Revision risk of salvage compared with acute total hip arthroplasty following femoral neck fracture: an analysis from the Dutch Arthroplasty Register
Peter P SCHMITZ 1, Gerjon HANNINK 2, Matthijs P SOMFORD 1, B Willem SCHREURS 3,4, and Job L C VAN SUSANTE 1
1 Rijnstate Hospital, Department of Orthopedics, Rijnstate Hospital, Arnhem; 2 Radboud University Medical Center, Department of Operating Rooms, Nijmegen; 3 Radboud University Medical Center, Department of Orthopedics, Nijmegen; 4 Dutch Arthroplasty Register (LROI), ‘s Hertogenbosch, The Netherlands
Background and purpose — There is no consensus on the treatment of patients with femoral neck fractures between internal fixation (IF) or directly treated with a total hip arthroplasty (fracture-THA) in particular for the age group 60–70 years. Failure of IF is not uncommon, resulting in salvage total hip arthroplasty (salvage-THA). The aim of our study was to compare revision rates of salvage-THA with fracture-THA and osteoarthritis (OA)-THA.
Patients and methods — Revision rates and reasons for revision were compared. Data collected in the Dutch Arthroplasty Register (LROI) between 2007 and 2018 was used. The study included 4,310 salvage-THAs, 12,159 fracture-THAs, and 274,147 OA-THAs. We performed Kaplan–Meier survival analyses and Cox regression to evaluate THA survival.
Results — No statistically significant difference in revision rates between salvage-THAs and fracture-THAs was found (HR 1.0, 95% CI 0.7–1.3) whereas the revision rate was higher compared with OA-THAs (HR 1.3, CI 1.0–1.5). The 5-year revision rate was 5.0% (CI 4.4–5.8) in salvage-THAs, 4.5% (CI 4.1–5.0) in fracture-THAs, and 3.1% (CI 3.0–3.2) in OA-THAs. A higher revision rate for infection was found in salvage-THAs in comparison with fracture-THAs (HR 1.6, CI 1.0–2.3).
Conclusion — We found no difference in revision rates for salvage-THAs compared with fracture-THAs. The risk of revision for infection was higher for salvage-THA.
Citation: Acta Orthopaedica 2022; 94: 399–403. DOI https://doi.org/10.2340/17453674.2023.17743.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2022-10-03. Accepted: 2023-05-30. Published: 2023-07-31.
Correspondence: PSchmitz@rijnstate.nl
PS and JvS designed the study; GH carried out data analyses; PS, GH, and JvS wrote the manuscript; PS, GH, MS, WS, and JvS contributed to revision of the manuscript.
Handling co-editors: Cecilia Rogmark and Philippe Wagner
Acta thanks Jan-Erik Gjertsen and Olof Leonardsson for help with peer review of this manuscript.
In general, elderly patients with a displaced femoral neck fracture are treated with (hemi)arthroplasty, whereas internal fixation of the fracture is mainly reserved for non-elderly patients in an attempt to preserve the hip joint. However, there is a lack of consensus in the literature concerning the best treatment in the age group 60–70 years [1]. Failure of internal fixation is not uncommon, even in the non-elderly (10–59%) [1-5]. Consequently, THA is still required after these failures, but now as a salvage procedure (salvage-THA). Internal fixation may negatively influence the outcome of these salvage-THAs, for example by higher complication rates such as infection [6]. However, literature is inconclusive regarding the results of salvage-THA.
A systematic review found a statistically significant higher risk of complications after salvage-THA compared with fracture-THA [7]. A retrospective study reported on the survival of a salvage-THA in comparison with a fracture-THA and found a higher risk of revision after salvage-THA [8]. On the other hand, a study from the Swedish Hip Arthroplasty Register found a similar revision rate for both groups [9].
If there is a higher risk of revision of salvage-THA in comparison with fracture-THA, it needs to be weighed against any benefits of preserving the hip joint by internal fixation of the fracture. Consequently, this information can be used in shared decision-making to choose between fracture-THA or internal fixation. A study based on national registers offers possibilities other than single or multicenter studies to monitor revision rates in salvage-THA versus fracture-THA.
The aim of our study was to determine the revision rates of salvage-THAs after failed internal fixation in comparison with fracture-THAs and OA-THAs. Furthermore, we compared the 3 most common reasons for revision in these groups.
