The extent of first-time THA revision is not associated with patient-reported outcomes at 1-year follow-up: a study of 426 aseptic revisions
Siri B WINTHER 1, Jomar KLAKSVIK 1, Olav A FOSS 1,2, Tina Strømdal WIK 1,2, Tarjei EGEBERG 1, and Otto S HUSBY 1,2
1 Department of Orthopaedic Surgery, St. Olavs Hospital HF, Trondheim; 2 Department of Neuromedicine and Movement Science, Faculty of Medicine and Health Science, Norwegian University of Science and Technology NTNU, Trondheim, Norway
Background and purpose — Studies evaluating pain and patient-reported outcome measures (PROMs) related to type of revision total hip arthroplasty (rTHA) are sparse. Our aim was to compare pain, physical function, quality of life, and patient satisfaction among different types of aseptic rTHA at 1-year follow-up.
Patients and methods — We performed a retrospective study from an institutional registry with 426 primary THAs scheduled for rTHA in a fast-track setting between 2012 and 2021. Revisions were grouped by 4 types of surgery: head and/or liner exchange, cup revision, stem revision, and cup and stem revision. Pain during mobilization and at rest (NRS 0–10), physical function (HOOS-PS and HHS) and health-related quality of life (EQ-5D) were registered preoperatively, at 3 months, and 1 year postoperatively. Patient satisfaction was surveyed at the 1-year follow-up by 2 questions related to hip function and willingness to undergo the same surgery.
Results — With a response rate of 85%, all outcomes improved in the 4 groups but there were neither statistical nor clinical differences between types of rTHA at 1-year follow-up. NRS pain during mobilization improved overall by 2.7 (95% confidence interval 2.3–3.1) until 1-year follow-up, both being statistically significant and clinically relevant. The improvements were mainly seen at the 3-month follow-up, with minor progress observed at 1 year. About 80% reported improved hip function and willingness to undergo the surgery again at the 1-year follow-up.
Conclusion — Significant improvements in NRS pain and PROMS were found in all groups after rTHA, with no group differences at 1 year. This is relevant preoperative information for both clinicians and patients eligible for rTHA.
Citation: Acta Orthopaedica 2023; 94: 360–365. DOI: https://doi.org/10.2340/17453674.2023.16906.
Copyright: © 2023 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for non-commercial purposes, provided proper attribution to the original work.
Submitted: 2023-04-25. Accepted: 2023-06-16. Published: 2023-07-20.
Correspondence: siri.bjorgen@ntnu.no
All authors contributed to the study design and data interpretation. OSH, TSW, and TE performed the surgeries. SBW contributed to data registration. JK performed the data analyses. All authors contributed to revising the draft manuscript written by SBW.
Handling co-editor: Taco Gosens
Acta thanks Kirill Gromov and Willem B Schreurs for help with peer review of this manuscript.
The number of primary total hip arthroplasties (THA) is expected to increase significantly over the coming decades due to a growth in the population, and hence the number of revisions (rTHA) will increase. Increased use of THA in younger patients, in combination with increasing life expectancy whereby patients live longer with their THA, also increases the requirement for revisions [1]. The success of THA has traditionally been measured by implant survival but has over the last decade been supplemented by patientreported outcome measures (PROMs) [2-4]. Patient satisfaction after arthroplasties is related to preoperative expectations, which should be based on realistic goals for postoperative outcomes [5]. The fast-track clinical pathway optimizes the patient course through all aspects of the treatment chain and emphasizes extensive preoperative information. This has been demonstrated to yield a high degree of patient satisfaction [6]. The fast-track patient course has conventionally been applied to primary arthroplasties but has recently been demonstrated to also yield good results in rTHA [7]. In addition to meting preoperative expectations and providing the patient with a satisfactory hospital experience, pain relief is the most important outcome for the patient [8,9]. It has previously been found that patients undergoing aseptic rTHA improve pain and PROMs at 1-year follow-up [4,9], and it has recently been demonstrated that 2-year postoperative PROMs are not associated with the indication for rTHA [10]. However, to what extent the type of rTHA influences PROMs has not been studied and needs further investigation. The less extensive revision procedure without exchange of the cup and/or stem yields no trauma to the bone and less trauma to the soft tissue. This might be expected to result in lower pain and better physical function in the head and/or liner exchange group. We aimed to compare PROMs from patients undergoing elective rTHA with respect to revision type, performed at a single hospital within a standardized fast-track patient course.
