 to 2.7, P = 0.7). No correlation was noted between interspace value and CTR as continuous variables (Spearman’s correlation coefficient –0.08, CI -0.29 to 0.13, P = 0.4). Distribution of the fracture pattern in relation to the interspace between the stem and the fracture is illustrated in Figure 5.
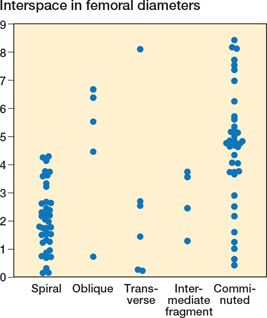
Figure 5. Vancouver type C fractures. Distribution of the fracture pattern in relation to the interspace between the tip of the stem and the most proximal end of the fracture.
Reoperations after surgical treatment of PPFFs
The median follow-up time between PPFF and reoperation, or death, or the end of 2019 was 3.7 years (range 11 days to 12.3 years). None of the 4 Vancouver type A fractures was reoperated on, while 18 type B fractures underwent at least 1 reoperation (35%) until 2019. This was statistically higher than the reoperation rate in type C fractures (11 cases, 11%, OR 0.2, CI 0.1 to 0.5, P < 0.001). In the regression model, adjusted for sex and age at the time of PPFF, patients with a type B fracture had a 3.1 times (CI 1.3 to 7) higher risk of reoperation compared with those who sustained a Vancouver C fracture (Table 4). As at the end of 2019, 33 patients with a type B fracture (67%) and 73 patients with a type C fracture (72%) had died (P = 0.4).
Each reoperation was studied in detail according to Tables 5 and 6 (see Appendix). In 10 type B fractures subsequently reoperated on, ORIF rather than stem revision had been chosen to treat fractures close to a loose stem, the plate or revision stem used was relatively short, or the fracture reduction or fixation was poor. 2 patients were reoperated on due to deep infection (11%).
In type C fractures that underwent reoperation, poor reduction of the PPFF was noted in 3 cases, and in 2 cases too long a screw was reported to cause pain. Other reasons were short plates, an intramedullary nail protruding into the knee joint, and short interspace between the intramedullary nail and the tip of the stem. 2 patients were reoperated on due to deep infection (18%). Examples of 2 fractures that went through a reoperation are illustrated in Figure 6. The number of reoperations in relation to Vancouver category and method of surgical treatment are presented in Table 7.

Figure 6. Cases with complication after treatment for PPFF. a–b. Vancouver type B2 with osteolysis treated with fixation using a conventional plate. The stem was revised 9 months later due to loosening. c–d. Vancouver type C treated with an intramedullary nail. The distal part of the nail protruded into the knee joint, and the patient was reoperated on 5 months later when the nail was changed to a shorter one.
Discussion
We aimed primarily to study the radiological morphology of PPFFs close to a Lubinus SP2 stem. Secondarily, we analyzed whether higher reoperation rate was correlated to the surgical method chosen or to the characteristics of the fracture and of the bone. To our knowledge, no other study has previously described the fracture pattern around the Lubinus SP2 femoral stem. We showed that the Vancouver type C fracture was the most common fracture type and the spiral fracture pattern was the most common pattern in fractures both around (Vancouver B) and distal to (Vancouver C) the cemented stem. The CTR was related to age and sex, while the RAI showed no correlation to the variables investigated in this study. The distance between the tip of the stem and the most proximal part of a type C fracture seemed not to be a predictor for higher reoperation rates. Vancouver type B fractures had a 3 times higher risk for reoperation than type C fractures.
The spiral fracture pattern has been reported as the most common pattern in cemented stems with force-closed design, both in the laboratory [8,17], and in clinical studies [18,19]. The Lubinus SP2 stem is an anatomical stem and belongs to the category of shape-closed design or composite beam. The higher share of Vancouver type C fractures (65%) can probably be explained by 3 factors: (a) the higher completeness of registered type C fractures as a result of matched data between 2 national registries [3], (b) the higher share of these fractures in Lubinus stems [7,20], and (c) fractures distal to the tip of the stem but close to it were defined as type C and not as type B. This definition was chosen in order to have a distinct criterion that would be easy to follow and would result in higher inter- and intra-observer agreement. Maybe the most characteristic feature in B fractures, in our material, was that the fracture line was mainly located distal to the lesser trochanter with only 2 exceptions.
CTR was measured 1 femoral width distal to the femoral stem in our study. This is the region for load transmission between the implant bone composite and the native bone. The interest of this study was focused on the bone-stock quality at the time of the PPFF and not at the time of the primary THR. A low CTR indicates a femur with thin cortex and is associated with osteoporosis and with a higher incidence of periprosthetic fractures [21,22], which was supported by our study in women with a high expected incidence of osteoporotic bone. The CTR was not different between type C and type B fractures around the Lubinus stem. This was in contrast to a study of PPFFs close to Exeter stems (force-closed design), where the CTR was significantly lower in Vancouver type C fractures compared with B fractures [19]. Our hypothesis that a lower CTR would be associated with a higher reoperation rate was not confirmed in the treatment of type B fractures. On the contrary, patients with a lower CTR had a lower reoperation rate compared with those with a higher CTR. In a recent study, increasing cortical thickness was related to a higher risk of Vancouver type B fractures [23].