Patients and methods
The LROI is a nationwide population-based register, covering all hospitals in the Netherlands, collecting data on arthroplasties. The database has a completeness of 98% for primary THA, 88% for hip revision arthroplasty to 2018 [10], and 98% for both primary and revision THA from 2018 [11]. In 2007, the LROI started to collect data prospectively on patient, procedure, and prosthesis characteristics. Earlier ipsilateral hip interventions such as internal fixation, arthroscopy, arthrodesis, osteotomy, and Girdlestone resection were registered as well. In mid-2013, body mass index, smoking behavior, and Charnley score were added to the database [10].
We included all registered patients who were treated with THA in the Netherlands between January 2007 and December 2018. Patients with any previous operation on the affected hip other than internal fixation of a femoral neck fracture were excluded. Based on indication and the history of the affected hip, 3 groups were distinguished: (1) THA as a salvage procedure for a failed previous internal fixation (salvage-THA), (2) THA as a direct treatment for a femoral neck fracture (fracture-THA), and (3) THA for primary osteoarthritis (OATHA).
Revision arthroplasty was defined as any change, addition, or removal of at least 1 component of the prosthesis [10]. In the LROI more than 1 cause of revision could be registered. Therefore, a hierarchical order of reasons for revision was used, i.e., infection, aseptic loosening, periprosthetic fracture, dislocation, and other [12]. The study is reported according to the STROBE guidelines [13].
Statistics
Kaplan–Meier survival analyses were performed to evaluate revision rates of the implants in all 3 groups. Results of Kaplan–Meier analyses (KM) were reported with 95% confidence intervals (CI). The median follow-up time and interquartile range (IQR) was calculated using the reversed Kaplan–Meier method [14]. The proportional hazard (PH) assumption was assessed through visual assessment of KM curves, log(−log) plots and testing of scaled Schoenfeld residuals. As the PH assumption was violated, we used weighted Cox regression as described in detail by Dunkler (2018) and Schemper (2009) [15,16] to compare revision rates in the 3 groups adjusted for age, sex, American Society of Anesthesiologists (ASA) score, approach (anterior, direct lateral, posterolateral, other), type of fixation (cemented, uncemented, hybrid), and implanted femoral head size. As missing values in potential confounders ranged between 0.2% and 6.6% and were assumed to be missing completely at random, listwise deletion (i.e., complete case analysis) was preferred to multiple imputation as biases and loss of power are both likely to be inconsequential [17]. Statistical analyses were performed using R (version 4.1.2, R Foundation for Statistical Computing, Vienna, Austria) with package “coxphw” (version 4.0.2; Dunkler 2018).
Ethics, funding, data sharing, and disclosures
Ethical approval was not applicable. Within the LROI data the personal identity number is encrypted; as such, all data received by the researchers were completely anonymous.
Data is available from the LROI but restrictions apply to the availability of this data, which was used under license for the current study. No funding was obtained, and the authors have no conflicts of interest to declare. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.17743
Results
Between January 2007 and December 2018, 4,310 salvage-THAs (4,174 patients), 12,159 fracture-THAs (11,750 patients), and 274,147 OA-THAs (273,692 patients) were registered (Figure 1). Mean age at time of primary operation was 67.7 (standard deviation [SD] 12.3) years, 70.2 (SD 9.4) years, and 69.7 (SD 9.5) years in these 3 groups, respectively. Median time of follow-up (IQR) was 4.8 (2.3–7.8) years for all patients, and 4.0 (1.9–6.4) years after salvage-THA, 3.5 (1.5–6.2) years after fracture-THA, and 4.9 (2.3–7.9) years after OA-THA. Patient and implant characteristics are listed in Table 1.