Patients and methods
Design
The study was an institutional register-based cohort study with THA patients who underwent rTHA with either a partial or a total exchange of implants in a fast-track clinical course at our orthopedic department.
Patients
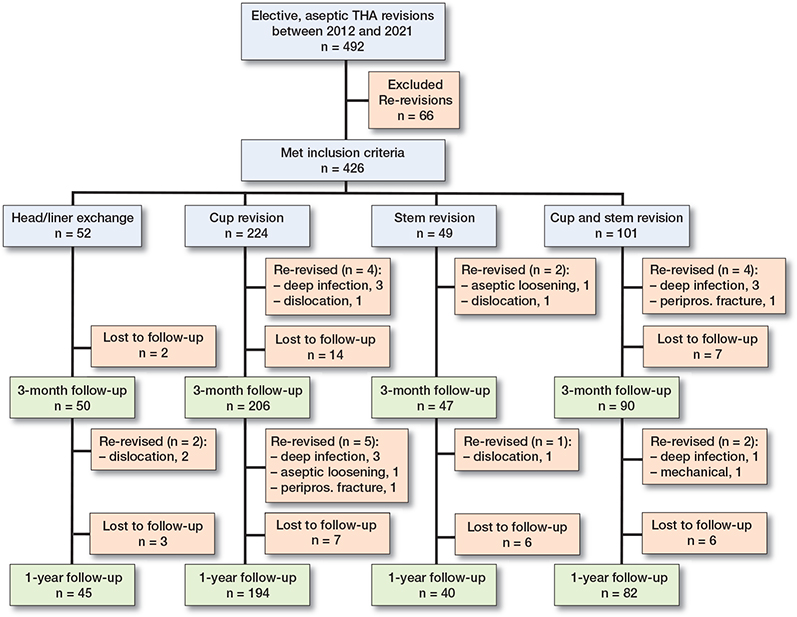
All THA patients scheduled for elective first-time aseptic revision from March 2012 through 2021 were eligible for study participation. In all rTHA 5 biopsies were taken intraoperatively, and the revision was defined as aseptic if there was no growth of bacteria in either of the samples. Acute events such as femoral and periprosthetic fractures were not included due to the elective setting of the fast-track pathway, neither were dislocations with closed reduction or with acute revision. All rTHA surgeries were categorized into 4 groups, based on the type of revision surgery: (a) head and/or liner exchange, (b) cup revision, (c) stem revision, (d) revision of both cup and stem. A flowchart of patient enrollment is presented in Figure 1. The study is reported according to STROBE guidelines.
Fast-track
Patient treatment was based on principles from the well-established standardized clinical fast-track patient course [6]. The multimodal analgesic regimen was standardized. Pre-medication consisted of paracetamol (1.5–2 g), dexamethasone (16–20 mg), and etoricoxib (90 mg) or naproxen (50 mg), without use of any benzodiazepines. Surgeries were performed under spinal anesthesia with 2.5–3.0 mL bupivacaine (0.5% plain). An epidural catheter was inserted and activated when needed postoperatively. Propofol infusions were administered for sedation if needed. A standardized program for intraoperative fluid administration consisted of 1–1.5 L Ringer’s acetate, 15 mg/kg tranexamic acid (max. 1.5 g), and cephalothin (2 g). All patients were given cephalosporin (1 g x 4) within 9 hours, or clindamycin (600 mg x 4) within 24 hours. The first dose was given 30 minutes preoperatively. Postoperatively in the hospital, patients received daily oxycodone (10 mg controlled release x 2), acetaminophen (1 g x 4), and naproxen + esomeprazole (x 2). In addition, oxycodone (5 mg immediate release) was given as rescue medication if needed (pain score on the numeric rating scale [NRS] > 4). Further details concerning the fast-track clinical patient course at our department have been published previously [11].