In some cases with type B fractures, it is difficult to decide whether ORIF or stem revision is the optimal treatment. 2 previous studies reported better results with plate fixation of B1 fractures around uncemented stems when the remaining attachment index (RAI) was higher than 2/3, compared with cases with RAI ≤ 2/3 [15,16]. This finding was not confirmed in our material, perhaps because we studied only one specific cemented stem belonging to the shape-closed design. Our findings may not be of relevance when other types of cemented stems are used and especially not when force-closed stems are used.
Several studies found no association between the classification of the fracture and the outcome of the surgical treatment [24-26]. Our fracture cohort was more homogeneous as all patients had the same type of primary stem. A higher reoperation rate after treatment of type B fractures in comparison with type C fractures was noted. This is probably secondary to the fact that the treatment of a fracture around an anatomical cemented stem is more complex than that of a fracture distal to it. Finally, most of the PPFF that underwent reoperation had previously been operated on with a shorter plate or stem, with ORIF instead of prosthetic revision, or with poor reduction of the fracture (see Tables 4 and 5). On the other hand, we cannot with certainty claim that these conditions are risk factors as we did not analyze in depth the cases that did not undergo reoperation.
Limitations
We did not have the possibility to calibrate the radiographs and therefore no absolute distances were reported. However, the use of “1 femoral width” as a measurement unit and the analysis only of ratio decreased the risk of bias. An interobserver evaluation of the fracture classification was not performed. This has been done previously involving 3 orthopedic surgeons, 2 of whom classified the fractures in this study [3].
Conclusion
Vancouver type C and spiral fractures were the most common fractures around a primary Lubinus SP2 cemented femoral stem. The 3 times higher reoperation rate in type B fractures, compared with type C, could be caused by their higher degree of complexity causing more technical errors and also their reduced capacity for healing. Two-thirds (19 out of 29) of all reoperations after surgical treatment of PPFF were related to technical errors and might have been avoided if the general principles of fracture fixation and periprosthetic fracture treatment had been followed.
- Cnudde P, Bulow E, Nemes S, Tyson Y, Mohaddes M, Rolfson O. Association between patient survival following reoperation after total hip replacement and the reason for reoperation: an analysis of 9,926 patients in the Swedish Hip Arthroplasty Register. Acta Orthop 2019; 90(3): 226-30. doi: 10.1080/17453674.2019.1597062.
- Thien T M, Chatziagorou G, Garellick G, Furnes O, Havelin L I, Mäkelä K, et al. Periprosthetic femoral fracture within two years after total hip replacement: analysis of 437,629 operations in the nordic arthroplasty register association database. J Bone Joint Surg Am 2014; 96(19): e167. doi: 10.2106/JBJS.M.00643.
- Chatziagorou G, Lindahl H, Garellick G, Kärrholm J. Incidence and demographics of 1751 surgically treated periprosthetic femoral fractures around a primary hip prosthesis. Hip Int 2019; 29(3): 282-8. doi: 10.1177/1120700018779558.
- Abdel M P, Watts C D, Houdek M T, Lewallen D G, Berry D J. Epidemiology of periprosthetic fracture of the femur in 32 644 primary total hip arthroplasties: a 40-year experience. Bone Joint J 2016; 98-b(4): 461-7. doi: 10.1302/0301-620x.98b4.37201.
- Lindberg-Larsen M, Petersen P B, Jørgensen C C, Overgaard S, Kehlet H. Postoperative 30-day complications after cemented/hybrid versus cementless total hip arthroplasty in osteoarthritis patients > 70 years. Acta Orthop 2020; 91(3): 286-92. doi: 10.1080/17453674.2020.1745420.
- SHAR. Svenska Höftprotesregistret. Årsrapport 2019; 2020. https://registercentrum.blob.core.windows.net/slr/r/2019-B1xpWMUSPO.pdf
- Chatziagorou G, Lindahl H, Kärrholm J. The design of the cemented stem influences the risk of Vancouver type B fractures, but not of type C: an analysis of 82,837 Lubinus SPII and Exeter Polished stems. Acta Orthop 2019; 90(2): 135-42. doi: 10.1080/17453674.2019.1574387.
- Erhardt J B, Khoo P P, Stoffel K K, Yates P J. Periprosthetic fractures around polished collarless cemented stems: the effect of stem design on fracture pattern. Hip Int 2013; 23(5): 459-64. doi: 10.5301/hipint.5000052.
- Leonidou A, Moazen M, Skrzypiec D M, Graham S M, Pagkalos J, Tsiridis E. Evaluation of fracture topography and bone quality in periprosthetic femoral fractures: a preliminary radiographic study of consecutive clinical data. Injury 2013; 44(12): 1799-804. doi: 10.1016/j.injury.2013.08.010.