| Factor | Salvage-THA n = 4,310 | Fracture-THA n = 12,159 | OA-THA n = 274,147 |
| Age, mean (SD) | 67.7 (12.3) | 70.2 (9.4) | 69.8 (9.6) |
| Missing | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Sex | |||
| Male | 1,617 (38) | 3,782 (31) | 90,824 (33) |
| Female | 2,691 (62) | 8,356 (69) | 182,882 (67) |
| Missing | 2 (0.0) | 21 (0.2) | 441 (0.2) |
| ASA | |||
| 1 | 717 (17) | 1,767 (15) | 56,085 (21) |
| 2 | 2,479 (57) | 6,787 (56) | 17,1135 (62) |
| 3–4 | 1,071 (25) | 3,196 (26) | 39,669 (14) |
| Missing | 43 (1.0) | 409 (3.4) | 7,258 (2.6) |
| Charnley a,b | |||
| A | 1,678 (39) | 2,916 (24) | 65,399 (24) |
| B1 | 149 (3.5) | 387 (3.2) | 47,146 (17) |
| B2 | 143 (3.3) | 451 (3.7) | 34,763 (13) |
| C | 63 (1.5) | 158 (1.3) | 3,857 (1.4) |
| Missing | 2,277 (53) | 8,247 (68) | 122,982 (45) |
| BMIa, mean (SD) | 25.6 (4.3) | 25.0 (4.3) | 27.5 (4.5) |
| Missing | 1,422 (33) | 4,436 (36) | 11,3467 (41) |
| Smokinga | |||
| Yes | 555 (13) | 1,156 (9.5) | 16,000 (5.8) |
| No | 2,246 (52) | 6,638 (55) | 138,275 (50) |
| Missing | 1,509 (35) | 4,365 (36) | 119,872 (44) |
| Approach | |||
| Anterior | 247 (5.7) | 1,253 (10) | 48,077 (17) |
| Anterolateral | 253 (5.9) | 937 (7.7) | 17,840 (6.5) |
| Straight lateral | 892 (21) | 2,553 (21) | 46,357 (17) |
| Posterolateral | 2,899 (67) | 7,258 (60) | 158,287 (58) |
| Other | 12 (0.3) | 46 (0.4) | 1,364 (0.5) |
| Missing | 7 (0.2) | 112 (0.9) | 2,222 (0.8) |
| Fixation | |||
| Cemented | 1,626 (38) | 4,280 (35) | 72,441 (26) |
| Uncemented | 1,951 (45) | 6,277 (52) | 176,180 (64) |
| Hybrid | 703 (16) | 1,426 (12) | 23,297 (8.5) |
| Missing | 30 (0.7) | 176 (1.4) | 2,229 (0.8) |
| Femoral head size, mm | |||
| > 38 | 40 (0.9) | 592 (4.9) | 3,674 (1.3) |
| 36 | 632 (4.7) | 2,283 (19) | 51,284 (19) |
| 32 | 1,953 (45) | 4,946 (41) | 133,025 (48) |
| 22–28 | 1,401 (32) | 3,539 (29) | 70,811 (26) |
| Missing | 284 (6.6) | 799 (6.6) | 15,353 (5.6) |
| a BMI, smoking behavior, and Charnley score were registered since mid-2013. | |||
| b Charnley score is a 4-item clinical classification system: A: one joint affected; B1: both joints affected; B2: contralateral joint with a prosthesis; C: several joints affected or a chronic disease that affects quality of life. | |||
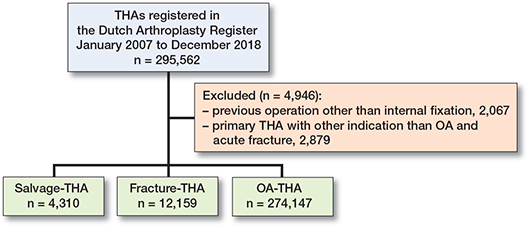
Figure 1. Flowchart patient selection.
Revision rates
The 5-year revision rates of the salvage-THAs were 5.0% (CI 4.4–5.8) and 6.8% (CI 5.7–8.2) after 10 years. The revision rates of the fracture-THAs were 4.5% (CI 4.1–5.0) at 5-year follow-up and 5.8% (CI 5.2–6.5) after 10 years. The OATHAs showed a revision rate of 3.1% (CI 3.0–3.2) after 5-year follow-up and 4.7% (CI 4.6–4.8) after 10 years (Figure 2).
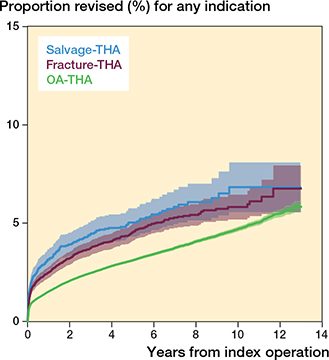
Figure 2. Crude analysis of Kaplan–Meier curves for revision with 95% confidence intervals in the 3 groups.