Surgical procedures and implants
All revisions were performed with the patient in a lateral position. Until 2015, they were performed using a direct lateral approach (DLA). From January 2015, this was changed to a posterior approach (PA) in combination with an extended trochanteric osteotomy when needed to remove the stem. For removal of cemented stems, mechanical instruments designed for cement removal were used alone or in combination with a long-wave ultrasound device. When uncemented cups were removed, an Explant system (Zimmer, Warsaw, IN, USA) was used. Cemented polyethylene cups were first reamed out, or mechanically removed in order to expose the cement. Uncemented implants were used for both acetabular and femoral reconstruction. The stems were coated with hydroxyapatite, and the cups were porous-coated, supplemented with fixation screws when necessary. Tantalum augments were used to reconstruct the pelvis in cases with major acetabular defects (Paprosky 2b, 3a). Bipolar cups or larger head diameter (36 mm) were preferred when dislocation was the main indication for surgery. Femoral defects were secured with stems that bypassed the defect, of at least 2.5 times the length of the femoral diameter. The patients were given 4 doses of first-generation cephalosporin for infection prophylaxis. 5 experienced orthopedic surgeons specialized in revision arthroplasty surgery performed or assisted on all rTHA procedures.
Data collection and outcomes
Data was registered at the preoperative outpatient clinic, during hospitalization, and at outpatient physical therapy at 3 months and at 1-year follow-up. All data was collected using paper forms and scanned into the database for electronic verification.
The primary outcome was pain during mobilization at 1-year follow-up, reported using the numeric rating scale (NRS 0–10) (0 representing no pain). Improvement in NRS pain from preoperatively to 1-year follow-up was also evaluated. Minimal clinical important improvement (MCII) is the minimum improvement relevant to the patient, representing a clinically significant improvement, and the patient acceptable symptom state (PASS) is defined as the threshold below which the patient considers the outcome satisfactory [12]. Patients with an improvement in NRS pain score of 1.7 or more from preoperatively to 1-year follow-up were defined as MCII responders, and patients with a lower NRS pain score than the PASS threshold of 4.6 at 1 year were defined as PASS responders. These thresholds were based on a previous publication [12].
Secondary outcomes were pain at rest, the disease-specific HHS and HOOS-PS, and the generic EQ-5D. Patient satisfaction was evaluated at 1-year follow-up by 2 specific anchor questions related to self-perceived hip function and willingness to have the same surgery again: “How does the leg that was operated on work today compared with before surgery?” and “Based on your experience to date, would you go through the same surgery again?”. The indication for revision was recorded by the lead surgeon immediately postoperatively and categorized by the group of revision surgeons for study purposes (Table 2). Time from primary THA to rTHA, surgery time, length of hospital stay (LOS), postoperative complications, and re-revisions within 1 year were also registered.
Statistics
A generalized linear mixed model was used to analyze pain during mobilization, preoperatively, and at 3 months and 1 year after surgery, for the 4 revision groups. Time points for data collection and the 4 groups were modelled as fixed factors. Age, sex, and surgical approach were used as covariates in the analysis. A random subject intercept was included. The data was modelled with an identity link function and normality of residuals was verified by histograms. 3.5% of the patients had bilateral revision surgeries. A preliminary analysis excluding bilateral revisions showed no influence on the outcomes. Therefore, they were treated as independent cases in the final analysis. Equivalence between groups was assumed when the 90% CI of the group differences fell within the interval defined by the MCII boundaries. All plots represent descriptive statistics, except Figure 2b, which is a model plot of the primary outcome, pain during mobilization. Continuous data is displayed in figures as mean with 95% confidence intervals (CI) and in tables as mean (range) score. Categorical data is presented in tables and figures as frequencies and percentages. Statistical analyses were performed using SPSS v28 (IBM Corp, Armonk, NY, USA).
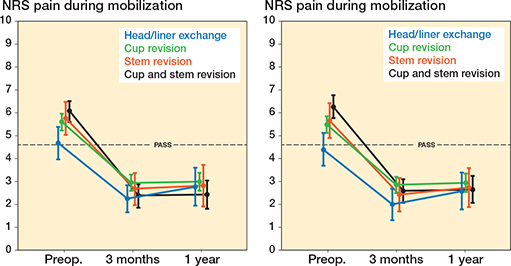
Figure 2. Pain during mobilization presented by descriptive values (left panel) and adjusted for age, sex, and surgical approach (right panel) of 4 different rTHA groups preoperatively and at 3-month and 1-year follow-up. PASS: patient acceptable symptom state.