- Powell-Bowns M F R, Oag E, Martin D, Clement N D, Scott C E H. Vancouver B and C periprosthetic fractures around the cemented Exeter Stem: sex is associated with fracture pattern. Arch Orthop Trauma Surg 2022; 142(11): 3221-8. doi: 10.1007/s00402-021-04113-6.
- Katz J N, Wright E A, Polaris J J, Harris M B, Losina E. Prevalence and risk factors for periprosthetic fracture in older recipients of total hip replacement: a cohort study. BMC Musculoskelet Disord 2014; 15: 168. doi: 10.1186/1471-2474-15-168.
- Chatziagorou G, Lindahl H, Kärrholm J. Surgical treatment of Vancouver type B periprosthetic femoral fractures: patient characteristics and outcomes of 1381 fractures treated in Sweden between 2001 and 2011. Bone Joint J 2019; 101-b(11): 1447-58. doi: 10.1302/0301-620x.101b11.bjj-2019-0480.r2.
- Duncan C P, Masri B A. Fractures of the femur after hip replacement. Instr Course Lect 1995; 44: 293-304. PMID: 7797866
- Duncan C P, Haddad F S. Unified Classification System (UCS). Periprosthetic Fracture Management: Thieme; 2013. pp 47-57.
- Andriamananaivo T, Odri G A, Ollivier M, Mattesi L, Renault A, Rongieras F, et al. Contribution of the remaining attachment index in the management of Vancouver B1 periprosthetic hip fracture. Orthop Traumatol Surg Res 2020; 106(7): 1413-17. doi: 10.1016/j.otsr.2020.06.016.
- Molina V, Da S C, Court C, Nordin J Y. [Periprosthetic fractures around total hip and knee arthroplasty. Periprosthetic femoral fractures: multicentric retrospective study of 580 cases]. Rev Chir Orthop Reparatrice Appar Mot 2006; 92(5 Suppl.): 2s60-2s4. PMID: 17802658.
- Morishima T, Ginsel B L, Choy G G, Wilson L J, Whitehouse S L, Crawford R W. Periprosthetic fracture torque for short versus standard cemented hip stems: an experimental in vitro study. J Arthroplasty 2014; 29(5): 1067-71. doi: 10.1016/j.arth.2013.10.016.
- Grammatopoulos G, Pandit H, Kambouroglou G, Deakin M, Gundle R, McLardy-Smith P, et al. A unique peri-prosthetic fracture pattern in well fixed femoral stems with polished, tapered, collarless design of total hip replacement. Injury 2011; 42(11): 1271-6. doi: 10.1016/j.injury.2011.01.008.
- Powell-Bowns M F R, Oag E, Martin D, Clement N D, Scott C E H. Vancouver B and C periprosthetic fractures around the cemented Exeter stem: sex is associated with fracture pattern. Arch Orthop Trauma Surg 2022; 142(11): 3221-8. doi: 10.1007/s00402-021-04113-6.
- Löwenhielm G, Hansson L I, Kärrholm J. Fracture of the lower extremity after total hip replacement. Arch Orthop Trauma Surg 1989; 108(3): 141-3. doi: 10.1007/BF00934256
- Sah A P, Thornhill T S, LeBoff M S, Glowacki J. Correlation of plain radiographic indices of the hip with quantitative bone mineral density. Osteoporos Int 2007; 18(8): 1119-26. doi: 10.1007/s00198-007-0348-6.
- Gromov K, Bersang A, Nielsen C S, Kallemose T, Husted H, Troelsen A. Risk factors for post-operative periprosthetic fractures following primary total hip arthroplasty with a proximally coated double-tapered cementless femoral component. Bone Joint J 2017; 99-b(4): 451-7. doi: 10.1302/0301-620x.99b4.bjj-2016-0266.r2.
- Stevens J, Clement N, Nasserallah M, Millar M, Joseph S. Femoral cortical thickness influences the pattern of proximal femoral periprosthetic fractures with a cemented stem. Eur J Orthop Surg Traumatol 2018; 28(4): 659-65. doi: 10.1007/s00590-018-2141-y.
- Fuchtmeier B, Galler M, Muller F. Mid-term results of 121 periprosthetic femoral fractures: increased failure and mortality within but not after one postoperative year. J Arthroplasty 2015; 30(4): 669-74. doi: 10.1016/j.arth.2014.11.006.
- Kinov P, Volpin G, Sevi R, Tanchev P P, Antonov B, Hakim G. Surgical treatment of periprosthetic femoral fractures following hip arthroplasty: our institutional experience. Injury 2015; 46(10): 1945-50. doi: 10.1016/j.injury.2015.06.017.
- Drew J M, Griffin W L, Odum S M, Van Doren B, Weston B T, Stryker L S. Survivorship after periprosthetic femur fracture: factors affecting outcome. J Arthroplasty 2016; 31(6): 1283-8. doi: 10.1016/j.arth.2015.11.038.