After adjustment for potential confounders, no statistical difference in revision rates between salvage-THAs and fracture-THAs was found (HR 1.0, CI 0.7–1.3). Both salvage-THAs and fracture-THAs showed a higher revision rate than OATHAs (HR 1.3, CI 1.0–1.5 and HR 1.3, CI 1.1–1.7, respectively). Unadjusted hazard ratios (CI) for revision among the 3 groups are presented in Table 2.
Reason for revision
The 3 most common reasons for revision were infection, dislocation, and aseptic loosening. Infection was the reason for revision in salvage-THAs, in the fracture-THAs, and in OATHAs in 1.2%, 0.6%, and 0.6%, dislocation in 1.2%, 1.4%, and 0.7%, and aseptic loosening in 1.0%, 1.0%, and 0.8%, respectively (Figure 3 and Table 3).
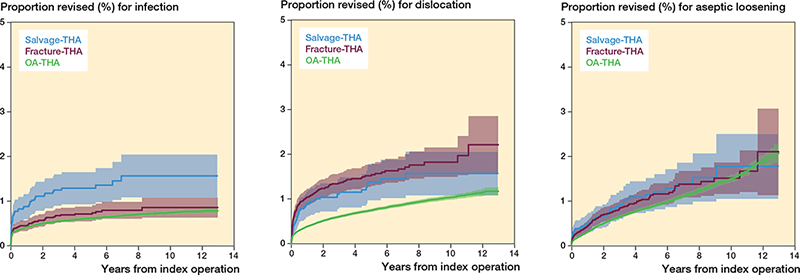
Figure 3. Crude analysis of Kaplan–Meier curves for reason for revision with 95% confidence intervals in the 3 groups.
After adjustment for potential confounders, a higher revision rate for infection was found in salvage-THAs than in fracture-THAs (HR 1.6, CI 1.0–2.3) and OA-THAs (HR 1.6, CI 1.2–2.2). The revision rate for dislocation was not different in salvage-THAs compared with fracture-THAs (HR 0.7, CI 0.4–1.1), whereas a higher revision rate for dislocation was found in both salvage-THAs (HR 1.5, CI 1.1–2.0) and fracture-THAs (HR 2.1, CI 1.5–3.0) than in OA-THAs. No differences were found in revision rates for aseptic loosening in salvage-THAs compared with fracture-THAs (HR 0.6, CI 0.3–1.3) and OA-THAs (HR 0.8, CI 0.5–2.1).
Discussion
This study found no certain difference in revision rate in salvage-THAs in comparison with fracture-THAs. The 5-year revision rate was 5.0% in salvage-THAs and 4.5% in fracture-THAs. Both groups had higher revision rates than OA-THAs. Notably, a higher revision rate for infection was found in salvage-THAs than in fracture-THAs.
Only a few studies report implant survival of salvage-THA in comparison with fracture-THA, and their results are inconclusive. Our findings are in accordance with a study from the Swedish Hip Arthroplasty Register where a subgroup analysis on the revision rate of salvage-THA and fracture-THA found a similar revision rate for these groups [9]. On the other hand, a retrospective cohort study comparing a group of 107 salvage-THAs with an age- and sex-matched group of 107 fracture-THAs found a significantly higher revision rate in the salvage-THA after 1, 5, and 10 years of follow-up [8]. The authors found complications in 36% of salvage-THAs and 13% complications after fracture-THAs. Functional outcome was significantly worse in the salvage-THA group. Furthermore, a systematic review consisting of 11 studies found a significantly higher risk of complications after salvage-THA in comparison with fracture-THA [7]. Lastly, a small study report found better hip function after fracture-THA compared with salvage-THA [18].
Several studies reported on the results of salvage-THA without the use of a direct comparison with fracture-THA. A large Norwegian register study found a higher revision rate in both salvage-THA and fracture-THA compared with OA-THA [19]. Salvage-THA had a higher revision rate due to dislocation and periprosthetic fracture. The revision rate for infection was similar after salvage-THA and OA-THA.