Ethics approval, data sharing, funding, and disclosures
The study was approved by the regional committee for medical and health research ethics (approval 123645) and the National Archive and Center for Research Data (approval 480820). The study was conducted in accordance with relevant guidelines and regulations. Patients were informed about the registry and gave written informed consent to study participation before inclusion. Grouped data or tables of data without possibility of identification are available. No grant or funding was received, and the authors declare no conflicts of interests. Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.16906
Results
Patients (Figure 1)
A total of 426 revisions were included, of which 52 were head/liner exchange, 224 cup revisions, 49 stem revisions, and 101 cup and stem revisions. Of the 426 revisions, 15 patients (3.5%) had bilateral revisions. 361 (85%) revisions completed the 1-year follow-up with an outcome completeness score of about 95%. The most common indications for rTHA were aseptic loosening (41%) and dislocation (27%). Patient demographics are presented in Table 1. Time from primary THA to rTHA, surgery time, LOS, postoperative complications, and re-revisions within 1 year are presented in Table 2. Indications for rTHA in each group are given in Table 3.
Outcomes
Pain during mobilization at 1-year follow-up (Figure 2)
No statistically significant between-group differences were found, nor any clinically meaningful differences by testing for equivalence (Figure 3). Mean pain score by groups was 2.6 (CI 1.8–3.4) in the head/liner, 2.9 (CI 2.5–3.3) in the cup, 2.7 (CI 1.9–3.6) in the stem, and 2.6 (CI 2.1–3.2) in the cup and stem revision group.
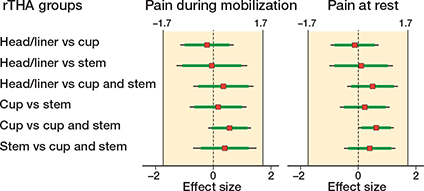
Figure 3. Equivalence plot of pain during mobilization and at rest for the groups at 1-year follow-up. Mean differences (red squares) with 90% CI (thick green lines) and 95% CI (thin lines).
Changes in pain score during mobilization from preoperatively to 1-year follow-up (Figure 2)
The mean pain score was statistically significantly improved in all groups by 2.7 (CI 2.3–3.1) with no difference between groups.
MCII and PASS pain responders for pain (Figure 4)
The numbers of MCII responders in the 4 groups were 51–69% for pain during mobilization and 37–47% for pain at rest. The corresponding numbers of PASS responders were 67–76% and 81–89% respectively.
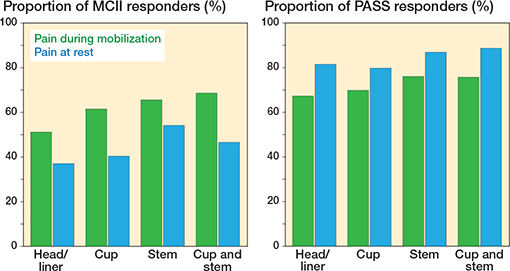
Figure 4. Proprotion of MCII (left panel) and PASS (right panel) responders at 1-year follow-up. Results are stratified into the 4 different revision THA groups.
PROMs (Figures 5 and 6) and patient satisfaction at 1-year follow-up (Figure 7)
No statistically significant differences were found among the groups at 1-year follow-up regarding NRS pain at rest, HOOS-PS, HHS, and EQ-5D, or in patient satisfaction.
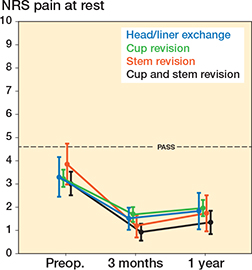
Figure 5. Pain at rest presented by descriptive values in 4 different rTHA groups preoperatively and at 3-month and 1-year follow-up. PASS, see Figure 2.