Prosthetic joint infection (PJI) was identified as the dominant reason for revision in the salvage-THA group in our study. A higher risk of PJI in THA after hardware removal has also been recognized in a retrospective case-series [6]. A higher risk of infection-related revision after salvage-THA (7%) in comparison with fracture-THA (2%) was also found by McKinley et al. [8]. It is well established that the risk for infection is increased by reoperations [20,21]. The latter probably explained the higher risk of infection-related revision after salvage-THA encountered in our study.
A higher risk of PJI after earlier internal fixation is important, as it may affect the clinical outcome of a THA [22]. As such, the doubled infection rate after a salvage-THA versus fracture-THAs (1.2% versus 0.6%), which was encountered in our registry-based study, is relevant. The knowledge that internal fixation may negatively influence the outcome of a potential future THA, as well as the finding of a similar total revision rate after both fracture-THA and salvage-THA, is important for clinical decision-making in treatment of femoral neck fracture. These findings are particularly relevant to the group aged 60–70 years, where no optimum treatment yet has been established [1,2].
Limitations and strengths
A strength of this registry study is the high number of fracturerelated THAs in comparison with the available literature. Some potential limitations must be discussed. First, the data on salvage-THAs is not detailed in terms of fracture type. Predominantly, a femoral neck fracture will have been the indication for a total hip arthroplasty, but inclusion of some trochanteric fractures cannot be ruled out. Second, information on BMI, smoking, and Charnley classification has only been registered in the LROI since 2013, preventing us from modelling these covariates in the period 2007 to 2013. However, a sensitivity analysis performed using complete data registered between 2014 and 2019 showed our results to be robust. Third, a Cox regression model was performed, adjusted for available covariates. Despite adjustment for covariates, confounding bias could play a role because differences in unmeasured covariates may still exist. Fourth, underestimation of septic loosening is a known problem as registration of infection is often not sufficient [23].
Conclusions
We found no difference in revision rates for salvage-THAs that are different from those in fracture-THAs. The risk of revision for infection was higher for salvage-THAs.
- Bhandari M, Devereaux P J, Tornetta P 3rd, Swiontkowski M F, Berry D J, Haidukewych G, et al. Operative management of displaced femoral neck fractures in elderly patients: an international survey. J Bone Joint Surg Am 2005; 87(9): 2122-30. doi:10.2106/jbjs.E.00535.
- Bartels S, Gjertsen J E, Frihagen F, Rogmark C, Utvåg S E. High failure rate after internal fixation and beneficial outcome after arthroplasty in treatment of displaced femoral neck fractures in patients between 55 and 70 years. Acta Orthop 2018; 89(1): 53-8. doi: 10.1080/17453674.2017.1376514.
- Rogmark C, Johnell O. Primary arthroplasty is better than internal fixation of displaced femoral neck fractures: a meta-analysis of 14 randomized studies with 2,289 patients. Acta Orthop 2006; 77(3): 359-67. doi: 10.1080/17453670610046262.
- Rogmark C, Kristensen M T, Viberg B, Rönnquist S S, Overgaard S, Palm H. Hip fractures in the non-elderly: who, why and whither? Injury 2018; 49(8): 1445-50. doi: 10.1016/j.injury.2018.06.028.
- Slobogean G P, Sprague S A, Scott T, Bhandari M. Complications following young femoral neck fractures. Injury 2015; 46(3): 484-91. doi: 10.1016/j.injury.2014.10.010.
- Scholten R, Füssenich W, Somford M P, van Susante J L C. High incidence of early periprosthetic joint infection following total hip arthroplasty with concomitant or previous hardware removal. Arch Orthop Trauma Surg 2019; 139(8): 1051-6. doi: 10.1007/s00402-019-03149-z.
- Mahmoud S S, Pearse E O, Smith T O, Hing C B. Outcomes of total hip arthroplasty, as a salvage procedure, following failed internal fixation of intracapsular fractures of the femoral neck: a systematic review and meta-analysis. Bone Joint J 2016; 98-b(4): 452-60. doi: 10.1302/0301-620x.98b4.36922.
- McKinley J C, Robinson C M. Treatment of displaced intracapsular hip fractures with total hip arthroplasty: comparison of primary arthroplasty with early salvage arthroplasty after failed internal fixation. J Bone Joint Surg Am 2002; 84(11): 2010-15. doi: 10.2106/00004623-200211000-00016.