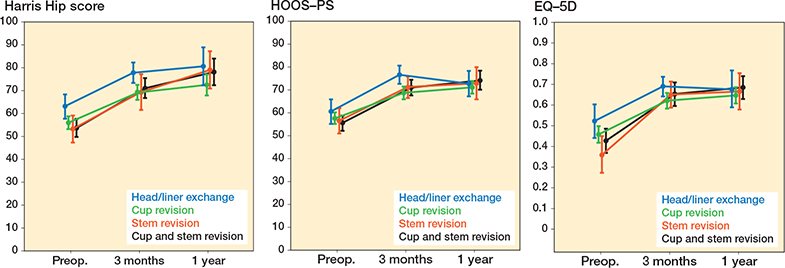
Figure 6. Descriptive values of the HHS (top), HOOS-PS (middle), and EQ-5D (bottom) in the 4 groups preoperatively and at 3-month and 1-year follow-up.
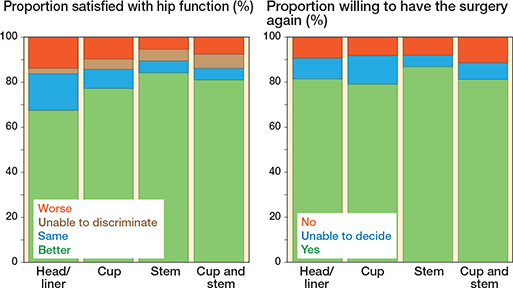
Figure 7. Patient satisfaction related to hip function (left) and willingness to have the surgery again (right) in the 4 groups at 1-year follow-up.
Discussion
At 1-year follow-up, neither statistically significant nor clinically relevant differences in pain score or PROMs were found between first-time revision types of a THA. The improvements from preoperatively to 1-year follow-up were both statistically significant and clinically relevant in all 4 revision groups. About 80% of the patients were PASS responders with an acceptable pain level at 1-year follow-up, which corresponds well to the number of patients reporting improved function and that they would have the same surgery again.
It has previously been shown that the outcomes following rTHA are not related to the indication for surgery and do not influence the results [10]. However, wear and osteolysis can be asymptomatic, which might explain the lower preoperative pain level in the head and/or liner exchange group in the present study. Exchange of modular parts yields no trauma to the bone, and the surgery is normally less traumatic to the soft tissues. We found a trend whereby the results for all PROMs up to 3 months’ follow-up were more favorable in the head/liner exchange group. This might, however, be due to advantageous preoperative scores as the improvements are similar to the other groups. On the other hand, the cup and stem revision group demonstrated the largest improvement in NRS pain during mobilization, but this group had a higher preoperative pain score. Nevertheless, the results at 1-year follow-up do not differ among the groups.
An average of 62% were MCII responders in the 4 groups in pain during mobilization whereas for pain at rest this was 45%. The head/liner exchange group had the lowest number of responders, probably a consequence of lower preoperative pain level. At 1-year follow-up, an average of 72% were PASS responders for pain during mobilization and 84% at rest (Figure 4). This is a reasonable finding as pain at rest is lower than pain during mobilization and lower preoperative pain scores leave less room for improvement, and the better preoperative pain score results in a concomitant higher probability of a satisfactory result at 1-year follow-up.
Pain, physical function, and quality of life were in line with previous publications on rTHA [13-17] with improvements in all 4 groups from preoperatively until 1-year follow-up, which is considered both statistically significant and clinically relevant [18-21]. The greatest improvements occurred within 3 months and thereafter levelled off at 1 year. A recent review found no difference in PROMs between 1 and 2 years after THA, hence leaving no additional value in collecting data in routine practice at both 1 and 2 years [22].
Age was significant in the statistical model and patients in the head/liner exchange group were younger than patients in the other groups. Thus, when adjusting for covariates, the pain score was below the other groups at all timepoints, yet no statistical differences were found (Figure 2). They also had a higher physical function score at all time points measured by the objective HHS compared with the other groups (Figure 6). This was the only group that reached a function level that was considered “good” as defined by the HHS at 1-year follow-up, whereas the other groups reached only a “fair” function level. However, pain and self-perceived function measured by the subjective HOOS-PS score deteriorated from 3 to 12 months in the head/liner exchange group (Figure 6). This might be related to higher expectations among the youngest patients regarding activity level, which requires good physical function with a corresponding acceptable pain level. This is consistent with the subjective anchor question concerning hip function where the head/liner exchange group has the lowest number who replied that function had improved from preoperatively until 1-year follow-up (Figure 7).
In line with previous findings [23], some 80% of the patients in the present study reported better hip function and willingness to have the surgery again at 1-year follow-up, which corresponds well with the number of PASS responders for pain. This indicates a correlation between patient satisfaction and pain, which emphasizes that pain might be the most important outcome for the patient following rTHA [23]. These results can be provided to patients in the preoperative information class that all fast-track patients attend prior to surgery.
The strength of the study is that the surgeries were performed in a single hospital department with a standardized fast-track patient course. Also, the evaluation of several different PROMS and a response rate of 85% at 1-year follow-up strengthens the study. Only elective aseptic revisions were included, which represents a study limitation as generalization of the results is limited to the elective setting.
In conclusion no difference in pain, physical function, or quality of life was found 1 year after rTHA comparing a less extensive with more extended procedures.
- Pabinger C, Lothaller H, Portner N, Geissler A. Projections of hip arthroplasty in OECD countries up to 2050. Hip Int 2018; 28(5): 498-506. doi: 10.1177/1120700018757940.
- Wilson I, Bohm E, Lübbeke A, Lyman S, Overgaard S, Rolfson O, et al. Orthopaedic registries with patient-reported outcome measures. EFORT Open Rev 2019; 4(6): 357-67. doi: 10.1302/2058-5241.4.180080.
- Ray G S, Ekelund P, Nemes S, Rolfson O, Mohaddes M. Changes in health-related quality of life are associated with patient satisfaction following total hip replacement: an analysis of 69,083 patients in the Swedish Hip Arthroplasty Register. Acta Orthop 2019:1-5. doi: 10.1080/17453674.2019.1685284.
- Siddiqi A, Warren J, Anis H K, Barsoum W K, Bloomfield M R, Briskin I, et al. Do patient-reported outcome measures improve after aseptic revision total hip arthroplasty? Hip Int 2021: 11207000211036320. doi: 10.1177/11207000211036320.
- Swarup I, Henn C M, Gulotta L V, Henn R F 3rd. Patient expectations and satisfaction in orthopaedic surgery: a review of the literature. J Clin Orthop Trauma 2019; 10(4): 755-60. doi: 10.1016/j.jcot.2018.08.008.
- Husted H. Fast-track hip and knee arthroplasty: clinical and organizational aspects. Acta Orthop 2012; 83(346, Suppl.): 1-39. doi: 10.3109/17453674.2012.700593.
- Lindberg-Larsen M, Petersen P B, Corap Y, Gromov K, Jørgensen C C, Kehlet H. Fast-track revision hip arthroplasty: a multicenter cohort study on 1,345 elective aseptic major component revision hip arthroplasties. Acta Orthop 2022; 93: 341-7. doi: 10.2340/17453674.2022.2196.
- Hamilton D F, Lane J V, Gaston P, Patton J T, Macdonald D, Simpson A H, et al. What determines patient satisfaction with surgery? A prospective cohort study of 4709 patients following total joint replacement. BMJ Open 2013; 3(4): e002525. doi: 10.1136/bmjopen-2012-002525.
- Wik T S, Klaksvik J, Husby O S, Rasch A, Winther S B. Patient-reported outcome after primary and aseptic revision hip arthroplasty: 1-year follow-up of 3,559 primary and 406 revision THAs in an institutional registry. Acta Orthop 2022; 93: 132-7. doi: 10.2340/17453674.2021.852.
- Innocenti M, Smulders K, Willems J H, Goosen J H M, van Hellemondt G. Patient-reported outcome measures, complication rates, and re-revision rates are not associated with the indication for revision total hip arthroplasty: a prospective evaluation of 647 consecutive patients. Bone Joint J 2022; 104-b(7): 859-66. doi: 10.1302/0301-620x.104b7.Bjj-2021-1739.R1.