- Leonardsson O, Rogmark C, Kärrholm J, Akesson K, Garellick G. Outcome after primary and secondary replacement for subcapital fracture of the hip in 10 264 patients. J Bone Joint Surg Br 2009; 91(5): 595-600. doi: 10.1302/0301-620x.91b5.22224.
- van Steenbergen L N, Denissen G A, Spooren A, van Rooden S M, van Oosterhout F J, Morrenhof J W, et al. More than 95% completeness of reported procedures in the population-based Dutch Arthroplasty Register. Acta Orthop 2015; 86(4): 498-505. doi: 10.3109/17453674.2015.1028307.
- LROI. Online LROI annual report 2018. http://www.lroirapportage.nl/media/pdf/PDF%20Online_LROI_annual_report_2018.pdf.
- Van Steenbergen L N, Mäkelä K T, Kärrholm J, Rolfson O, Overgaard S, Furnes O, et al. Total hip arthroplasties in the Dutch Arthroplasty Register (LROI) and the Nordic Arthroplasty Register Association (NARA): comparison of patient and procedure characteristics in 475,685 cases. Acta Orthop 2021; 92(1): 15-22. doi: 10.1080/17453674.2020.1843875.
- von Elm E, Altman D G, Egger M, Pocock S J, Gøtzsche P C, Vandenbroucke J P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008; 61(4): 344-9. doi: 10.1016/j.jclinepi.2007.11.008.
- Schemper M, Smith T L. A note on quantifying follow-up in studies of failure time. Control Clin Trials 1996; 17(4): 343-6. doi: 10.1016/0197-2456(96)00075-x.
- Dunkler D, Ploner M, Schemper M, Heinze G. Weighted Cox regression using the R Package coxphw. J Statistical Software 2018; 84(2): 1-26. doi: 10.18637/jss.v084.i02.
- Schemper M, Wakounig S, Heinze G. The estimation of average hazard ratios by weighted Cox regression. Stat Med 2009; 28(19): 2473-89. doi: 10.1002/sim.3623.
- Graham J W. Missing data analysis: making it work in the real world. Annu Rev Psychol 2009; 60: 549-76. doi: 10.1146/annurev.psych.58.110405.085530.
- Blomfeldt R, Törnkvist H, Ponzer S, Söderqvist A, Tidermark J. Displaced femoral neck fracture: comparison of primary total hip replacement with secondary replacement after failed internal fixation: a 2-year follow-up of 84 patients. Acta Orthop 2006; 77(4): 638-43. doi: 10.1080/17453670610012728.
- Gjertsen J E, Lie S A, Fevang J M, Havelin L I, Engesaeter L B, Vinje T, et al. Total hip replacement after femoral neck fractures in elderly patients: results of 8,577 fractures reported to the Norwegian Arthroplasty Register. Acta Orthop 2007; 78(4): 491-7. doi: 10.1080/17453670710014130.
- de Jong L, Klem T, Kuijper T M, Roukema G R. Factors affecting the rate of surgical site infection in patients after hemiarthroplasty of the hip following a fracture of the neck of the femur. Bone Joint J 2017; 99-b(8): 1088-94. doi: 10.1302/0301-620x.99b8.Bjj-2016-1119.R1.
- Dapunt U, Spranger O, Gantz S, Burckhardt I, Zimmermann S, Schmidmaier G, et al. Are atrophic long-bone nonunions associated with low-grade infections? Ther Clin Risk Manag 2015; 11: 1843-52. doi: 10.2147/tcrm.S91532.
- Kuijpers M F L, Hannink G, van Steenbergen L N, Schreurs B W. Outcome of revision hip arthroplasty in patients younger than 55 years: an analysis of 1,037 revisions in the Dutch Arthroplasty Register. Acta Orthop 2020; 91(2): 165-70. doi: 10.1080/17453674.2019.1708655.
- Kamp M C, Liu W Y, Goosen J H M, Rijnen W H C, van Steenbergen L N, van der Weegen W. Mismatch in capture of periprosthetic joint infections between the Dutch Arthroplasty Register (LROI) and a detailed regional periprosthetic joint infection registry. J Arthroplasty 2022; 37(1): 126-31. doi: 10.1016/j.arth.2021.09.001.