- Winther S B, Foss O A, Wik T S, Davis S P, Engdal M, Jessen V, et al. 1-year follow-up of 920 hip and knee arthroplasty patients after implementing fast-track. Acta Orthop 2015; 86(1): 78-85. doi: 10.3109/17453674.2014.957089.
- Tubach F, Ravaud P, Martin-Mola E, Awada H, Bellamy N, Bombardier C, et al. Minimum clinically important improvement and patient acceptable symptom state in pain and function in rheumatoid arthritis, ankylosing spondylitis, chronic back pain, hand osteoarthritis, and hip and knee osteoarthritis: results from a prospective multinational study. Arthritis Care Res (Hoboken) 2012; 64(11): 1699-707. doi: 10.1002/acr.21747.
- van der Wees P J, Wammes J J, Akkermans R P, Koetsenruijter J, Westert G P, van Kampen A, et al. Patient-reported health outcomes after total hip and knee surgery in a Dutch University Hospital setting: results of twenty years clinical registry. BMC Musculoskelet Disord 2017; 18(1): 97. doi: 10.1186/s12891-017-1455-y.
- Zampelis V, Ornstein E, Franzén H, Atroshi I. A simple visual analog scale for pain is as responsive as the WOMAC, the SF-36, and the EQ-5D in measuring outcomes of revision hip arthroplasty. Acta Orthop 2014; 85(2): 128-32. doi: 10.3109/17453674.2014.887951.
- Postler A E, Beyer F, Wegner T, Lutzner J, Hartmann A, Ojodu I, et al. Patient-reported outcomes after revision surgery compared to primary total hip arthroplasty. Hip Int 2017; 27(2): 180-6. doi: 10.5301/hipint.5000436.
- Adelani M A, Mall N A, Nyazee H, Clohisy J C, Barrack R L, Nunley R M. Revision total hip arthroplasty with retained acetabular component. J Bone Joint Surg Am 2014; 96(12): 1015-20. doi: 10.2106/jbjs.L.01177.
- Korbee S, Van Kempen R, Van Wensen R, Van der Steen M, Liu W Y. Measurement properties of the HOOS-PS in revision total hip arthroplasty: a validation study on validity, interpretability, and responsiveness in 136 revision hip arthroplasty patients. Acta Orthop 2022; 93: 742-9. doi: 10.2340/17453674.2022.4572.
- Katakam A, Hosseinzadeh S, Humphrey T J, Collins A, Shin D, Melnic C M, et al. Different designs of proximal femoral stems for total hip arthroplasty: mid-term clinical and patient-reported functional outcomes. Cureus 2021; 13(11): e19745. doi: 10.7759/cureus.19745.
- Tubach F, Ravaud P, Beaton D, Boers M, Bombardier C, Felson D T, et al. Minimal clinically important improvement and patient acceptable symptom state for subjective outcome measures in rheumatic disorders. J Rheumatol 2007; 34(5): 1188-93. https://www.jrheum.org/content/jrheum/34/5/1188.full.pdf.
- Walters S J, Brazier J E. Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual Life Res 2005; 14(6): 1523-32. doi: 10.1007/s11136-004-7713-0.
- Singh J A, Schleck C, Harmsen S, Lewallen D. Clinically important improvement thresholds for Harris Hip Score and its ability to predict revision risk after primary total hip arthroplasty. BMC Musculoskelet Disord 2016; 17: 256. doi: 10.1186/s12891-016-1106-8.
- Ramkumar P N, Navarro S M, Haeberle H S, Ng M, Piuzzi N S, Spindler K P. No difference in outcomes 12 and 24 months after lower extremity total joint arthroplasty: a systematic review and meta-analysis. J Arthroplasty 2018; 33(7): 2322-9. doi: 10.1016/j.arth.2018.02.056.
- Hamilton D F, Simpson P M, Patton J T, Howie C R, Burnett R. Aseptic revision knee arthroplasty with total stabilizer prostheses achieves similar functional outcomes to primary total knee arthroplasty at 2 years: a longitudinal cohort Study. J Arthroplasty 2017; 32(4): 1234-40.e1. doi: 10.1016/j.arth.2016.10.028.